Abstract
Managing endovascular thrombectomy (ET) in diabetic ischemic stroke (IS) with novel anticoagulants is challenging due to putative risk of intracerebral hemorrhage. The study evaluates increased hemorrhagic transformation (HT) risk in Rivaroxaban-treated diabetic rats post ET. Diabetes was induced in male Sprague-Dawley rats by intraperitoneal injection of 60 mg/kg streptozotocin. After 4-weeks, rats were pretreated orally with 30 mg/kg Rivaroxaban/saline; prothrombin time was monitored. IS and ET was induced after 1 h, by thread-induced transient middle cerebral artery occlusion (tMCAO) that mimicked mechanical ET for proximal MCA occlusion at 60 min. After 24 h reperfusion, infarct volumes, HT, blood-brain barrier (BBB) permeability, tight junction at peri-ischemic lesion and matrix metalloproteinase-9 (MMP-9) activity was measured. Diabetic rats seemed to exhibit increased infarct volume and HT at 24 h after ET than normal rats. Infarct volumes and functional outcomes did not differ between Rivaroxaban and diabetic control groups. A significant increase in HT volumes and BBB permeability under Rivaroxaban treatment was not detected. Compared to diabetic control group, neither the occludin expression was remarkably lower in the Rivaroxaban group nor the MMP-9 activity was higher. Together, Rivaroxaban does not increase HT after ET in diabetic rats with proximal MCA occlusion, since Rivaroxaban has fewer effects on post-ischemic BBB permeability.
Similar content being viewed by others
Introduction
Atrial fibrillation (AF) is the most common sustained cardiac arrhythmia encountered clinically1,2. In 2050 there will be an estimated 72 million AF patients in Asia3, with a 5-fold higher risk of ischemic stroke (IS). Embolic cerebral infarction associated with AF can be prevented by oral anticoagulants4. But some anticoagulants such as warfarin increase the risk of intracranial hemorrhage5. The introduction of direct thrombin (Dabigatran)6 and factor Xa inhibitors (Rivaroxaban and Apixaban), known as non-vitamin K antagonist oral anticoagulants (NOACs), are a major breakthrough because they are non-inferior or even superior to warfarin for prevention of stroke and bleeding side effects without monitoring7,8.
NOACs carry a substantially lower risk of intracranial hemorrhage (ICH) than warfarin. A mouse model suggests that doses of Rivaroxaban 30-fold higher than those administered clinically are required to induce intracranial hemorrhage9. Patients with NOAC-associated ICH had smaller ICH volumes and better clinical outcomes compared with warfarin-associated ICH in a small multicenter study10. Recent studies also show no increased risk of hemorrhagic transformation (HT) after IS in normal rats or mice under NOAC treatment, regardless of whether they received tissue-type plasminogen activator treatment or not11,12. But, the most recent clinical studies suggest there are some bleeding risks with Rivaroxaban. Compared to other NOACs and vitamin K antagonists, a retrospective cohort study showed Rivaroxaban was associated with increased gastrointestinal bleeding13. Among NOACs, Rivaroxaban patients have a significantly higher risk of major bleeding than Apixaban14 and Dabigatran patients15,16. So, the risk of HT with Rivaroxaban may be a concern.
Diabetes is an increasingly growing epidemic; patients with diabetes are at a 2–6-fold increased risk of stroke17. 70% patients with recent stroke have overt diabetes or pre-diabetes distinguished by impaired fasting glucose or impaired glucose tolerance18. In addition, diabetes and hyperglycemia predict early neurological deterioration following IS and patients have poorer prognosis than the non-diabetic population19. Pre-stroke hyperglycemia causes infarct expansion, develops greater HT and results in worse clinical outcome due to damage of blood-brain barrier (BBB)17,20,21.
Although intravenous recombinant tissue plasminogen activator (rt-PA) is the standard treatment for acute IS, the narrow time window and strict exclusion criteria limit its applications22. In 2015, a series of clinical trials showed that endovascular thrombectomy (ET) had higher rate of recanalization and good clinical outcome23,24,25. However, diabetes and anticoagulants are also independent predictors for HT after ET, which affect patients’ outcomes26,27. Hitherto, despite the increased risk of HT after ET in patients with diabetes, no data concerning the effects of Rivaroxaban and diabetes on ET in ischemic stroke have been published. Clinical study of NOACs in this subgroup of patients is challenging owing to high technique requirements and perioperative complication risk. The present study used an experimental diabetes and ET model of IS in rats to assess the effect of anticoagulation with Rivaroxaban on the risk of HT and its neurological outcome.
Materials and Methods
Animals
The study was approved by the Animal Care and Experiment Committee of the Ninth People’s Hospital affiliated to the School of Medicine, Shanghai Jiao Tong University [approval No. HKDL(2016)261] and all methods were performed in accordance with the relevant guidelines and regulations. Ninety-six male Sprague-Dawley rats (6–8 weeks, 200–250 g, Slac laboratory animal, Shanghai, China) received water and food without restrictions and were housed in a 12:12 h light/dark cycle at 24 °C with appropriate humidity. Surgeries were performed under isoflurane anesthesia; the suffering was minimized. The ARRIVE guidelines increase the reproducibility and quality of the data28.
