Abstract
Deiodinase 2 (DIO2) plays an important role in thyroid hormone metabolism and its regulation. However, molecular mechanism that regulates DIO2 activity remains unclear; only mutaions in selenocysteine insertion sequence binding protein 2 and selenocysteine tranfer RNA (tRNA[Ser]Sec) are reported to result in decreased DIO2 activity. Two patients with clinical evidence of abnormal thyroid hormone metabolism were identified and found to have TSHR mutations as well as DIO2 T92A single nucleotide polymorphism (SNP). Primary-cultured fibroblasts from one patient present a high level of basal DIO2 enzymatic activity, possibly due to compensation by augmented DIO2 expression. However, this high enzymatic active state yet fails to respond to accelerating TSH. Consequently, TSHR mutations along with DIO2 T92A SNP (“double hit”) may lead to a significant reduction in DIO2 activity stimulated by TSH, and thereby may have clinical relevance in a select population of hypothyroidism patients who might benefit from a T3/T4 combination therapy.
Similar content being viewed by others
Introduction
Thyroid hormone metabolism is tightly regulated by the hypothalamic-pituitary-thyroid (HPT) axis through its positive and negative feedback mechanisms. Meanwhile, thyroid hormone regulation at the cellular level remains largely unknown except for several important deiodinases (DIOs). Among them, type 2 iodothyronine deiodinase (DIO2) converts inactive (thyroxine, T4) to “active” thyroid hormone (3,5,3′-triiodothyronine, T3) and plays a significant role as a determinant of the final concentration of T3.
Apart from thyroid-stimulating hormone (thyrotropin, TSH) suppression for the prevention of recurrent thyroid cancer, TSH also has been used as a reference for optimizing levothyroxine (L-T4) dosages for hypothyroidism. L-T4 monotherapy has remained the standard of treatment with the belief that peripheral conversion of L-T4 into T3 is intact1,2. However, questions about the efficacy of L-T4 monotherapy still remain since 10% to 15% of patients complain of residual symptoms of hypothyroidism, including neurocognitive dysfunction, poor well-being and physical deterioration. Although there has been inconsistent efficacy across trials with the clinical significance of relatively low T3 in humans not well established, several animal models indicate that maintaining normal T3 levels is a biological priority, and that the elevation in serum T3 through the administration of both L-T4 and liothyronine (L-T3) may have benefit in some patients3,4,5. Recent studies suggest that deiodinase activity may vary from its encoding gene and highlight the possible role for individualized medicine based on DIO single nucleotide polymorphisms (SNPs)6,7. Molecular mechanisms on regulating DIO activities enlighten this approach more precisely, not only for the selection of the patients who can benefit to the combination of L-T4 and L-T3, but also for the therapeutic application of thyroid hormones organ- or cell-specifically.
This study first describes patients with a novel form of abnormal thyroid hormone metabolism characterized by substantially decreased DIO2 activity. Mutational analysis reveals that these patients have the DIO2 T92A SNP and loss-of-function mutations of the TSHR gene. Herein, the causal relationship between this combination of genetic alterations and decreased DIO2 activity is described.
Materials and Methods
Measurement of hormones in serum and clinical studies
Serum TSH, free T4, and T3, thyroperoxidase (TPO) antibody, thyroglobulin (Tg) antibody and TSH-receptor antibody levels were measured by immunochemiluminescence assays (Cobas, Roche Diagnostics GmbH, Mannheim, Germany). Serum selenium was measured by inductively coupled plasma -mass spectrometry (NexION®350D, PerkinElmer Inc., MA, USA). TRH stimulation test was performed as follows: Two ampules (400 μg) of relefact TRH (protirelin®, Aventis Pharma Limited, Germany) were administered intravenously at 8:00 AM after overnight fasting. Serum TSH levels were measured before injection of relefact TRH and after 30, 60, 90, 120, 150, and 180 minutes. Informed consent was obtained from participants after study was approved by the Institutional Review Board of Gachon University Gil Medical Center, Incheon, South Korea (GBIRB2013-278) and all research was performed in accordance with relevant guidelines and regulations.
Molecular genetic studies
Genomic DNA was extracted by standard methods from EDTA blood, and whole exome sequencing was performed. Briefly, a pre-enrichment DNA library was constructed according to the Illumina TrueSeq DNA sample preparation guide (Illumina, Inc., San Diego, CA, USA). Exome enrichment was peformed using Illumina TrueSeq Exome Enrichment probes and streptavidin beads. The enriched exome library was loaded onto flow cells of an Illumina cBot for cluster generation. The flow cells with clusters of the enriched exome libraries were transferred to an Illumina HiSeq. 2000. High-throughput sequencing was then performed for each captured library to ensure that each sample met the desired average sequencing depth of 40-fold. TSHR mutations and DIO2 SNP were confirmed by Sanger sequencing. Genomic DNA was amplified using polymerase chain reaction (PCR) with primers for each exon of the TSHR gene8 and exon 2 of the DIO2 gene9. The PCR product was sequenced with the forward and reverse primers used for the PCR amplifications using an ABI 3500xL DNA Analyzer (Applied Biosystems, Foster City, CA, USA).
