Abstract
The cancer risk in patients with alopecia areata (AA) or alopecia totalis (AT)/alopecia universalis (AU) remains unknown. In this study, national statistical data were used to study the association between these forms of alopecia and the risk of cancer. We enrolled 668,604 patients who were treated for alopecia from 2007 to 2014, and age- and sex-matched control subjects. AA and AT/AU patients had slightly higher overall cancer risks (hazard ratio (HR), 1.043; 95% confidence interval (CI), 1.022–1.065 and HR, 1.07; 95% CI, 1.013–1.129, respectively) than controls, after adjusting for confounding factors. The risks of oral cavity, esophagus, liver, biliary tract, pancreas, larynx, lung, kidney, breast, cervix, ovary, uterus, testis, nerve, and skin cancers; and lymphoma, multiple myeloma, and leukemia, were not increased in alopecia patients. In AA or AT/AU patients, the only increased risk was that of thyroid cancer. In AA patients alone, the risks of bladder and prostate cancers were increased. Thus, the cancer risks varied by the alopecia subtype. Careful monitoring is needed to explore if the actual risks of thyroid, bladder, and prostate cancers are increased in alopecia patients.
Similar content being viewed by others
Introduction
Alopecia areata (AA) is an inflammatory autoimmune disorder featuring temporary, non-scarring, patchy hair loss associated with genetic and environmental factors and T-cell-mediated immunological reactions. Alopecia totalis (AT) refers to total scalp hair loss, and alopecia universalis (AU) to hair loss over the entire body. AT and AU are poor prognostic forms of alopecia. Typical AA generally has a lifetime prevalence of about 2%1.
AA is associated with comorbidities such as psychiatric illnesses and autoimmune disorders. Associations between AA and autoimmune diseases including vitiligo, thyroid disease, irritable bowel syndrome, psoriasis, systemic lupus erythematosus, rheumatoid arthritis, and diabetes mellitus have been suggested. AA may be accompanied by depression and anxiety2. According to the recent World Health Organization Global Burden of Disease Study, the estimated disability-adjusted life years (DALY) lost by AA patients were higher than those lost by psoriasis patients3, particularly by patients with severe AA. The burden of AA is increasing, and some comorbidities have been reported; however, there have been few studies on cancer risks. Sun et al. reported that female patients with alopecia were at an increased risk of thyroid cancer4. However, this study was a small study, and the cancer risk remains unclear.
To date, national databases have not been used to explore possible associations between alopecia (total or by subtype) and cancers. In the present study, we explored the associations between various AA subtypes and cancer using a National Health Insurance System (NHIS) database.
Results
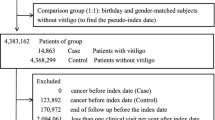
Baseline characteristics of the study population
In total, 668,604 patients were diagnosed with alopecia from 2007 to 2014. We included 608,190 patients with AA and 60,414 with AT/AU in the present study; follow-up ceased on December 31, 2015 (Fig. 1). The mean follow-up time was 4.92 ± 2.32 years. The demographic and clinical characteristics of the study population are shown in Table 1. The mean ages at diagnosis of AA and AT/AU were 40.16 ± 12.74 and 41.29 ± 13.86 years, respectively. The proportions of males with AA and AT/AU were 50.78% and 52.46%, respectively.
Cancer risks based on the AA subtype
Table 2 and Fig. 2 show the results obtained when the AA and AT/AU groups were analyzed by reference to ICD-10 codes. After adjusting for all confounding factors including age, gender, diabetes mellitus, hypertension, dyslipidemia, and income level, the overall cancer risk was higher in both the AA group (hazard ratio (HR), 1.043; 95% confidence interval (CI), 1.022–1.065) and the AT/AU group (HR, 1.070; 95% CI, 1.013–1.129). Notably, the risk of thyroid cancer was higher in the AT/AU group (HR, 1.332; 95% CI, 1.207–1.470) than the AA group (HR, 1.165; 95% CI, 1.122–1.210) or the control group. The risk of prostate cancer was significantly increased in the AA group (HR, 1.259; 95% CI, 1.139–1.391) compared with the AT/AU group (HR, 1.243; 95% CI, 0.963–1.604). In addition, the risk of bladder cancer was significantly increased in the AA group (HR, 1.216; 95% CI, 1.059–1.397) compared with the AT/AU group (HR, 1.024; 95% CI, 0.694–1.512). The risks for cancer of the oral cavity, esophagus, liver, biliary tract, pancreas, larynx, lung, kidney, breast, cervix, ovary, uterus, testis, nerves, and skin; and those for lymphoma, multiple myeloma, and leukemia, were not elevated in alopecia patients. Thus, neither AA nor AT/AU was associated with increased risks of cancers other than thyroid, prostate, and bladder cancers.