Ninety-six rats were divided into 4 groups: Normal group, 18 normal rats (non-diabetic) underwent 1 h transient middle cerebral artery occlusion (tMCAO); Control group, 36 diabetic rats underwent 1 h tMCAO; Rivaroxaban group, 36 diabetic rats received Rivaroxaban treatment 1 h before tMCAO; Sham group, 6 diabetic rats underwent similar operation although with only superficial filament insertion into proximal internal carotid artery.
Type 1 diabetes models
Seventy-eight rats fasted overnight. Diabetes was induced by a single intraperitoneal injection of 60 mg/kg streptozotocin (STZ, Sigma, St Louis MO, USA) dissolved in pH 4.5 citrate buffer, to a final concentration of 10 mg/ml. Diabetes was confirmed 3 days after STZ administration by tail pricking to analyze the blood glucose levels. Animals with random blood glucose concentrations >11.0 mmol/L were considered diabetic and included in the study29.
Drug administration
Four weeks post-establishment of diabetic models, 36 rats received 30 mg/kg Rivaroxaban (Bayer HealthCare AG, Wuppertal, Germany) via gastric gavage 1 h before tMCAO. This dose was determined according to previous studies and a preliminary experiment that tested 3, 10, and 30 mg/kg doses of Rivaroxaban. 30 mg/kg dosage increased the prothrombin time27 by 2- to 3-fold, and this effect was sustained for >4 h9,12. Micronized Rivaroxaban was dissolved in saline at 3 mg/mL. To eliminate effects of trauma caused by the gastric gavage, remaining animals received 10 mL/kg saline via gastric gavage 1 h before operation. The gastric gavage was introduced under brief 3% isoflurane anesthesia30.
Endovascular thrombectomy (ET) models
Because the tMCAO model showed abrupt cerebral blood reperfusion after the thread was mechanically pulled out, it could be used as an ET model31.
All rats were anesthetized with a mixture of nitrous oxide/oxygen/isoflurane (69%:30%:1%) during surgical preparation with an inhalation mask. Focal cerebral ischemia and ET was induced using the tMCAO model as described previously11,32,33. The rats’ body temperature was monitored and maintained at 37.0 ± 0.5 °C by a heating pad during the surgical procedure. The right middle cerebral artery (MCA) was occluded by inserting a 4–0 surgical nylon filament through the common carotid artery. Regional cerebral blood flow (CBF) was continuously monitored under general anesthesia with the probe located 1 mm posterior to the bregma and 5 mm from the midline of a hemisphere, an area comprising the territory of MCA, by laser-Doppler-flowmetry (Periflux system 5000, Perimed, Järfälla, Sweden). A significant drop in CBF indicated successful proximal occlusion of the MCA by the thread head. A similar degree of reduction in CBF was achieved in both Control and Rivaroxaban-treated rats. After 60 min of tMCAO, the nylon thread was gently removed (“endovascular mechanical thrombectomy”). CBF was restored after reperfusion and appeared to be similar in both groups. The anesthesia of all groups lasted until closure of the skin wound on the neck. Buprenorphine Hydrochloride (TIPR Pharmaceutical Responsible Co., Ltd, Tianjin, China) 0.05 mg/kg was injected subcutaneously to relieve post-surgical pain34. The animals were returned to their cages immediately after they had regained consciousness. Rats that died owing to subarachnoid hemorrhage, anesthetic accident or difficulty in inserting the thread were excluded.
Coagulation status
The rats’ coagulation status was determined by measuring Prothrombin time27 with CoaguChekXS (Roche Diagnostics GmbH, Mannheim, Germany). PT was monitored before inserting and after removing the nylon filament.
Neurological deficit
Neurological deficit was assessed using the Bederson and Garcia scales scores35 24 h post-reperfusion and 12 rats per group from the Control and Rivaroxaban group were included. Bederson scale: 0 = no deficit; 1 = flexion of forelimb; 2 = consistent reduction in resistance to lateral push toward the paretic side; 3 = circling toward the paretic side; 4 = fall down to the paretic side; 5 = unable to move spontaneously; 6 = dead. The 18-point Garcia scale includes testing spontaneous activity, symmetry in the movement of four limbs, forepaw outstretching, climbing, body proprioception and vibrissae touch. The observation was performed by a person blinded to the experimental groupings. Rats that died within the observation period were given 0 points in the Garcia scale score.
Preparation of sections and tissue samples
24 h post-ET surgery, animals were anesthetized and transcardially perfused with phosphate-buffered saline (PBS; pH 7.2). The whole brain was removed, 3-mm-thick coronal sections were cut, and stained with 2% 2,3,5-triphenyltetrazoliumchloride (TTC, Sigma, St Louis, MO, USA). Six rats in the Normal, Control, Rivaroxaban group determined the infarct volume that was calculated by the standard method36,37 with an image analysis program (ImageJ, version 1.37 V, NIH, Bethesda, MD, USA), thus correcting edema. The infract volume was expressed as a percentage of the whole contralateral hemisphere.
Infarct volume (%) = [(total cortex volume in the contralateral cerebral hemisphere − noninfarcted cortex volume in the ipsilateral cerebral hemisphere)/total cortex volume in the contralateral cerebral hemisphere] × 100%37.
