Abstract
Emerging evidence has shown that self-perception of overweight/obese status is associated with unfavorable cardiometabolic outcomes, above and beyond actual body weight. Given the lack of research among Asian populations, we examined the association between weight perception and metabolic syndrome (MetS) and cardiometabolic risks among Koreans. Data from the 2010–2015 Korea National Health and Nutrition Examination Survey, including women (N = 12,181) and men (N = 9,448) aged 19–65 years, were analyzed. Weight status perception was measured by participants’ self-evaluation of their body size (“very/slightly obese,” “normal,” and “very/slightly thin”). Overall, 23.2% of women and 28.7% of men had MetS. Our cross-sectional multilevel logistic analyses showed a significant positive association between self-perceived obesity (vs. perceived normal weight) and MetS, independent of BMI and sociodemographic/behavioral/medical conditions, with a stronger association detected among men (OR = 1.38, p < 0.05) than women (OR = 1.22, p < 0.05), confirmed by a statistically significant interaction. Additionally, perceived obesity was associated with high blood pressure (OR = 1.27, p < 0.05) and high triglycerides (OR = 1.38, p < 0.05) among men and low high-density lipoprotein cholesterol (OR = 1.15, p < 0.05) among women. While further prospective research is needed, our findings suggest that perception of being obese may be an unfavorable indicator of cardiometabolic health among Koreans regardless of actual body weight.
Similar content being viewed by others
Introduction
Self-perception of body weight has been linked with psychological, behavioral, and biological outcomes above and beyond actual body weight. Among individuals with normal weight, accurate weight perception (i.e., perception of being normal weight) has been consistently linked with more favorable health outcomes compared to weight misperception1,2. However, among individuals with overweight/obesity, the findings have been inconsistent. Some studies have reported that individuals with overweight/obesity who misperceived their weight status as being normal were less likely to have intentions and make attempts to control their weight than their counterparts who accurately perceived their weight status, suggesting that accurate weight perception may be an essential component of successful obesity prevention and weight management3,4,5. This perspective has been either implicitly or explicitly adopted in awareness-raising strategies in public health and clinical practices such as school-based obesity screening with notification of the results through body-mass index (BMI) report cards and weight-loss counseling seeking to motivate weight control by accurately informing patients of their overweight/obese status6,7,8.
Recent research, however, has revealed contradictory findings, whereby weight misperception (vs. accurate perception) among individuals with overweight/obesity led to more favorable outcomes in weight gain9,10,11, depressive symptoms10,12, and cardiometabolic functioning10,13. Furthermore, in a recent systematic review, Haynes and colleagues (2018) concluded that perception of obesity (vs. perception of normal weight) is associated with more unfavorable weight-related outcomes such as disordered eating, unhealthy weight control practice, and weight gain, regardless of the accuracy of the perception14. These studies suggested that individuals who identify their weight status as being overweight/obese may be more vulnerable to the negative psychological processes related with weight-based stigma and discrimination8,9,10,11,12,13,14,15, which in turn can lead to chronic stress reactions, maladaptive coping behaviors, and biological alterations16,17,18. Other studies also suggested that perception of being overweight/obese may be associated with greater use of disordered weight control behaviors (DWCB) including fasting, self-induced vomiting, and taking laxatives/diuretics14. From this viewpoint, investigators have proposed that awareness-oriented approaches in obesity prevention and weight management could stigmatize individuals due to their body weight and impose psychological and metabolic burdens9,10,11,12,13,14.
In South Korea, the population metabolic health indicators have worsened over the past decade. For instance, an increasing trend in the prevalence of obesity was reported among Korean adults (i.e., from 26.9% in 1998 to 32.0% in 2011)19. Moreover, the prevalence of metabolic syndrome (MetS), the clustering of cardiometabolic risk factors (CMRs) such as insulin resistance, central obesity, hypertension, and dyslipidemia, sharply increased from 24.9% in 1998 to 31.3% in 2007 among adults20. However, gaps exist in the current understanding of the association between weight perception and cardiometabolic risks among Asian populations. For instance, despite the emerging evidence showing the harmful influences of accurate weight perception on cardiometabolic outcomes among individuals with obesity in Western countries9,10,11,13, previous Korean studies generally framed weight misperception as a cognitive bias that should be corrected regardless of weight status21,22,23.
Thus, in the present study, we investigated the association of weight perception with MetS and CMRs among Korean adults. Based on prior literature, we hypothesized that perception of being obese (vs. perception of being normal weight status) would be positively associated with MetS and CMRs among Koreans. We also examined whether the association differed across gender and weight status. Based on previous evidence showing greater weight-based discrimination directed toward women than men24,25, we expected that the association between weight perception and MetS and CMRs would be stronger among women than men.
Results
Descriptive Statistics
As shown in Table 1, the mean age of the subjects was 44.7 (SD = 12.5) years (45.0 years in women and 44.3 years in men), and the mean BMI was 23.9 (SD = 3.3) kg/m2 (24.5 kg/m2 in women and 23.5 kg/m2 in men). The prevalences of MetS and CMRs were 25.6% for MetS (23.2% in women and 28.7% in men), 27.9% for high fasting plasma glucose (22.2% in women and 35.3% in men), 32.4% for high blood pressure (26.1% in women and 40.4% in men), 35.4% for low high-density lipoprotein cholesterol (41.8% in women and 27.0% in men), 28.9% for high triglyceride (19.8% in women and 40.6% in men), and 33.0% for high waist circumference (37.7% in women and 27.0% in men).