Cell culture
Fibroblasts were obtained by skin biopsy from patient A and normal controls, and then genotyped: (1) Wild type (WT) (TSHR WT + DIO2 WT), (2) Hetero (TSHR WT + heterozygous DIO2 T92A), (3) Homo (TSHR WT + homozygous DIO2 T92A), and (4) Patient (heterozygous TSHR R450H + homozygous DIO2 T92A). Primary tissue culture was performed by explant technique. Briefly, dissected tissues were finely chopped and rinsed with PBS. The tissues were seeded onto the surface of a tissue culture flask in 1 ml of Dulbecco’s Modified Eagle’s medium (DMEM) medium supplemented with 40% fetal bovine medium volume made up to 5 ml, and then changed weekly until a substantial outgrowth of cells was observed. Cells were then incubated in DMEM medium supplemented with 15% FBS, penicillin (100 U/mL), and streptomycin (100 μg/mL). All cultured cells were incubated in a humidified atmosphere at 37 °C and at 5% CO2. The study used cells with 5–10 passages for all experiments. The C2C12 myoblast progenitor and IMR90 human fibroblast cells were grown in DMEM supplemented with 10% heat-inactivated fetal bovine (FBS), penicillin (100 U/mL), and streptomycin (100 μg/mL). The TαT1 cells were kindly provided by Prof. B. Haugen (University of Colorado), and cultured as described previously10. The TαT1 cells required plates coated with Matrigel (Decton Dickison BD) to facilitate adhesion. Briefly, Matrigel was diluted 1:30 in DMEM and allowed to air dry in hood before plating cells. The TαT1 cells were seeded on Matrigel-coated plates and grown in DMEM containing 10% FBS, penicillin (100 U/mL), and streptomycin (100 μg/mL). All cultured cells were incubated in a humidified atmosphere at 37 °C and at 5% CO2.
TSH and cAMP Treatment and quantitative RT-PCR
Primary cultured cells (2 × 104 cells/well) were seeded into a 6-well culture tray. After 24 hour incubation, the cells were serum-starved for 18 hours. For TSH treatment, different TSH concentrations (0, 1, and 10 IU) were added for either 3 or 6 hours. For cAMP, cells were treated with 1 mM db-cAMP (Sigma) for 16 hours. Total RNA was extracted from cultured cells using TRIzol reagent (Invitrogen, Carlsbad, USA), following the manufacturer’s instructions (Beckman Coulter, Brea, USA). Extracted RNA was subsequently reverse transcribed using a RevertAid™ H Minus First Strand cDNA Synthesis Kit (Fermentas Inc., Hanover, USA) with oligo(dT)15–18 as a random primer. All real time RT-PCR measurements were performed using the ABI Prism 7000 Sequence Detection System (Applied Biosystems, Foster City, USA). All PCR amplifications (40 cycles) were performed in a total volume of 25 μl containing 150 ng of cDNA using an SYBR Green I qPCR kit (TaKaRa, Shiga, Japan), according to the manufacturer’s recommendations. The specific primers for human DIO2 were as follows: 5′-TCCAGTGTGGTGCATGTCTC-3′ and 5′-CTGGCTCGTGAAAGGAGGTC-3′. By normalizing to Gapdh, the relative quantification of gene expression was performed using the comparative threshold (Ct) method, as described by the manufacturer (Applied Biosystems). The values were expressed as the fold change over the control. Relative gene expression was displayed as 2−ΔCt (ΔCt = Cttarget gene − CtGapdh). The fold change was calculated as 2−ΔΔCt (ΔΔCt = ΔCtcontrol − Cttreatment).
Western blotting
The TαT1 and IMR90 cells (2 × 104 cells/well) were seeded into a 6-well culture tray. After 24 hour incubation, the cells were serum-starved for 18 hours. Cells were treated with TSH (0, 1, and 10 IU) for 8 hours or T4 (0, 20, and 100 pM) for 16 hours. Samples were lysed at 4 °C in RIPA buffer (150 mM NaCl, 1% Nonidet P-40, 0.5% sodium deoxycholate, 0.1% SDS, and 50 mM Tris buffer, pH 8.0). The lysate were centrifuged at 13000 rpm for 20 min at 4 °C. Supernatant was collected and re-suspended in SDS-PAGE buffer and immediately boiled at 100 °C for 5 minutes. Proteins were analyzed by SDS-PAGE on 12% polyacrylamide gels and electroblotted onto PVDF membrane (polyvinylidine difluoride membrane, Millipore). The membrane blots were blocked with 5% BSA for 1 hour, and then incubated with primary antibodies at 4 °C overnight: anti-DIO2 antibody at a 1:2000 dilution (Abcam), anti-TSHR antibody at a 1:1500 dilution (Abbiotec), and amti-Actin antibody at a 1:2000 dilution (Santa Cruz). After washing with PBS/0.1% Tween-20, the membrane was incubated with secondary antibodies (anti-rabbit or anti-goat antibodies, Santa Cruz) for 1 hour at room temperature and then visualized by the WEST-ZOL plus ECL Western blotting detection system (iNtRON BioTechnology).
cAMP assay
Primary cultured cells (2 × 104 cells/well) were incubated in 6-well plates for 24 hours and serum-starved for 18 hours. Cells were treated with 0 and 1 IU of TSH for 30 minutes. For the cAMP assay, cells were treated with 0.1 N hydrochloric acid to stop endogenous phosphodiesterase activity. After cell lysis, samples were centrifuged at 600 g at room temperature and supernatant was collected. cAMP was measured using the cAMP direct immunoassay kit (Millpore) following the manufacturer’s instructions. Each experiment was repeated three times.
