Abstract
Leukotriene B4 (LTB4) is essential for host immune defence. It increases neutrophil recruitment, phagocytosis and pathogen clearance, and decreases oedema and inflammasome activation. The host response and the role of LTB4 during Achromobacter xylosoxidans infection remain unexplored. Wild-type (129sv) and LTB4 deficient (Alox5 −/−) mice were intratracheally infected with A. xylosoxidans. Wild-type 129sv infected mice survived beyond the 8th day post-infection, exhibited increased levels of LTB4 in the lung on the 1st day, while levels of PGE2 increased on the 7th day post-infection. Infected Alox5 −/− mice showed impaired bacterial clearance, increased lung inflammation, and succumbed to the infection by the 7th day. We found that exogenous LTB4 does not affect the phagocytosis of A. xylosoxidans by alveolar macrophages in vitro. However, treatment of infected animals with LTB4 protected from mortality, by reducing the bacterial load and inflammation via BLT1 signalling, the high affinity receptor for LTB4. Of importance, we uncovered that LTB4 induces gene and protein expression of α-defensin-1 during the infection. This molecule is essential for bacterial clearance and exhibits potent antimicrobial activity by disrupting A. xylosoxidans cell wall. Taken together, our data demonstrate a major role for LTB4 on the control of A. xylosoxidans infection.
Similar content being viewed by others
Introduction
Cystic fibrosis (CF) is a genetic disease caused by mutations in the cystic fibrosis transmembrane conductance regulator (CFTR), an ion-channel responsible for the transport of ions across the epithelial barrier1. The major CF complication is the persistent colonisation of the respiratory tract by opportunistic microorganisms, such as Achromobacter xylosoxidans 2,3. The bacillus produces virulence factors, exhibits clearance-evading mechanisms, and may resist to multiple classes of antibiotics4. It has been associated with the exacerbation of pulmonary symptoms and rapid decline in lung function5. CF patients have increased levels of granulocyte colony stimulating factor (G-CSF), interleukin (IL)-6, tumour necrosis factor (TNF)-α; and eicosanoids (EICs) such as leukotriene B4 (LTB4) and prostaglandin E2 (PGE2), compared to healthy controls6,7,8. Patients with chronic A. xylosoxidans infection produce high amounts of TNF-α in the sputum7; furthermore, components of A. xylosoxidans cell wall induce pro-inflammatory cytokine production by lung cells, monocytes and macrophages in vitro 9,10,11.
EICs are lipid mediators derived from the metabolism of arachidonic acid (AA) and related polyunsaturated fatty acids (PUFAs), present in membrane phospholipids. Three major enzymatic pathways–driven by the lipoxygenases (LOs), cyclooxygenases (COXs) and cytochrome P450 (CYP) epoxyhydrolases—convert free AA to generate leukotrienes (LTs), prostaglandins (PGs), epoxyeicosatrienoic acids (EETs) and hydroxyeicosatetraenoic acids (HETEs)12. Downstream mediators of 5-LO protect mice from infections with Klebsiella pneumoniae 13, Mycobacterium tuberculosis 14, Streptococcus pyogenes 15. LTB4 induces leukocyte recruitment16, increases phagocytosis and pathogen killing15,17, and increases antimicrobial peptide (AMP) production, like α-defensin-118. Recently, our group reported that LTB4 reduces lung inflammation and prevents scorpion envenomation-induced death by down-regulating inflammasome activation and IL-1β production19. Despite the clinical importance of A. xylosoxidans, whether LTB4 elicits protective mechanisms against this bacterial infection still needs to be elucidated.