Multilevel Analyses
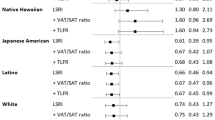
Our multivariable multilevel models showed that weight perception was significantly associated with MetS and CMRs, but differentially across gender (p-values for interaction tests <0.05, Supplementary Table 1.) Counter to our expectation, generally stronger associations were found among men than women for most of the outcomes, except for low HDL-C. As shown in Tables 2 and 3, perception of being obese (vs. perception of being normal weight) was significantly positively associated with MetS among both women (OR = 1.18, 95% CI: 1.04, 1.35, p < 0.05) and men (OR = 1.42, 95% CI: 1.24, 1.63, p < 0.05), after adjusting for BMI, sociodemographic factors, and survey year (Model 1). The direction and statistical significance of these relationships remained consistent after further adjusting for comorbidity (Model 2) and behavioral factors (smoking/drinking/physical activity, Model 3), and DWCB (Model 4).
In terms of the association with CMRs, we found that perception of being obese (vs. perception of being normal weight) was significantly associated with high BP (OR = 1.27, 95% CI: 1.12, 1.44, p < 0.05) and high TG (OR = 1.42, 95% CI: 1.24, 1.63, p < 0.05) among men, after adjusting for BMI, sociodemographic factors, and survey year in Model 1. The direction and significance of these associations were consistent after further adjusting for other covariates across different models. However, there was no such relationship for high FPG and low HDL-C among men.
Conversely, among women, perception of being obese (vs. perception of being normal weight) was marginally, but not statistically, significantly associated with low HDL-C (OR = 1.11, 95% CI: 0.98, 1.25, p < 0.10), after adjusting for BMI, sociodemographic factors, and survey year in Model 1. The size of this association slightly increased after further adjusting for behavioral factors such as smoking, drinking, physical activity, and DWCB (OR = 1.15, 95% CI: 1.01, 1.33, p < 0.05). However, we failed to find a significant relationship for other CMRs among women. Notably, perception of being obese (vs. perception of being normal weight) was associated with high FPG (OR = 1.38, 95% CI: 1.12, 1.71, p < 0.05) among women.
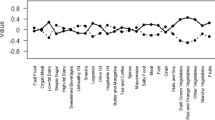
Our analysis also showed that DWCB was generally inversely associated with MetS and CMRs, but there were some differences between women and men particularly for MetS and high TG (interaction p-values < 0.05, Supplementary Table 1). For instance, after adjusting for all other covariates, DWCB was inversely associated with MetS (OR = 0.66, 95% CI: 0.52, 0.83, p < 0.05) and high TG (OR = 0.82, 95% CI: 0.69, 0.98, p < 0.05) among women, (Table 2) but not among men (OR for MetS = 0.93, 95% CI: 0.73, 1.17, p > 0.05; OR for high TG = 0.93, 95% CI: 0.73, 1.17, p > 0.05, Table 3).
Tables 4 and 5 showed the results of our sensitivity analyses only among a subset of participants with concordant BMI and waist circumference. In general, the findings between our primary and sensitivity analyses were largely consistent. For instance, perception of being obese (vs. perception of being normal weight) was significantly associated with MetS among both women (OR = 1.27, 95% CI: 1.04, 1.52, p < 0.05) and men (OR = 1.64, 95% CI: 1.39, 1.93, p < 0.05), after adjusting for BMI, sociodemographic factors, and survey year. In terms of CMRs, perception of being obese (vs. perception of being normal weight) was significantly associated with high BP (OR = 1.24, 95% CI: 1.07, 1.44, p < 0.05) and high TG (OR = 1.22, 95% CI: 1.06, 1.40, p < 0.05) among men. Although we failed to find evidence of significant association between perception of being obese and low HDL-C among women in some models (i.e., OR = 1.14, 95% CI: 0.97, 1.36, p > 0.05 in Model 1), the direction of the associations were consistent with our primary analysis across all models.
It is notable that, in our sensitivity analysis, perception of being underweight (vs. perception of being normal weight) was significantly positively associated with MetS in both women (OR = 1.51, 95% CI: 1.07, 2.14, p < 0.05) and men (OR = 1.42, 95% CI: 1.13, 1.79, p < 0.05) and high FPG in women (OR = 1.43, 95% CI: 1.14, 1.80, p < 0.05).
Our analysis of interactions between weight perception and weight status among women and men, separately, showed that there was no evidence of significant interaction except for high blood pressure (interaction p-value <0.05) among men (Supplementary Tables 2 and 3).
Discussion
Given the lack of understanding regarding the linkage between weight perception and cardiometabolic health in Asian countries, the present study examined whether weight perception was cross-sectionally associated with MetS and CMRs among a nationally representative sample of Korean adults. We found that individuals who identified their weight status as being slightly/very obese (vs. normal weight) were 18–54% more likely to meet the criteria of MetS, independent of their actual body weight and other sociodemographic/medical/behavioral factors. Counter to our expectation, the size of the association was greater among men than women. Moreover, the association with specific CMR differed across gender. Among men, those who self-classified their weight as being obese (vs. normal) were 25–29% more likely to have high BP and 37–54% more likely to have high TG. Among women, individuals who described their weight as being obese (vs. normal) were 10–15% more likely to have low HDL-C. These associations did not differ across weight status for all outcomes, except for high BP in men. To our knowledge, this study is the first to document such relationships among Koreans.
