Abstract
Oxaliplatin-based chemotherapy is used to treat patients with esophageal adenocarcinoma (EAC), but no biomarkers are currently available for patient selection. We performed a prospective, clinical trial to identify potential biomarkers associated with clinical outcomes. Tumor tissue was obtained from 38 patients with resectable EAC before and after 2 cycles of oxaliplatin-fluorouracil chemotherapy. Pre-treatment mRNA expression of 280 DNA repair (DNAR) genes was tested for association with histopathological regression at surgery, disease-free survival (DFS) and overall survival (OS). High expression of 13 DNA damage repair genes was associated with DFS less than one year (P < 0.05); expression of 11 DNAR genes were associated with worse OS (P < 0.05). From clinical associations with outcomes, two genes, ERCC1 and EME1, were identified as candidate biomarkers. In cell lines in vitro, we showed the mechanism of action related to repair of oxaliplatin-induced DNA damage by depletion and knockout of protein binding partners of the candidate biomarkers, XPF and MUS81 respectively. In clinical samples from the clinical trial, pre-treatment XPF protein levels were associated with pathological response, and MUS81 protein was associated with 1-year DFS. XPF and MUS81 merit further validation in prospective clinical trials as biomarkers that may predict clinical response of EAC to oxaliplatin-based chemotherapy.
Similar content being viewed by others
Introduction
Esophageal cancer is the sixth most common cancer worldwide, and its incidence has increased markedly in recent decades1,2,3. In North America and Europe, adenocarcinoma is the most prevalent subtype4.
Cisplatin or oxaliplatin-based combination chemotherapy before surgical resection is currently a standard of care for patients with locally advanced, resectable, HER2-negative esophageal adenocarcinoma (EAC), supported by a meta-analysis2 and a Cochrane review. Oxaliplatin-based chemotherapy is as effective as cisplatin-based chemotherapy in advanced esophagogastric cancer, but with lower rates of renal toxicity, neutropenia, alopecia and thromboembolism5,6. It is therefore often preferred for patients with co-morbidities, such as the elderly, where it may be given as doublet chemotherapy rather than triplet7. In combination with radiation, oxaliplatin-based chemo-radiotherapy is as effective as cisplatin-based chemo-radiotherapy and more convenient for patients8.
A concern about offering all resectable patients chemotherapy prior to surgery is our inability to predict which tumors are relatively resistant to treatment and therefore may progress during treatment to become inoperable. We recently showed that major changes can occur in driver mutation presence/frequency in the EAC genome during 2 cycles of oxaliplatin-fluorouracil chemotherapy9. Such changes, and epigenetic alterations, can cause rapid alterations to gene expression10, which are very likely to affect clinical outcomes. Better selection of patients for the appropriate pre-operative therapy could therefore improve survival rates and quality of life for patients with this disease.
As a translational study between clinical trial and the basic science laboratory, we obtained tumor tissue in a prospective clinical trial of oxaliplatin-fluorouracil chemotherapy in patients with operable EAC. The aim of the hypothesis-generating clinical study was to identify DNA damage repair genes that might predict clinical outcomes. This approach identified 2 candidate biomarkers, which we then studied at a mechanistic level in appropriate cell lines in vitro. Building on our previous work showing changes in the EAC genome during chemotherapy, we also compared protein levels of the 2 biomarkers in clinical samples obtained before and after 2 cycles of oxaliplatin-fluorouracil chemotherapy.
Results
Clinical outcomes
Thirty-eight patients with confirmed EAC were recruited and had a full dataset available for analysis (Table 1). At a median follow-up of 21.3 months, 28 patients (57.1%) had died. Kaplan-Meier estimates of median OS and DFS were 23.8 months (95% CI 14.8 to 33.0 months) and 17.8 months (95% CI 7.4 to 27.6 months) respectively, consistent with published studies11,12.