Cumulative incidences of overall and thyroid cancer in patients with different subtypes of alopecia (Kaplan-Meier modeling). (a) overall cancer, and (b) thyroid cancer. Control: Control subjects AA group: Patients with alopecia areata except alopecia totalis/alopecia universalis. AT/AU group: Patients with alopecia totalis/alopecia universalis.
Discussion
To our knowledge, this is the first study to investigate the total cancer risk in alopecia patients using a population-based approach. We found that the total cancer risk was increased in alopecia patients compared with age- and sex- matched controls. This was attributable to an increase in the risks of thyroid, prostate, and bladder cancer depending on the alopecia subtype. In particular, the risk of thyroid cancer was higher in the AT/AU group than in the age- and sex- matched control group or the AA group.
Alopecia is a hair-loss disorder associated with inflammation and an autoimmune response5, affecting an estimated 4.5 million people in the United States6. AA is thought to be a TH1-mediated autoimmune disease in which the hair follicle loses its status as an immunoprivileged site, resulting in perifollicular CD8+ cytotoxic T cell infiltration followed by elevated IFN-γ production7. Genetic polymorphisms in genes encoding cytokines affect their transcriptional levels, associated with inter-individual variations in cytokine production, thus influencing the outcomes of cancers and autoimmune diseases8. Lew et al. reported that the single-nucleotide polymorphism IL17RA (rs879577) was significantly enriched in AA patients9. In addition, a significant association between the intron 3VNTR polymorphism of the IL-4 gene and AA susceptibility was reported in a Turkish population10. Kalkan et al. found that the AA risk was associated with the FAS-670 A/G and the FAS ligand (FASLG)-124 A/G polymorphisms11. Recently, Tanemura et al. suggested that AA was a Th17-cell-associated autoimmune disease caused by infiltration of CD4+ expressing IL-17A, and Th17 cells, around hair follicles12. Additionally, low serum 25-hydroxyvitamin D [25(OH)D] levels were suggested to contribute to AA pathogenesis13.
We found that the risk of thyroid cancer was higher in AA patients than the general population. Chu et al. performed a nationwide population-based study in Taiwan and found a relationship between AA and thyroid diseases14. In addition, recent studies have shown that AA is associated with autoimmune thyroiditis, but the causative AA subtype was not identified, and thyroid autoantibodies were absent15,16. Sun et al. reported that the risk of thyroid cancer was increased in females with alopecia, but found no association with AA in general, or a particular AA subtype4. Although no association between AA and thyroid cancer was noted in previous studies, it is significant that our present large-scale study revealed such a relationship, most notably in the AT/AU group.
The association between AA and thyroid cancer may be attributable to shared pathological features. Chronic inflammation increases the long-term risk of cancer of the thyroid, prostate, and bladder17. FAS and FASLG are pro-apoptotic proteins playing major roles in both cancer development and that of various diseases of the immune system18. Reduced FAS expression and/or increased FASLG expression facilitate tumor development and progression by inhibiting tumor cell apoptosis or by inducing immune cell apoptosis. Recently, FAS and FASLG polymorphisms have been reported in various cancers and alopecia11,19. Additional mechanism studies including FAS and FASLG are needed to define the risk of thyroid cancer in AT/AU patients.
We found that AA was associated with an increased risk of prostate cancer (HR, 1.259; 95% CI, 1.139–1.391) compared with AT/AU. Few previous reports have sought associations between AA and prostate cancer. Even the suggested association between androgenic alopecia and prostate cancer remains unclear20,21,22,23. However, androgen levels is suggested influence the pathogenesis of prostate cancer24. Taylor et al. suggested a relationship between a vitamin D receptor gene polymorphism and prostate cancer25. Recently, Conic et al. found that AA was associated with vitamin D deficiency and increased androgen levels, as are thyroid disease, anemia, and eczema26. Thus, increased androgen levels and a vitamin D deficiency may contribute to the pathogenesis of both diseases. Another shared mechanism may be the pathway involving Th17 cells and IL-17. Zhang et al. suggested that IL-17 promoted the initiation and growth of prostate cancer, and that the IL-17-MMP7 pathway was involved in prostatic intraepithelial neoplasia prior to the development of prostate cancer27. However, these mechanisms do not adequately explain the relationship between AA and prostate cancer.