Our results are consistent with the findings from recent studies showing that perception of normal weight (i.e., weight underperception) was associated with lower systolic blood pressure13 and more favorable physiological functioning (i.e., a composite measure of inflammatory, cardiovascular, and metabolic biomarkers)10 among US youth with overweight/obesity. While these studies found no difference in the association across gender10,13, we found a stronger association between weight perception and MetS among men than women. This is contrary to our initial hypothesis that perceived normal weight (vs. perceived obesity) would be more protective among women than men given that fat bias has been found to be more strongly directed toward women than men24,25.
Moreover, when it comes to CMR, we found different patterns across gender, whereby significant associations were found for high BP and high TG among men, whereas a significant association was detected for low HDL-C among women. Given the prior evidence connecting perceived obesity with MetS among individuals with normal weight26, our study replicates and extends the previous research by documenting that dyslipidemia (i.e., low HDL-C in women and high TG in men) and high BP could drive the overall association between weight perception and MetS.
In a broader sense, our findings are also in line with previous evidence showing a protective association of perception of normal weight (i.e., weight underperception vs. accurate perception) with weight change9,10,11 and depressive symptoms12 among adolescents and young adults with overweight/obesity. Similarly, our findings also align with a previous prospective study documenting a positive association between weight overperception (vs. accurate perception) and risk of weight gain and obesity among adolescents with normal weight2.
To understand how self-assessment of weight status can be associated with cardiometabolic and psychological health outcomes, recent studies have focused on emotional responses related with perception of body size6,7,8,9,10,11,12,13,14,15,27,28. That is, studies have suggested that, considering negative societal values and images attached to obesity, self-evaluation of being obese could be associated with weight bias internalization, low self-esteem, and body dissatisfaction8,9,10,11,12,13,14,15,27,28. An accumulated body of research has shown that weight stigma is prevalent in a number of populations across diverse social groups16,29,30,31,32, and weight discrimination can induce sustained psychological distress and maladaptive coping behaviors, which can lead to biological alterations such as prolonged hyperactivation of the hypothalamic-pituitary-adrenal axis and cortisol secretion, increased weight gain, and dysregulation of inflammatory and cardiometabolic processes10,17,18,33.
Additionally, recent studies have found that being identified as overweight/obese by others (i.e., weight labeling) and by BMI report cards through BMI screening is associated with increased weight gain among US female youth34,35. By inter-relating weight stigma, identification of overweight/obese status by others or BMI report cards, and self-perception of being obese, recent studies have suggested that individuals who accurately perceive their overweight/obese status might experience negative psychological processes related with weight stigma and body dissatisfaction, which can result in weight gain and cardiometabolic dysregulations8,9,10,13,27.
Recent studies have shown that weight bias may be prevalent in South Korea24. While a plump body was favored in the traditional Korean society, the rapid economic and sociocultural changes reshaped the normative body image, bringing out the widespread thin-ideal in Koreans24,36,37,38. This was supported by recent studies showing that Koreans hold the strongest preference for individuals with thin body (vs. individuals with obesity) among all participants globally from the seventy-two countries involved in the Project Implicit39. Moreover, the prevalence of disordered weight control behaviors and body dissatisfaction among Korean adolescents and young adults were found to be comparable to that among US adolescents and young adults40,41. As proposed by Robinson (2017), it is possible that Koreans with perception of obesity may experience higher levels of psychological distress due to their perception of belonging to a socially stigmatized group, which can be detrimental to psychological and cardiometabolic well-being28.
Additionally, we also found that women who identified themselves as being slightly/very thin (vs. normal weight) were 36–38% more likely to have high FPG. Previous prospective and cross-sectional studies documented that perceived underweight (vs. normal weight) was associated with increased risk of depression among adolescents1,12,42 and adults43. This study is the first to report an association with cardiometabolic outcomes. It has been suggested that perception of underweight may be related to body image distortion and dissatisfaction, reflecting a desire for masculinity particularly among adolescent and young adult men42,43,44,45,46. However, further research is warranted to verify and understand such association with cardiometabolic outcomes in women as well as men.
Contrary to prior evidence showing a positive association between DWCB and weight gain2,47,48,49, we found that DWCB was generally inversely associated with MetS and CMRs among women and men. Most prior studies, though not all, have found that DWCB (i.e., fasting, skipping meals, self-induced vomiting, and using diet pills) was associated with an elevated risk of subsequent weight gain and obesity47,48,49. Regarding the paradoxical associations between dieting and weight gain, prior studies mainly suggested potential explanations such as food preoccupation and over-/binge eating47,48,49, increased psychological distress50, and metabolic adaptation48,51. Nevertheless, in other studies, caloric restriction, defined as reduced caloric intake without deprivation of necessary nutrients, has been linked with favorable cardiometabolic outcomes52,53,54. Further prospective studies with more detailed information on dietary behaviors are necessary to understand the association in the Korean context.
Our study has several limitations. First, our cross-sectional design is susceptible to reverse causation. It is possible that individuals with MetS were more likely to have psychological distress and depressive symptoms, which could influence self-perception of weight status and weight control behaviors. Although our models adjusted for an extensive range of variables such as BMI (as a quadratic term), medical history (depression and cancer/stroke/heart attack/renal failure/cirrhosis), and behavioral (smoking, alcohol drinking, and exercise) and sociodemographic profiles, we cannot preclude reverse causality. Additionally, misclassification of weight perception pattern is possible, particularly among those with discrepant BMI and WC values. However, our sensitivity analysis using only individuals with concordant BMI and WC values showed largely consistent associations with our primary analyses. Lastly, while prior studies suggested over-/binge eating as potential behavioral pathways linking weight perception and DWCB with weight gain27,47, we were not able to obtain information on over-/binge eating.