DNA repair gene mRNA expression in clinical samples before and after chemotherapy
High pre-treatment expression of 7 DNAR genes demonstrated a potential association with lack of pathological response (P < 0.05) and 13 DNAR genes were potentially associated with DFS less than one year (P < 0.05) following oxaliplatin-fluorouracil chemotherapy (Table 2). These included two genes known to play an important role in repairing inter-strand cross-links (ICLs) induced by platinum chemotherapies, ERCC1 (log fold-change (FC) −0.624, P = 0.025) and EME1 (logFC −0.573, P = 0.037). Higher levels of expression of 11 DNAR genes were associated with worse OS (Table 2) (P < 0.05), with the most significant relationship per unit increase being for ERCC1 (Hazard Ratio [HR] 3.21; 95% CI [1.55, 6.22]; P = 0.001). None of these results reached significance when adjusted for multiple testing; the data were used for hypothesis testing to identify potential candidate genes using a raw P-value of less than 0.05. No significant associations were found between DNAR genes and pathological T-stage, N-stage, age or sex.
Based on our recent demonstration of major changes in the EAC genome during 2 cycles of oxaliplatin-fluorouracil chemotherapy9, we studied expression of DNAR genes in post-chemotherapy biopsy specimens compared with pre-chemotherapy specimens. We found that expression of 15 DNAR genes was significantly increased following oxaliplatin-fluorouracil (adjusted for multiple testing, P-value < 0.05) (Fig. 1a). These included two genes whose pre-chemotherapy expression levels were associated with worse clinical outcomes: ERCC1 (logFC 0.270, adjusted P = 0.043) (Fig. 1b) and MUS81 (log FC = 0.482, adjusted P = 0.009) (Fig. 1c), the binding partner for EME1 (see below).
Expression of DNA repair genes in EAC tissue following two cycles of oxaliplatin-fluorouracil chemotherapy. (a) Significantly increased expression (P values adjusted for multiple testing <0.05) for log fold-change (FC) of 15 genes including ERCC1 and MUS81. (b,c) Significant changes shown by box and whisker plot for: (b)ERCC1 mRNA expression (logFC 0.270, adjusted P = 0.043); (c)MUS81 mRNA expression (log FC = 0.482, adjusted P = 0.009).
ERCC1 mRNA expression correlates with XPF protein levels in clinical samples
Based collectively on the significant findings outlined above and genes known to play a part in ICL repair, two substrate-specific heterodimeric endonucleases, XPF/ERCC1 and MUS81/EME1, were identified as candidate biomarkers. These proteins have structure-specific activity at junctions between single-strand and double-strand DNA13. Subunits of both endonucleases exhibit interdependent stability, with expression levels of each subunit regulated by its heterodimeric partner14,15. For IHC purposes, the available EME1 and ERCC1 antibodies lack specificity, and do not differentiate active ERCC1 isoforms16. To validate the mRNA expression data for ERCC1 and EME1 at the protein level, we instead used antibodies to XPF and MUS81, having first demonstrated high specificity and validity of these antibodies by Western blot and IHC in XPF and MUS81 siRNA treated cells (Supplementary Figures S1 and S2). Correlation of pre-treatment tumor mRNA expression with XPF and MUS81 protein expression, measured by IHC composite score, showed a statistically significant association between ERCC1 mRNA expression and XPF protein levels (P = 0.041) in the clinical samples.
Association of XPF and MUS81 protein levels with clinical endpoints
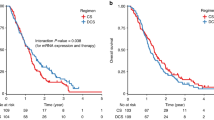
Adjusting for prognostic variables, age, stage and gender, we studied the protein levels of XPF and MUS81 in pre-treatment tumor biopsies to derive potential relationships with clinical outcomes. Typical examples of pre-treatment biopsy staining are shown in Fig. 2a for XPF, and Fig. 2d for MUS81. Low XPF protein levels were associated with pathological response to oxaliplatin-fluorouracil chemotherapy (Fig. 2c) (OR = 3.85, P = 0.049). High MUS81 protein levels were associated with worse 1-year DFS (OR = 5.00, P = 0.04) and worse OS (median 15.5 months vs. not reached, P = 0.013).