Quantification of HT
HT volume was measured as follows: a previously published spectrophotometric method measuring hemoglobin concentration and photograph scoring12. However, the hemoglobin concentration results were below the sensitivity of the method, and hence, were not presented. In order to evaluate the HT volume quantitatively, we used image analysis as an alternative38. In brief, regions of hemorrhage were visually identified and outlined manually, and areas were then integrated to yield total volumes. The unstained coronal sections were imaged every 3 mm and evaluated by two independent raters that were masked to group assignment. ImageJ (version 1.37 V, NIH, Bethesda, MD, USA) was used to analyze HT volumes.
Hemorrhage score ranged from 0–to 4: 0 = no hemorrhage; 1 = dispersed individual petechiae; 2 = confluent petechial; 3 = small diffuse hemorrhage or hematoma; 4 = large diffuse hemorrhage or hematoma39. Each of the Normal, Control, and Rivaroxaban group used 12 rats to evaluate HT score.
BBB permeability for Evans Blue (EB)
To quantify post-ischemic BBB permeability, 6 animals each from the Control and Rivaroxaban groups were operated as described above with ET surgery. Animals were briefly reanesthetized 24 h after reperfusion and 2% EB (Sigma, St Louis MO, USA) in saline (4 mL/kg) was injected into the femoral vein. After 2 h, rats were transcardially perfused with PBS and the ipsilateral hemisphere was removed and homogenized in 3 mL formamide. After extraction in 60 °C water for 24 h, the samples were centrifuged at 2000 × g for 20 min. EB concentration of the supernatant was determined at 620 nm (Thermo Scientific BioMate 3S) and quantified as µg of EB/mg tissue using a standard curve40.
Gelatin zymography and western blot
For western blot and gelatin zymography, 6 rats each from the Control, Rivaroxaban, and Sham groups were treated as above. 24 h post-reperfusion, the rats were anesthetized by intraperitoneal injection of chloral hydrate (400 mg/kg) and transcardially perfused with PBS. Brains were removed quickly and divided into ipsilateral–peri-ischemic and contralateral–nonischemic hemispheres. Each hemispheric brain was frozen immediately in dry ice and stored at −80 °C until use.
Gelatin zymography was performed using the frozen brain tissue. Frozen brain samples were homogenized in 10× volume lysis buffer (150 mmol/L NaCl, 1% SDS, 0.1% deoxycholic acid, and 50 mmol/L Tris-HCl; pH 7.4) containing protease inhibitors. The supernatant was collected at 9000 × g for 15 min at 4 °C. The total protein concentration was determined by Bicinchoninic acid kit (Sigma, St Louis MO, USA). The activity of matrix metalloproteinase-9 (MMP-9) in each sample was measured using a gelatin-zymography kit (Xinfan Biotechnology, Shanghai, China) according to the manufacturer’s instructions. Brief, each sample containing 20 μg protein was diluted with the homogenizing buffer in the kit, mixed with an equal volume of sample buffer, and electrophoretically resolved for 2 h. The gels were washed and incubated for 24 h in incubation buffer at 37 °C and stained with Coomassie blue. Quantitative densitometric analysis was performed with ImageJ software.
For occludin levels, 7 μg of total protein extract was electrophoresed on 12% polyacrylamide gels and transferred to a polyvinylidene fluoride membrane (Millipore). The membrane was incubated in 5% skimmed milk in Tris-buffered saline with 0.2% Tween 20 (TBST) at room temperature for 1 h, and probed with primary antibodies overnight at 4 °C: rabbit anti-occludin (1:1000, Abcam) and monoclonal rabbit anti-β-actin was (1:2000, Abcam). The signals were quantified with an Odyssey Infrared Imaging System (LI-COR Biosciences, Lincoln, NE, USA) and analyzed by ImageJ.
Statistical analysis
Statistical analysis was performed by a blinded investigator using IBM SPSS Statistics v.19 (SPSS Inc., Chicago, IL, USA). Values are expressed as mean ± s.d., median (quartile) or rate as appropriate. Mean body weight, blood glucose, PT, neurological scores and EB content were analyzed using unpaired t-test; infarct volumes, occludin levels and the activity of MMP-9 were compared with one-way ANOVA; HT scores and HT volumes were analyzed with Kruskal-Wallis ANOVA; and mortality rate was evaluated by Chi-square test. Differences with a probability value of P < 0.05 were considered statistically significant.
Results
Baseline characteristics
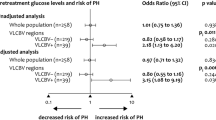
Rats’ body weight was significantly lowered 4 weeks after STZ injection (from 230.45 ± 3.75 g to 199.50 ± 4.23 g of the Rivaroxaban group, P < 0.01; and from 229.89 ± 3.52 g to 197.15 ± 3.86 g of the Control group, P < 0.01). Mean body weight and blood glucose before ET surgery were not significantly different between the Control and Rivaroxaban group (Table 1). CBF immediately declined to <30% of basal levels during tMCAO, which was recovered to basal levels in both groups. There was no significant difference in CBF before tMCAO, during tMCAO, or at reperfusion between the Control and Rivaroxaban groups (Fig. 1). PT was significantly increased in the Rivaroxaban group (15.68 ± 0.45s before tMCAO and 16.59 ± 0.54s after tMCAO, P < 0.01; Table 1).
