Abstract
Intimate partner violence (IPV) and HIV are highly prevalent worldwide among MSM. However, the association between IPV and HIV seroconversion is virtually unknown. This 12-month prospective cohort study was conducted among MSM in Shenyang, China to explore the causality between IPV and the incidence of HIV. Adjusted Hazard Ratios (aHRs) of HIV acquisition were derived from a multivariate time-dependent Cox model and applied to calculate population attributable fractions (PAFs). Among 476 HIV-negative MSM subjects, 89(18.7%) reported being victims of IPV in the past 3 months (P3M). IPV was significantly correlated with lower education, having more condomless anal intercourse (CAI) and being depressed (each P < 0.05). The incidence of HIV among IPV victims was 11.3/100 PY compared to 3.8/100 PY in non-IPV-victims. Furthermore, IPV victimization was independently associated with HIV seroconversion (aHR = 4.1, PAF = 37.9%). Other predictors for seroconversion included non-local residence in Liaoning province (aHR = 3.9, PAF = 45.2%), engaging in condomless receptive anal intercourse (CRAI)(aHR = 3.1, PAF = 24.2%) or CAI with casual male partners (aHR = 3.8, PAF = 26.3%) in the P3M and syphilis infection (aHR = 4.7, PAF = 33.7%) (each P < 0.05). IPV increased the HIV seroconversion risk of MSM, with a high PAF. HIV prevention programs should integrate IPV screening and intervention, and MSM affected by IPV need to be preferentially enrolled in pre-exposure prophylaxis.
Similar content being viewed by others
Introduction
Globally, men who have sex with men (MSM) population continue to disproportionately suffer from HIV1,2,3,4. MSM are also currently the group with fastest growth in the HIV epidemic occurring in China. The proportion of new HIV cases nationwide in China due to male homosexual contact each year has increased from 12.2% in 20075 to 26.4% in 20166. This indicates that some risk factors that fuel the rapid spread of HIV among Chinese MSM are still not well controlled.
HIV transmission events can occur in various social contexts, and therefore, social factors are core elements that may affect HIV vulnerability, transmission and the impact of behavioral prevention programs. However, few HIV prevention programs address these issues, especially for MSM, due to the very limited available data on these topics in comparison to the substantial number of investigations conducted regarding their risky sexual behavior7,8,9,10. Intimate partner violence (IPV) is one prominent social factor that is highly prevalent in many communities and is linked to more mortality and a higher burden of several other diseases among the general population. It is defined as the continuum from a single episode of violence to ongoing battering within a close relationship11. IPV has been associated with a higher prevalence of HIV, particularly among heterosexual females12,13. Recent work has hinted that MSM may have a similar or higher prevalence of IPV compared with the heterosexual population. The National Violence Against Women Survey (NVAWS) in the United States showed that the lifetime prevalence of physical IPV was 25% in MSM compared to 8% in heterosexual males and 21% in females14. Studies on MSM in Shanghai, China revealed that approximately 40% of MSM had experienced IPV during their lifetime15,16.
Although the causality between IPV and HIV infection has been well-established in the female population, this does not mean that it also applies equally to MSM. There is a distinctive difference in the sexual behaviors, physiology, and cultural features of MSM and heterosexual females. However, little is known globally about the effects of partner violence on the HIV epidemic in the MSM population. Literature on this topic mainly originates from cross-sectional studies conducted in developed Western countries, which observed associations between IPV and HIV high-risk practices (e.g., condomless anal intercourse [CAI], substance abuse) and the prevalence of HIV in MSM17,18,19,20,21,22,23,24. Two studies conducted in China found that MSM that report IPV were more likely to engage in CAI and had a higher prevalence of HIV15,25. However, the causality between IPV and HIV infection could not be established because of its cross-sectional study design. One single longitudinal study on MSM in the United States reported a long-term direct relationship between lifetime IPV and HIV seroconversion during a 5-year follow-up26. In most circumstances, IPV among MSM is a time-varying determinant that may change as a result of changes in partners or partner dynamics27. To understand the causality between IPV and HIV, it is more rational and feasible to shorten the monitoring interval of IPV and to analyze it as a time-dependent determinant by examining the correlation between a recent IPV experience and HIV seroconversion.
The contribution of a risk factor to a disease is usually quantified using a population attributable fraction (PAF). A PAF is interpreted as the proportional reduction in population disease risk that would occur if exposure to a specific risk factor were reduced to an alternative ideal exposure scenario. Hence, a risk factor with a higher PAF would require greater intervention. However, nothing is known about the PAF of IPV for the incidence of HIV in MSM, and this knowledge gap has made it more difficult to prioritize intervention strategies.