Immunostaining of TSHR and DIO2
Pituitary human samples were kindly provided by Prof. S. H. Park (Seoul National University). Tissues were fixed with cold 4% paraformaldehyde in 0.1 M phosphate buffer at pH 7.4 and embedded into paraffin wax. The 4–5 micron of paraffin sections on Fisherbrand Superfrost Plus (Cat #: 12-550-15) slides were loaded into glass slide holders for deparaffinization and rehydration as follows: three times in xylene for 5 minutes, two times in 100% ethanol for 10 minutes, two times in 95% ethanol for 10 minutes, two times in 70% ethanol for 10 minutes and twice in H2O for 5 minutes. The rack is transferred into 200 ml of pre-warmed (94~96 °C) target retrieval solution in a glass container in the water bath at 95 °C for 30 minutes and the slides were cooled down on the bench top for 30 minutes. The slides were permeabilized with 0.3% Triton X-100 in PBS for 30 minutes and incubated with blocking buffer containing 10% FBS in PBS for 1 hour. Samples were incubated with primary antibodies; DIO2 rabbit antibody at a 1:1000 dilution (Abcam) and TSHR rabbit antibody at a 1:250 dilution (Abbiotec) in blocking buffer for 2 hours at room temperature. After washing with PBS, secondary antibody FITC goat anti-rabbit IgG antibody at 1:500 dilution (Invitrogen) was incubated for 1 hour at room temperature. Samples were mounted on VECTASHIELD mounting with DAPI (Invitrogen).
Measurement of Type 2 Iodothyronine Deiodinase Activity
Type 2 iodothyronine deiodinase activity was measured as previously described11,12, with minor modifications. Briefly, cells were scraped off, and transferred into 1.5 ml ice-cold buffer [PBS containing 20 mm dithiothreitol (DTT)]. After centrifugation at 3000 rpm for 10 min at 4 oC, the supernatant was discarded. Pellets were sonicated in 120 μl assay buffer (100 mM potassium phosphate, pH 7.0, containing 1 mM EDTA and 20 mM DTT)/tube and were incubated in a total volume of 50 μl with 2 nM of [125I]T4, which was purified using LH-20 (Pharmacia Biotech, Uppsala, Sweden) column chromatography on the day of experiment, in the presence of 1 mM PTU for 1 hr at 37 oC. The reaction was terminated by the addition of 100 μl 2% BSA and 800 μl 10% trichloroacetic acid. After centrifugation at 1,500 g for 10 min at 4 oC, the supernatant was applied to a small column packed with AG 50W-X2 resin (bed volume 1 ml; Bio-Rad Laboratories, Hercules, CA) and then eluted with 2 ml of 10% glacial acetic acid. Separated 125I was counted with a γ-counter. Nonenzymatic deiodination was corrected by subtracting I− released in control tubes without sonicated samples. The protein concentration was determined by Bradford’s method with BSA as a standard13. The deiodinating activity was calculated as fmol I− released/mg protein/hour, after multiplication by a factor of 2 to correct for random labeling at the equivalent 3′ and 5′ positions.
Statistical analysis
All the experiments were repeated at least three times and the results were presented as the means ± standard deviation (SD), as indicated. Statistical analysis was done using PASW Statistics, version 17.0 (SPSS Inc., Chicago, IL, USA). Statistically significant differences between groups were tested using a Student’s t-test. P values < 0.05 were considered significant.
Results
Clinical characteristics of patients with abnormal thyroid hormone metabolism characterized by substantially decreased DIO2 activity
A 68-year-old Korean man (I-1 in Fig. 1a; patient A) was referred to the tertiary hospital with abnormal thyroid function tests from a local clinic. The patient had symptoms of anorexia and weight gain for three months. Initial serum TSH was 85.50 mIU/L (0.27–4.20) and free T4 (fT4) was 0.16 ng/dL (0.93–1.70) at local clinic. The patient had hypothyroidism and began to take L-T4 100 μg per day for three months. Although his symptoms related to hypothyroidism improved, his serum TSH level was not suppressed (Fig. 1b). At the hospital, thyroid function and thyroid autoantibody tests were as follows: TSH 98.74 mIU/L, fT4 1.10 ng/dL, T3 64.93 ng/dL (80.00–200.00), Tg antibody 114.8 IU/mL (0.0–115.0), TPO antibody 16.34 IU/mL (0.00–34.00), and TSH-receptor antibody 3.0 IU/L (0.0–1.5). Initially, laboratory error of the immunoassay for serum TSH level was suspected due to heterophile antibody interference. Linearity of serum TSH level was measured following serial dilution, along with serum TSH concentration before and after the addition of a heterophile blocking antibody, and tested by another kit (IMMULITE 2000, Siemens). These three tests for heterophile interference phenomenon were all negative. L-T3 30 μg was administered three times a day instead of L-T4 100 μg per day. Serum TSH level was dramatically decreased to 5.53mIU/L. Thereafter, L-T4 combined with L-T3 was prescribed, and the patient’s thyroid function was maintained normal range up to five years. The patient’s eldest son (II-1) had subclinical hypothyroidism, and his thyroid function was as follows: TSH 4.97 mIU/L, fT4 1.41 ng/dL, T3 103.00 ng/dL, Tg antibody 16.3 IU/mL, TPO antibody 16.4 IU/mL, and TSH-receptor antibody 0.8 IU/L. The daughter-in-law (II-2) had normal thyroid function but positive for autoantibodies for thyroid disease as follows: TSH 2.78 mIU/L, fT4 0.99 ng/dL, T3 112.50 ng/dL, Tg antibody 55.7 IU/mL, TPO antibody 294.2 IU/mL, and TSH-receptor antibody 2.5 IU/L. The patient’s daughter (II-4) and younger son (II-5) both had subclinical hypothyroidism. The patient’s grandson (III-1) had congenital hypothyroidism and was taking L-T4, and his TSH was appropriately suppressed with L-T4, indicating intact DIO2 activity. Neither of the family members, but patient A agreed to provide fibroblast samples.