CBF of diabetic rats during ET surgery. (A) The diabetes and ET tMCAO model in rats. Rats received 60 mg/kg streptozotocin (STZ) intraperitoneally. Four weeks later, the rats received 30 mg/kg Rivaroxaban or saline orally. (B) Laser Doppler measurements during tMCAO surgery in diabetic control rats (n = 33, full line) and Rivaroxaban-treated diabetic rats (n = 33, dash line).
Neurological score and outcomes
The neurological score did not differ significantly in the Rivaroxaban group than the Control group (2.75 ± 0.18 versus 2.64 ± 0.20 for Bederson scale score, P = 0.70; 7.42 ± 0.42 versus 7.93 ± 0.29 for Garcia scale score, P = 0.31; Fig. 2A,B).
No difference in Neurological outcome under Rivaroxaban treatment post-ET. (A) Bederson scale score in 30 mg/kg Rivaroxaban-pretreated rats (n = 12) is 2.75 ± 0.18 and diabetic control rats (n = 12) is 2.64 ± 0.20, without significant difference (unpaired t-test, P = 0.70). (B) Garcia scale score in 30 mg/kg Rivaroxaban-pretreated rats (n = 12) is 7.42 ± 0.42 and diabetic control rats (n = 12) is 7.93 ± 0.29, not significantly different (unpaired t-test, P = 0.31).
Two rats died owing to anesthetic accident and 1 due to subarachnoid hemorrhage in both the Control and Rivaroxaban groups, which were excluded from statistical analysis. The mortality rate of both the Rivaroxaban and Control groups was 9.09% (P = 1.00; Table 1).
Infarct volume and HT assessment
The infarct volumes and HT between the normal, diabetic control and Rivaroxaban-pretreated rats were compared. No statistical significance in infarct volume was found among the three groups (one-way ANOVA, P = 0.07). tMCAO for 1 h led to an ischemic lesion size of 36.04 ± 6.92% of the Rivaroxaban group, which was similar to that of the Control group (34.48 ± 6.90%, P = 0.85). However, diabetic control rats (P = 0.06) and Rivaroxaban-pretreated rats (P = 0.04) showed an increased infarct volume 24 h post-reperfusion than normal rats (17.67 ± 1.76%), although a statistical significance was not reached (Fig. 3A,B).
Diabetic rats show increased infarct volume and HT post-ET than normal rats; Rivaroxaban does not increase infarct volumes and HT scores in diabetic rats post-ET. (A) Representative images showing 2,3,5-triphenyltetrazoliumchloride (TTC) staining for infarct volume in normal rats (n = 6), diabetic control rats (n = 6) and Rivaroxaban-pretreated rats (n = 6). (B) Bar graph depicting infarct volume in all the groups. Ischemic lesion size of the normal group is 17.67 ± 1.76%, the diabetic control group is 34.48 ± 6.90% and the Rivaroxaban group is 36.04 ± 6.92% 24 h after 1 h tMCAO (one-way ANOVA, P = 0.07). (C) Representative images showing visible hemorrhage in normal (n = 12), diabetic control (n = 12) and Rivaroxaban-pretreated rats (n = 12). (D) Macroscopic hemorrhage scored by a masked rater. Individual scores and bars indicate median and range. HT score of normal group, diabetic control group, and Rivaroxaban group is 0 (IQR: 0–0), 1.5 (IQR: 0–2.75), and 1.5 (IQR: 0–3), respectively, at 24 h post-ET surgery. Both the Control and Rivaroxaban groups have higher HT score than the Normal group (*P < 0.05), while the Control and Rivaroxaban group have similar HT score (P = 1.00) (Kruskal-Wallis ANOVA and a Dunn-Bonferroni test for post hoc comparisons). (E) Box-plot depicting HT volume of rats in all the groups. Median of HT volume of the Normal, Control, and Rivaroxaban group group is 0 mm3 (IQR: 0–0 mm3, n = 12), 35.1 mm3 (IQR: 0–241.20 mm3, n = 12) and 76.8 mm3 (IQR: 0–270.53 mm3, n = 12), respectively, at 24 h after 1 h tMCAO. Both the Control and Rivaroxaban groups have larger HT volume than the Normal group (*P < 0.05) while the Control and Rivaroxaban group have similar HT volume (P = 1.00) (Kruskal-Wallis ANOVA and a Dunn-Bonferroni test for post hoc comparisons).
No HT was found in normal rats while 8 of the 12 diabetic control rats and 8 of the 12 Rivaroxaban-pretreated rats displayed HT (P < 0.01). Median HT score of the Control group was 1.5 (IQR: 0–2.75) and that of the Rivaroxaban group was 1.5 (IQR: 0–3) 24 h post-ET surgery. Compared to the Control group, pretreatment with Rivaroxaban (30 mg/kg) did not significantly increase the HT score (P = 1.00; Fig. 3C,D). Image analysis was used to quantitatively evaluate the HT volume in rats because similar to Tejima’s situation38, the type of HT that we observed in the ischemic core was consistently hemorrhagic infarction, not parenchymal hematoma, so we think this method of assessing HT is reasonable. Results of image analysis also showed that HT volume increased significantly in the Control (Median 35.10 mm3, IQR: 0–241.20 mm3, P < 0.05) and Rivaroxaban groups (Median 76.80 mm3, IQR: 0–270.53 mm3, P = 0.03) when compared with the Normal group (Median 0 mm3, IQR: 0–0 mm3), but did not differ significantly between the Control and the Rivaroxaban group (P = 1.00) (Kruskal-Wallis ANOVA followed by Dunn-Bonferroni test; Fig. 3E).