However, our study also had the following strengths. To the best of our knowledge, this study is the first to document the associations of weight status perception with CMRs in an Asian sample. We used a large nationally representative sample with objectively measured anthropometric and biochemical information. Additionally, we investigated differential associations across gender and weight category, and extended our analysis to examine CMRs as well as MetS. Lastly, given the well-documented clustering of CMRs within households55,56 and geographic localities57, we performed four-level multilevel models, incorporating all sampling stages (areas-neighborhoods-households-individuals) as units of analysis, thereby adjusting for clustering induced by the hierarchical data structure. To our knowledge, our analysis is the first to use a full four-level multilevel approach with the KNHANES datasets.
The findings of this study suggest that the self-perception of being obese may be associated with unfavorable cardiometabolic health markers, regardless of actual body weight. That is, while accurate weight perception may be a sign of healthier cardiometabolic functioning than weight misperception among individuals with normal weight, the opposite may be true for individuals with obesity. Our findings support the emerging perspective that raises concerns regarding awareness-oriented approaches for weight management and obesity prevention implemented in clinical and public health practices. At the policy level, obesity prevention strategies that focus on alarming those at elevated risk of obesity such as BMI report cards interventions need to take into account the potential unexpected adverse influences of “accurate” perception among individuals with obesity. In clinical practice, providers may be able to incorporate information on weight perception in risk identification for cardiometabolic dysregulation. As suggested by recent studies, weight loss and obesity prevention approaches may benefit from focusing on lifestyle changes such as healthy eating and physical activity.
Methods
Study Population
Data were from the 2010–2015 Korea National Health and Nutrition Examination Survey (KNHANES), conducted by the Korea Centers for Disease Control and Prevention (K-CDC)58. With a nationally representative sample, the survey monitors the health, behavioral, and nutritional profiles of Koreans. KNHANES employed a stratified three-stage cluster sampling procedure, including 192 geographic areas (i.e., neighborhood/town/township) as primary sampling units (PSU), 20 households within each PSU as secondary sampling units, and all household members aged 1 year or older as final sampling units58.
Of the 60,917 individuals initially targeted, 48,482 individuals participated in the survey (Fig. 1). Of these, we included adults aged 19–65 years, with BMI > = 18.5 kg/m2, not pregnant/breastfeeding, and without any missing information on the variables used in our analyses, yielding an analytic sample of 21,629 individuals (12,181 women and 9,448 men). All participants consented to participate in the survey. Since we used de-identified public-use data, this study received an IRB review exemption by the Office of Human Research Administration at the Harvard T.H. Chan School of Public Health.
Subject Evaluation and Laboratory Assessment
Anthropometric information was obtained by trained medical staff at mobile examination centers. Height and weight, respectively, were measured with a portable stadiometer (with precision of 1 mm with participants standing barefoot) and electronic scale (with precision of 100 g with participants wearing a light gown). Obesity was defined as a BMI (weight in kilograms divided by height in meters squared) value of 25.0 kg/m2 or above, according to the revised criteria for Asian-Pacific populations from the World Health Organization59,60. Waist circumference (WC) was measured with a measuring tape (with precision of 1 mm) at the midway between the iliac crest and lower rib margin after normal expiration58.
After participants had rested in a sitting position (> = 5 minutes), systolic and diastolic blood pressures (BP) were assessed with a standard mercury sphygmomanometer from the right arm three times each for systolic and diastolic BPs, with a 30-second interval between measurements. Our analysis used the mean values of the second and third assessments of BP based on the K-CDC’s guideline and previous literature61.
Blood samples were collected from participants’ antecubital vein after fasting (> = 8 hours), centrifuged and refrigerated at the mobile examination center, then transferred in ice boxes to a central laboratory in Seoul within 24 hours. Triglycerides (TG), fasting plasma glucose (FPG), and high-density lipoprotein cholesterol (HDL-C) were assessed with an automated hematology analyzer at the central laboratory58.
Metabolic Syndrome and Cardiometabolic Risk Factors
MetS was defined, according to the revised definition of the National Cholesterol Education Program-Adult Treatment Panel III, as the presence of > = 3 CMRs: (a) high WC (> = 90 cm for men, > = 80 for women)62, (b) high FPG (> = 100 mg/dL, or anti-hyperglycemic agent use), (c) high BP (> = 130/85 mmHg, or antihypertensive agent use), (d) low HDL-C (<40 mg/dL for men, <50 mg/dL for women), and (e) high TG (> = 150 mg/dL)63. The criteria for each CMR was based on the Joint Scientific Statement by the International Diabetes Federation, National Heart, Lung, and Blood Institute, and American Heart Association63.
Weight Status Perception
Perceived body weight status was measured with the question, “How would you describe your body shape?” The original responses (“very obese,” “slightly obese,” “normal,” “slightly thin,” and “very thin”) were grouped as “very/slightly obese,” “normal,” and “slightly/very thin.”58
Disordered weight control behaviors (DWCB)
Participants were asked whether they had engaged in the following behaviors for weight control over the past year: fasting, skipping meals, following a one-food diet (i.e., eating only one specific food for diet), and using unprescribed diet pills, with a yes/no response option for each item58. Based on prior literature, a composite indicator variable for DWCB was generated to represent whether a participant engaged in at least one of the four behaviors over the past year.
