Abstract
Hypoglycaemia is an important complication of Plasmodium falciparum malaria infection, which can be lethal if not treated. A decrease in blood sugar (BS) level has been correlated with disease severity, parasitaemia and the use of certain antimalarial drugs. This study explored the relationship between pancreatic pathology, including the expressions of insulin and glucagon in the islets of Langerhans, and the BS levels in P. falciparum malaria patients. Pancreatic tissues from malaria patients were divided into three groups, namely those with BS < 40 mg/dl, BS = 40–120 mg/dl, and BS > 120 mg/dl. In P. falciparum malaria, pancreatic tissues showed numerous parasitised red blood cells (PRBCs) in the capillaries, oedema, acinar necrosis and the presence of inflammatory cells. The islet size and the expression of insulin were significantly increased in P. falciparum malaria patients with hypoglycaemia. In addition, insulin expression was positively correlated with islet size and negatively correlated with BS levels. This pioneer study documents an increase in insulin expression and an increase in islet size in hypoglycaemic patients with P. falciparum malaria. This could contribute to the pathogenesis of hypoglycaemia and provides evidence for the potential need to effectively manage the hypoglycaemia seen in malaria infection.
Similar content being viewed by others
Introduction
Malaria caused by Plasmodium falciparum is still a widespread parasitic infection causing high morbidity and mortality. The main clinical presentations of severe malaria include cerebral malaria, metabolic acidosis, anaemia, acute kidney injury, pulmonary oedema, renal failure, hypoglycaemia, hypertension and shock1. Of these severe manifestations, clinical hypoglycaemia occurs in 8–30% of all severe P. falciparum malaria cases2,3. Children and pregnant women are prone to develop hypoglycaemia in severe malaria possibly linked to lowered immunity. The clinical symptoms of severe hypoglycaemia include hunger, sweating, palpitation, dyspnoea, tachycardia, confusion, anxiety, somnolence, seizure, breathlessness, coma, and conditions may progress to death if not properly treated1. The presentation of hypoglycaemia can mimic clinical cerebral malaria but can be differentiated by blood sugar (BS) determination.
Insulin stimulates cells to take up glucose from blood resulting in lower BS levels. On the other hand, glucagon stimulates hepatocytes to release glucose into the blood. Hypoglycaemia in malaria is diagnosed when BS levels are below 2.2 mmol/l or 40 mg/dl1. The causes of hypoglycaemia in severe P. falciparum malaria had been reported to be due to the consumption of glucose by malaria parasites4, the effect of antimalarials such as quinine5, malarial hepatitis6, defects in the gluconeogenesis pathway7, the effect of tumor necrosis factor release and the influence of other cytokines produced during malaria infection8.
Various studies have described histological changes in the pancreas with infectious diseases. In the study of canine babesia, pancreatic tissues show interstitial and stromal oedema, parenchymal haemorrhages, parenchymal necrosis, fat necrosis and infiltration of a large number of neutrophils9. In human pancreatic tissues with leptospirosis, the histopathological changes include oedema, mild inflammatory infiltrate of lymphocytes, haemorrhages, congestion, fat necrosis and calcification10. Oedema and pancreatitis were histopathological changes noted in dengue fever11. The histopathology of pancreatic tissues with P. falciparum malaria infection is still incompletely understood and only limited information is available. This study aimed to explore pancreatic pathology in P. falciparum malaria and to investigate the expressions of insulin and glucagon in the islets of Langerhans in parallel.
Results
Summary of clinical data
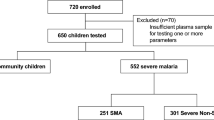
Pancreatic tissues were obtained from 27 patients who died from P. falciparum malaria, comprising of 8 cases defined with hypoglycaemia (BS < 40 mg/dl), 9 cases with BS = 40–120 mg/dl, and 10 cases defined with hyperglycaemia (BS > 120 mg/dl). Eight normal pancreas from non-malaria patients were used as controls. No difference in clinical parameters was observed across the groups, including: mean age (years) (26.7 ± 6.0, 21.8 ± 4.2, 33.5 ± 8.1), sex ratio (M:F) (5:3, 6:3, 7:3), number of days of fever (4.3 ± 1.0, 1.3 ± 1.1, 2.9 ± 1.0), haemoglobin level (g/dl) (9.2 ± 0.9, 10.6 ± 1.2, 10.0 ± 1.4), and white blood cell count (×103/μl) (9.2 ± 2.2, 12.1 ± 5.2, 12.2 ± 3.3) (all P > 0.05). There was a significant negative correlation between parasitaemia and BS levels (rs = −0.610, P = 0.046).