One important component in the implementation of a comprehensive HIV prevention strategy is to not only gain an understanding of the role of recent IPV victimization in HIV incidence for MSM but also to quantitatively assess the effects of IPV on new HIV infections. To that end, the purposes of this prospective cohort study were (1) to investigate the prevalence of IPV in a sample of MSM in Shenyang, China in order to explore possible relationships between IPV and other risk factors and the incidence of HIV in these men and (2) to estimate and compare the new HIV infection risk attributable to IPV and other risk factors by calculating PAFs.
Results
Baseline participant characteristics
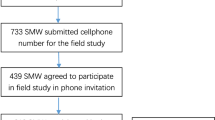
As shown in Fig. 1, a total of 507 MSM attended our baseline-screening survey. Of these, 476 baseline HIV negative MSM were included in the longitudinal survey.
At baseline, eligible MSM subjects were relatively young, with a median age of 28.0 (IQR: 24.0–34.0) years old. Approximately two-fifths of the participants had received at least a college education, and 64.3% were single. Approximately 40% of participants reported having had multiple male casual male sex partners, 20.2% had CAI with male casual partners and 22.0% reported engaging in CRAI in past three months. The baseline seroprevalence of syphilis was 12.2%. The detection rate of symptoms of depression (CES-D score ≥ 15) was 37.2%.
The prevalence of IPV and its associated factors
In the three months prior to enrollment, nearly one-fifth (18.7%) of our MSM participants reported that they had been subjected to IPV from male partners. Specifically, 9.9% had been a victim of physical IPV, 13.7% had been victimized by psychological IPV including threats and emotional abuse, and 9.5% were victims of sexual IPV (Table 1).
After adjusting for background variables including age, monthly income and marital status, MSM who had been victims of IPV in the P3M were more likely to be less-educated (high school and below) (aOR = 1.8, 95%CI = 1.1–3.0), to have CAI in the P3M (CIAI with male partners: aOR = 1.8, 95%CI = 1.1–2.9; CAI with regular male partners: aOR = 1.8, 95%CI = 1.1–3.0) and suffer from symptoms of depression (aOR = 2.8, 95%CI = 1.7–4.5) (each P < 0.05) (Table 2).
HIV seroconversion and its qualitative correlation with IPV and other factors
A total of 476 MSM were recruited in this cohort, of which 437 (91.8%) were retained. Sixteen had HIV seroconversion events during a 299.5 person-year (PY) follow-up, with a calculated total incidence of 5.3 (95%CI: 3.1–8.5) /100 PY. The HIV incidence was 11.3 (95%CI: 4.7–21.9) /100 PY in MSM who had been victims of IPV in the P3M compared to 3.8 (95%CI: 1.7–7.1)/100 PY in those MSM who had not experienced IPV.
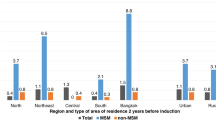
Table 3 shows the risk factors associated with HIV seroconversion in a multivariate Cox analysis after controlling for background variables including age, education level, monthly income and marital status. As shown in the radar chart (Fig. 2), our multivariate analysis showed that individuals who had been subjected to IPV in the P3M were more likely to seroconvert to HIV (aHR = 4.1, 95%CI = 1.5–11.6), with a PAF of 37.9%, a value that was higher than that of most other behavioral risk factors. In addition to IPV, we also identified the following as risk factors for HIV seroconversion (each p < 0.05): non-local residence in Liaoning province (aHR = 3.4, 95%CI = 1.4–10.5; PAF = 45.2%), CAI with casual male partners in the P3M (aHR = 3.8, 95%CI = 1.2–3.2; PAF = 26.3%), CRAI with male partners in the P3M (aHR = 3.1, 95%CI = 1.1–9.3; PAF = 24.2%), and syphilis infection (aHR = 4.7, 95%CI = 1.6–13.5; PAF = 33.7%). Furthermore, having had ≥2 casual male partners had a marginally significant association with HIV seroconversion (aHR = 2.9, 95%CI = 1.0–8.4, p = 0.051). There was no significant difference between specific types of IPV (i.e., physical violence, or psychological violence and sexual violence) (P > 0.05) (data not shown).
Discussion
As far as we are aware, this is the first prospective cohort study to explore the causal pathway between a recent IPV experience and HIV incidence among the MSM population. Our results suggest that being a recent victim of IPV was an independent determinant of HIV seroconversion among MSM in China (aHR = 4.1). Additionally, IPV had a higher PAF for HIV seroconversion (37.9%) than other traditional behavioral risk factors, such as CAI with casual male partners (26.3%) and CRAI with male partners (24.2%). Thus, our results confirm the findings of previous cross-sectional surveys20,24,25 and add to the existing literature by quantitatively characterizing and comparing the PAFs of IPV and other traditional behavioral risk factors for HIV seroconversion. This is important because if we want to control the spread of the HIV epidemic among MSM by adopting a comprehensive intervention strategy, this intervention must address IPV factors in male-to-male relationships.