Covariates Assessment
Educational attainment (middle school or less, high school, and college graduate or higher) was measured based on the participants’ highest academic diploma achieved. Quartiles of equivalized total household income (i.e., self-reported total household income divided by the number of household members squared) was used to measure economic status. Marital status was grouped as married, widowed/divorced/separated, and never married58. Smoking behavior was categorized as a non-smoker (lifetime smoking less than 5 packs), former smoker (have not smoked within the last 30 days with lifetime smoking of 5 packs or more), and current smoker (smoked within the last 30 days with lifetime smoking of 5 packs or more). A binary variable for high-risk alcohol use was created, indicating heavy drinking (> = 7 glasses for men and > = 5 glasses for women per each instance), which occurred frequently (> = 2 times/week) over the past 12 months. Regular moderate-level physical activity, a binary variable, was defined as engaging in exercise that moderately elevated breathing or heart rate for 10 minutes or more each instance, for 3 days or more every week. Self-reported information on medical history was used to create indicator variables for physician-diagnosed depression and chronic severe condition (any of stroke/cancer/heart attack/renal failure/cirrhosis)58.
Data Availability
All data used in this study is publicly available upon request via https://knhanes.cdc.go.kr/.
Statistical Analysis
To understand the association between weight perception pattern and MetS, we constructed four-level multilevel logistic models, where individuals (N = 21,623: level 1) were nested within households (N = 13,182: level 2), nested within neighborhoods (N = 1,152: level 3), and nested within geographic areas (N = 16: level 4), thereby adjusting for the potential clustering of MetS within households and neighborhoods induced by the hierarchical data structure. Based on prior evidence of differences in pathophysiology of MetS by gender64 and significant interactions between gender and weight perception in our samples (p-values for interaction tests for MetS and CMRs <0.05, Supplementary Table S1), we constructed gender-stratified models.
A set of covariates was sequentially added to the models: age (year, as a linear term), BMI (kg/m2, as a quadratic term), menopause (for women), sociodemographic factors such as education, marital status, household income, urbanicity of residential area, and survey year in Model 1; comorbidity such as history of depression and severe chronic condition (cancer/stroke/coronary heart disease) in Model 2; health-related behaviors smoking, drinking, and exercise in Model 3. Based on prior literature showing an association between weight perception and DWCB15 and an association between DWCB and weight gain47,48,49, we further included DWCB in Model 4, based on Model 3, to understand whether DWCB explains the potential association between weight perception and MetS.
To address the potential issue of confounding by actual body weight, we included BMI (kg/m2) as a mean-centered quadratic term based on the most favorable (smallest) deviance information criteria statistics from a model with a quadratic BMI compared to models with a categorical or linear continuous BMI. To better understand which specific CMR contributed to the potential association between weight perception and MetS, we examined high FPG, high BP, low HDL-C, and high TG separately as an outcome.
Concerning possible misclassification of weight perception among individuals with discordant BMI and waist circumference (WC) categories (e.g., an individual with high WC but still within the “normal” BMI range), we performed sensitivity analysis by restricting the analyses only to individuals with concordant BMI and WC categories (including 10,174 women with either WC > = 80 cm and BMI > = 25 kg/m2 or WC < 80 cm and BMI < 25 kg/m2; and 7,631 men with either WC > = 90 cm and BMI > = 25 kg/m2 or WC < 90 cm and BMI < 25 kg/m2).
As a post-hoc analysis, we tested whether the associations were stronger among individuals with obesity (BMI > = 25.0 kg/m2) among women and men separately.
All statistical analyses were performed with MLwiN 3.01 (Bristol University). We employed the Markov Chain Monte Carlo method with the Metropolis-Hastings algorithm based on uninformative priors for multilevel analyses65.
References
Al Mamun, A. et al. Adolescents’ perceived weight associated with depression in young adulthood: a longitudinal study. Obesity (Silver Spring, Md.) 15, 3097–3105, https://doi.org/10.1038/oby.2007.369 (2007).
Liechty, J. M. & Lee, M. J. Body size estimation and other psychosocial risk factors for obesity onset among US adolescents: findings from a longitudinal population level study. Int. J. Obes. (Lond.) 39, 601–607, https://doi.org/10.1038/ijo.2014.191 (2015).
Duncan, D. et al. Does perception equal reality? Weight misperception in relation to weight-related attitudes and behaviors among overweight and obese US adults. International Journal of Behavioral Nutrition and Physical Activity 8, 20 (2011).
Edwards, N. M., Pettingell, S. & Borowsky, I. W. Where perception meets reality: self-perception of weight in overweight adolescents. Pediatrics 125, e452–458, https://doi.org/10.1542/peds.2009-0185 (2010).
Johnson, F., Beeken, R. J., Croker, H. & Wardle, J. Do weight perceptions among obese adults in Great Britain match clinical definitions? Analysis of cross-sectional surveys from 2007 and 2012. BMJ open 4, e005561 (2014).
Dollar, E., Berman, M. & Adachi-Mejia, A. M. Do No Harm: Moving Beyond Weight Loss to Emphasize Physical Activity at Every Size. Prev. Chronic Dis. 14, E34, https://doi.org/10.5888/pcd14.170006 (2017).
Changing the Weight-loss Subject. JAMA 317, 2477, doi:10.1001/jama.2017.7240 (2017).