Histopathological changes of pancreatic tissues in P. falciparum malaria patients
Pancreatic tissues from P. falciparum malaria patients usually showed oedema, acinar necrosis and inflammatory reactions, in addition to the presence of parasitised red blood cells (PRBCs). However, there was no difference in the overall total score of histopathological changes between malaria patients and control group (P = 0.392). The histopathology of pancreatic tissues from malaria patients, compared to normal pancreatic tissues is illustrated in Fig. 1. Normal histology of the pancreas shows intact islets of Langerhans and acinar cells forming exocrine glands (Fig. 1A). The number of pancreatic islets in malaria patients is similar to the control group (1–2 cells/mm2). Numerous PRBCs were frequently seen in the capillaries of pancreas from severe malaria patients (Fig. 1B). Oedema was characterised by widening of the pancreatic interlobular and interglandular spaces (Fig. 1C). There was a significant difference between pancreatic oedema in malaria patients and the control group (P = 0.002), especially in malaria patients with BS < 40 mg/dl (P = 0.004) and those with BS = 40–120 mg/dl (P = 0.004). Necrosis of acinar cells is considered in pale staining cells with the loss of nuclei and visible cellular distortion, causing deformation in pancreatic parenchyma (Fig. 1D). Acinar necrosis was evident in all groups of malaria patients compared to the control group (P < 0.001). The presence of inflammatory cells, particularly lymphocytes, neutrophils and occasionally eosinophils in the interlobular septum and interglandular areas were significantly higher in all malaria patients compared to the control group (P = 0.011) (Fig. 1E). Fibrosis was not observed in the malarial pancreas. Areas of haemorrhage in pancreatic parenchyma and fat necrosis in peripancreatic tissue were occasionally seen in malaria patients compared to normal pancreas (P = 0.196 and P = 0.067, respectively). The quantification of total histopathological changes in the pancreatic tissues of malaria patients compared with the control group are shown in Table 1.
Histopathological changes of pancreas in P. falciparum malaria patients. Normal pancreas shows unremarkable islets of Langerhans and intact acini cells (A, ×400). Pancreatic changes include presence of parasitised red blood cells (PRBCs) within the pancreatic capillaries (B- arrows, ×400), oedema in interlobular and intergladular spaces of pancreatic parenchyma (C- arrows, ×200), acinar necrosis (D- arrows, ×400), and presence of lymphocytes (E- arrows), and eosinophils (E- arrowheads) in the interlobular spaces (×400).
Evaluation of pancreatic islet size
The comparative size of islets of Langerhans is depicted in Fig. 2A. The diameter of an islet was largest in P. falciparum malaria with hypoglycaemia (135.80 ± 10.23 µm), compared to P. falciparum malaria with BS = 40–120 mg/dl (91.89 ± 3.08 µm, P = 0.001), P. falciparum malaria with hyperglycaemia (70.46 ± 1.80 µm, P < 0.001), and the control group (95.07 ± 6.82 µm, P = 0.004). The calculated area of a pancreatic islet was 15,136.99 ± 2,625.02 µm2, 6,702.34 ± 458.21 µm2 and 3,922.37 ± 200.76 µm2, respectively, as compared to control group (7,012.70 ± 1,088.41 µm2). There was a significant negative correlation between the size of pancreatic islets and BS levels (rs = −0.869, P < 0.001) in malaria patients (Fig. 2B). No significant association was revealed between islet size and other clinical parameters (age, sex, days of fever, parasitaemia, haemoglobin, white blood cell count, albumin and globulin) (all P > 0.05).
The size of pancreatic islets (µm) of P. falciparum malaria patients. Data presented as mean ± SEM. *significant difference between groups, P < 0.05 (A), and negative correlation between islet size, as measured by islet diameter in P. falciparum malaria patients (n = 27) and blood sugar (BS) levels (B).