BBB Permeability, occludin level and MMP-9 activity
EB extravasation was similar in the Control (15.67 ± 3.36 μg/mg) and Rivaroxaban groups (16.00 ± 3.18 μg/mg) (P = 0.94) (Fig. 4A,B).
Effects of Rivaroxaban on BBB permeability in rats. (A) Topography and extent of EB extravasation in Rivaroxaban-pretreated (n = 6) and diabetic control rats (n = 6). (B) Bar graph depicting EB extravasation in all the groups. EB extravasation of the Control group (15.67 ± 3.36 μg/mg) and Rivaroxaban group (16.00 ± 3.18 μg/mg) is similar at 24 h post-ET surgery (unpaired t-test, P = 0.94).
Occludin expression level was 0.53 ± 0.04, 0.39 ± 0.02, and 0.34 ± 0.03 respectively in the Sham, Control, and Rivaroxaban groups; compared with the Sham group, occludin was significantly lower in the Control (P < 0.01) and Rivaroxaban groups (P < 0.01); however, the Control and the Rivaroxaban group had similar occludin expression level (P = 0.28) (one-way ANOVA followed by LSD test; Fig. 5A) (Also see Supplementary File).
Effects of Rivaroxaban on occludin expression and MMP-9 activity in rats. (A) A representative western blot showing changes in occludin expression (n = 6 in each group). Both the Control and Rivaroxaban groups have significantly lower occludin expression level than the Sham group (*P < 0.05), while the Control and Rivaroxaban group have similar occludin expression level (P = 0.28) (one-way ANOVA and a LSD test for post hoc comparisons). (B) A representative zymogram showing changes in MMP-9 activity (n = 6 in each group). Both the Control and Rivaroxaban groups have significantly higher MMP-9 activity than the Sham group (*P < 0.05), while the Control and Rivaroxaban group have similar MMP-9 activity (P = 0.08) (one-way ANOVA and a LSD test for post hoc comparisons).
MMP-9 activity was 0.41 ± 0.03, 1.61 ± 0.04, and 1.77 ± 0.09 respectively in the Sham, Control, and Rivaroxaban groups. Both the Control (P = 0.01) and Rivaroxaban groups (P < 0.01) showed significantly higher MMP-9 activity than the Sham group while the Control group and the Rivaroxaban group had similar MMP-9 activity (P = 0.08) (one-way ANOVA followed by LSD test) (Fig. 5B) (Also see Supplementary File).
Discussion
Our study proposes 2 new findings: (1) Rivaroxaban does not increase the risk of HT in experimental cerebral ischemia and ET in diabetic rats. (2) Rivaroxaban does not increase BBB permeability post-ET for proximal MCA occlusion in diabetic rats.
Previous studies used tMCAO rodent model to simulate acute ischemic stroke (AIS) patients with rt-PA recanalization. However, the clinical relevance was questioned due to distinct CBF profiles upon reperfusion between tMCAO (abrupt reperfusion) and alteplase treatment (gradual reperfusion), resulting in differing pathophysiologies. Thus, the tMCAO model is an ET model31.
This and previous studies have consistently demonstrated that anticoagulation with Rivaroxaban will not increase HT with or without thrombolysis in various models of focal cerebral ischemia and recanalization in mice and rats11,12, similar to the human situation41. AHA/ASA AIS guidelines (2015) pointed out that the benefit of ET in stroke patients under anticoagulation is unclear42 and hitherto, only one case of 83-year-old woman treated by both rt-PA and ET under Rivaroxaban treatment was reported43. The author concluded that thrombolysis and/or ET might be safe for patients treated with the new anticoagulant Rivaroxaban. Meanwhile, the safety of Rivaroxaban in diabetic patients is unclear. We, firstly, established a model of diabetes and ET during oral anticoagulation with Rivaroxaban. Herein, we concluded that anticoagulation with Rivaroxaban does not cause an excess risk of HT in diabetes post-ET.
To induce Rivaroxaban-associated ICH, three doses (3, 10, and 30 mg/kg) were used in the preliminary experiment. The results showed that 30 mg/kg could increase the PT by 2–3-fold, and the drug’s action lasted for >4 h. Zhou et al.9 demonstrated a similar phenomenon. Since the dose is >30-fold higher than that in clinical practice44, these findings suggest that even very high doses of Rivaroxaban cannot increase the risk of HT in diabetic rats post-cerebral infarction and ET, and confirmed the safety profiles of this drug.
The emerging neurovascular unit concept underlies the important contribution of cerebral blood vessels to the pathophysiology of stroke45. Cerebrovasculature is susceptible to damage by hyperglycemia19. Vascular injury and potentially subsequent vascular dysfunction in diabetes may be as important as the neuronal injury in determining neurological deficit. Diabetes cerebrovascular remodeling is characterized by increased vessel tortuosity, vascular endothelial growth factor (VEGF) expression, and MMP-2, and -9 activity46. Newly formed or remodeled cerebrovasculature vessels cannot resist the impact of ischemia/reperfusion injury and increased bleeding occurs. In other words, VEGF secretion and angiogenesis led to HT in diabetes. Hollborn et al.47 found that the activated blood coagulation factor Xa induced chemotaxis of retinal pigment epithelial cells and stimulated the release of angiogenic growth factors such as VEGF. So, inhibition of factor Xa may have a direct effect on VEGF secretion and suppress coagulation-induced angiogenesis. It can partially explain our result of no extravagant HT in Rivaroxaban-treated diabetes experimental cerebral ischemia and ET.