XPF and MUS81 protein levels in EAC tissue by immunohistochemistry. (a) Esophageal adenocarcinoma pre-treatment biopsies stained for XPF protein, photographed at x20 magnification; intensity scores (i) 0, (ii) 1, (iii) 2 and (iv) 3. (b) Significant increase in XPF protein levels when pre-treatment biopsies were compared with post-treatment resection samples following 2 cycles of oxaliplatin-fluorouracil chemotherapy (median pre-treatment 2, IQR 0–4; median post-treatment 4.5, IQR 3–6; P = 0.004, Wilcoxon signed rank test). (c) A waterfall plot of the association between pre-treatment tumour XPF level and pathological response following oxaliplatin-chemotherapy. Each line represents the degree of Mandard regression in an individual patient. Patients exhibiting Mandard grades 1–3 were classified as pathological responders; those with Mandard grades 4 and 5 were classified as non-responders10. Low XPF expression was associated with pathological response (odds ratio 3.85, P = 0.041). (d) MUS81 staining of esophageal adenocarcinoma pre-treatment biopsies, photographed at X20 magnification, showing examples of (i) high and (ii) low expression. (e) Trend towards increased MUS81 staining when pre-treatment biopsies were compared with post-treatment resection samples following 2 cycles of oxaliplatin-fluorouracil chemotherapy (median pre-treatment 6, IQR 3–9; median post-treatment 9, IQR 6–9; P = 0.051, Wilcoxon signed rank test).
We also compared XPF and MUS81 protein levels before and after 2 cycles of chemotherapy. As demonstrated for ERCC1 mRNA expression, there was a significant increase in XPF staining (Fig. 2b) (median pre-treatment 2, IQR 0–4; median post-treatment 4.5, IQR 3–6; P = 0.004, Wilcoxon signed rank test). For MUS81, there was a non-significant increase in staining in the post-treatment samples (Fig. 2e).
XPF and MUS81 protein levels in a retrospective surgical cohort
To check whether our findings from the clinical trial cohort related to prediction of response to oxaliplatin-fluorouracil chemotherapy, rather than a prognostic effect, we looked for an association between XPF or MUS81 protein levels and OS in a cohort of patients who received surgery alone for EAC, frequency matched by clinical characteristics to the oxaliplatin-fluorouracil cohort (Table 1). Adjusting for prognostic variables, age, stage and gender, no association was observed between XPF or MUS81 protein levels and OS in the surgery-alone cohort of patients. These data suggest that neither of the proteins studied is a prognostic biomarker for patients with EAC who do not receive platinum-based chemotherapy prior to surgery.
XPF, ERCC1 and MUS81 are not commonly mutated in EAC
Since the mutational statuses of XPF, ERCC1 and MUS81 in EAC have not previously been reported in detail, we performed Whole Exome Sequencing (WES), in samples obtained pre-chemotherapy from 30 patients. No pathogenic somatic mutations were detected. In one patient, there was an increase in somatic copy number of ERCC1 (ratio 1.82). Based on this subset analysis, we speculate that XPF and MUS81 are not commonly mutated in EAC. IHC may therefore represent a suitable means of detecting functional protein levels for this disease.
Cells deficient in XPF or MUS81 protein levels are more sensitive to oxaliplatin treatment
Finally, to obtain mechanistic in vitro corroboration of the observations from the clinical data, we measured the oxaliplatin sensitivity of cell lines deficient in XPF, MUS81 and EME1. Oxaliplatin IC50 measured by cell proliferation assay was up to 3-fold higher in the mock and control transfected cells (P < 0.01), compared with either the XPF-depleted or the MUS81-depleted cell lines (Fig. 3a–d). In genetically altered MUS81 and EME1 variants of the HCT116 cell line, oxaliplatin sensitivity of the parental cell line was more than twofold higher than the MUS81 knockout and EME1 haploinsufficient variants (P < 0.05), confirmed by clonogenic survival assays (Fig. 3e).