Characteristics of Patient A and his family. (a) Pedigree of the Patient A in this study. The letter ‘P’ indicates a proband (Patient A, I-1) of this family. The patients are represented by DIO2 activity and thyroid disease state. The results of DIO2 and TSHR genotypes of the patients and their thyroid functions in this family are also presented. (b) Serial thyroid function tests and thyroid hormone dosages of the proband (I-1) are presented. Note that TSH is suppressed only after L-T3 is administered and thyroid function is maintained normal range with combination of L-T4 and L-T3.
A 75 year-old Korean woman (patient B) suffered from a thyroid goiter (up to 10 cm in diameter) since her early twenties. Her thyroid function tests revealed extremely high TSH levels, inappropriately high fT4 and relatively low T3 levels; TSH 82 mIU/L, fT4 > 7.70 ng/dL, T3 64 ng/dL without thyrotoxic symptoms. Her goiter decreased in size dramatically when given L-T3 30 μg two times a day, followed by decrease in TSH level to 8.21 mIU/L and increase of T3 level to 94 ng/dL without differences in fT4 level (Table 1). TRH stimulation test revealed that it was less likely due to either RTH or TSH secreting pituitary adenoma for inappropriately increased TSH (Table 2). The patient was strongly suspicious for decreased DIO2 activity but denied the provision of skin samples for evaluation of its activity.
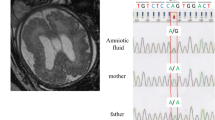
Genetic analysis of patients A and B identify Concurrent TSHR mutations and DIO2 T92A polymorphism
Nucleotide sequencing of patient A (I-1) revealed to have a homozygous SNP in the DIO2 gene (c.274 A > G, DIO2 T92A), which had previously been identified in a certain portion of population as significant SNP14,15 and a heterozygous mutation in TSHR gene (c.1349 G > A, R450H)8,16,17,18 (data not shown). Interestingly, patients B also had a homozygous DIO2 T92A together with heterozygous TSHR F525S (data not shown). In the family of patient A, I-2 had no genetic alterations in DIO2 and TSHR genes, and II-1, II-2, II-4, and II-5 had heterozygous DIO2 T92A and TSHR R450H. III-1 had heterozygous DIO2 T92A and homozygous TSHR R450H (Fig. 1a). Whole exome sequencing of patient B does not identify any other genetic alterations that could be disease-causing (data not shown).
Expressions of TSHR and DIO2 are observed in pituitary gland and fibroblast
The role of DIO2 in feedback regulation of hypothalamic-pituitary-thyroid (HPT) axis mediated by TSH is well known19. In the same context, DIO2 and TSHR are known to be expressed in human pituitary gland and20,21,22 mouse thyrotrope TαT1 cells23. Furthermore, DIO2 and TSHR have been reported to be expressed in several types of cells: mouse myoblast C2C12 cells24, human osteoblasts12, and human fibroblasts25. In this study we found that TSHR exists in human pituitary tissues (Fig. 2a) and also confirmed that both DIO2 and TSHR expressed in C2C12 and TαT1 cells and primary-cultured skin fibroblasts (Fig. 2b).
Expression of TSHR and DIO2 in pituitary gland and fibroblast (a) (upper panel) Immunocytochemistry results of TSHR in human pituitary tissues. The fixed pituitary tissue is stained with anti-TSHR antibody (green) and mount on VECTASHIELD mounting with DAPI (blue). Scale Bar, 100 μm. (lower panel) Close-up regions indicate localization of TSHR protein on human pituitary. Scale Bar, 50 μm. (b) Western blot analysis of DIO2 and TSHR in C2C12 and TαT1 cell lines (left panel) and primary-cultured skin fibroblast cells (right panel). Cells are lysed and analyzed by SDS-PAGE on 12% polyacrylamide gels and electroblotted onto PVDF membrane. Immunoblotting is conducted with the antibodies: anti-DIO2 rabbit antibody at a 1:2000 dilution, anti-TSHR rabbit antibody at a 1:1500 dilution and anti-Actin goat antibody at a 1:2000 dilution. Multiple exposures are shown in the Supplementary Figure 1.
TSHR mutation and DIO2 variation decrease DIO2 activiy
All patients in this study have heterozygous loss-of-function TSHR mutations (R450H and F525S) in addition to homozygous DIO2 T92A SNP. Biallelic TSHR R450H and F525S mutations have been reported to be a cause of congenital hypothyroidism in a few cases8,16,17,26. Whether TSHR R450H mutations may influence DIO2 activity in patients with biallelic DIO2 T92A SNP were investigated since his fibroblasts were available and primary-cultured human skin fibroblasts previously used for analysis of thyroid hormone metabolism25.