Moreover, we found that AA was associated with an increased risk of bladder cancer (HR, 1.216; 95% CI, 1.059–1.397). Androgen-mediated signaling by the androgen receptor is known to play roles in bladder and urothelial cancer28. Th17 and Treg cells (especially the former) were involved in the development and progression of bladder cancer29. These mechanisms partially overlap with those of prostate cancer (described above). However, it remains difficult to completely explain the associations between alopecia and prostate/bladder cancer; further studies are needed.
In addition, we found that the incidence of skin cancer was not increased in AA patients, consistent with previous studies30,31. Miller et al. found that the risks of non-melanoma skin cancers (basal cell carcinoma and squamous cell carcinoma), and melanoma, were not increased among AA patients in Cleveland (OH, USA)30. Our results also showed that the risk of skin cancer was not increased in AT/AU patients.
Our study had certain limitations. We lacked information on the numbers of alopecia lesions and their treatment, lifestyles, smoking and drinking status, and the levels of physical activity. Also, the ages at onset of alopecia and various cancers differ; our follow-up duration may have been inadequate. Despite these limitations, we found that a large-scale analysis of national data revealed that the risks of thyroid, prostate, and bladder cancer increased depending on the alopecia subtype. Further basic and clinical studies are required. Regular follow-up in terms of thyroid and urinary tract cancers (prostate and bladder cancers) may be necessary for alopecia patients.
Materials and Methods
Ethics approval
This study was approved by the Institutional Review Board of the Korean NHIS (no. NHIS-2017–1–138). The study design was approved by the Ethics Committee of Seoul St. Mary’s Hospital, the Catholic University of Korea (approval no. KC17ZESI0312) and followed all relevant principles of the Declaration of Helsinki.
Data sources
We used the NHIS database, which contains medical information on almost all Koreans. The NHIS manages all health-related data, including checkup results, treatment details, long-term care of the elderly, institutional data, and the frequencies of cancers and rare diseases. The NHIS uses the comprehensive database of the Health Insurance and Review Agency (HIRA)32. The database contains patient demographics, outpatient histories, diagnoses and comorbidities based on the International Classification of Disease (ICD)−10 codes, and prescription and procedural details33. All patients are assigned identification numbers and all data are managed anonymously.
Study population
We retrieved data on patients who visited clinics or hospitals and received the diagnostic code (ICD-10) for alopecia (L63) more than once in any year from January 2007 to December 2014. Of these, subjects under 20 years of age or with a history of cancer during a 2005–2006 washout period were excluded. Finally, alopecia patients older than 20 years were included (n = 668,604) (Fig. 1). The control group (n = 3,343,020) was randomly selected at a 1:5 ratio; this group contained matched age- and sex-stratified subjects who were not treated for alopecia during the same period. In addition, we divided alopecia patients into two groups, as follows: 1) an AA group (ICD-10 codes L63.8 and L63.9) including all types of AA except AT/AU (ICD-10 L63); and, 2) an AT/AU group (ICD-10 codes L63.0 and L63.1).
Cancer information was also extracted from the NHIS database; we sought incident cancer reports to 2015. The Korean government maintains records of patients with cardiovascular and cerebrovascular diseases, cancers, and rare incurable diseases (RIDs), and supports such patients financially. We used the cancer code (ICD-10 C00-C96).