Upregulation of MMPs may be a common link between diabetes and IS pathologies. In IS, increased MMP-9 disrupts basal lamina and neurovascular unit structure promoting edema and HT48,49,50. MMP-9 knockout mice are protected against IS19,51. In diabetes, the MMP system is dysregulated and vascular wall integrity may be weakened, setting the stage for an aggravated damage during stroke. Cerebrovascular permeability increases in diabetes because of diabetes-induced damage to the BBB function and/or because of the immature nature of the newly formed vessels52. Tight junction proteins such as occludin and claudin-5 have essential roles in regulating BBB stability53, and endogenous overexpression of MMP-9 in brain endothelial cells results in significant degradation of tight junction proteins occludin and claudin-554. Our result accords with the opinion that MMP-9 expression increases significantly in diabetes post-IS. Furthermore, Rivaroxaban may have little effect on MMP-9 expression. This study also reveals that Rivaroxaban does not increase occludin degradation and has no effect on BBB stability in diabetes post-experimental ET, which is similar to normal experimental stroke models55.
Limitations: In this study, HT was designed to be assessed by a scoring method and spectrophotometric measurement of hemoglobin concentration. However, as the HT in both the experimental and Control groups was hemorrhagic infarction, the optical density could not be detected at such a low level; therefore, the results were not reported here. Ploen et al.12 reported that even treated with rt-PA, the hemoglobin concentration of HT in 30 mg/kg Rivaroxaban-pretreated mice was still very low (0.68 μL). In this situation, we used image analysis as an alternative to evaluate the HT volume quantitatively and also found that HT volume did not differ significantly between the Control and Rivaroxaban group.
Our results provide evidence that Rivaroxaban does not increase HT post-ET in diabetes rats. Fewer effects of Rivaroxaban on post-ischemic BBB permeability may be partially explanatory. The clinical application of NOACs (Rivaroxaban) not only can reduce the incidence of AF-related IS but also may not affect ET treatment once AIS happens.
References
Camm, A. J. et al. Guidelines for the management of atrial fibrillation: the Task Force for the Management of Atrial Fibrillation of the European Society of Cardiology (ESC). Europace. 12, 1360–1420 (2010).
Lip, G. Y., Tse, H. F. & Lane, D. A. Atrial fibrillation. Lancet. 379, 648–661 (2012).
Tse, H. F. et al. Stroke prevention in atrial fibrillation–an Asian stroke perspective. Heart Rhythm. 10, 1082–1088 (2013).
Aguilar, M. I. & Hart, R. Oral anticoagulants for preventing stroke in patients with non-valvular atrial fibrillation and no previous history of stroke or transient ischemic attacks. Cochrane Database Syst Rev. 20, Cd001927 (2005).
Fang, M. C. et al. Death and disability from warfarin-associated intracranial and extracranial hemorrhages. Am J Med. 120, 700–705 (2007).
Connolly, S. J. et al. Dabigatran versus warfarin in patients with atrial fibrillation. N Engl J Med. 361, 1139–1151 (2009).
Patel, M. R. et al. Rivaroxaban versus warfarin in nonvalvular atrial fibrillation. N Engl J Med. 365, 883–891 (2011).
Granger, C. B. et al. Apixaban versus warfarin in patients with atrial fibrillation. N Engl J Med. 365, 981–992 (2011).
Zhou, W. et al. Hemostatic therapy in experimental intracerebral hemorrhage associated with rivaroxaban. Stroke. 44, 771–778 (2013).
Wilson, D. et al. Volume and functional outcome of intracerebral hemorrhage according to oral anticoagulant type. Neurology. 86, 360–366 (2016).
Kono, S. et al. Rivaroxaban and apixaban reduce hemorrhagic transformation after thrombolysis by protection of neurovascular unit in rat. Stroke. 45, 2404–2410 (2014).
Ploen, R. et al. Rivaroxaban does not increase hemorrhage after thrombolysis in experimental ischemic stroke. J Cereb Blood Flow Metab. 34, 495–501 (2014).
Hohnloser, S. H., Basic, E. & Nabauer, M. Comparative risk of major bleeding with new oral anticoagulants (NOACs) and phenprocoumon in patients with atrial fibrillation: a post-marketing surveillance study. Clin Res Cardiol. 106, 618–628 (2017).
Lip, G. Y. et al. Real-world comparison of major bleeding risk among non-valvular atrial fibrillation patients initiated on apixaban, dabigatran, rivaroxaban, or warfarin. A propensity score matched analysis. Thromb Haemost. 116, 975–986 (2016).
Torjesen, I. Bleeding risk higher with rivaroxaban than dabigatran for stroke prevention, head-to-head trial shows. BMJ. 355, i5362 (2016).