This cohort study supports a causal pathway from recent IPV to new HIV infection. The relationship presented in this study is coherent. To control for potential time-dependent confounders, we selected a relatively shorter follow-up interval or recall period to define partner violence, captured exposure changes during follow-up, and performed a Cox model to analyze IPV and other behaviors as time-dependent covariates in order to account for time-dependent confounding. We demonstrate that being a recent victim of IPV during the follow-up period was an important contributor to the increased incidence of HIV among MSM. This is in accordance with a previous finding that experiencing IPV during one’s lifetime was associated with a subsequent HIV infection26. It also confirms that IPV is an important predictor of HIV incidence, with both short-term and long-term effects, and more emphasis needs to be put on mitigating its negative impact on the HIV epidemic in the MSM population.
Moreover, our research further quantitatively assessed and compared the effects of IPV and other predictors of the burden of HIV incidence in MSM. A total of 37.9% of incident HIV infection could be attributed to recent IPV victimization, which is higher than the corresponding value estimated in heterosexual women from high prevalence areas of both HIV and IPV (South Africa: PAF = 11.9%, Uganda: PAF = 22.2%)12,28. This implies that interventions aimed at effectively controlling violence in the MSM population would achieve a better reduction in the incidence of HIV than in heterosexual populations. Compared with the traditional behavioral risk factors detected in this study, we also found that a higher PAF was associated with recent victimization of IPV. This indicates that violence has a greater impact on HIV seroconversion than traditional behavioral predictors in MSM. These findings illustrate that IPV prevention may be a highly cost-effective strategy for controlling the ever-increasing HIV epidemic in MSM, and a comprehensive HIV intervention strategy that includes IPV evaluation and intervention must be established to control the spread of HIV in the MSM community.
In addition to IPV, traditional predictors such as CAI, male sexual partner concurrency and syphilis infection remained important contributors to the incidence of HIV in our MSM subjects. Although other studies have confirmed their negative impact on the HIV epidemic29,30,31, our data also highlight behavioral interventions that would be the most beneficial in the MSM population to curb the spread of HIV. Our study also observed a positive link between migrant MSM and the incidence of HIV, i.e., migrants may lack social support and their MSM subpopulation lacks access to the healthcare system, making them a high risk group32,33. It will be important to determine whether this subpopulation also suffers from a higher rate of IPV in the future.
At baseline, we found that about one-fifth of MSM subjects in this study were victims of IPV in the past 3 months, with a prevalence of physical IPV of 10.0%, psychological IPV of 13.7% and sexual IPV of 9.5%. These values are somewhat higher than what were previously reported with respect to recent IPV experiences among MSM. For example, the reported prevalence of experiencing either physical or sexual IPV was only 7.3% among American MSM couples in the past 3 months34. One six-country multicenter study on MSM revealed the prevalence of sexual IPV in the past year ranged from 2.5% to 4.5%35. Although there is a lack of available comparison data on recent IPV experiences in China, a previous survey of MSM in Shanghai reported that approximately 40% MSM had experienced some form of IPV during their lifetime15,16. These results seem to indicate that MSM in China experience a higher level of violence, and therefore public health departments should cooperate with the public security department to strengthen IPV screening and develop professional skills to collect IPV information from this vulnerable population.
Furthermore, our findings showed that victims of IPV are more likely to be involved in sexual risk-taking and to suffer from depression. These could be important contributors to the causal pathway from IPV to HIV infection identified in this study. In our MSM cohort, IPV victims had a lower education level, which is similar to what was observed among heterosexual women and MSM in Western countries36,37,38. A lower education level may be a barrier to social, economic, and healthcare resources, leading to an elevated vulnerability to IPV as well as HIV infection36,39,40,41. Additionally, our findings are consistent with peer studies that show that victims are more likely to be engaging in CAI15,22,42,43. We also found that IPV victims seemed more likely to find their sexual partners over the internet. MSM who were recruited via the internet are more likely to encourage high-risk sexual behaviors44,45,46. These risky behaviors could increase the risk of acquiring HIV among IPV victims. Moreover, our findings are consistent with previous studies from western countries that victims of IPV are more likely to suffer from symptoms of depression18,47,48. Men in a violent relationship who are being victimized and suffer from symptoms of depression might encounter difficulties in seeking help to end the relationship, or their turbulent relationships may make them poorly compliant with prescribed treatment. This finding could partially explain the important role of IPV as a significant contributing factor to HIV acquisition among MSM. It may also support the hypothesis that IPV health professionals that offer traditional behavioral strategies combined with psychiatric help might have a greater potential effect than those working with victims in isolation.
