Abstract
The repair of injured peripheral nerve is still challenging for surgeons. The end-to-end and tension-free neurorrhaphy is the current gold standard for reconstruction after complete nerve transection without significant defect. The main objective of this study neurorrhaphy in digit replantation affects the sensory recovery and neuropathic pain in replanted digit. Total 101 patients who received replantation of single completely amputated digit were included for analysis in this study. In group I (n = 49), the digital nerves were repaired with end-to-end and tension-free neurorrhaphy and then wrapped into a tendon-derived collagen nerve conduit. In group II (n = 52), the digital nerves were repaired with end-to-end and tension-free neurorrhaphy only. The static two-point discrimination (s2PD) was performed to evaluate sensory recovery. Visual analog scale (VAS) scores of pain at rest and with exertion were measured respectively. The s2PD tests at three and six months after surgery did not show any significant difference between the two groups. The VAS scores at rest and with exertion of group I were significantly reduced compared with those of group II at three and six months after surgery. Thus, we concluded that nerve wrap into a collagen conduit after end-to-end and tension-free neurorrhaphy could attenuate neuropathic pain after digit replantation but have no benefit for sensory recovery.
Similar content being viewed by others
Introduction
The repair of vessels, nerves, tendons and bones of amputated digit is essential for the survival and functional recovery of replanted digit1,2,3. After the advance of microsurgery in decades, the survival rates of digital replantation have been reported up to 80%4,5. A satisfactory range of motion and appearance could also be restored by primary replantation and secondary surgeries, if necessary, in most cases6. However, the repair of injured nerve is still challenging in digit replantation. The recovery after nerve injury is commonly incomplete and disappointing even when the injured nerves were repaired without any tension by microsurgical techniques7. In addition, neuropathic pain can develop after nerve injury, when deleterious changes occur in injured nerve8. A previous study has revealed that the neuropathic pain can occur in up to 45% patients after replantation9.
The end-to-end and tension-free neurorrhaphy is the current gold standard for reconstruction after complete nerve transection without significant defect. Nerve wrap with biodegradable conduits, also known as nerve tubulization, is widely applied as a strategy in treatment of small nerve defect10 and multiple studies has demonstrated that nerve wrap has superior or similar outcomes compared with tensile neurorrhaphy (neurorrhaphy with tension) and nerve graft10,11,12.
One important mechanism that influences recovery and causes neuropathic pain is the scar formation at the site of nerve anastomosis8,13,14,15. Recent progress based on the nerve transection model in rats has demonstrated that nerve wrap after end-to-end and tension-free neurorrhaphy could decrease perineural scar tissue formation16,17. However, there is few literature, to the best of our knowledge, evaluating the clinical efficacy of nerve wrap after end-to-end and tension-free neurorrhaphy.
Methods
Ethical approval
The study was approved by the Ethics Committee of Shanghai Jiaotong University Affiliated Sixth People’s Hospital. Informed consent was obtained from all donors in accordance with the Declaration of Helsinki.
Participants and study setting
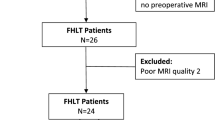
Total 101 patients who received replantation of single completely amputated digit from 1 March 2016 to 1 March 2017 were included in this study. The Tamai’s level of amputation was classified according to the classification system described previously18. For cases amputated at Tamai level I and II, there might be no nerve suitable for repair. Hence, this study only included patients with amputation at Tamai level III, IV and V. Complete amputations were defined as complete separation of all parts without any bridging tissues. Patients with any of the following criteria were excluded: nerve defect, single or multiple organ failure, peripheral arterial diseases, additional wound on artery in the ipsilateral arm or forearm, age below 18, replant failure, peripheral neuropathy before injury. Patient characteristics including age, smoking, amputation level, and mechanism of injury were summarized in Table 1. The mechanisms of injury were classified into blade, saw, crush, and avulsion injuries.
Nerve wrap
The nerves were first repaired using epineurial fashion technique with 10–0 nylon sutures under the operating microscope (Fig. 1). The current practices of nerve wrap after end-to-end and tension-free neurorrhaphy was empirical. Some surgeons in our hospital routinely conducted nerve wrap using a tendon-derived collagen conduit (Tianxinfu Medical Appliance, Beijing, China) while the other did not. For nerve wrap, the repaired nerve was first wrapped with the collagen conduit (with a gap) at the site of anastomosis and the gap was then closed with sutures (Fig. 2).