Robinson, E., Haynes, A., Sutin, A. R. & Daly, M. Telling people they are overweight: helpful, harmful or beside the point? Int. J. Obes. (Lond.) 41, 1160–1161, https://doi.org/10.1038/ijo.2017.85 (2017).
Sonneville, K. R. et al. Helpful or harmful? Prospective association between weight misperception and weight gain among overweight and obese adolescents and young adults. Int. J. Obes. (Lond.) 40, 328–332, https://doi.org/10.1038/ijo.2015.166 (2016).
Daly, M., Robinson, E. & Sutin, A. R. Does Knowing Hurt? Perceiving Oneself as Overweight Predicts Future Physical Health and Well-Being. Psychol. Sci. 28, 872–881, https://doi.org/10.1177/0956797617696311 (2017).
Rancourt, D., Thurston, I. B., Sonneville, K. R., Milliren, C. E. & Richmond, T. K. Longitudinal impact of weight misperception and intent to change weight on body mass index of adolescents and young adults with overweight or obesity. Eating behaviors 27, 7–13, https://doi.org/10.1016/j.eatbeh.2017.08.002 (2017).
Thurston, I. B. et al. Cross-sectional and Prospective Examination of Weight Misperception and Depressive Symptoms Among Youth with Overweight and Obesity. Prevention Science, 1–12 (2016).
Unger, E. S. et al. Protective Misperception? Prospective Study of Weight Self-Perception and Blood Pressure in Adolescents With Overweight and Obesity. J. Adolesc. Health 60, 680–687, https://doi.org/10.1016/j.jadohealth.2016.12.017 (2017).
Haynes, A., Kersbergen, I., Sutin, A., Daly, M. & Robinson, E. A systematic review of the relationship between weight status perceptions and weight loss attempts, strategies, behaviours and outcomes. Obes. Rev. 19, 347–363, https://doi.org/10.1111/obr.12634 (2018).
Sonneville, K. R., Thurston, I. B., Milliren, C. E., Gooding, H. C. & Richmond, T. K. Weight misperception among young adults with overweight/obesity associated with disordered eating behaviors. Int. J. Eat. Disord. 49, 937–946, https://doi.org/10.1002/eat.22565 (2016).
Puhl, R. M. & Heuer, C. A. Obesity stigma: important considerations for public health. Am. J. Public Health 100, 1019–1028, https://doi.org/10.2105/AJPH.2009.159491 (2010).
Vadiveloo, M. & Mattei, J. Perceived Weight Discrimination and 10-Year Risk of Allostatic Load Among US Adults. Ann. Behav. Med. 51, 94–104, https://doi.org/10.1007/s12160-016-9831-7 (2017).
Pearl, R. L. et al. Association between weight bias internalization and metabolic syndrome among treatment-seeking individuals with obesity. Obesity (Silver Spring, Md.) 25, 317–322, https://doi.org/10.1002/oby.21716 (2017).
Kim, C. S. et al. Prevalence, Awareness, and Management of Obesity in Korea: Data from the Korea National Health and Nutrition Examination Survey (1998–2011). Diabetes Metab. J. 38, 35–43, https://doi.org/10.4093/dmj.2014.38.1.35 (2014).
Lim, S. et al. Increasing prevalence of metabolic syndrome in Korea the Korean national health and nutrition examination survey for 1998–2007. Diabetes Care 34, 1323–1328 (2011).
Joh, H. K., Oh, J., Lee, H. J. & Kawachi, I. Gender and socioeconomic status in relation to weight perception and weight control behavior in Korean adults. Obes Facts 6, 17–27, https://doi.org/10.1159/000346805 (2013).
Lim, H. & Wang, Y. Body weight misperception patterns and their association with health-related factors among adolescents in South Korea. Obesity (Silver Spring, Md.) 21, 2596–2603, https://doi.org/10.1002/oby.20361 (2013).
Kim, Y. & Kawachi, I. School- and Individual-level Predictors of Weight Status Misperception among Korean Adolescents: A National Online Survey. PLoS One 11, e0154826, https://doi.org/10.1371/journal.pone.0154826 (2016).
Brewis, A. A., Han, S. Y. & SturtzSreetharan, C. L. Weight, gender, and depressive symptoms in South Korea. Am. J. Hum. Biol. 29, n/a–n/a, https://doi.org/10.1002/ajhb.22972 (2017).
Holliday, R. & Elfving-Hwang, J. Gender, Globalization and Aesthetic Surgery in South Korea. Body & Society 18, 58–81, https://doi.org/10.1177/1357034x12440828 (2012).
Yoon, S. H. et al. Combined effect of body mass index and body size perception on metabolic syndrome in South Korea: results of the fifth Korea National Health and Nutrition Examination Surveys (2010–2012). BMC Public Health 15, 554, https://doi.org/10.1186/s12889-015-1839-6 (2015).
Robinson, E., Hunger, J. M. & Daly, M. Perceived weight status and risk of weight gain across life in US and UK adults. Int. J. Obes. (Lond.) 39, 1721–1726, https://doi.org/10.1038/ijo.2015.143 (2015).
Robinson, E. Overweight but unseen: a review of the underestimation of weight status and a visual normalization theory. Obes. Rev. 18, 1200–1209, https://doi.org/10.1111/obr.12570 (2017).
Puhl, R. M. & Heuer, C. A. The stigma of obesity: a review and update. Obesity (Silver Spring, Md.) 17, 941–964, https://doi.org/10.1038/oby.2008.636 (2009).