Although IPV was shown to be an important contributing factor to the HIV epidemic among MSM, the current support services and interventions for MSM are still inadequate49. For this reason, replicating this association in the context of trials capable of assessing effective prevention strategies should be a priority. First, given the higher level of risky sexual behaviors among victims of IPV, traditional behavioral intervention strategies need to incorporate IPV. The value of combined prevention strategies has been shown to be effective in the general population of Uganda50. Second, in recent years, many studies have shown that bio-medical prevention, in particular PrEP combined with HIV prevention, could reduce the risk of acquiring HIV among MSM and other high-risk populations51,52. Hence, the popular PrEP strategy may be a good candidate strategy for reducing the risk of HIV among MSM who are affected by IPV. Third, it is essential to establish and improve IPV support services for the MSM population to help IPV victims terminate a troubled relationship as soon as possible. IPV has been said to be a barrier to HIV disclosure53, and therefore may increase the risk of HIV transmission. Finally, it will also be necessary to change the social attitudes, beliefs, and cultural norms that support IPV54,55.
This study has the following strengths; it is the first prospective cohort study to examine the causal relationship between recent IPV to HIV seroconversion in the MSM population. We also quantitatively calculated the effect of IPV on HIV seroconversion by estimating the PAF, which can help public health workers to better understand the extent of IPV’s influence on HIV. Our cohort retention rate was high, owing to multiple measures taken to maintain participant compliance during follow-up. We used Cox proportional hazard models and analyzed time-dependent covariates to better understand the influence of IPV on HIV incidence among MSM.
This study also has some limitations. Since IPV is a sensitive subject for study participants, we cannot rule out the possibility of a social desirability bias through self-reporting measures. It may not be possible to generalize these results to other MSM populations in other countries or regions because the recruitment occurred only in Shenyang, China. Although we followed this cohort for a relatively long time (12-months), a longer observation period would have been beneficial to further confirm our findings. We did not collect the lifetime IPV experiences among MSM. The results of this study found a significantly higher incidence of HIV among MSM who were victims of IPV, but whether this phenomenon could be observed in the perpetrators of IPV in this population will need to be verified in future studies. Out of consideration for the direction of this study, we did not deeply explore the formation of the internal social psychology of IPV among MSM, which will be an important direction for future research.
In conclusion, in addition to conventional high-risk behaviors, being a recent victim of IPV was an important contributor to HIV seroconversion in our MSM population. IPV also seemed to increase the risk of CAI and depression. Therefore, addressing IPV should be a priority during HIV intervention. HIV prevention strategies need to become more sophisticated and should incorporate IPV screening followed by effective intervention. In the subgroup of MSM affected by IPV, it is also essential to pursue bio-medical prevention (including PrEP) in order to reduce their risk of acquiring HIV. It should be a priority to establish and improve the support services for IPV victims and to give them advice on how to terminate an unhealthy, potentially life-threatening relationship.
Methods
Ethic Statement
This study was approved by the Institutional Review of the First Affiliated Hospital of China Medical University, and research procedures were carried out strictly in accordance with relevant guidelines. Written informed consents were obtained from each participant prior to their interview and blood collection. To ensure privacy, every participant was uniquely assigned an identification code (PID) instead of his real name during the survey to link their questionnaire and laboratory testing results.
Study design and enrollment
From January 1st until December 31st, 2014, an open cohort enrollment of HIV-negative MSM was implemented in Shenyang city in Northeast China, which with an estimated 140,000 MSM has the second-largest population of MSM in China after Beijing56. Recruitment was performed in two ways: (1) Venue-based sampling: with the help of the Shenyang Sunshine Working Group, a local MSM non-government organization (NGO), eligible MSM were recruited from suitable venues (e.g., MSM parks, bars, clubs and bathhouses); (2) Peer referrals: MSM were encouraged to recruit their MSM friends or peer male partners to take part in this survey.
Inclusion criteria included the following: (1) HIV serologic negativity; (2) biologically male; (3) 18 years of age or older; (4) self-reported admission of having anal intercourse with male partners within the past six months, and (5) were willing to participate in the cohort and provide written informed consent. Eligible MSM participants were followed-up on every three months. At both baseline and follow-up visits, questionnaire-based interviews and risk-reduction counseling were conducted by trained staff in a separate private interview room of the VCT (HIV Voluntary Counseling & Testing) clinic. Each interview lasted for an average of half an hour, and was conducted by a trained experienced interviewer with at least an undergraduate degree. To meet the psychological needs of each MSM, our interview team consisted of two male interviewers and one female interviewer. No MSM participants had received or were receiving PrEP, as there are still no PrEP guidelines in mainland China. An experienced physician then collected 10 ml of venous blood for HIV and syphilis testing. Those subjects who tested positive for HIV or syphilis were referred to clinics or hospitals to receive appropriate treatment and subsequent medical care. A local MSM non-government organization (Shenyang Sunshine Working Group), and other relevant departments provided counseling and referral services at the study site for MSM subjects who were affected by IPV.