Here, we investigated the impact of 5-LO deficiency on lung inflammation, bacterial clearance and mortality in A. xylosoxidans-induced pneumonia. We observed that Alox5 −/− mice are more susceptible to A. xylosoxidans infection than the 129sv wild-type mice. They exhibited increased mortality, higher bacterial burden and augmented lung inflammation and oedema. Furthermore, we determined that LTB4 protected against A. xylosoxidans infection, as intranasal administration of LTB4 to Alox5 −/− mice reduced bacterial burden and lung oedema, increased neutrophil recruitment and prevented death. To confirm that LTB4 signalling is essential for lung protection during A. xylosoxidans infection, we treated infected 129sv mice with LTB4 receptor 1 antagonist (BLT1) and observed increased bacterial burden and oedema in the lungs, as well as higher mice mortality. Importantly, we demonstrated that LTB4 was fundamental for α-defensin-1 expression in infected alveolar macrophages in vitro, and in the lungs of A. xylosoxidans infected mice. This peptide is crucial for A. xylosoxidans clearance, once silencing of α-defensin-1 mRNA abrogated killing of A. xylosoxidans induced by LTB4. Using transmission electron microscopy, we confirmed that α-defensin-1 reduced A. xylosoxidans viability by disrupting the bacterial cell wall.
Results
Infection with A. xylosoxidans induces the production of eicosanoids
To understand the host response to infections with A. xylosoxidans, we first established a murine experimental lung infection model with this pathogen. The moving average interpolation method20 and biometric tables for median-lethal dose (LD50) calculation21 were used to predict the lethal and sublethal LD50 inoculums of A. xylosoxidans in 129sv mice. The median lethal and sublethal doses were estimated as 6.2 × 108 and 2 × 108 bacilli, respectively (Supplementary Table 1).
Using a sublethal inoculum (2 × 108 bacilli) of A. xylosoxidans, we first assessed the production of PGE2 and LTB4 induced by infection in the lung parenchyma. In the lungs of 129sv mice, LTB4 levels peaked on the 1st day post-infection (Fig. 1a), and declined thereafter to reach basal levels by the 3rd day. However, detectable levels of PGE2 were observed only on the 7th day post-infection (Fig. 1b). Interestingly, Alox5 −/− mice produced similar amounts of PGE2 between days 1 and 3 post-infection, which did not differ from the uninfected mice (Fig. 1c). However, as all Alox5 −/− mice succumbed to the infection within 5 days, we could not measure PGE2 production after this time-point (Fig. 1c). Irrespective of the infection, Alox5 −/− mice demonstrated higher production of PGE2 than the 129sv mice (Fig. 1b,c).
A. xylosoxidans infection induces LTB4 and PGE2 production in the lung. 129sv wild-type (a,b) or Alox5 −/− (c) mice were inoculated i.t. with 100 μL of PBS (dashed line) or with sublethal inoculum of A. xylosoxidans (2 × 108 in 100 μL of PBS). Lung tissue was collected at 1, 3 and 7 days post-infection (all Alox5 −/− died within 7 days [†]) and processed for LTB4 and PGE2 measurements in the lung parenchyma. Data are mean ± SEM from one representative experiment (n = 4–5 mice group for each time-point). *p < 0.05 for uninfected (UN) versus infected mice at the same time-point by a one-way analysis of variance with a Newman-Keuls multiple comparison post-test.
5-LO deficiency increases mortality, bacterial burden and lung inflammation
Previous investigations indicate that Alox5 −/− mice are more susceptible to infections and envenomation17,19. To evaluate the role of 5-LO products in the infection with A. xylosoxidans, 129sv and Alox5 −/− mice were infected with sublethal A. xylosoxidans inoculums. We observed that the infection was robust but self-limiting in the 129sv mice, as no CFUs were recovered 7 days post-infection (Fig. 2b). Downstream products of 5-LO actively affect the course of infection with A. xylosoxidans, revealed by the increased mortality of Alox5 −/− mice (Fig. 2a). Following infection, 100% of the Alox5 −/− mice died within the first 5 days, while 85% of the wild-type mice survived 7 days post-infection (Fig. 2a) (wild-type animals survived for at least 14 days post-infection, the last observed time-point, data not shown).