Statistical analysis
Baseline characteristics are presented as means with standard deviations or as numbers with percentages. We calculated cancer incidence rates (in 1,000 person-years) by dividing the number of incident cases by the total follow-up period. Cox’s proportional hazards regression analysis was used to evaluate the association between alopecia presence and subtype, and cancer incidence. Overall and site-specific cancer risks of AA or AT/AU patients compared to those of the age- and sex-matched control population were expressed as hazard ratios (HRs) with 95% confidence intervals (CIs). Model 1 was adjusted for age, gender, and income level; and diabetes mellitus, hypertension, and dyslipidemia status. To avoid temporal bias, we matched the date of alopecia diagnosis with the dates of registration of control subjects. The cumulative cancer incidences by alopecia presence and subtype were calculated using Kaplan–Meier curves, and the log-rank test was employed to analyze differences among the groups. All data were analyzed with the aid of SAS version 9.4 (SAS Institute, Cary, NC, USA) and R version 3.1.0 (the R Foundation for Statistical Computing, Vienna, Austria, http://www.R-project.org) software.
References
Pratt, C. H. et al. Alopecia areata. Nat Rev Dis Primers 3, 17011 (2017).
Villasante Fricke, A. C. & Miteva, M. Epidemiology and burden of alopecia areata: a systematic review. Clin Cosmet Investig Dermatol 8, 397–403 (2015).
Search GBD Data [webpage on the Internet] Seattle, WA: Institute for Health Metrics and Evaluation; 2014. Available from:http://www.healthdata.org/search-gbd-data?s=Alopecia%20areata, [Accessed February 13, 2015]. [cited February 13, 2015].
Sun, L. M. et al. Women with alopecia exhibit a higher risk for thyroid cancer: a nationwide cohort study. J Dermatol Sci 74, 18–22 (2014).
Gilhar, A., Etzioni, A. & Paus, R. Alopecia areata. N Engl J Med 366, 1515–1525 (2012).
McMichael, A. J. et al. Alopecia in the United States: outpatient utilization and common prescribing patterns. J Am Acad Dermatol 57, S49–51 (2007).
Todes-Taylor, N., Turner, R., Wood, G. S., Stratte, P. T. & Morhenn, V. B. T cell subpopulations in alopecia areata. J Am Acad Dermatol 11, 216–223 (1984).
Alzolibani, A. A. & Zedan, K. Macrolides in chronic inflammatory skin disorders. Mediators Inflamm 2012, 159354 (2012).
Lew, B. L. et al. Association between IL17A/IL17RA Gene Polymorphisms and Susceptibility to Alopecia Areata in the Korean Population. Ann Dermatol 24, 61–65 (2012).
Kalkan, G. et al. The association between Interleukin (IL)-4 gene intron 3 VNTR polymorphism and alopecia areata (AA) in Turkish population. Gene 527, 565–569 (2013).
Kalkan, G., Ates, O., Karakus, N. & Sezer, S. Functional polymorphisms in cell death pathway genes FAS and FAS ligand and risk of alopecia areata. Arch Dermatol Res 305, 909–915 (2013).
Tanemura, A. et al. Alopecia areata: infiltration of Th17 cells in the dermis, particularly around hair follicles. Dermatology 226, 333–336 (2013).
Aksu Cerman, A., Sarikaya Solak, S. & Kivanc Altunay, I. Vitamin D deficiency in alopecia areata. Br J Dermatol 170, 1299–1304 (2014).
Chu, S. Y. et al. Comorbidity profiles among patients with alopecia areata: the importance of onset age, a nationwide population-based study. J Am Acad Dermatol 65, 949–956 (2011).
Alkhalifah, A., Alsantali, A., Wang, E., McElwee, K. J. & Shapiro, J. Alopecia areata update: part I. Clinical picture, histopathology, and pathogenesis. J Am Acad Dermatol 62 177–188, quiz 189–190 (2010).
Kasumagic-Halilovic, E. Thyroid autoimmunity in patients with alopecia areata. Acta Dermatovenerol Croat 16, 123–125 (2008).
Demaria, S. et al. Cancer and inflammation: promise for biologic therapy. J Immunother 33, 335–351 (2010).
Griffith, T. S., Brunner, T., Fletcher, S. M., Green, D. R. & Ferguson, T. A. Fas ligand-induced apoptosis as a mechanism of immune privilege. Science 270, 1189–1192 (1995).
Liu, Y. et al. FASLG polymorphism is associated with cancer risk. Eur J Cancer 45, 2574–2578 (2009).
Bhargava, S. Increased DHT levels in androgenic alopecia have been selected for to protect men from prostate cancer. Med Hypotheses 82, 428–432 (2014).
Cremers, R. G. et al. Androgenic alopecia is not useful as an indicator of men at high risk of prostate cancer. Eur J Cancer 46, 3294–3299 (2010).