Maintenance of follow-up
To maximize retention, every participant was asked to provide at least two current forms of contact information, including mobile phone numbers and internet-based chat services (WeChat or Tencent QQ), which could be used as reminders for up-coming and missed appointments. Specially dedicated research staff were in charge of ensuring follow-up. Reminder calls were made 1 to 2 weeks before the follow-up day. When a participant missed a follow-up day, staff would call the participant to reschedule the next appointment as soon as possible. If participants could not be reached by phone, WeChat or Tencent QQ messages and peer acquaintances would be used to contact the participants. We offered progressive incentives to further encourage participants to continue to follow-up: participants who attended the baseline visit were given 30 RMB (approximately US$4.34) in cash; those who completed the second visit were given 40 RMB (approximately US$5.79) in cash; those who completed the third visit and beyond were given 50 RMB (approximately US$7.24) in cash.
Data collection
Face-to-face interviews using structured questionnaires were performed to collect the participants’ demographic, behavioral, and IPV information. Depression assessments were performed at baseline and at each 3-month follow-up visit.
Socio-demographic and behavioral variables
Participants were asked to report their socio-demographic information (e.g., residence location, educational level, monthly income, and marital status), sexual risk behavior in the P3M (e.g., multiple male sexual partners, condom use with different partners and role) and substance use in the P3M [e.g., rush (poppers or alkyl nitrites), ice, ketamine, amphetamines, MDMA (“ecstasy”), and tramadol].
Intimate partner violence
To obtain accurate estimates of current victimization among male-to-male relationships, our definition of an IPV experience was the same as the one issued by CDC57. Asking behaviorally specific questions encouraged greater disclosure. The respondents could identify themselves as victims and describe how their partners treated them. Respondents were asked to report “unwanted partner violence” (in order to eliminate participants who were masochists) from a male-to-male sexual partner in past three months based on a series of questions. Participants who responded with “yes” to any of these questions were defined as having been a victim of IPV.
Depression
The study’s approach to measuring symptoms of depression was assessed by the Center for Epidemiologic Studies Depression Scale. CES-D scores ranged from 0 to 60, with 20 items that described either somewhat elevated or very elevated levels of depression symptoms. The symptoms of depression were quantified by the total score (score of 0–15: no depression; score greater than 15: may have depression)58.
Laboratory tests
Blood specimens were collected from each participant for diagnosing HIV and syphilis. HIV serostatus was evaluated with an enzyme-linked immunosorbent assay (ELISA) (InTec Products Company, Xiamen, China), and confirmed with an HIV-1/2 western blot (HIV Blot 2.2 WBTM, Genelabs Diagnostics, Singapore). We selected syphilis, a common STI disease among MSM, as a biologic marker to reflect high-risk behavior, mainly because syphilis detection sampling is more convenient and is highly accepted. Syphilis infection status was determined using the rapid plasma reagin (RPR) test (Shanghai Rongsheng, Shanghai, China), and confirmed with the Treponemapallidum particle assay (TPPA) (Fujirebio Inc, Tokyo, Japan). Only samples that yielded positive results in both tests were considered syphilis-positive (i.e., recently and currently infected with syphilis) when the seroprevalence of syphilis was calculated. Otherwise a negative result was reported59.
Statistical analysis
In our analysis, an HIV seroconversion event was assumed to have occurred at the midpoint between the time of a new HIV diagnosis and the time of the most recent previous HIV-negative visit. Unconditional logistic regression models were performed to examine baseline factors associated with the prevalence of IPV. Factors with P < 0.20 in the univariate analysis were included as logistic variables, and those with P < 0.05 were retained in the final multiple regression model.
Time-dependent Cox proportional-hazards regression models adjusting for the effects of exposure changes on outcome were estimated with adjusted hazard ratios and 95% confidence intervals (CI) as a measure of the relative risk of HIV seroconversion. Factors with P < 0.20 in the univariate analysis were included in the multivariate Cox model, with adjustments for potential confounders such as age, monthly income, education level, and marital status. An important feature of this model is that it includes time-dependent covariates (including IPV and other behavioral factors as well as syphilis/depression status) in the risk set at each observation time point according to their covariate status, which can change at different time intervals.
To specifically assess the effects of IPV on the incidence of HIV, variables kept in the multivariate Cox regression model were further analyzed by PAF and associated 95% CIs, which reflect the fraction of HIV incidence in the whole population. Here, population is defined as the cohort that is associated with the exposure of IPV and other relative factors. This was further computed based on the aHR using the standard formula [p(aHR – 1)/aHR]60. STATA (StataCorp LP) Version 13.0 was employed for data analysis. A two-tailed P < 0.05 was considered statistically significant.
References
UNAIDS. The Gap report, vol. 2014. New York: UNAIDS, http://files.unaids.org/en/media/unaids/contentassets/documents/unaidspublication/2014/UNAIDS_Gap_report_en.pdf (2016).