Primary-cultured fibroblasts were altered with TSHR and DIO2 expression levels in response to TSH stimulation, as reported in TαT1 cells27. TSH treatment revealed that TSHR was decreased but DIO2 was increased dose-dependently in fibroblasts and TαT1 cells (Fig. 3a). In contrary, T4 treatment revealed that TSHR and DIO2 were decreased dose-dependently in fibroblasts and TαT1 cells (Fig. 3b). Notably, basal level of DIO2 activity was significantly higher in the patient’s fibroblast cells than all other tested fibroblast cells (Fig. 4a,b). When TSH was treated, DIO2 mRNA expressions in fibroblast cells of WT, Hetero, and Homo were all increased in time- and dose-dependent manner, but no increase was detected in the patient’s fibroblast cells (Fig. 4c). Furthermore, DIO2 activity also did not increase in the patient’s cells (Fig. 4d).
Western blot analysis of TSHR and DIO2 in TαT1 cell line and primary-cultured skin fibroblast cells. Cells are incubated in 6-well plates for 24 h and serum-starved for 18 h, and then incubated with indicated concentrations of either TSH (1 and 10 IU) or L-T4 (20 and 100 pM) for 8 h. Cells are lysed and analyzed by SDS-PAGE on 12% polyacrylamide gels and electroblotted onto PVDF membrane. Immunoblotting is conducted with the antibodies: anti-DIO2 rabbit antibody at a 1:2000 dilution, anti-TSHR rabbit antibody at a 1:1500 dilution and anti-Actin goat antibody at a 1:2000 dilution. (a) TSH treatment reveals that TSHR is decreased but DIO2 is significantly increased in 10 IU-treated TαT1 cells and fibroblast. Quantification of band intensity was performed using ImageJ software. *p < 0.05 vs. 0. (b) L-T4 treatment reveals that TSHR and DIO2 are decreased dose-dependently in TαT1 cells and fibroblast. Quantification of band intensity was performed using ImageJ software. *p < 0.05 vs. 0. Multiple exposures are shown in the Supplementary Figure 2.
DIO2 expression and activity. (a,b) Basal levels of DIO2 expression and enzymatic activity in primary-cultured skin fibroblast cells. Cells are from normal controls with wild type DIO2 genotype (WT), and heterozygous (Hetero) or homozygous (Homo) DIO2 T92A variants, and patient with homozygous DIO2 T92A variant and heterozygous TSHR R450H mutation (Patient). Notably, basal levels of DIO2 expression and activity are significantly higher in the patient’s fibroblast cells than all other tested fibroblast cells. *p < 0.05 vs. WT. (c) Relative DIO2 mRNA expression levels in primary-cultured skin fibroblast cells. The TSH-non-treated cells are used as negative control (0). Total RNA is extracted from the cells and DIO2 mRNA expression level is analyzed by quantitative real-time RT-PCR. DIO2 mRNA expressions in WT, Hetero, and Homo are all increased, but no increase is detected in the patient. *p < 0.05 vs. negative control in each tested fibroblast. #p < 0.05 vs. WT in each TSH-treated group. (d) Relative DIO2 enzymatic activities in primary-cultured skin fibroblast cells. DIO2 enzymatic activities in WT, Hetero, and Homo are all increased, but no increase is detected in the patient. *p < 0.05 vs. negative control in each tested fibroblast. #p < 0.05 vs. WT in each TSH-treated group.
Since DIO2 gene contains a cyclic-AMP (cAMP)-response element28,29 in promoter region, cAMP treatment can induce DIO2 expression even in the absence of TSH. To investigate whether no response of DIO2 mRNA expression and DIO2 activation with TSH stimulation in patient is caused by TSHR mutation, DIO2 expression changes after treatment of cAMP in the fibroblasts were tested. DIO2 mRNA expression in patient was significantly increased by cAMP treatment (Fig. 5a). TSH augments cellular cAMP levels28,29. Next, the influence of TSHR mutation on cAMP production by TSH was tested. When 1 IU of TSH was treated, cAMP was increased in all fibroblasts, but significantly less increased in the patient’s fibroblasts compared to WT, Hetero and Homo (Fig. 5b).
Relative DIO2 mRNA expression levels in cAMP-treated cells and cAMP assay results in TSH-treated in primary-cultured skin fibroblast cells. (a) Cells are treated with 1 mM db-cAMP for 16 h (+cAMP) and total RNA is extracted from the cells and DIO2 mRNA expression level is analyzed by quantitative real-time RT-PCR. The cAMP-non-treated cells are used as negative control (−cAMP). DIO2 mRNA expressions in WT, Hetero, Homo and patient are significantly increased by cAMP treatment. *p < 0.05 vs. negative control in each tested fibroblast. (b) Cells were treated with 1 IU of TSH for 30 min and then are treated with 0.1 N hydrochloric acid to stop endogenous phosphodiesterase activity. After cell lysis, intracellular cAMP concentration is measured using cAMP direct immunoassay kit. The TSH-non-treated cells are used as negative control. cAMP is increased in all groups, but significantly less increased in the patient. *p < 0.05 vs. negative control in each tested fibroblast. #p < 0.05 vs. WT.
Discussion
Deiodinases (DIOs), one of the selenoproteins, are essential for life; however, the underlying molecular mechanisms of their regulation remain to be elucidated. For DIO2, high concentration of T414,27,30 and some SNP of DIO2 gene, especially DIO2 T92A, have been reported to decrease its enzymatic activity14. Although generally believed that DIO2 T92A is associated with both an impaired baseline psychological well-being on L-T4 and an enhanced response to combination L-T4/L-T3 therapy among hypothyroidism patients15, there is still controversy to this assertion because DIO2 T92A has relatively high prevalence among general populations and all the subjects having this SNP do not show typical characteristics in thyroid function tests. Only a few genetic alterations, which are related to abnormal thyroid hormone metabolism, involve the selenocysteine insertion sequence binding protein 2 (SECISBP2 also known as SBP2) and selenocysteine transfer RNA (tRNA[Ser]Sec) mutations25,31. There have been a few reports on decreased DIO2 activity arisen from SBP2 mutation worldwide32,33,34,35.