5-LO deficiency impairs bacterial clearance, and increases lung oedema and mortality. Wt and Alox5 −/− mice were i.t. infected with sublethal inoculum of A. xylosoxidans (2 × 108/100 μL in PBS) for survival determination until 7 days post-infection (n = 8 mice per strain) (a). Log-Rank test was used to compare survival between the strains. Comparison of bacterial burden (b), lung weight (c), and BALF protein content (d). Uninfected (UN) mice receiving i.t. 100 μL of PBS were used as negative control (dashed lines). Data are mean ± SEM of three independent experiments (n = 5–14 mice per group at each time-point). *p < 0.05 for UN versus infected animals at each time-point and for both strains, # p < 0.05 for wt versus Alox5 −/− mice using student’s t- test (b) or one-way analysis of variance with Newman-Keuls multiple post-test (c,d). †Mice died, NR: not recovered (using this method). BALF: bronchoalveolar lavage fluid.
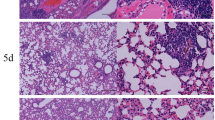
To investigate the potential mechanisms resulting in early mortality, we determined bacterial burden and inflammation in the lungs of both mouse strains. The Alox5 −/− mice exhibited a 5- and 9-fold higher lung bacterial burden compared to the wild-type, at days 1 and 3 post-infection, respectively (Fig. 2b). We did not find bacteria in the spleen and blood of both infected mouse strains (data not shown). Lung inflammation was more pronounced in the Alox5 −/− mice, which exhibited an increase of 47% in lung weight compared to an increase of 38% in 129sv mice (Fig. 2c). BALF protein concentrations increased 129% in Alox5 −/− mice, while 129sv mice exhibited an increase of 39% at days 1 and 3 post-infection (Fig. 2d). Compared to 129sv, the Alox5 −/− mice showed a small reduction in the BALF neutrophil counts at day 1, but a significant increase in neutrophils at day 3 post-infection (Fig. 3a). The increased inflammation in the lungs of Alox5 −/− mice was confirmed by histological analysis, showing a massive leukocyte infiltration in the lung parenchyma (Fig. 3b,c), and increased damage of the lung architecture (Fig. 3d).
Alox5 −/− mice exhibit pronounced lung inflammation following pulmonary infection with A. xylosoxidans. Neutrophil and mononuclear cell counts in the BALF of A. xylosoxidans (2 × 108/100 μL of PBS) or PBS inoculated 129sv and Alox5 −/−mice at 1, 3 and 7 days post sublethal infection (a). Representative HE stained lung sections at day 1 (b) and 3 post-infection (c) (100× and 1000× [in inset] resolution, scale bar: 100 µm). Percentage of immune cell infiltrated area corresponding to the extent of lung damage (d). Data are mean ± SEM of two independent experiment (n = 5–10 mice per group at each time-point). Differences were considered significant with p < 0.05 calculated using one-way ANOVA (Newman-Keuls multiple comparison test) (a). *p < 0.05 for untreated (UN) versus infected, # p < 0.05 for wt versus Alox5 −/− by student’s t-test (d) or one-way analysis of variance with Newman-Keuls multiple comparison (a), †mice died.
Absence of 5-LO enhances TNF-α, IL-1α and MIP-1α in infected lungs
Inflammation is a crucial process in host response against aggressors, and is mediated by the action of pro-inflammatory cytokines, chemokines and eicosanoids, which promote leukocyte recruitment and oedema19,22,23. Therefore, we next assessed the levels of cytokine and chemokine in lung parenchyma of infected animals. At the 1st and 3rd day, infection with A. xylosoxidans induced significant release of TNF-α, MIP-1α, IL-1α and MCP-1 in both 129sv and Alox5 −/− mice (Fig. 4). Compared to 129sv mice, the levels of TNF-α, IL-1α, and MIP-1α were 76%, 58%, and 42% higher in Alox5 −/− mice at the 1st day post-infection (Fig. 4a–c). However, at the 3rd day post-infection, only levels of MIP-1α were higher in the Alox5 −/− mice (Fig. 4b). The MCP-1 production was similar in both strains at all observed time-points (Fig. 4d). On the 7th day post-infection, these cytokines were detected at very low levels in the lungs of 129sv mice.