Outcome assessment
Visual analog scale (VAS) score ranges from 0 (no pain) to 100 mm (worst pain possible). Because motion-evoked pain is frequently observed after nerve repair, similar to previous study19, we measured VAS score at rest and with exertion respectively according to the patient’s experience of average pain in the past week. The application of pain medication was also recorded. The static two-point discrimination (s2PD) were performed to evaluate sensory recovery. The s2PD test results was categorized as “Excellent” (≤6 mm), “Good” (7–15 mm), and “Poor” (>15 mm) respectively according to the Mackinnon classification20. VAS and s2PD tests were conducted at three and six months after surgery.
Statistics
The significance of differences between groups in each variable was assessed using Pearson’s Chi-squared test or Student’s t test unless labeled otherwise. All data were presented as mean ± standard deviation.
Results
The mean age of all patients was 39.4 ± 10.2 years. There were 90 amputated digits from men (89%) and 11 amputated digits from women (11%). Patients were divided into two groups based on whether received nerve wrap. The demographic and clinical characteristics were summarized in Table 1. All these variables had no significant differences between the two groups.
In group I (n = 49), the digital nerves were repaired with end-to-end and tension-free neurorrhaphy and then wrapped into a tendon-derived collagen nerve conduit. In group II (n = 52), the digital nerves were repaired with end-to-end and tension-free neurorrhaphy only. To evaluate the outcomes of sensory recovery, s2PD tests were conducted at three and six months after surgery. We did not observe any significant difference in sensory recovery after digit replantation between the two groups (Table 2). The VAS scores at rest and with exertion of group I were significantly reduced compared with those of group II at both three and six months after surgery (Table 3). Consistently, Tinel’s sign at the repair site was more frequently present in group II than group I.
Traumatic neuroma was presented in three patients (all in group 2) by the end of follow up. The difference in the incidence of traumatic neuroma was insignificant between the two groups (P value = 0.24, Fisher’s exact test).
Discussion
The conventional wisdom was that nerve warp could limit the regenerating axons in a proper orientation and thus bridge the gap between the two nerve stumps. For those with tension-free repair, nerve wrap was believed to be unnecessary21. However, recent progress has revealed that nerve wrap after end-to-end and tension-free neurorrhaphy could decrease perineural scar tissue formation and thus improve the prognosis in rats16,17. The clinical application of nerve wrap after end-to-end and tension-free neurorrhaphy is currently empirical and off-label, highlighting the need for clinical evidence. In this study, we show nerve wrap after end-to-end and tension-free neurorrhaphy could attenuate neuropathic pain after digit replantation but have no benefit for sensory recovery. Notably, digital nerves are sensory and it is still unclear whether nerve wrap could bring benefits for the injuries on motor and mixed nerve. Further studies are required to address this question.
There are various types of conduits differed with materials including collagen, biological and synthetic polymers21. In this study, we wrapped the anastomosed nerve with collagen conduits because the degradation of collagen could be completed within three months and delayed degradation leads to the formation of scar22,23. The currently available nerve conduits were generally designed for the treatment of nerve defect. Conceivably, these designs might not be optimal for nerve wrap after tension-free and end-to-end anastomosis. Novel designs might further increase the therapeutic benefits of nerve wrap.
The limitations of our study include a non-randomized design and a small sample size. Notably, all patients with traumatic neuroma belonged to group 2 and there is a clear tendency towards significance. A future study with larger sample size could address whether nerve wrap could reduce the incidence of traumatic neuroma.
Conclusions
Nerve wrap into a collagen conduit after end-to-end and tension-free neurorrhaphy could attenuate neuropathic pain after digit replantation but show no benefit for sensory recovery.
References
Kleinert, H. E., Serafin, D., Kutz, J. E. & Atasoy, E. Reimplantation of amputated digits and hands. The Orthopedic clinics of North America 4, 957–967 (1973).
Morrison, W. A., O’Brien, B. M. & MacLeod, A. M. Evaluation of digital replantation–a review of 100 cases. The Orthopedic clinics of North America 8, 295–308 (1977).
Kleinert, H. E. & Tsai, T. M. Microvascular repair in replantation. Clinical orthopaedics and related research, 205–211 (1978).
Chang, D. H., Ye, S. Y., Chien, L. C. & Ma, H. Epidemiology of digital amputation and replantation in Taiwan: A population-based study. Journal of the Chinese Medical Association: JCMA 78, 597–602 (2015).
Dec, W. A meta-analysis of success rates for digit replantation. Techniques in hand & upper extremity surgery 10, 124–129 (2006).