Since Ishii et al. first reported that TSH may induce DIO2 in thyroid gland in 198336, regulation of DIO2 by TSH has been demonstrated in thyroid tissue, brown adipocyte and osteoblasts11,12,29. Furthermore, recent studies also show that increased TSH is associated with increased T3 but not T4 as well as T3/T4 in the pediatric age group, suggesting the role of TSH to regulate conversion of T4 to T3 through DIO237. Additionally, the authors have shown that this relationship was also seen in the young adult group. Within the euthyroid range, increasing TSH levels are associated with increasing T3/T4 ratio, indicating TSH enhances preferentially T3 production and proportionally T4 reduction, which results from the DIO2 activity enhanced by TSH38.
A previous study reported that cAMP produced by interaction of TSH and TSHR affected the cAMP response element located upstream of promoter region of DIO228. The authors’ results also indicate that lack of cAMP production caused by loss-of-function mutation of TSHR and DIO2 T92A SNP cooperatively causes decreased DIO2 enzymatic activity, which is confirmed by experiments of the patient’s dermal fibroblasts. Surprisingly, the patient’s primary-cultured fibroblasts showed exaggerated basal level of DIO2 mRNA expression and enzyme activity, but these fibroblasts had a blunted response to TSH when accerelating doses of TSH was treated, indicating compensatory high enzymatic active state yet fails to respond to TSH.
The TSHR R450H mutation, known as a loss-of-function mutation, has uniquely been found only in Korean, Japanese, Taiwanese, and Chinese populations, and were derived from a common ancestral allele8,16,17,26. Patients II-1, II-4, and II-5 in family A who have heterozygous R450H had mild subclinical hypothyroidism and patient III-1 who had a homozygous TSHR R450H mutation had severe congenital hypothyroidism. The prevalence of TSHR R450H mutation is reported as 0.47% in the general Japanease population18 and the prevalence of biallelic TSHR mutations was estimated to 4.3% in Japanese patients with moderate to severe congenital hypothyroidism8. Patient A (I-1) having heterozygous TSHR R450H and homozygous DIO2 T92A showed evident decreased DIO2 activity, but III-1 having homozygous TSHR R450H and heterozygous DIO2 T92A did not show decreased DIO2 activity. Considering age-related deterioration of DIO2 activity which was also referred by recent report showing inconsistency of correlation between TSH and T3/T4 ratio over 40 s and over, DIO2 activity is likely very sensitive to the aging process39. In this respect, III-1 needs to be in close monitoring with aging. Other patients (II-4, II5) having heterozygous TSHR R450H and heterozygous DIO2 T92A also need to be evaluated for their DIO2 activity and monitored thereafter.
Another TSHR F525S mutation found in patient B was also reported as a loss-of-function mutation16. Decreased DIO2 activity in this patient can be explained similarly to patient A. Normalization of TSH in eight congenital hypothyroidism patients by adding a small dose of L-T3 into L-T4 further provides evidence that supports the notion described in this study40. More genomic data as well as relevant clinical outcome are needed to confirm this relationship. Lack of direct measured DIO2 activity from patient B and other family members of patient A is a limitation of this study, but patient B is certainly believed to have the decreased DIO2 activity based on their clinical data and presentation.
In conclusion, TSH stimulates DIO2 activity, and TSHR mutations and homozygous DIO2 T92A SNP (“double hit”) result in a novel form of abnormal thyroid hormone metabolism. This study may greatly contribute to the selection of appropriate patients with hypothyroidism who can benefit from L-T3/L-T4 combination treatment, and to provide them with optimized medical care.
References
Jonklaas, J. et al. Guidelines for the treatment of hypothyroidism: prepared by the american thyroid association task force on thyroid hormone replacement. Thyroid: official journal of the American Thyroid Association 24, 1670–1751, https://doi.org/10.1089/thy.2014.0028 (2014).
Wiersinga, W. M., Duntas, L., Fadeyev, V., Nygaard, B. & Vanderpump, M. P. ETA Guidelines: The Use of L-T4 + L-T3 in the Treatment of Hypothyroidism. European thyroid journal 1, 55–71, https://doi.org/10.1159/000339444 (2012).
Michaelsson, L. F. et al. Treating Hypothyroidism with Thyroxine/Triiodothyronine Combination Therapy in Denmark: Following Guidelines or Following Trends? European thyroid journal 4, 174–180, https://doi.org/10.1159/000437262 (2015).
Gullo, D. et al. Levothyroxine monotherapy cannot guarantee euthyroidism in all athyreotic patients. PloS one 6, e22552, https://doi.org/10.1371/journal.pone.0022552 (2011).
Nygaard, B., Jensen, E. W., Kvetny, J., Jarlov, A. & Faber, J. Effect of combination therapy with thyroxine (T4) and 3,5,3′-triiodothyronine versus T4 monotherapy in patients with hypothyroidism, a double-blind, randomised cross-over study. European journal of endocrinology / European Federation of Endocrine Societies 161, 895–902, https://doi.org/10.1530/EJE-09-0542 (2009).