Impact of 5-LO deficiency on cytokine and chemokine production in the lungs of A. xylosoxidans-infected mice. TNF-α (a), MIP-1α (b), IL-1α (c), and MCP-1 (d) concentrations at 1, 3 and 7 days following infection. The data are mean ± SEM of three independent experiments (n = 5–10 mice per group at each time-point). *p < 0.05 for untreated (UN) versus infected mice, # p < 0.05 for wt versus Alox5 −/− using one-way analysis of variance and Newman-Keuls multiple comparison test.
Intranasal LTB4 restores lung innate immune response and reduces mortality in the Alox5−/− infected mice
As the Alox5 −/− mice were more susceptible to infection than the 129sv, we evaluated the effect of LTB4 treatment on the genetically modified mice. Infected Alox5 −/− mice treated with LTB4 exhibited 66% survival at the 7th day post-infection, compared to 0% survival of vehicle-treated infected Alox5 −/− mice (Fig. 5a). At the 3rd day post-infection, LTB4-treated mice showed significantly lower bacterial burdens (Fig. 5b), and lower BALF protein extravasation (Fig. 5d). As expected, LTB4 treatment increased neutrophil recruitment at the 1st day post-infection (Fig. 5c), while no differences were observed in the mononuclear cell recruitment (data not shown).
LTB4 treatment reduces susceptibility of Alox5 −/− mice to pulmonary infection with A. xylosoxidans. Survival rate of infected Alox5 −/− mice with or without LTB4 treatment was evaluated for 7 days (a) (n = 6 total), and p < 0.05 considered significant using Log-Rank test. Quantification of bacterial burden (b), BALF neutrophil counts (c) and protein content (d) at 1 and 3 days post-infection. The data are mean ± S.E.M of three independent experiment (n = 4–10 mice per group at each day). *p < 0.05 for uninfected (UN) versus infected mice, # p < 0.05 for Alox5 −/− versus Alox5 −/− + LTB4 using one-way analysis of variance (Newman-Keuls multiple comparison test). BALF: bronchoalveolar lavage fluid.
Blocking of BLT1 signalling impairs lung innate immune response and increases mortality in 129sv mice
Since LTB4 administration protected the Alox5 −/− infected mice, we next investigated the effect of BLT1 signalling blockade on the 129sv mice. Our results demonstrate that the treatment of 129sv-infected mice with U-75302, a BLT1 antagonist, resulted in 100% mortality (Fig. 6a). At the 3rd day post-infection, the treatment increased lung bacterial burden (Fig. 6b), without affecting neutrophil recruitment in BALF (Fig. 6c). Interestingly, BLT1 antagonist increased the protein concentration in the BALF of infected mice (Fig. 6d).
Blockade of BLT1 signalling increases susceptibility of 129sv mice to A. xylosoxidans infection. Survival rate for infected wt mice with or without BLT1 antagonist treatment was evaluated for 7 days (a) (n = 6 total), and p < 0.05 considered significant using Log-Rank test. Quantification of bacterial burden (b), BALF neutrophil counts (c) and protein content (d). Data are mean ± S.E.M of one representative experiment (n = 4–6 mice per group at each day). *p < 0.05 for untreated (UN) versus infected mice, # p < 0.05 for 129sv versus 129sv + BLT1 antagonist U-75302 using one-way ANOVA (Newman-Keuls multiple comparison test). BALF: bronchoalveolar lavage fluid.
LTB4 increases killing of A. xylosoxidans and Defa1 expression in alveolar macrophages
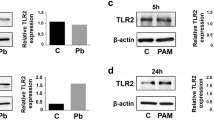
To assess the mechanism by which LTB4 confers resistance to infection with A. xylosoxidans, we first evaluated the bacterial phagocytosis. For this purpose, AMJ2-C11 cells (murine alveolar macrophage cell lineage) were pre-treated or not with increasing concentrations of LTB4, followed by infection with FITC-labelled A. xylosoxidans. We observed that LTB4 did not affect the percentage of FITC+ cells (Fig. 7a) or MFI of infected AMJ2-C11 (data not shown), indicating that LTB4 did not increase phagocytosis of FITC-labelled bacteria. Next, we evaluated the ability of AMJ2-C11 to kill A. xylosoxidans in the presence or absence of exogenous LTB4. We observed that at 6 h after incubation, AMJ2-C11 cells pre-treated with 100 nM of LTB4 enhanced the bactericidal activity against A. xylosoxidans (Fig. 7b). At 24 h after incubation, all concentrations of LTB4 enhanced killing of A. xylosoxidans by AMJ2-C11 cells (Fig. 7b). Once LTB4 is known to induce pathogen killing by increasing the production of AMPs18,24, we determined the expression of Defa1 in infected AMJ2-C11 cells. Notably, we detected that pre-treatment of AMJ2-C11 cells with LTB4 increased the expression of Defa1 at 2 and 6 h post-infection with A. xylosoxidans (Fig. 7c).