Puhl, R. & Brownell, K. D. Bias, discrimination, and obesity. Obes. Res. 9, 788–805, https://doi.org/10.1038/oby.2001.108 (2001).
Puhl, R. M. et al. A multinational examination of weight bias: predictors of anti-fat attitudes across four countries. Int. J. Obes. 39, 1166–1173, https://doi.org/10.1038/ijo.2015.32 (2015).
Puhl, R., Peterson, J. L. & Luedicke, J. Fighting obesity or obese persons? Public perceptions of obesity-related health messages. Int. J. Obes. (Lond.) 37, 774–782, https://doi.org/10.1038/ijo.2012.156 (2013).
Blodorn, A., Major, B., Hunger, J. & Miller, C. Unpacking the psychological weight of weight stigma: A rejection-expectation pathway. J. Exp. Soc. Psychol. 63, 69–76, https://doi.org/10.1016/j.jesp.2015.12.003 (2016).
Hunger, J. M. & Tomiyama, A. J. Weight labeling and obesity: a longitudinal study of girls aged 10 to 19 years. JAMA pediatrics 168, 579–580, https://doi.org/10.1001/jamapediatrics.2014.122 (2014).
Almond, D., Lee, A. & Schwartz, A. E. Impacts of classifying New York City students as overweight. Proc. Natl. Acad. Sci. USA 113, 3488–3491, https://doi.org/10.1073/pnas.1518443113 (2016).
Kim, Y. et al. Risk factors for disordered weight control behaviors among Korean adolescents: Multilevel analysis of the Korea Youth Risk Behavior Survey. Int. J. Eat. Disord. 51, 124–138, https://doi.org/10.1002/eat.22820 (2018).
Thomas, J. J., Lee, S. & Becker, A. E. Updates in the epidemiology of eating disorders in Asia and the Pacific. Curr Opin Psychiatry 29, 354–362, https://doi.org/10.1097/yco.0000000000000288 (2016).
Pike, K. M. & Dunne, P. E. The rise of eating disorders in Asia: a review. Journal of eating disorders 3, 33, https://doi.org/10.1186/s40337-015-0070-2 (2015).
Marini, M. et al. Overweight people have low levels of implicit weight bias, but overweight nations have high levels of implicit weight bias. PLoS One 8, e83543, https://doi.org/10.1371/journal.pone.0083543 (2013).
Jung, J. & Forbes, G. B. Body dissatisfaction and disordered eating among college women in China, South Korea, and the United States: contrasting predictions from sociocultural and feminist theories. Psychol. Women Q. 31, 381–393, https://doi.org/10.1111/j.1471-6402.2007.00387.x (2007).
Lee, H. J. et al. The association between disturbed eating behavior and socioeconomic status: the Online Korean Adolescent Panel Survey (OnKAPS). PLoS One 8, e57880, https://doi.org/10.1371/journal.pone.0057880 (2013).
Blashill, A. J. & Wilhelm, S. Body Image Distortions, Weight, and Depression in Adolescent Boys: Longitudinal Trajectories into Adulthood. Psychol. Men Masc. 15, 445–451, https://doi.org/10.1037/a0034618 (2014).
Gaskin, J. L. et al. Perception or reality of body weight: which matters to the depressive symptoms. J. Affect. Disord. 150, 350–355, https://doi.org/10.1016/j.jad.2013.04.017 (2013).
Calzo, J. P., Corliss, H. L., Blood, E. A., Field, A. E. & Austin, S. B. Development of muscularity and weight concerns in heterosexual and sexual minority males. Health Psychol. 32, 42–51, https://doi.org/10.1037/a0028964 (2013).
Calzo, J. P., Sonneville, K. R., Scherer, E. A., Jackson, B. & Austin, S. B. Gender Conformity and Use of Laxatives and Muscle-Building Products in Adolescents and Young Adults. Pediatrics, https://doi.org/10.1542/peds.2015-4073 (2016).
Calzo, J. P. et al. Patterns of body image concerns and disordered weight- and shape-related behaviors in heterosexual and sexual minority adolescent males. Dev. Psychol. 51, 1216–1225, https://doi.org/10.1037/dev0000027 (2015).
Neumark-Sztainer, D., Wall, M., Story, M. & Standish, A. R. Dieting and unhealthy weight control behaviors during adolescence: associations with 10-year changes in body mass index. J. Adolesc. Health 50, 80–86, https://doi.org/10.1016/j.jadohealth.2011.05.010 (2012).
Pietilainen, K. H., Saarni, S. E., Kaprio, J. & Rissanen, A. Does dieting make you fat? A twin study. Int. J. Obes. (Lond.) 36, 456–464, https://doi.org/10.1038/ijo.2011.160 (2012).
Stice, E., Presnell, K., Shaw, H. & Rohde, P. Psychological and behavioral risk factors for obesity onset in adolescent girls: a prospective study. J. Consult. Clin. Psychol. 73, 195–202, https://doi.org/10.1037/0022-006X.73.2.195 (2005).
Tomiyama, A. J. et al. Low calorie dieting increases cortisol. Psychosom. Med. 72, 357–364, https://doi.org/10.1097/PSY.0b013e3181d9523c (2010).
Fothergill, E. et al. Persistent metabolic adaptation 6 years after “The Biggest Loser” competition. Obesity 24, 1612–1619, https://doi.org/10.1002/oby.21538 (2016).