Expressions of insulin and glucagon
Insulin- and glucagon- expressing cells were detected as brown color in the cytoplasm of the cells in the islets of Langerhans. Generally, insulin expression was demonstrated in the center of the pancreatic islets, whereas glucagon expression was located at the periphery of the islets (control, Fig. 3A,B). In this study, insulin expression was prominent in the group of P. falciparum malaria patients with hypoglycaemia (Fig. 3C), and those with BS = 40–120 mg/dl (Fig. 3E), compared to the control group (P = 0.014 and P = 0.011, respectively). A trend towards a reduction in the expression of insulin was revealed in malaria with hyperglycaemia (Fig. 3G). For glucagon expression, weak positive staining was observed in malaria patients with hypoglycaemia (Fig. 3D), whereas moderate positive staining was present in the group of P. falciparum malaria patients with BS = 40–120 mg/dl (Fig. 3F) and the hyperglycaemic group (Fig. 3H). No significant difference in glucagon expression was observed between all malaria patients and the control group (P = 0.386). The quantified total expression scores of insulin and glucagon are shown in Fig. 4. There was a significant negative correlation between BS levels and the total insulin expression score (rs = −0.728; P = 0.002) (Fig. 5A). In addition, insulin expression was directly correlated with islet size (rs = 0.696; P = 0.004) (Fig. 5B).
The immunohistochemical staining for insulin and glucagon. Representative sections of human pancreas immunostained for insulin (left panel) and glucagon (right panel) from normal pancreatic tissues (A and B), pancreatic tissues of P. falciparum malaria patient with BS < 40 mg/dl (C and D), pancreatic tissues with BS = 40–120 mg/dl (E and F) and pancreatic tissues with BS > 120 mg/dl (G and H). All images are ×200 magnification.
Expressions of insulin (A) and glucagon (B) in P. falciparum malaria and control groups. A significant increase in insulin expression was observed in malaria group with BS < 40 mg/dl (P = 0.014) and malaria group with BS = 40–120 mg/dl (P = 0.011), compared with the control group. No significant difference in glucagon expression was observed in all groups.
Discussion
Histopathological changes documented in pancreatic tissues of P. falciparum malaria patients include oedema in the interlobular and interglandular spaces, acinar necrosis and inflammatory reactions. Although these changes were frequently found in P. falciparum malaria patients with hypoglycaemia (oedema and necrosis), similar histopathological changes were reported in other infectious diseases including dengue infection11, leptospirosis10 and babesia9. Limited studies have been reported on the pathology of pancreatic tissues in severe P. falciparum malaria. Previous rare autopsy findings showed an enlarged pancreas with minimal fluid in the peritoneal cavity, related clinically to pancreatitis12, and necrotic pancreatic tissue13. Our findings are similar to reports in animals infected by other plasmodium species. In a study of P. berghei in mice, pancreatic tissues revealed acute inflammatory reactions of acini, islets cells and interlobular duct14. Another study of Macaca mulatta monkeys infected with P. knowlesi showed acinar necrosis and the disappearance of pancreatic islets15. In addition, hypoglycaemia was observed in animal models infected with P. knowlesi16. The inflammatory cells such as lymphocytes and neutrophils are crucial in the control of malarial parasite replication, which contribute to the subsequent elimination and resolution of the infection through the process of phagocytosis and/or production of inflammatory mediators17. Fibrosis, areas of haemorrhages and fat necrosis in the pancreatic tissues were not features of P. falciparum malaria patients.
The presence of PRBCs within the capillaries can cause an increase in blood viscosity. In addition, malaria parasites in the red blood cells (RBCs) can cause decrease in RBC membrane deformity. These circulatory disturbances can lead to tissue hypoxia, release of pancreatic acinar enzymes, impaired capillary and venous drainage, which in turn can lead to haemorrhagic pancreatic necrosis18. Fibrosis is characterized by the accumulation of extracellular matrix and an increase in fibroblastic reaction. Though fibrosis is not significantly present in P. falciparum malaria patients, possibly due to the acute nature of malaria infection, a previous study has reported that high BS levels can stimulate the proliferation of pancreatic stellate cells and subsequent increased in fibroblast production19.