Oxaliplatin sensitivity is increased when cancer cells are deficient in MUS81, XPF or EME1. (a–f) siRNA depletion of MUS81 or XPF in two EAC cell lines (a,b) OE33 cells and (c,d) Flo1 cells. In OE33 cells, oxaliplatin IC50 was 2.46 μM (±0.35) in mock-transfected, 2.02 μM (±0.47) in control-transfected, 0.92 (±0.35, P < 0.01) after MUS81 depletion and 0.77 (±0.33, P < 0.01) after XPF depletion. For Flo1, oxaliplatin IC50 was 1.70 μM (±0.47) in the mock- and 1.23 μM (±0.23) in the control-transfected cells, 0.2 (±0.05, P < 0.01) after MUS81 depletion and 0.34 (±0.18, P < 0.01) after XPF depletion. (e) Clonogenic survival of HCT116 colorectal cancer cells is significantly reduced in MUS81 knockout or EME1 haplo-insufficient variants.
Discussion
The development and validation of predictive biomarkers to guide rational selection of pre-operative therapy for individual patients should be a high priority to reduce the frequency with which patients are treated with inappropriate chemotherapy and to improve survival rates for patients with EAC.
In this translational study, tumor mRNA levels of 280 DNA damage repair genes were measured before and after two cycles of oxaliplatin-fluorouracil chemotherapy for 38 patients with EAC. The clinical study was hypothesis-generating, with the aim being to identify DNA repair genes for development as predictive biomarkers for the objective selection of patients for platinum chemotherapy. Unlike retrospective cohort studies limited by the amount of diagnostic material available, particular strengths of this study included the availability of sufficient tissue to obtain a full complement of mRNA scores before and after treatment, WES data for a subgroup of the cohort and validation of two mechanistically justified biomarkers at the protein level.
When association of DNA repair gene expression with clinical endpoints was investigated, high levels of ERCC1 mRNA expression were associated with worse one-year DFS and OS. In order to validate these mRNA expression findings with semi-quantitative protein measurement in matched tissue samples, we attempted to study ERCC1 protein levels by IHC. As previously highlighted, the commercially available anti-ERCC1 antibodies were insufficiently specific and failed to differentiate between isoforms of ERCC1, leading to unacceptable risk of false positive data16. Since XPF/ERCC1 and MUS81/EME1 are heterodimeric endonucleases, with each subunit tightly regulating levels of its binding partner14,15, we demonstrated the specificity of the anti-XPF and anti-MUS81 IHC as surrogates for anti-ERCC1 and anti-EME1. Using this method, we demonstrated a significant relationship between ERCC1 mRNA expression levels and XPF protein levels in our clinical cohort. This is an important finding, justifying the use of XPF IHC as a means of measuring expression of the XPF-ERCC1 heterodimer in clinical samples. High levels of XPF protein were associated with lack of pathological response, and high levels of MUS81 protein were associated with worse DFS and OS.
No association was detected between expression of XPF and prognosis in a matched cohort of patients treated with surgery alone, supporting the potential development of this biomarker as predictive of response to platinum-based chemotherapy. This finding is consistent with a meta-analysis in non-small cell lung cancer patients, which showed that ERCC1 expression is not a prognostic biomarker for patients treated with surgery alone17.
Our results are consistent with previous findings on treatment failure following oxaliplatin-based chemotherapy of EAC. In an important study, Leichman et al. demonstrated an inverse relationship between intra-tumoral ERCC1 mRNA expression and progression-free and overall survival in patients with operable esophageal cancer receiving neoadjuvant oxaliplatin-fluorouracil and radiation therapy18. Our findings suggest that high levels of ERCC1 mRNA are associated with poor DFS and OS in a similar subject group.
MUS81 is an appealing target for cancer therapy on account of its extensive network of synthetic lethalities in preclinical model systems19. Our data are consistent with the known mechanism of action of MUS81 and our corroboration of the mechanism in vitro (Fig. 3). It is currently thought that XPF/ERCC1 is responsible for making the initial incisions that initiate ICL repair, while MUS81/EME1 is utilised to process an intermediate that persists when the XPF-dependent pathway fails20, hence the value of using two levels of the same pathway as mechanistic biomarkers. The inter-dependence between ICL repair pathway proteins is of interest in target discovery to sensitise cancers to platinum therapy as well as in biomarker development for patient selection in which panels of mechanistically selected biomarkers are likely to be superior to single biomarkers used in isolation21.