LTB4 increases killing of A. xylosoxidans and Defa-1 expression in alveolar macrophages without affecting phagocytosis. AMJ2-C11 was treated or not with crescent concentrations of LTB4 (1, 10 and 100 nM). Cells were infected with FITC-labelled A. xylosoxidans (MOI 50:1) and incubated for 2 h at 37 °C, 5% CO2. After this period, the cells were washed, incubated with trypan blue 0.4% pH 4.4 and submitted to flow cytometry analysis for phagocytosis determination (a). Representative histogram out of four independent experiments is shown (n = 12). For bacterial killing assay, cells were infected with A. xylosoxidans (MOI 5:1) and incubated for 6 or 24 h at 37 °C, 5% CO2. Then, the cells were lysed with saponin (0.05%), mixed with 10 μL of a resazurin solution (0.5 mg/mL) and after 8 h at 37 °C the RFU was measured by fluorimeter microplate reader (b). One representative experiment out of three is shown as mean ± S.E.M. (n = 4–5 wells), # p < 0.05 for untreated versus LTB4 treated cells, using one-way analysis of variance (Newman-Keuls multiple comparison test). Cells treated or not with 100 nM of LTB4 were infected with A. xylosoxidans (MOI 30:1), incubated for 30, 120 or 360 minutes and submitted to quantification of Defa1 mRNA expression by Real-Time PCR (c). One representative experiment out of two is shown as mean ± S.E.M. (n = 6–8 wells), # p < 0.05 for AMJ2-C11 infected versus LTB4 treated and infected AMJ2-C11 cells using Two-way analysis of variance (Bonferroni post-test).
LTB4 potentiates the gene and protein expression of α-defensin-1 in the infected lungs
Next, we determined the gene expression and secretion of α-defensin-1 in the lungs of infected 129sv and Alox5 −/− mice. Compared to uninfected animals, pulmonary infection with A. xylosoxidans significantly increased Defa1 expression in both strains of animals. However, 5-LO deficiency compromised the expression of Defa1 induced by infection (Fig. 8a). Next, we assessed if treatment with LTB4 could restore the expression of Defa1 in lungs of Alox5 −/− mice. We observed that at the 1st day post-infection, treatment with LTB4 rescued the expression of Defa1 in lungs of infected Alox5 −/− mice (Fig. 8b). We also evaluated the secretion of α-defensin-1 in BALF of both strains of animals. We observed that uninfected Alox5 −/− mice present less α-defensin-1 when compared with uninfected 129sv mice (Fig. 8c). When infected with A. xylosoxidans, 129sv produce increased levels of α-defensin-1 compared to infected Alox5 −/− mice, on 1st day post-infection (Fig. 8c). At the 3rd day post-infection, Alox5 −/− mice treated with LTB4 exhibited similar amounts of α-defensin-1 compared to untreated 129sv-infected mice.