Whether the increase in islet size is caused by malaria infection per se, or is secondary to antimalarial drugs, needs to be further investigated. Nevertheless, the enlarged pancreatic islets can contribute to hyperinsulinemia and subsequent hypoglycaemia seen in P. falciparum malaria patients.
The present study used immunohistochemical methods to demonstrate the expressions of insulin and glucagon in terms of distribution and intensity in the pancreatic tissues of P. falciparum malaria patients. Similar to previous reports, insulin immunopositive cells were found in greater density in the central part of the islets of Langerhans, compared to islet cells expressing glucagon, which are frequently detected around the periphery of pancreatic islets20.
The increased expression of insulin in P. falciparum malaria patients with hypoglycaemia can be secondary to the malaria parasite itself, the use of antimalarial drugs, alteration in the gluconeogenesis pathway, the effects of cytokines during malaria infection and renal injury6. Malaria parasites in the circulation need glucose from the host in order to produce energy, mainly via aerobic glycolysis, for their survival4. A previous report showed that high parasitaemia is associated with high glucose requirements by malaria parasites, which can lead to clinical hypoglycaemia21. Antimalarial drugs, such as quinine and quinidine have an effect on glucose metabolism in malaria patients, causing a decrease in BS level5. Most of our malaria patients were treated with quinine. Quinine has been reported to be a more potent stimulant of insulin secretion than quinidine5. These drugs act similarly to glucose on potassium permeability of the beta cells membrane, causing calcium influx and subsequent release of insulin to reduce BS levels5. We accept that quinine/quinidine have an effect in lowering insulin level and is still used in endemic areas and in places where artesunate is not available. Our data suggests the need for precautious use of quinine/quinidine in these circumstances, and recommend closed monitoring of the BS level of malaria patients. Other antimalarial drugs, such as chloroquine, amodiaquine, mefloquine and halofantrine have no direct effect on insulin secretion22. Interestingly, the gluconeogenesis pathway is abnormal in severe P. falciparum malaria patients due to insufficient galactose substrate, resulting to low BS levels7. The effect of cytokines released during P. falciparum malaria infection, such as tumour necrosis factor (TNF), interleukin (IL)- 1 and 6 can inhibit the activity of phosphoenolpyruvate carboxykinase in the gluconeogenesis pathway and also mediate a reduction in hepatic glycogen content, hence the lower BS levels23,24. In addition, IL-1 and 6 have been reported to stimulate islet cell hyperplasia25. It can be hypothesised that IL-1 and 6 released during malaria infection can cause islet cell hyperplasia resulting to enlargement of pancreatic islets and subsequent increase in insulin expression. Furthermore, the kidney is an important organ involved in glucose regulation. Occurrence of acute kidney injury in severe P. falciparum malaria can affect the net glucose release and reabsorption, resulting in hypoglycaemia26.
The maintenance of a normal BS level is a critically important process in the metabolism in living organisms. Other parasitic infections have been reported to cause hypoglycaemia, e.g. trypanosomiasis in both human and animals27 and Chagas’s disease in a murine model28. Although these studies have shown that hypoglycaemia is not a major cause of death, in patients with severe P. falciparum malaria it is an important clinical manifestation that may well contribute significantly to high mortality rates. This pioneer study documents an increase in insulin expression and an increase in islet size in P. falciparum malaria patients with hypoglycaemia. The study will be useful for clinicians interested in understanding and managing the process of hypoglycaemia in severe P. falciparum malaria. The paper sets out recognizable histopathologic and immunologic changes associated with malarial pancreatic tissues.
Materials and Methods
Pancreatic tissues
Pancreatic tissues from P. falciparum malaria patients and control pancreas were obtained from the Department of Tropical pathology, Faculty of Tropical Medicine, Mahidol University, Bangkok, Thailand. For malarial cases, pancreatic tissues were divided into three groups based on the BS levels before death, namely BS < 40 mg/dl, BS between 40–120 mg/dl, and BS > 120 mg/dl. Control pancreatic tissues were obtained from accidental death cases, which showed normal islets of Langerhans, secretory acini, blood vessels, ducts and interstitial area. The study protocol was approved by the Ethics Committee of the Faculty of Tropical Medicine, Mahidol University, Thailand (MUTM 2015–041–01 and MUTM 2015-041-02). Methods were performed in accordance with the relevant guidelines and regulations of the above committee. Written informed consent from closest relatives was obtained for all malaria patients. The Ethics Committee of the Faculty of Tropical Medicine, Mahidol University, Thailand approved the use of control pancreatic tissues obtained from discarded autopsy specimen.