Matsuzaki, H., Kouda, H. & Maniwa, K. Secondary surgeries after digital replantations: a case series. Hand surgery: an international journal devoted to hand and upper limb surgery and related research: journal of the Asia-Pacific Federation of Societies for Surgery of the Hand 17, 351–357 (2012).
Allan, C. H. Functional results of primary nerve repair. Hand clinics 16, 67–72 (2000).
Cohen, S. P. & Mao, J. Neuropathic pain: mechanisms and their clinical implications. BMJ (Clinical research ed) 348, f7656 (2014).
Hovgaard, C., Angermann, P. & Hovgaard, D. The social and economic consequences of finger amputations. Acta orthopaedica Scandinavica 65, 347–348 (1994).
Lohmeyer, J. A. et al. Prospective clinical study on digital nerve repair with collagen nerve conduits and review of literature. Journal of reconstructive microsurgery 30, 227–234 (2014).
Weber, R. A., Breidenbach, W. C., Brown, R. E., Jabaley, M. E. & Mass, D. P. A randomized prospective study of polyglycolic acid conduits for digital nerve reconstruction in humans. Plastic and reconstructive surgery 106, 1036–1045; discussion 1046–1038 (2000).
Battiston, B., Geuna, S., Ferrero, M. & Tos, P. Nerve repair by means of tubulization: literature review and personal clinical experience comparing biological and synthetic conduits for sensory nerve repair. Microsurgery 25, 258–267 (2005).
Decrouy-Duruz, V., Christen, T. & Raffoul, W. Evaluation of surgical treatment for neuropathic pain from neuroma in patients with injured peripheral nerves. Journal of neurosurgery 1–6 (2017).
Marcol, W. et al. Reduction of post-traumatic neuroma and epineural scar formation in rat sciatic nerve by application of microcrystallic chitosan. Microsurgery 31, 642–649 (2011).
Lane, J. M., Bora, F. W. Jr. & Pleasure, D. Neuroma scar formation in rats following peripheral nerve transection. The Journal of bone and joint surgery American volume 60, 197–203 (1978).
Lee, J. Y., Parisi, T. J., Friedrich, P. F., Bishop, A. T. & Shin, A. Y. Does the addition of a nerve wrap to a motor nerve repair affect motor outcomes? Microsurgery 34, 562–567 (2014).
Tetik, C. et al. Conventional versus epineural sleeve neurorrhaphy technique: functional and histomorphometric analysis. Annals of plastic surgery 49, 397–403 (2002).
Tamai, S. Twenty years’ experience of limb replantation–review of 293 upper extremity replants. The Journal of hand surgery 7, 549–556 (1982).
El-Diwany, M. et al. Replantation vs revision amputation in single digit zone II amputations. Journal of plastic, reconstructive & aesthetic surgery: JPRAS 68, 859–863 (2015).
Mackinnon, S. E. & Dellon, A. L. Clinical nerve reconstruction with a bioabsorbable polyglycolic acid tube. Plastic and reconstructive surgery 85, 419–424 (1990).
Arslantunali, D., Dursun, T., Yucel, D., Hasirci, N. & Hasirci, V. Peripheral nerve conduits: technology update. Medical devices (Auckland, NZ) 7, 405–424 (2014).
Griffin, J. W., Hogan, M. V., Chhabra, A. B. & Deal, D. N. Peripheral nerve repair and reconstruction. The Journal of bone and joint surgery American volume 95, 2144–2151 (2013).
Pabari, A., Lloyd-Hughes, H., Seifalian, A. M. & Mosahebi, A. Nerve conduits for peripheral nerve surgery. Plastic and reconstructive surgery 133, 1420–1430 (2014).
Author information
Authors and Affiliations
Contributions
H.Z. was responsible for study design and manuscript writing. X.Z. was responsible for follow-up and data collection. H.W. was responsible for study design and data analysis. None of the authors has a financial interest in any of the products, devices, or drugs mentioned in this manuscript.
Corresponding authors
Ethics declarations
Competing Interests
The authors declare that they have no competing interests.
Additional information
Publisher's note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Zhu, X., Wei, H. & Zhu, H. Nerve wrap after end-to-end and tension-free neurorrhaphy attenuates neuropathic pain: A prospective study based on cohorts of digit replantation. Sci Rep 8, 620 (2018). https://doi.org/10.1038/s41598-017-19134-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-017-19134-8
This article is cited by
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.