Wartofsky, L. Combination L-T3 and L-T4 therapy for hypothyroidism. Current opinion in endocrinology, diabetes, and obesity 20, 460–466, https://doi.org/10.1097/01.med.0000432611.03732.49 (2013).
Wiersinga, W. M. Paradigm shifts in thyroid hormone replacement therapies for hypothyroidism. Nature reviews. Endocrinology 10, 164–174, https://doi.org/10.1038/nrendo.2013.258 (2014).
Narumi, S. et al. TSHR mutations as a cause of congenital hypothyroidism in Japan: a population-based genetic epidemiology study. The Journal of clinical endocrinology and metabolism 94, 1317–1323, https://doi.org/10.1210/jc.2008-1767 (2009).
Leiria, L. B. et al. The rs225017 polymorphism in the 3′ UTR of the human DIO2 gene is associated with increased insulin resistance. PloS one 9, e103960, https://doi.org/10.1371/journal.pone.0103960 (2014).
Yusta, B., Alarid, E., Gordon, D., Ridgway, E. C. & Mellon, P. L. The thyrotropin beta-subunit gene is repressed by thyroid hormone in a novel thyrotrope cell line, mouse T alphaT1 cells. Endocrinology 139, 4476–4482, https://doi.org/10.1210/endo.139.11.6283 (1998).
Murakami, M. et al. Expression and regulation of type II iodothyronine deiodinase in human thyroid gland. Endocrinology 142, 2961–2967, https://doi.org/10.1210/endo.142.7.8280 (2001).
Morimura, T. et al. Expression of type 2 iodothyronine deiodinase in human osteoblast is stimulated by thyrotropin. Endocrinology 146, 2077–2084, https://doi.org/10.1210/en.2004-1432 (2005).
Bradford, M. M. A rapid and sensitive method for the quantitation of microgram quantities of protein utilizing the principle of protein-dye binding. Analytical biochemistry 72, 248–254 (1976).
Canani, L. H. et al. The type 2 deiodinase A/G (Thr92Ala) polymorphism is associated with decreased enzyme velocity and increased insulin resistance in patients with type 2 diabetes mellitus. The Journal of clinical endocrinology and metabolism 90, 3472–3478, https://doi.org/10.1210/jc.2004-1977 (2005).
Panicker, V. et al. Common variation in the DIO2 gene predicts baseline psychological well-being and response to combination thyroxine plus triiodothyronine therapy in hypothyroid patients. The Journal of clinical endocrinology and metabolism 94, 1623–1629, https://doi.org/10.1210/jc.2008-1301 (2009).
Lee, S. T. et al. Molecular screening of the TSH receptor (TSHR) and thyroid peroxidase (TPO) genes in Korean patients with nonsyndromic congenital hypothyroidism. Clinical endocrinology 75, 715–721, https://doi.org/10.1111/j.1365-2265.2011.04156.x (2011).
Chang, W. C. et al. R450H TSH receptor mutation in congenital hypothyroidism in Taiwanese children. Clinica chimica acta; international journal of clinical chemistry 413, 1004–1007, https://doi.org/10.1016/j.cca.2012.02.027 (2012).
Tsunekawa et al. Frequency and clinical implication of the R450H mutation in the thyrotropin receptor gene in the Japanese population detected by Smart AmplificationProcess 2. BioMed research international 2014, 964635, https://doi.org/10.1155/2014/964635 (2014).
Fonseca, T. L. et al. Coordination of hypothalamic and pituitary T3 production regulates TSH expression. The Journal of clinical investigation 123, 1492–1500, https://doi.org/10.1172/JCI61231 (2013).
Schneider, M. J. et al. Targeted disruption of the type 2 selenodeiodinase gene (DIO2) results in a phenotype of pituitary resistance to T4. Molecular endocrinology 15, 2137–2148, https://doi.org/10.1210/mend.15.12.0740 (2001).
Prummel, M. et al. Expression of the thyroid-stimulating hormone receptor in the folliculo-stellate cells of the human anterior pituitary. The Journal of clinical endocrinology and metabolism 85, 4347–4353, https://doi.org/10.1210/jcem.85.11.6991 (2000).
Theodoropoulou, M. et al. Thyrotrophin receptor protein expression in normal and adenomatous human pituitary. The Journal of endocrinology 167, 7–13 (2000).
Wege, N. et al. PPARalpha modulates the TSH beta-subunit mRNA expression in thyrotrope TalphaT1 cells and in a mouse model. Molecular nutrition & food research 57, 376–389, https://doi.org/10.1002/mnfr.201200409 (2013).
Dentice, M. et al. The FoxO3/type 2 deiodinase pathway is required for normal mouse myogenesis and muscle regeneration. The Journal of clinical investigation 120, 4021–4030, https://doi.org/10.1172/JCI43670 (2010).
Dumitrescu, A. M. et al. Mutations in SECISBP2 result in abnormal thyroid hormone metabolism. Nature genetics 37, 1247–1252, https://doi.org/10.1038/ng1654 (2005).
Nagashima, T. et al. Novel inactivating missense mutations in the thyrotropin receptor gene in Japanese children with resistance to thyrotropin. Thyroid: official journal of the American Thyroid Association 11, 551–559, https://doi.org/10.1089/105072501750302859 (2001).