UNAIDS. 2016 Global AIDS Response Progress Report, CANADA, January 2014–December 2015, http://www.unaids.org/en/dataanalysis/knowyourresponse/countryprogressreports/2016countries/ (2016).
UNAIDS. 2016 Global AIDS Response Progress Report, Japan, http://www.unaids.org/en/dataanalysis/knowyourresponse/countryprogressreports/2016countries/ (2016).
UNAIDS. 2016 Global AIDS Response Progress Report, Netherlands, http://www.unaids.org/en/dataanalysis/knowyourresponse/countryprogressreports/2016countries// (2016).
SCAWCO. China 2010 UNGASS Country Progress Report (2008–2009), http://data.unaids.org/pub/report/2010/china_2010_country_progress_report_en.pdf (2010).
NCAIDS, N. China CDC. Update on the AIDS/STD epidemic in China the third quarter of, 2016. China J AIDS STD. 22, 849 (2016).
Hoff, C. C., Campbell, C. K., Chakravarty, D. & Darbes, L. A. Relationship-Based Predictors of Sexual Risk for HIV Among MSM Couples: A Systematic Review of the Literature. AIDS Behav. 20, 2873–2892 (2016).
Beyrer, C. et al. Global epidemiology of HIV infection in men who have sex with men. Lancet. 380, 367–377 (2012).
Chow, E. P., Wilson, D. P. & Zhang, L. Patterns of condom use among men who have sex with men in China: a systematic review and meta-analysis. AIDS Behav. 16, 653–663 (2012).
Kalichman, S. C. et al. Diminishing Perceived Threat of AIDS and Increasing Sexual Risks of HIV Among Men Who Have Sex with Men, 1997–2015. Archives of sexual behavior. 46(4), 895–902 (2017).
Prevention, C. F. D. C. A. Understanding intimate partner violence. Fact sheet. 17, 2008 (2006).
Jewkes, R. K., Dunkle, K., Nduna, M. & Shai, N. Intimate partner violence, relationship power inequity, and incidence of HIV infection in young women in South Africa: a cohort study. Lancet. 376, 41–48 (2010).
Finneran, C. & Stephenson, R. Intimate partner violence, minority stress, and sexual risk-taking among U.S. men who have sex with men. Journal of homosexuality. 61, 288–306 (2014).
Messinger, A. M. Invisible victims: same-sex IPV in the National Violence Against Women Survey. Journal of interpersonal violence. 26, 2228–2243 (2011).
Dunkle, K. L. et al. Male-on-male intimate partner violence and sexual risk behaviors among money boys and other men who have sex with men in Shanghai, China. Sexually transmitted diseases. 40, 362–365 (2013).
Ibragimov, U. et al. Estimating self-reported sex practices, drug use, depression, and intimate partner violence among MSM in China: a comparison of three recruitment methods. AIDS care. 29, 125–131 (2017).
Relf, M. V., Huang, B., Campbell, J. & Catania, J. Gay identity, interpersonal violence, and HIV risk behaviors: an empirical test of theoretical relationships among a probability-based sample of urban men who have sex with men. The Journal of the Association of Nurses in AIDS Care: JANAC. 15, 14–26 (2004).
Houston, E. & McKirnan, D. J. Intimate partner abuse among gay and bisexual men: Risk correlates and health outcomes. Journal of Urban Health. 84, 681–690 (2007).
Stults, C. B., Javdani, S., Greenbaum, C. A., Kapadia, F. & Halkitis, P. N. Intimate partner violence and substance use risk among young men who have sex with men: The P18 cohort study. Drug and alcohol dependence. 154, 54–62 (2015).
Stall, R. et al. Association of co-occurring psychosocial health problems and increased vulnerability to HIV/AIDS among urban men who have sex with men. Am J Public Health. 93, 939–942 (2003).
Mustanski, B., Garofalo, R., Herrick, A. & Donenberg, G. Psychosocial health problems increase risk for HIV among urban young men who have sex with men: preliminary evidence of a syndemic in need of attention. Annals of behavioral medicine: a publication of the Society of Behavioral Medicine. 34, 37–45 (2007).
Stephenson, R., de Voux, A. & Sullivan, P. S. Intimate Partner Violence and Sexual Risk-taking among Men Who Have Sex with Men in South Africa. The western journal of emergency medicine. 12, 343–347 (2011).
Dyer, T. P. et al. Application of syndemic theory to black men who have sex with men in the Multicenter AIDS Cohort Study. Journal of urban health: bulletin of the New York Academy of Medicine. 89 (2012).
Li, Y., Baker, J. J., Korostyshevskiy, V. R., Slack, R. S. & Plankey, M. W. The association of intimate partner violence, recreational drug use with HIV seroprevalence among MSM. AIDS Behav. 16, 491–498 (2012).