Ravussin, E. et al. A 2-Year Randomized Controlled Trial of Human Caloric Restriction: Feasibility and Effects on Predictors of Health Span and Longevity. J. Gerontol. A Biol. Sci. Med. Sci. 70, 1097–1104, https://doi.org/10.1093/gerona/glv057 (2015).
Horne, B. D., Muhlestein, J. B. & Anderson, J. L. Health effects of intermittent fasting: hormesis or harm? A systematic review. Am. J. Clin. Nutr. 102, 464–470, https://doi.org/10.3945/ajcn.115.109553 (2015).
Mattson, M. P., Longo, V. D. & Harvie, M. Impact of intermittent fasting on health and disease processes. Ageing Res Rev, https://doi.org/10.1016/j.arr.2016.10.005 (2016).
Bosy-Westphal, A. et al. Familial influences and obesity-associated metabolic risk factors contribute to the variation in resting energy expenditure: the Kiel Obesity Prevention Study. The American Journal of Clinical Nutrition 87, 1695–1701 (2008).
Ehret, G. B. et al. Genetic variants in novel pathways influence blood pressure and cardiovascular disease risk. Nature 478, 103–109, https://doi.org/10.1038/nature10405 (2011).
Leal, C. & Chaix, B. The influence of geographic life environments on cardiometabolic risk factors: a systematic review, a methodological assessment and a research agenda. Obes. Rev. 12, 217–230, https://doi.org/10.1111/j.1467-789X.2010.00726.x (2011).
Kweon, S. et al. Data resource profile: the Korea National Health and Nutrition Examination Survey (KNHANES). Int. J. Epidemiol. 43, 69–77, https://doi.org/10.1093/ije/dyt228 (2014).
Oh, S. W. Obesity and metabolic syndrome in Korea. Diabetes Metab. J. 35, 561–566, https://doi.org/10.4093/dmj.2011.35.6.561 (2011).
Park, S., Lee, S., Hwang, J. & Kwon, J. W. The impact of weight misperception on health-related quality of life in Korean adults (KNHANES 2007–2014): a community-based cross-sectional study. BMJ open 7, e016098, https://doi.org/10.1136/bmjopen-2017-016098 (2017).
Tran, B. T., Jeong, B. Y. & Oh, J.-K. The prevalence trend of metabolic syndrome and its components and risk factors in Korean adults: results from the Korean National Health and Nutrition Examination Survey 2008–2013. BMC Public Health 17, 71, https://doi.org/10.1186/s12889-016-3936-6 (2017).
Lee, S. Y. et al. Appropriate waist circumference cutoff points for central obesity in Korean adults. Diabetes Res. Clin. Pract. 75, 72–80, https://doi.org/10.1016/j.diabres.2006.04.013 (2007).
Alberti, K. G. et al. Harmonizing the metabolic syndrome: a joint interim statement of the International Diabetes Federation Task Force on Epidemiology and Prevention; National Heart, Lung, and Blood Institute; American Heart Association; World Heart Federation; International Atherosclerosis Society; and International Association for the Study of Obesity. Circulation 120, 1640–1645, https://doi.org/10.1161/circulationaha.109.192644 (2009).
Regitz-Zagrosek, V., Lehmkuhl, E. & Weickert, M. O. Gender differences in the metabolic syndrome and their role for cardiovascular disease. Clin. Res. Cardiol. 95, 147–147, https://doi.org/10.1007/s00392-006-0377-8 (2006).
Dunn, E. C., Milliren, C. E., Evans, C. R., Subramanian, S. V. & Richmond, T. K. Disentangling the relative influence of schools and neighborhoods on adolescents’ risk for depressive symptoms. Am. J. Public Health 105, 732–740, https://doi.org/10.2105/AJPH.2014.302374 (2015).
Acknowledgements
This work was supported by the Ellen Feldberg Gordon Challenge Fund for Eating Disorders Research and the Strategic Training Initiative for the Prevention of Eating Disorders at the Harvard T.H. Chan School of Public Health and Boston Children’s Hospital, Boston, Massachusetts, USA. The authors declare that the study sponsor had no role in any aspects of the study including study design, collection, analysis, and interpretation of data, writing the manuscript, and the decision to submit the manuscript for publication. The authors would like to thank the participants of KNHANES V–VI (2010–2015) and thank the Korea Centers for Disease Control and Prevention for the provision of the data for this study. The authors would also like to thank Mr. Christopher Charlton at the Centre for Multilevel Modeling at the University of Bristol for his support in statistical programming, Dr. Paul Bain at the Countway Library of Medicine, Harvard Medical School, for his supports in searching the literature and establishing the bibliography, and Dr. Amy Ehntholt and Mr. Chad Bayowski for all their valuable comments on this work.
Author information
Authors and Affiliations
Contributions
Y.K. conceived the study design, performed the analysis, and drafted the manuscript. I.K. supervised the study, including study design, analysis, and interpretation of the results, S.B.A. advised the study design and interpretation of the results, and S.V.S. advised the analytic strategy. All authors participated in the development of the study, discussed the results, and critically revised the manuscript.
Corresponding author
Ethics declarations
Competing Interests
The authors declare no competing interests.
Additional information
Publisher's note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Kim, Y., Austin, S.B., Subramanian, S. et al. The Cardiometabolic Burden of Self-Perceived Obesity: A Multilevel Analysis of a Nationally Representative Sample of Korean Adults. Sci Rep 8, 7901 (2018). https://doi.org/10.1038/s41598-018-26192-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-018-26192-z
This article is cited by
-
Perception of body size and body dissatisfaction in adults
Scientific Reports (2022)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.