Christoffolete, M. A. et al. Atypical expression of type 2 iodothyronine deiodinase in thyrotrophs explains the thyroxine-mediated pituitary thyrotropin feedback mechanism. Endocrinology 147, 1735–1743, https://doi.org/10.1210/en.2005-1300 (2006).
Leonard, J. L. Dibutyryl cAMP induction of type II 5′deiodinase activity in rat brain astrocytes in culture. Biochemical and biophysical research communications 151, 1164–1172 (1988).
Murakami, M. et al. Thyrotropin receptors in brown adipose tissue: thyrotropin stimulates type II iodothyronine deiodinase and uncoupling protein-1 in brown adipocytes. Endocrinology 142, 1195–1201, https://doi.org/10.1210/endo.142.3.8012 (2001).
Araki, O. et al. Expression of type 2 iodothyronine deiodinase in corticotropin-secreting mouse pituitary tumor cells is stimulated by glucocorticoid and corticotropin-releasing hormone. Endocrinology 144, 4459–4465, https://doi.org/10.1210/en.2003-0419 (2003).
Schoenmakers, E. et al. Mutation in human selenocysteine transfer RNA selectively disrupts selenoprotein synthesis. The Journal of clinical investigation 126, 992–996, https://doi.org/10.1172/JCI84747 (2016).
Di Cosmo, C. et al. Clinical and molecular characterization of a novel selenocysteine insertion sequence-binding protein 2 (SBP2) gene mutation (R128X). The Journal of clinical endocrinology and metabolism 94, 4003–4009, https://doi.org/10.1210/jc.2009-0686 (2009).
Azevedo, M. F. et al. Selenoprotein-related disease in a young girl caused by nonsense mutations in the SBP2 gene. The Journal of clinical endocrinology and metabolism 95, 4066–4071, https://doi.org/10.1210/jc.2009-2611 (2010).
Hamajima, T., Mushimoto, Y., Kobayashi, H., Saito, Y. & Onigata, K. Novel compound heterozygous mutations in the SBP2 gene: characteristic clinical manifestations and the implications of GH and triiodothyronine in longitudinal bone growth and maturation. European journal of endocrinology / European Federation of Endocrine Societies 166, 757–764, https://doi.org/10.1530/EJE-11-0812 (2012).
Schoenmakers, E. et al. Mutations in the selenocysteine insertion sequence-binding protein 2 gene lead to a multisystem selenoprotein deficiency disorder in humans. The Journal of clinical investigation 120, 4220–4235, https://doi.org/10.1172/JCI43653 (2010).
Ishii, H. et al. Induction of outer and inner ring monodeiodinases in human thyroid gland by thyrotropin. The Journal of clinical endocrinology and metabolism 57, 500–505, https://doi.org/10.1210/jcem-57-3-500 (1983).
Karavani, G., Strich, D., Edri, S. & Gillis, D. Increases in thyrotropin within the near-normal range are associated with increased triiodothyronine but not increased thyroxine in the pediatric age group. The Journal of clinical endocrinology and metabolism 99, E1471–1475, https://doi.org/10.1210/jc.2014-1441 (2014).
Park, S. Y. et al. Free triiodothyronine/free thyroxine ratio rather than thyrotropin is more associated with metabolic parameters in healthy euthyroid adult subjects. Clinical endocrinology, https://doi.org/10.1111/cen.13345 (2017).
Strich, D., Karavani, G., Edri, S. & Gillis, D. TSH enhancement of FT4 to FT3 conversion is age dependent. European journal of endocrinology/European Federation of Endocrine Societies, https://doi.org/10.1530/EJE-16-0007 (2016).
Strich, D., Naugolny, L. & Gillis, D. Persistent hyperthyrotropinemia in congenital hypothyroidism: successful combination treatment with levothyroxine and liothyronine. Journal of pediatric endocrinology & metabolism: JPEM 24, 347–350 (2011).
Acknowledgements
The authors thank all patients and family members for their participation and Professors P. Reed Larsen and Gilbert Daniels for their insightful advice. We also thank Professors B. Haugen, and S.H. Park for provision of TαT1 cells and human brain tissues. Supported by the Basic Science Research Program, National Research Foundation of Korea (NRF-2013R1A1A1A05005629 to SL) and Korea Research-driven Hospitals Grant fostered for Gachon University Gil Medical Center (FRD2014-04-02 to SL).
Author information
Authors and Affiliations
Contributions
J.J., S.Y.P. and S.L. found the patients and performed clinical and genetic studies. E.P. and J.K. performed cellular and molecular experiments. O.A., K.T. and M.M. performed DIO2 enzymatic experiments. Authors analyzed and discussed the data. S.L. and S.-Y.J. were responsible for the overall conceptual composition of the study and wrote the manuscript.
Corresponding authors
Ethics declarations
Competing Interests
The authors declare no competing interests.
Additional information
Publisher's note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Park, E., Jung, J., Araki, O. et al. Concurrent TSHR mutations and DIO2 T92A polymorphism result in abnormal thyroid hormone metabolism. Sci Rep 8, 10090 (2018). https://doi.org/10.1038/s41598-018-28480-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-018-28480-0
This article is cited by
-
Genetics of primary congenital hypothyroidism—a review
Hormones (2021)
-
Importance of Thyroid Hormone level and Genetic Variations in Deiodinases for Patients after Acute Myocardial Infarction: A Longitudinal Observational Study
Scientific Reports (2020)
-
Targeting the right population for T3 + T4 combined therapy: where are we now and where to next?
Endocrine (2020)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.