Davis, A. et al. Intimate Partner Violence and Correlates With Risk Behaviors and HIV/STI Diagnoses Among Men Who Have Sex With Men and Men Who Have Sex With Men and Women in China: A Hidden Epidemic. Sexually transmitted diseases. 42, 387–392 (2015).
Beymer, M. R. et al. Disparities Within the Disparity-Determining HIV Risk Factors Among Latino Gay and Bisexual Men Attending a Community-Based Clinic in Los Angeles, CA. Journal of acquired immune deficiency syndromes (1999). 73, 237–244 (2016).
Purcell, D. W. et al. Incorporating couples-based approaches into HIV prevention for gay and bisexual men: opportunities and challenges. Archives of sexual behavior. 43, 35–46 (2014).
Kouyoumdjian, F. G. et al. Intimate partner violence is associated with incident HIV infection in women in Uganda. AIDS. 27, 1331–1338 (2013).
Xu, J. J. et al. High HIV incidence epidemic among men who have sex with men in china: results from a multi-site cross-sectional study. Infectious diseases of poverty. 5, 82 (2016).
Jia, Z. et al. HIV burden in men who have sex with men: a prospective cohort study 2007–2012. Scientific reports. 5, 11205 (2015).
Xu, J. J. et al. Syphilis and HIV seroconversion among a 12-month prospective cohort of men who have sex with men in Shenyang, China. Sexually transmitted diseases. 37, 432–439 (2010).
Zou, X. et al. Rural-to-urban migrants are at high risk of sexually transmitted and viral hepatitis infections in China: a systematic review and meta-analysis. BMC infectious diseases. 14, 490 (2014).
Yu, Y. et al. High-risk behaviour and HIV infection risk among non-local men who have sex with men with less than a single year’s residence in urban centres: a multicentre cross-sectional study from China. Sex Transm Infect. 94(1), 51–54 (2018).
Wall, K. M., Sullivan, P. S., Kleinbaum, D. & Stephenson, R. Actor-partner effects associated with experiencing intimate partner violence or coercion among male couples enrolled in an HIV prevention trial. BMC public health. 14, 209 (2014).
Finneran, C., Chard, A., Sineath, C., Sullivan, P. & Stephenson, R. Intimate Partner Violence and Social Pressure among Gay Men in Six Countries. The western journal of emergency medicine. 13, 260–271 (2012).
Kubicek, K., McNeeley, M. & Collins, S. Same-sex relationship in a straight world: individual and societal influences on power and control in young men’s relationships. Journal of interpersonal violence. 30, 83–109 (2015).
Greenwood, G. L. et al. Battering victimization among a probability-based sample of men who have sex with men. Am J Public Health. 92, 1964–1969 (2002).
Stephenson, R., Rentsch, C., Salazar, L. F. & Sullivan, P. S. Dyadic characteristics and intimate partner violence among men who have sex with men. Western Journal of Emergency Medicine. 12, 324 (2011).
Mirandola, M. et al. Socio-demographic factors predicting HIV test seeking behaviour among MSM in 6 EU cities. European journal of public health. 27(2), 313–318 (2016).
Li, R. et al. Prevalence of prior HIV testing and associated factors among MSM in Zhejiang Province, China: a cross-sectional study. BMC public health. 16, 1152 (2016).
Wagenaar, B. H., Sullivan, P. S. & Stephenson, R. HIV knowledge and associated factors among internet-using men who have sex with men (MSM) in South Africa and the United States. PloS one. 7, e32915 (2012).
Meng, X. et al. Relative Risk for HIV Infection Among Men Who Have Sex with Men Engaging in Different Roles in Anal Sex: A Systematic Review and Meta-analysis on Global Data. AIDS Behav. 19(5), 882–889 (2014).
Stephenson, R., Freeland, R. & Finneran, C. Intimate partner violence and condom negotiation efficacy among gay and bisexual men in Atlanta. Sexual health. Epub ahead of print (2016).
Pan, S. et al. Internet-Based Sex-Seeking Behavior Promotes HIV InfectionRisk: A 6-Year Serial Cross-Sectional Survey to MSM in Shenyang. China. BioMed research international. 2016, 2860346 (2016).
Liu, Y. et al. Seeking Male Sexual Partners via Internet and Traditional Venues among Chinese Men Who Have Sex with Men: Implications for HIV Risk Reduction Interventions. AIDS Behav. 20, 2222–2230 (2016).
Tang, W. et al. Gay mobile apps and the evolving virtual risk environment: a cross-sectional online survey among men who have sex with men in China. Sex Transm Infect. Epub ahead of print (2016).
Tsai, A. C., Tomlinson, M., Comulada, W. S. & Rotheram-Borus, M. J. Intimate Partner Violence and Depression Symptom Severity among South African Women during Pregnancy and Postpartum: Population-Based Prospective Cohort Study. PLoS medicine. 13, e1001943 (2016).