Polymorphisms of ERCC1 and XPF have been reported in Chinese patients with esophageal cancer, potentially influencing clinical outcomes following platinum-based chemotherapy22,23. We analysed exome sequencing data from 30 patients in our cohort. The somatic sequences observed do not suggest that mutations in XPF, MUS81 and ERCC1 are common in EAC, leading us to conclude that immunodetection of XPF and MUS81 by IHC is a reasonable strategy for detecting protein levels that may impact on repair of platinum-induced DNA damage. In a related study, we showed major changes in mutation presence or frequency could occur in EAC following 2 cycles of pre-operative chemotherapy, and we proposed that these ‘clonal shifts’ could be arise from selection of drug-resistant cancer cells during treatment9. We extended this analysis to the induction of DNA damage repair genes following chemotherapy, and found higher expression of 15 genes, including ERCC1 and MUS81, and higher XPF and MUS81 protein staining. Since we have shown that MUS81 deficiency and XPF deficiency are both associated with sensitivity to oxaliplatin chemotherapy, it is reasonable to speculate that cells within a tumor that have high expression of MUS81 or XPF will have a greater chance to clonally evolve and to survive through treatment. This might explain the significant induction of ERCC1 mRNA and XPF protein following chemotherapy, and similar trends with MUS81. These data indicate the need to monitor the tumor during therapy; it is hoped that developments in circulating tumor biomarkers will allow such monitoring via a blood test in the future.
In conclusion, our translational study has identified 2 DNA damage repair proteins that are potential biomarkers for predicting clinical response to oxaliplatin-fluorouracil chemotherapy. To support this hypothesis, we have combined gene expression data analysis with mechanistic assays of oxaliplatin-induced DNA damage, and we have used IHC to further evaluate the candidate biomarkers identified. We advocate validation of XPF and MUS81 in a large, independent cohort of EAC patients, to enable their development as potential biomarkers to identify patients who will benefit from oxaliplatin-based chemotherapy.
Methods
Patients
The clinical study was approved by the Oxfordshire Regional Ethics Committee and all methods were performed in accordance with the relevant guidelines and regulations, with registrations: prospectively with EudraCT 2005-000834-34 and retrospectively with ISRCTN18146225 (date of assignment 12.10.2017). All participants had World Health Organisation (WHO) performance status 0–2 and provided written informed consent. Recruitment occurred between May 2006 and February 2010. Individuals over the age of 18 with histologically proven invasive cancer of the esophagus or esophagogastric junction (EGJ), as per Union for International Cancer Control (UICC) definition of esophageal cancer (6th edition), but excluding Siewert type III EGJ tumors, were eligible for inclusion. Exclusion criteria included: stage I (T1 N0) disease or any evidence of metastatic disease. See Supplementary Information.
A matched cohort of 54 EAC patients treated with surgery alone between 1997 and 2004 was used to study if either biomarker identified in the study was prognostic in the absence of peri-operative chemotherapy. Patients were frequency matched for age, sex and stage, as shown in Table 1.
Investigations and Treatment
Patients had clinical examination, full blood count and measurement of serum biochemistry at baseline and before each cycle of chemotherapy. Pre-treatment staging was performed by contrast-enhanced computed tomography (CT), 18fluorodeoxyglucose (FDG-) positron emission tomography (PET)-CT, and endoscopic ultrasound. Staging laparoscopy was performed for all patients with tumors involving the esophago-gastric junction, and distal esophageal tumors extending below the diaphragm. Pre-treatment tumor and normal tissue samples (from macroscopically normal squamous epithelium 5–10 cm proximal to the upper limit of visible tumor) were biopsied endoscopically, and samples obtained from surgery in those proceeding to surgical resection. Samples were placed immediately into RNAlater solution, for later RNA extraction, or formalin, for subsequent processing into paraffin blocks, or flash frozen in liquid nitrogen. A strict sampling handling protocol was mandatory, with uniform fixation times, tissue processing and storage conditions for all samples in the study.