Histopathological preparation and evaluation
Left-over pancreatic tissues in paraffin blocks were re-embedded and processed using the standard histological protocol. Pancreatic tissues were sectioned at 4 μm thickness for histopathology and immunohistochemistry studies. Histopathological sections of pancreatic tissues were stained with Mayer’s haematoxylin and eosin (H&E). To study the average size of islets of Langerhans, islets were measured and evaluated by randomisation of 40 pancreatic islets under ×100 magnification using the “ImageJ” software program, developed by the National Institutes of Health, Bethesda, Maryland, USA. In addition, the pancreatic tissues were interpreted based on seven histological criteria, namely presence of parasitised red blood cells (PRBCs), oedema, haemorrhage, inflammatory infiltration, acinar necrosis, fat necrosis and fibrosis, under ×200 magnification. The changes were graded on a scale of 0–3. All criteria were assessed in the lobule, interlobular and intergladular areas, except for fat necrosis where the occurrence was at the peripancreatic tissue level. The grading criteria were based on previously described studies29,30, with minor modifications (Table 2).
Immunohistochemistry study of insulin and glucagon
The expressions of insulin and glucagon were detected by immunohistochemical staining, using an avidin-biotin peroxidase complex method (Vector Laboratories, Inc., USA). Primary antibodies used were rabbit polyclonal anti-insulin and anti-glucagon (Cell Signaling Technology, Inc., USA). Pancreatic tissues at 4 µm thickness were placed on an adhesive poly-L-lysine slide and heated in a hot oven at 56 °C for 30 minutes. Tissue sections were de-paraffinised and rehydrated in xylene and a decreasing series of graded alcohol, respectively. Then, the pancreatic tissue sections were incubated in 3% hydrogen peroxide diluted in distilled water for 30 minutes at 37 °C in order to block the endogenous peroxidase activity in the tissue. To retrieve the antigen, tissue sections were incubated with 0.1 M sodium citrate buffer at pH 6.0 in a 800 W microwave for 20 minutes. When the slides cooled down to room temperature (RT), the sections were washed in PBS buffer at pH 7.4. To reduce the non-specific background, the sections were incubated with diluted normal goat serum for 30 minutes. Then the pancreatic sections were incubated with a primary antibody (rabbit polyclonal anti-insulin or anti-glucagon (1:200 dilution) in a moisture chamber overnight at 4 °C. The following day, sections of pancreas were washed with PBS buffer at pH 7.4 for three time then incubated with diluted biotinylated goat anti-rabbit Ig G for 30 minutes at RT and treated with avidin-biotin peroxidase complex (ABC) conjugated with horseradish peroxidase (HRP) for 30 minutes. After all sections were washed, the tissue sections were reacted with 0.05% 3,3′ diaminobenzidine (DAB) and 0.01% H2O2 for 3 minutes, resulting in a brown coloration, which indicated the target antigen. Subsequently, pancreatic sections were counterstained with Mayer’s haematoxylin and mounted with a coverslip for microscopic evaluations.
Evaluation of immunohistochemical staining
The expressions of insulin and glucagon were evaluated in the cytoplasm of the islet cells in the pancreatic islets. Twenty islets from each pancreatic section were randomly observed at ×400 magnification. The percentages of insulin- and glucagon- expressing cells were determined by counting the number of positive cells over the total number of cells in each islet, multiplied by 100. The intensity of staining with both antibodies was subjectively scored as follows: 0 = no staining, 1 = weakly positive, 2 = moderately positive, and 3 = strongly positive. The total score (TS) was calculated by multiplying the percentage of positive cells (%) and staining intensity (I), according to previous study31.