La Flair, L. N., Bradshaw, C. P. & Campbell, J. C. Intimate partner violence/abuse and depressive symptoms among female health care workers: longitudinal findings. Women’s health issues: official publication of the Jacobs Institute of Women’s Health. 22, e53–59 (2012).
Freeland, R., Goldenberg, T. & Stephenson, R. Perceptions of Informal and Formal Coping Strategies for Intimate Partner Violence Among Gay and Bisexual Men. American journal of men’s health. Epub ahead of print (2016).
Wagman, J. A. et al. Effectiveness of an integrated intimate partner violence and HIV prevention intervention in Rakai, Uganda: analysis of an intervention in an existing cluster randomised cohort. The Lancet. Global health. 3, e23–33 (2015).
Arnold, E. A. & Steward, W. T. HIV transmission in MSM: considerations for PrEP scale-up. The lancet. HIV. 3, e62–63 (2016).
McCormack, S. et al. Pre-exposure prophylaxis to prevent the acquisition of HIV-1 infection (PROUD): effectiveness results from the pilot phase of a pragmatic open-label randomised trial. Lancet. 387, 53–60 (2016).
Colombini, M., James, C., Ndwiga, C. & Mayhew, S. H. The risks of partner violence following HIV status disclosure, and health service responses: narratives of women attending reproductive health services in Kenya. Journal of the International AIDS Society. 19, 20766 (2016).
Ridings, L. E. et al. Longitudinal Investigation of Depression, Intimate Partner Violence, and Supports Among Vulnerable Families. Journal of interpersonal violence. Epub ahead of print (2016).
Coker, A. L. et al. Social support protects against the negative effects of partner violence on mental health. Journal of women’s health & gender-based medicine. 11, 465–476 (2002).
Liang, D. H. & Li, J. The preliminary study of civil non-profit organizations in the programe of MSM health education. Chin J AIDS STD. 12, 271–272 (2006).
Breiding, M. J., Basile, K. C., Smith, S. G., Black, M. C. & Mahendra, R. Intimate partner violence: definitions. Centers for Disease Control and Prevention National Center for Injury Prevention and Control, https://www.cdc.gov/violenceprevention/intimatepartnerviolence/definitions.html (2015).
Ostrow, D. G. et al. HIV-related symptoms and psychological functioning in a cohort of homosexual men. The American journal of psychiatry. 146, 737–742 (1989).
Todd, J. et al. Risk factors for active syphilis and TPHA seroconversion in rural African population. Sex Trans Infect. 77(1), 37–45 (2001).
Oehlert, G. W. A note on the delta method. Am Statist. 46(1), 27–29 (1992).
Acknowledgements
The authors appreciate the assistance of volunteers from the sunny group in Shenyang for their help with participant recruitment. We thank all of the MSM who participated in this study for sharing their information and their time. We also thank Dr. MacDonald from University of Eastern Finland for revising the study language. The study was funded by the Mega-Projects of National Science Research of the 12th Five-Year Plan (2012ZX10001-006) and the 13th Five-Year Plan (2017ZX10201101).
Author information
Authors and Affiliations
Contributions
The work presented here was carried out as a collaboration between all authors. All authors read and approved of the final manuscript. Conceived and designed the experiments: H.Y.W., J.J.X., H.S., N.W.; performed the study and experiments: H.Y.W., Z.X.C., X.M.; analyzed the data: H.Y.W., X.M., Z.X.C.; contributed materials/reagents/analysis tools: Y.J.J., W.Q.G.; wrote and revised the manuscript: H.Y.W., J.J.X., J.Z., H.S., N.W. All authors reviewed the manuscript.
Corresponding authors
Ethics declarations
Competing Interests
The authors declare no competing interests.
Additional information
Publisher's note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Wang, Hy., Wang, N., Chu, Zx. et al. Intimate Partner Violence Correlates With A Higher HIV Incidence Among MSM: A 12-Month Prospective Cohort Study in Shenyang, China. Sci Rep 8, 2879 (2018). https://doi.org/10.1038/s41598-018-21149-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-018-21149-8
This article is cited by
-
Domestic Violence among LGBT + People in China: Results from a national court rulings review
Journal of Family Violence (2023)
-
Sexual Behavior Transition and Acute and Early HIV Infection Among Men Who Have Sex With Men: Evidence from an Open Cohort in China, 2011–2019
Archives of Sexual Behavior (2022)
-
Moderating effect of self-efficacy on the association of intimate partner violence with risky sexual behaviors among men who have sex with men in China
BMC Infectious Diseases (2021)
-
The mediating role of self-stigma and self-efficacy between intimate partner violence (IPV) victimization and depression among men who have sex with men in China
BMC Public Health (2020)
-
Sexual Partnership-Level Correlates of Intimate Partner Violence Among Men Who Have Sex with Men and Transgender Women in Lima, Peru
Archives of Sexual Behavior (2020)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.