Patients received two cycles of oxaliplatin-fluorouracil chemotherapy. A cycle of treatment lasted 21 days and consisted of oxaliplatin (130 mg/m2 IV) on day 1, followed by fluorouracil (1000 mg/m2/day IV) on days 1–4. Restaging was performed by 15F-FDG PET-CT. Patients who did not progress to become inoperable were operated on 4–6 weeks after completion of chemotherapy. Pathological response was determined using the histological grading of tumor regression described by Mandard24. All slides were independently reviewed by two specialist gastrointestinal pathologists, with 96% concordance25.
RNA quantification
Gene expression was measured in the tumor biopsies and post-surgical resection samples. RNA was extracted using the Qiagen AllPrep DNA/RNA Micro Kit (Qiagen Inc., Valencia, CA) following the manufacturer’s instructions. RNA purity was verified via NanoDrop spectrophotometer (Thermo Fisher Scientific, Waltham, MA). Extracted mRNA samples were hybridised to Illumina HumanHT-12-v3 Expression BeadChips (Illumina, San Diego, CA). Raw gene expression data was processed using Illumina GenomeStudio software (v1.6) to generate expression intensities which were considered in a logged base 2 scale. Data were then analysed using R statistical software (v2.15) (http://www.Rproject.org) (R development Core Team, 2012) with BioConductor packages (Gentleman et al., 2004), limma (v3.12.3)(Smyth, 2005), vsn (v3.24) and survival (v2.36.13), for microarray analyses and SPSS software version 19.0 (IBM Inc., Armonk, NY, USA) for all other analyses. A P-value of <0.05 was considered statistically significant. Differential expression between the experimental groups was assessed by generating relevant contrasts corresponding to the two-group comparison. Hazard ratios for OS and DFS according to gene expression level were calculated using Cox regression (see Statistical methods section below). For functional pathway analysis, the Gene Set Analysis (GSA) R package was used to determine the significance of pre-defined sets of genes (the biocarta gene sets) with respect to outcome variables. Finally, a hypothesis-driven approach was undertaken and validation focused on the differentially expressed genes amongst 280 genes belonging to DNA damage repair pathways expected to be relevant for the treatment response (Supplementary Table S1).
Immunohistochemistry
Immunohistochemistry (IHC) was carried out using the Leica Bond-Max automated immunostainer (Leica Microsystems, Wetzlar, Germany), using the manufacturer’s protocol. IHC was conducted on 5 μm sections cut from paraffin-embedded biopsies, stained with mouse anti-XPF (clone SPM228) at 1:200 dilution or mouse anti-MUS81 (clone MTA30 2G10/3) at 1:1000 dilution, both from Abcam, Cambridge, MA). Antibodies to XPF, MUS81 and ERCC1 (Santa Cruz sc-17809) were tested for specificity using cell pellets depleted for XPF or MUS81 protein by siRNA interference (Supplementary Figures S1 and S2). For XPF measurement, two independent assessors scored staining semi-quantitatively via a score relating nuclear staining intensity and the percentage of stained nuclei. For MUS81, high expression was defined by a median cutoff, greater than 10% of nuclei staining with high intensity. Further details available in Supplementary Information.
Whole exome sequencing
Thirty EAC patients were prioritized for whole exome sequencing (WES) on the basis of pathological response, disease free survival (DFS) and overall survival (OS) at 2 years, performed as previously described9.
Cell lines and in vitro experiments
Colorectal cancer cell line HCT116 and isogenic variants (MUS81 null and EME1 haplo-insufficient)25 were provided by Prof. Kiyoshi Miyagawa (University of Tokyo, Japan). Esophageal cell lines OE33 and Flo1 were obtained from ECACC. For siRNA depletion, cells were treated 96 and 48 hours prior to plating using ON-TARGETplus siRNA (GE Lifesciences, Dharmacon, USA) to MUS81 and XPF, and Lipofectamine® RNAiMAX transfection reagent (Thermofisher), following manufacturers’ instructions (full details in Supplementary Information).