Bai, Y., Deng, H., Shantsila, A. & Lip, G. Y. Rivaroxaban Versus Dabigatran or Warfarin in Real-World Studies of Stroke Prevention in Atrial Fibrillation: Systematic Review and Meta-Analysis. Stroke. 48, 970–976 (2017).
Rosamond, W. et al. Heart disease and stroke statistics–2007 update: a report from the American Heart Association Statistics Committee and Stroke Statistics Subcommittee. Circulation. 115, e69–171 (2007).
Kernan, W. N. & Inzucchi, S. E. Type 2 Diabetes Mellitus and Insulin Resistance: Stroke Prevention and Management. Curr Treat Options Neurol. 6, 443–450 (2004).
Baird, T. A. et al. Persistent poststroke hyperglycemia is independently associated with infarct expansion and worse clinical outcome. Stroke. 34, 2208–2214 (2003).
Elgebaly, M. M. et al. Neurovascular injury in acute hyperglycemia and diabetes: A comparative analysis in experimental stroke. Transl Stroke Res. 2, 391–398 (2011).
Ergul, A., Kelly-Cobbs, A., Abdalla, M. & Fagan, S. C. Cerebrovascular complications of diabetes: focus on stroke. Endocr Metab Immune Disord Drug Targets. 12, 148–158 (2012).
Grunwald, I. Q. et al. Endovascular stroke treatment today. AJNR Am. J Neuroradiol. 32, 238–243 (2011).
Berkhemer, O. A. et al. A randomized trial of intraarterial treatment for acute ischemic stroke. N Engl J Med. 372, 11–20 (2015).
Saver, J. L. et al. Stent-retriever thrombectomy after intravenous t-PA vs. t-PA alone in stroke. N Engl J Med. 372, 2285–2295 (2015).
Goyal, M. et al. Randomized assessment of rapid endovascular treatment of ischemic stroke. N Engl J Med. 372, 1019–1030 (2015).
Jiang, S. et al. Predictors of Outcome and Hemorrhage in Patients Undergoing Endovascular Therapy with Solitaire Stent for Acute Ischemic Stroke. PLoS One. 10, e0144452 (2015).
Nogueira, R. G. et al. Predictors and clinical relevance of hemorrhagic transformation after endovascular therapy for anterior circulation large vessel occlusion strokes: a multicenter retrospective analysis of 1122 patients. J Neurointerv Surg. 7, 16–21 (2015).
Kilkenny, C., Browne, W. J., Cuthill, I. C., Emerson, M. & Altman, D. G. Improving bioscience research reporting: the ARRIVE guidelines for reporting animal research. PLoS Biol. 8, e1000412 (2010).
Murunga, A. N. et al. Grapefruit Derived Flavonoid Naringin Improves Ketoacidosis and Lipid Peroxidation in Type 1 Diabetes Rat Model. PLoS One. 11, e0153241 (2016).
Torjman, M. C., Joseph, J. I., Munsick, C., Morishita, M. & Grunwald, Z. Effects of isoflurane on gastrointestinal motility after brief exposure in rats. Int J Pharm. 294, 65–71 (2005).
Sutherland, B. A. et al. The transient intraluminal filament middle cerebral artery occlusion model as a model of endovascular thrombectomy in stroke. J Cereb Blood Flow Metab. 36, 363–369 (2016).
Bohmann, F. et al. No influence of dabigatran anticoagulation on hemorrhagic transformation in an experimental model of ischemic stroke. PLoS One. 7, e40804 (2012).
Liu, J. R. et al. Transient filament occlusion of the middle cerebral artery in rats: does the reperfusion method matter 24 hours after perfusion? BMC Neurosci. 13, 154 (2012).
Jablonski, P., Howden, B. O. & Baxter, K. Influence of buprenorphine analgesia on post-operative recovery in two strains of rats. Lab Anim. 35, 213–222 (2001).
Desland, F. A., Afzal, A., Warraich, Z. & Mocco, J. Manual versus Automated Rodent Behavioral Assessment: Comparing Efficacy and Ease of Bederson and Garcia Neurological Deficit Scores to an Open Field Video-Tracking System. J Cent Nerv Syst Dis. 6, 7–14 (2014).
Gao, D. et al. Resveratrol reduces the elevated level of MMP-9 induced by cerebral ischemia-reperfusion in mice. Life Sci. 78, 2564–2570 (2006).
Chen, C. H. et al. Hydrogen Gas Reduced Acute Hyperglycemia-Enhanced Hemorrhagic Transformation in a Focal Ischemia Rat Model. Neuroscience. 169, 402–414 (2010).
Tejima, E., Katayama, Y., Suzuki, Y., Kano, T. & Lo, E. H. Hemorrhagic transformation after fibrinolysis with tissue plasminogen activator: evaluation of role of hypertension with rat thromboembolic stroke model. Stroke. 32, 1336–1340 (2001).
Kelly-Cobbs, A. I. et al. Targets of vascular protection in acute ischemic stroke differ in type 2 diabetes. Am J Physiol Heart Circ Physiol. 304, H806–815 (2013).
Cao, G. et al. YiQiFuMai powder injection ameliorates blood-brain barrier dysfunction and brain edema after focal cerebral ischemia-reperfusion injury in mice. Drug Des Devel Ther. 10, 315–325 (2016).