Muller, D. C. et al. Age-dependent associations between androgenetic alopecia and prostate cancer risk. Cancer Epidemiol Biomarkers Prev 22, 209–215 (2013).
Amoretti, A., Laydner, H. & Bergfeld, W. Androgenetic alopecia and risk of prostate cancer: a systematic review and meta-analysis. J Am Acad Dermatol 68, 937–943 (2013).
Gann, P. H., Hennekens, C. H., Ma, J., Longcope, C. & Stampfer, M. J. Prospective study of sex hormone levels and risk of prostate cancer. J Natl Cancer Inst 88, 1118–1126 (1996).
Taylor, J. A. et al. Association of prostate cancer with vitamin D receptor gene polymorphism. Cancer Res 56, 4108–4110 (1996).
Conic, R. Z., Miller, R., Piliang, M., Bergfeld, W. & Atanaskova Mesinkovska, N. Comorbidities in patients with alopecia areata. J Am Acad Dermatol 76, 755–757 (2017).
Zhang, Q. et al. Interleukin-17 promotes formation and growth of prostate adenocarcinoma in mouse models. Cancer Res 72, 2589–2599 (2012).
Inoue, S., Mizushima, T. & Miyamoto, H. Role of the androgen receptor in urothelial cancer. Mol Cell Endocrinol (2017).
Chi, L. J. et al. Involvement of T helper type 17 and regulatory T cell activity in tumour immunology of bladder carcinoma. Clin Exp Immunol 161, 480–489 (2010).
Miller, R., Conic, R. Z., Bergfeld, W. & Mesinkovska, N. A. Prevalence of Comorbid Conditions and Sun-Induced Skin Cancers in Patients with Alopecia Areata. J Investig Dermatol Symp Proc 17, 61–62 (2015).
Mostaghimi, A., Qureshi, S., Joyce, C., Guo, Y. & Huang, K. P. Reduced incidence of skin cancer in patients with alopecia areata: A retrospective cohort study. Cancer Epidemiol 41, 129–131 (2016).
Song, S. O. et al. Trends in Diabetes Incidence in the Last Decade Based on Korean National Health Insurance Claims Data. Endocrinol Metab (Seoul) 31, 292–299 (2016).
Koo, B. K., Lee, C. H., Yang, B. R., Hwang, S. S. & Choi, N. K. The incidence and prevalence of diabetes mellitus and related atherosclerotic complications in Korea: a National Health Insurance Database Study. PLoS One 9, e110650 (2014).
Acknowledgements
This study was supported by a National Research Foundation of Korea (NRF) grant funded by the Korea government (MSIP) (grant nos NRF-2015R1C1A2A01054767 and No.2016R1C1B1008288). Employment: Recent (while engaged in the research project), present or anticipated employment by any organization that may gain or lose financially through this publication is none to declare. The study was approved by the Ethics Committee of the Catholic Medical Center Office of the Human Research Protection Program (approval no. KC17ZESI0312).
Author information
Authors and Affiliations
Contributions
J.H.L., Y.M.S., J.Y.L., Y.M.P., and Y.B.L. conceived and designed the study. K.D.H. and Y.G.P. analyzed and interpreted the data. J.H.L., Y.M.S., and Y.B.L. drafted the manuscript. All authors supervised the writing of the manuscript and approved the final manuscript.
Corresponding authors
Ethics declarations
Competing Interests
The authors declare no competing interests.
Additional information
Publisher's note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Lee, J.H., Song, Y., Do Han, K. et al. Cancer risk by the subtype of alopecia. Sci Rep 8, 9748 (2018). https://doi.org/10.1038/s41598-018-28142-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-018-28142-1
This article is cited by
-
Baricitinib Safety for Events of Special Interest in Populations at Risk: Analysis from Randomised Trial Data Across Rheumatologic and Dermatologic Indications
Advances in Therapy (2023)
-
A Review of Safety Outcomes from Clinical Trials of Baricitinib in Rheumatology, Dermatology and COVID-19
Advances in Therapy (2022)
-
Economic Burden and Healthcare Resource Use of Alopecia Areata in an Insured Population in the USA
Dermatology and Therapy (2022)
-
Association between male pattern baldness and testicular germ cell tumor: a meta-analysis
BMC Cancer (2019)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.