Statistical methods
For definitions of disease-free survival (DFS) and overall survival (OS), see Supplementary Information. Individuals were censored at the last date they were known to be alive and disease-free (DFS), or alive (OS). Kaplan-Meier curves were calculated for DFS and OS. Due to the relatively small number of individuals in the study and in order not to exclude potentially useful candidate genes, analyses of the relationship between pre-treatment gene expression levels and clinical outcomes were not corrected for multiple testing. Individual gene expression was tested for association with pathological response, one year DFS and OS, and a P-value of <0.05 was considered statistically significant. For comparison of pre- and post- treatment gene expression, P-values were adjusted for multiple testing using the Benjamini and Hochberg (1995) procedure26.
Novelty and impact
We performed a translational clinical trial to discover biomarkers for esophageal adenocarcinoma (EAC) patients who are likely to benefit from oxaliplatin-based chemotherapy. Through mRNA expression profiling, we identified DNA repair genes associated with clinical outcomes. Two novel biomarkers were identified and studied by immunohistochemistry of clinical samples and mechanistic studies in cancer cell lines. These biomarkers merit further validation in prospective clinical trials in patients with EAC.
References
Ferlay, J. et al. Estimates of worldwide burden of cancer in 2008: GLOBOCAN 2008. Int J Cancer. 127, 2893–917 (2010).
Sjoquist, K. M. et al. Survival after neoadjuvant chemotherapy or chemoradiotherapy for resectable oesophageal carcinoma: an updated meta-analysis. Lancet Oncol. 12, 681–92 (2011).
Jemal, A. et al. Global cancer statistics. CA Cancer J Clin. 61, 69–90 (2011).
Kamangar, F., Dores, G. M. & Anderson, W. F. Patterns of cancer incidence, mortality, and prevalence across five continents: defining priorities to reduce cancer disparities in different geographic regions of the world. J Clin Oncol. 24, 2137–50 (2006).
Cunningham, D. et al. Capecitabine and oxaliplatin for advanced esophagogastric cancer. N Engl J Med. 358, 36–46 (2008).
Al-Batran, S. E. et al. Phase III trial in metastatic gastroesophageal adenocarcinoma with fluorouracil, leucovorin plus either oxaliplatin or cisplatin: a study of the Arbeitsgemeinschaft Internistische Onkologie. J Clin Oncol. 26, 1435–42 (2008).
Sylvie, L. et al. Impact of age on the feasibility and efficacy of neoadjuvant chemotherapy in patients with locally advanced oesophagogastric cancer. Eur J Cancer. 51, 1918–26 (2015).
Conroy, T. et al. Definitive chemoradiotherapy with FOLFOX versus fluorouracil and cisplatin in patients with oesophageal cancer (PRODIGE5/ACCORD17): final results of a randomised, phase 2/3 trial. Lancet Oncol. 15, 305–14 (2014).
Findlay, J. M. et al. Differential clonal evolution in oesophageal cancers in response to neo-adjuvant chemotherapy. Nat Commun 7, 11111 (2016).
Krushkal, J. et al. Concerted changes in transcriptional regulation of genes involved in DNA methylation, demethylation, and folate-mediated one-carbon metabolism pathways in the NCI-60 cancer cell line panel in response to cancer drug treatment. Clin Epigenetics. 8, 73 (2016).
Medical Research Council Oesophageal Cancer Working Group. Surgical resection with or without preoperative chemotherapy in oesophageal cancer: a randomised controlled trial. Lancet. 359, 1727-33 (2002).
Ychou, M. et al. Perioperative chemotherapy compared with surgery alone for resectable gastroesophageal adenocarcinoma: an FNCLCC and FFCD multicenter phase III trial. J Clin Oncol. 29, 1715–21 (2011).
Ciccia, A., McDonald, N. & West, S. C. Structural and functional relationships of the XPF/MUS81 family of proteins. Annu Rev Biochem. 77, 259–87 (2008).
Forment, J. V., Blasius, M., Guerini, I. & Jackson, S. P. Structure-specific DNA endonuclease Mus81/Eme1 generates DNA damage caused by Chk1 inactivation. PloS One. 6, e23517 (2011).
Hatch, S. B. et al. XPF protein levels determine sensitivity of malignant melanoma cells to oxaliplatin chemotherapy: Suitability as a biomarker for patient selection. Int J Cancer. 15, 1495–503 (2013).