Statistical analysis
Data were recorded into a computer database and analysed with SPSS software version 18.0. All quantitative data were represented as mean ± standard error of mean (SEM). The test for normality of distribution was calculated using Kolmogorov-Smirnov test. Comparisons of the difference in the size of pancreatic islets between groups were analysed by one way ANOVA. Correlations between variables of histological and immunohistochemical analyses and clinical data were analysed by Spearman’s rank correlation (rs). Mean differences in the total scores of histopathological and immunohistochemical studies between experimental groups were analysed by Mann-Whitney U test. The P-value < 0.05 was considered to be statistically significant.
References
Trampuz, A., Jereb, M., Muzlovic, I. & Prabhu, R. M. Clinical review: Severe malaria. Crit Care 7, 315–323, https://doi.org/10.1186/cc2183 (2003).
Thien, H. V., Kager, P. A. & Sauerwein, H. P. Hypoglycemia in falciparum malaria: is fasting an unrecognized and insufficiently emphasized risk factor? Trends Parasitol 22, 410–415, https://doi.org/10.1016/j.pt.2006.06.014 (2006).
Pandya, H. P. & Bhansali, P. Prognostic factors in severe and complicated malaria. Int J Med Sci. Public Health 5, 298–303 (2016).
Homewood, C. A. Carbohydrate metabolism of malarial parasites. Bull World Health Organ 55, 229–235 (1977).
Davis, T. M., Karbwang, J., Looareesuwan, S., Turner, R. C. & White, N. J. Comparative effects of quinine and quinidine on glucose metabolism in healthy volunteers. Br J Clin Pharmacol 30, 397–403 (1990).
Balaraju, G., Sridhar, D. & Muralidhar, L. Prognostic value of blood glucose levels at the time of admission in complicated malaria. Int J Multi. Res Dev 3, 118–121 (2016).
Dekker, E. et al. Glucose homeostasis in children with falciparum malaria: precursor supply limits gluconeogenesis and glucose production. J Clin Endocrinol Metab 82, 2514–2521, https://doi.org/10.1210/jcem.82.8.4131 (1997).
Elased, K. M., Taverne, J. & Playfair, J. H. Malaria, blood glucose, and the role of tumour necrosis factor (TNF) in mice. Clin Exp Immunol 105, 443–449 (1996).
Mohr, A. J., Lobetti, R. G. & van der Lugt, J. J. Acute pancreatitis: a newly recognised potential complication of canine babesiosis. J S Afr Vet Assoc 71, 232–239 (2000).
Daher, E. F., Brunetta, D. M., de Silva Junior, G. B., Puster, R. A. & Patrocinio, R. M. Pancreatic involvement in fatal human leptospirosis: clinical and histopathological features. Rev Inst Med Trop Sao Paulo 45, 307–313 (2003).
Shamim, M. Frequency, pattern and management of acute abdomen in dengue fever in Karachi, Pakistan. Asian J Surg 33, 107–113, https://doi.org/10.1016/S1015-9584(10)60019-X (2010).
Kumar, S., Jain, A. P. & V. Falciparum malaria presenting as acute pancreatitis. J Vector Borne Dis 47, 121–122 (2010).
Afandi, D. et al. Autopsy findings in severe malaria – a case report. Med J Indones 17, 2010–2015 (2008).
Onyesom, I. & Adu, F. Phyllanthus amarus possesses malarial curative and pancreatic tonic potentials in experimental mice. J Chem Pharm Res 7, 7–15 (2015).
Chen, L., Li, G., Lu, Y. & Luo, Z. Histopathological changes of Macaca mulatta infected with Plasmodium knowlesi. Chin Med J (Engl) 114, 1073–1077 (2001).
Anderios, F., Noorrain, A. & Vythilingam, I. In vivo study of human Plasmodium knowlesi in Macaca fascicularis. Exp Parasitol 124, 181–189, https://doi.org/10.1016/j.exppara.2009.09.009 (2010).
Autino, B., Corbett, Y., Castelli, F. & Taramelli, D. Pathogenesis of malaria in tissues and blood. Mediterr J Hematol Infect Dis 4, e2012061, https://doi.org/10.4084/MJHID.2012.061 (2012).