Li, W. H. et al. Efficacy and safety of dabigatran, rivaroxaban, and warfarin for stroke prevention in Chinese patients with atrial fibrillation: the Hong Kong Atrial Fibrillation Project. Clin Cardiol. 40, 222–229 (2016).
Powers, W. J. et al. 2015 American Heart Association/American Stroke Association Focused Update of the 2013 Guidelines for the Early Management of Patients With Acute Ischemic Stroke Regarding Endovascular Treatment: A Guideline for Healthcare Professionals From the American Heart Association/American Stroke Association. Stroke. 46, 3020–3035 (2015).
Kimura, S. et al. Revascularization for acute ischemic stroke is safe for rivaroxaban users. J Stroke Cerebrovasc Dis. 23, e427–431 (2014).
Patel, A., Goddeau, R. P. Jr. & Henninger, N. Newer Oral Anticoagulants: Stroke Prevention and Pitfalls. Open Cardiovasc Med J. 10, 94–104 (2016).
Lo, E. H. Experimental models, neurovascular mechanisms and translational issues in stroke research. Br J Pharmacol. 153(Suppl 1), S396–405 (2008).
Li, W. et al. Adaptive cerebral neovascularization in a model of type 2 diabetes: relevance to focal cerebral ischemia. Diabetes. 59, 228–235 (2010).
Hollborn, M. et al. Activated blood coagulation factor X (FXa) induces angiogenic growth factor expression in human retinal pigment epithelial cells. Invest Ophthalmol Vis Sci. 53, 5930–5939 (2012).
del Zoppo, G. J. & Mabuchi, T. Cerebral microvessel responses to focal ischemia. J Cereb Blood Flow Metab. 23, 879–894 (2003).
Fagan, S. C., Hess, D. C., Hohnadel, E. J., Pollock, D. M. & Ergul, A. Targets for vascular protection after acute ischemic stroke. Stroke. 35, 2220–2225 (2004).
Montaner, J. et al. Matrix metalloproteinase expression is related to hemorrhagic transformation after cardioembolic stroke. Stroke. 32, 2762–2767 (2001).
Asahi, M. et al. Effects of matrix metalloproteinase-9 gene knock-out on the proteolysis of blood-brain barrier and white matter components after cerebral ischemia. J Neurosci. 21, 7724–7732 (2001).
El-Remessy, A. B. et al. Neuroprotective and blood-retinal barrier-preserving effects of cannabidiol in experimental diabetes. Am J Pathol. 168, 235–244 (2006).
Hawkins, B. T. & Davis, T. P. The blood-brain barrier/neurovascular unit in health and disease. Pharmacol Rev. 57, 173–185 (2005).
Chen, F., Ohashi, N., Li, W., Eckman, C. & Nguyen, J. H. Disruptions of occludin and claudin-5 in brain endothelial cells in vitro and in brains of mice with acute liver failure. Hepatology. 50, 1914–1923 (2009).
Dittmeier, M., Kraft, P., Schuhmann, M. K., Fluri, F. & Kleinschnitz, C. Pretreatment with rivaroxaban attenuates stroke severity in rats by a dual antithrombotic and anti-inflammatory mechanism. Thromb Haemost. 115, 835–843 (2016).
Acknowledgements
This work was supported by the National Natural Science Foundation of China [No. 81271302 to J.R. Liu, Key Program No. 81530034 to B.Q. Zhao, No. 81271457 to B.Q. Zhao, and No. 81471331 to W.Y. Fan]; Research Innovation Project from Shanghai Municipal Science and Technology Commission [No. 14JC1404300, to J.R. Liu]; Technology Innovation Project of Shanghai Shen Kang Hospital Development Center [No. SHDC12015310, to J.R. Liu]; Project (2015) from SHSMU-ION Research Center for Brain Disorders [No. 2015NKX006, to J.R. Liu]; State Key Laboratory of Medical Neurobiology, Fudan University [No. SKLMN2014002 to J.R. Liu]; Clinical Research Project from Shanghai Jiao Tong University School of Medicine [No. DLY201614 to J.R. Liu]; Project from Shanghai Municipal Education Commission—Gaofeng Clinical Medicine Grant Support [No. 20161422 to J.R. Liu]; and Biomedicine Key Program from Shanghai Municipal Science and Technology Commission [No. 16411953100 to J.R. Liu].
Author information
Authors and Affiliations
Contributions
F.D.L., R.Z., X.Y.F., Y.H.S., Y.L.W. and X.L.S. performed experiments. G.F.L., Y.S.L., Y.Z., X.W.H., M.T.Z. and J.W.Y. analyzed data. F.D.L., J.R.L. and B.Q.Z. designed and interpreted experiments. F.D.L., R.Z., X.Y.F., Y.H.S., J.R.L. and B.Q.Z. wrote the manuscript.
Corresponding authors
Ethics declarations
Competing Interests
The authors declare no competing interests.
Additional information
Publisher's note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Liu, FD., Zhao, R., Feng, XY. et al. Rivaroxaban does not influence hemorrhagic transformation in a diabetes ischemic stroke and endovascular thrombectomy model. Sci Rep 8, 7408 (2018). https://doi.org/10.1038/s41598-018-25820-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-018-25820-y
This article is cited by
-
Modeling blood–brain barrier pathology in cerebrovascular disease in vitro: current and future paradigms
Fluids and Barriers of the CNS (2020)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.