Friboulet, L. et al. ERCC1 isoform expression and DNA repair in non-small-cell lung cancer. N Engl J Med 368, 1101–10 (2013).
Hubner, R. A., Riley, R. D., Billingham, L. J. & Popat, S. Excision repair cross-complementation group 1 (ERCC1) status and lung cancer outcomes: a meta-analysis of published studies and recommendations. PLoS ONE. 6, e25164 (2011).
Leichman, L. P. et al. S0356: a phase II clinical and prospective molecular trial with oxaliplatin, fluorouracil, and external-beam radiation therapy before surgery for patients with esophageal adenocarcinoma. J Clin Oncol. 29, 4555–60 (2011).
Wu, F. et al. Down-regulation of Mus81 as a potential marker for the malignancy of gastric cancer. Anticancer Res. 30, 5011–4 (2010).
Zhang, J. & Walter, J. C. Mechanism and regulation of incisions during DNA interstrand cross-link repair. DNA Repair (Amst). 19, 135–42 (2014).
Mulligan, J. M. et al. Identification and validation of an anthracycline/cyclophosphamide-based chemotherapy response assay in breast cancer. J Natl Cancer Inst. 106, djt335 (2014).
Liu, Y. et al. XPF-673C>T polymorphism effect on the susceptibility to esophageal cancer in Chinese population. PLoS One. 9, e94136 (2014).
Rumiato, E. et al. ERCC1 C8092A (rs3212986) polymorphism as a predictive marker in esophageal cancer patients treated with cisplatin/5-FU-based neoadjuvant therapy. Pharmacogenet Genomics. 23, 597–604 (2013).
Mandard, A. M. et al. Pathologic assessment of tumor regression after preoperative chemoradiotherapy of esophageal carcinoma. Clinicopathologic correlations. Cancer. 73, 2680–6 (1994).
Hiyama, T. et al. Haploinsufficiency of the Mus81-Eme1 endonuclease activates the intra-S-phase and G2/M checkpoints and promotes rereplication in human cells. Nucleic Acids Res. 34, 880–92 (2006).
Benjamini, Y. & Hochberg, Y. Controlling the False Discovery Rate - a Practical and Powerful Approach to Multiple Testing. Journal of the Royal Statistical Society. 57, 289–300 (1995).
Acknowledgements
This work was supported by the Wellcome Trust [075491/Z/04], NIHR Biomedical Research Centre Oxford, Oxford University Clinical Academic Graduate School, NIHR University College Hospitals Biomedical Research Centre and the CRUK ECMC. We thank the High-Throughput Genomics Group at the Wellcome Trust Centre for Human Genetics (funded by Wellcome Trust grant reference 090532/Z/09/Z and MRC Hub grant G0900747 91070) for the generation of the sequencing data.
Author information
Authors and Affiliations
Contributions
T.P.M., R.S.G., N.D.M., M.R.M., P.J.M. and R.A.S. conceived and designed the translational study. M.R.M., R.S.G. and N.D.M. recruited and treated patients in the clinical trial. J.M.F., C.K., F.C.G., N.S., J.B.C., I.T. and F.B. were responsible for interpretation of expression and exome sequencing data and all the statistical analyses. T.P.M., L.M.W., R.C. and R.C. performed the immunohistochemistry and analysis of staining. T.P.M., R.C., J.M.F., P.J.M., M.R.M. and R.A.S. wrote the manuscript and discussed it with all co-authors before they all approved the final version.
Corresponding author
Ethics declarations
Competing Interests
The authors declare no competing interests.
Additional information
Publisher's note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
MacGregor, T.P., Carter, R., Gillies, R.S. et al. Translational study identifies XPF and MUS81 as predictive biomarkers for oxaliplatin-based peri-operative chemotherapy in patients with esophageal adenocarcinoma. Sci Rep 8, 7265 (2018). https://doi.org/10.1038/s41598-018-24232-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-018-24232-2
This article is cited by
-
Molecular mechanisms associated with chemoresistance in esophageal cancer
Cellular and Molecular Life Sciences (2022)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.