Zhou, Z. G. & Chen, Y. D. Influencing factors of pancreatic microcirculatory impairment in acute panceatitis. World J Gastroenterol 8, 406–412 (2002).
Zha, M. et al. High glucose aggravates the detrimental effects of pancreatic stellate cells on Beta-cell function. Int J Endocrinol 2014, 165612, https://doi.org/10.1155/2014/165612 (2014).
Bosco, D. et al. Unique arrangement of alpha- and beta-cells in human islets of Langerhans. Diabetes 59, 1202–1210, https://doi.org/10.2337/db09-1177 (2010).
Nsonwu-Anyanwu, A. C. et al. Falciparum malaria associated changes in biochemical indices in children. J Med Allied Sci 7, 29–33 (2017).
Phillips, R. E. et al. Hypoglycaemia and antimalarial drugs: quinidine and release of insulin. Br Med J (Clin ResEd) 292, 1319–1321 (1986).
del Rey, A. et al. IL-1 resets glucose homeostasis at central levels. Proc Natl Acad Sci USA 103, 16039–16044, https://doi.org/10.1073/pnas.0607076103 (2006).
Kiely, A., McClenaghan, N. H., Flatt, P. R. & Newsholme, P. Pro-inflammatory cytokines increase glucose, alanine and triacylglycerol utilization but inhibit insulin secretion in a clonal pancreatic beta-cell line. J Endocrinol 195, 113–123, https://doi.org/10.1677/JOE-07-0306 (2007).
Campbell, I. L., Hobbs, M. V., Dockter, J., Oldstone, M. B. & Allison, J. Islet inflammation and hyperplasia induced by the pancreatic islet-specific overexpression of interleukin-6 in transgenic mice. Am J Pathol 145, 157–166 (1994).
Dickerson, R. N. et al. Increased hypoglycemia associated with renal failure during continuous intravenous insulin infusion and specialized nutritional support. Nutrition 27, 766–772, https://doi.org/10.1016/j.nut.2010.08.009 (2011).
Sivajothi, S., Rayulu, V. C. & Sudhakara Reddy, B. Haematological and biochemical changes in experimental Trypanosoma evansi infection in rabbits. J Parasit Dis 39, 216–220, https://doi.org/10.1007/s12639-013-0321-6 (2015).
Nagajyothi, F. et al. Alterations in glucose homeostasis in a murine model of Chagas disease. Am J Pathol 182, 886–894, https://doi.org/10.1016/j.ajpath.2012.11.027 (2013).
Schmidt, J. et al. A better model of acute pancreatitis for evaluating therapy. Ann Surg 215, 44–56 (1992).
Gulcubuk, A. et al. Pathologic alterations detected in acute pancreatitis induced by sodium taurocholate in rats and therapeutic effects of curcumin, ciprofloxacin and metronidazole combination. Pancreatology 5, 345–353, https://doi.org/10.1159/000086534 (2005).
Viriyavejakul, P., Khachonsaksumet, V. & Punsawad, C. Liver changes in severe Plasmodium falciparum malaria: histopathology, apoptosis and nuclear factor kappa B expression. Malar J 13, 106, https://doi.org/10.1186/1475-2875-13-106 (2014).
Acknowledgements
This work was supported by Research Grant from the Faculty of Tropical Medicine, Mahidol University, Fiscal year 2015 (Grant No.: 0303/2558). SG is the grant recipient. We thank all staff at the Department of Tropical Pathology, Faculty of Tropical Medicine, Mahidol University, Thailand for their support throughout this study.
Author information
Authors and Affiliations
Contributions
S.G., C.P. and P.V. performed histopathology and immunohistochemistry work, analysed the data, and drafted the manuscript. S.A.W. and P.V. initiated the research idea, designed the experiments and revised the final manuscript. All authors have approved the final version of this manuscript.
Corresponding author
Ethics declarations
Competing Interests
The authors declare no competing interests.
Additional information
Publisher's note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Glaharn, S., Punsawad, C., Ward, S.A. et al. Exploring pancreatic pathology in Plasmodium falciparum malaria patients. Sci Rep 8, 10456 (2018). https://doi.org/10.1038/s41598-018-28797-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-018-28797-w
This article is cited by
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.