LTB4 induces and potentiates the release of the antimicrobial peptide alpha-defensin-1. qRT-PCR was used to evaluate Defa1 mRNA expression in lung parenchyma of wt, Alox5 −/− and LTB4 treated Alox5 −/− mice at 1, 3 and 7 days post-infection (a,b) and for quantification of α-defensin-1 peptide by ELISA in BALF (c). Data are mean ± S.E.M of three independent experiments (n = 4–15 mice per group at each time-point) for qRT-PCR and of one independent experiment (n = 4 mice per group at each time-point) for ELISA assay. *p < 0.05 for untreated (UN) versus infected mice, # p < 0.05 for 129sv versus Alox5 −/− or Alox5 −/− versus Alox5 −/− + LTB4 using one-way analysis of variance (Newman-Keuls multiple comparison test). AMJ2-C11 cells were submitted to silencing of α-defensin-1 mRNA using siRNA. After 36 h of transfection, cells were pre-treated or not with LTB4 and then infected with A. xylosoxidans (MOI 5:1), and submitted for killing evaluation at 6 h (d). Data are mean ± S.E.M of one independent experiment (n = 5), # p < 0.05 for AMJ2-C11 infected versus LTB4 treated and infected AMJ2-C11 cells, using one-way analysis of variance (Newman-Keuls multiple comparison test). 105 CFU of A. xylosoxidans incubated for 3 h, with crescent concentrations (5, 50 and 500 pg) of recombinant α-defensin-1 peptide were submitted to viability assay by resazurin metabolism (e). Data are mean ± S.E.M of one independent experiment (n = 5), # p < 0.05 for Ax versus α-defensin-1 treated Ax cells using one-way analysis of variance (Newman-Keuls multiple comparison test). Transmission electron microscopy of A. xylosoxidans (109 CFU/ml) incubated with 500 pg of recombinant α-defensin-1 peptide for 2 h (f). Bars represent 1 µM.
The clearance of A. xylosoxidans induced by LTB4 depends on α-defensin-1 activity
To prove that increased killing of A. xylosoxidans induced by LTB4 is dependent on α-defensin-1 activity, we first silenced α-defensin-1 mRNA in AMJ2-C11 cells, and pre-treated the silenced cells with LTB4 before the infection with A. xylosoxidans. We observed that silenced AMJ2-C11 cells were unable to kill A. xylosoxidans, even in presence of exogenous LTB4 (Fig. 8d). Following, we incubated 1 × 105 bacilli of A. xylosoxidans with increasing concentrations of recombinant α-defensin-1, and after 3 h we evaluated the antimicrobial activity of α-defensin-1. We observed a reduction of 40% in bacteria viability incubated with higher concentrations (500 pg) of recombinant α-defensin-1 (Fig. 8e). To determine how α-defensin-1 affects the viability of A. xylosoxidans, we performed a transmission electron microscopy of the bacteria incubated with α-defensin-1. We observed that this peptide disrupts A. xylosoxidans cell wall (Fig. 8f).
Discussion
A. xylosoxidans, a pathogen frequently recovered from the lungs of CF patients, is associated with impairment of lung function4. Here, we aimed to determine the role of LTB4 in A. xylosoxidans lung infection to identify better therapeutic strategies. First, we established a sublethal inoculum of A. xylosoxidans for i.t. infection of 129sv (wild-type) mice. We found that the sublethal dose of 2 × 108 bacteria induced a strong, but self-limiting infection restricted to the lungs, which was cleared by the 7th day post-infection. At this time point, we observed an almost complete bacterial elimination, indicating that immune competent hosts were able to control the lung infection. In different time-points, the infection of 129sv mice was characterized by significant neutrophil recruitment, oedema formation, and the production of TNF-α, MIP-1α, IL-1α, MCP-1, LTB4, PGE2, and α-defensin-1 in the lungs. Some of these results are in accordance with previously published reports demonstrating that chronic infection with A. xylosoxidans in humans was associated with increased production of TNF-α and IL-66,7, and that CF patients presented higher concentration of LTB4 and PGE2 in body fluids such as airway secretions and sputum6,8.
Products of 5-LO activity are essential to mount an efficient immune response in several infectious and inflammatory conditions14,15,17,19,25. Therefore, we investigated the role of LTB4 during infection with A. xylosoxidans. Using Alox5 −/− mice, we found that downstream mediators of 5-LO activity were crucial for survival, for the efficient clearance of A. xylosoxidans, and control of lung oedema. Indeed, 5-LO deficiency results in similar phenotypes during several infectious or inflammatory diseases13,15,17,19,26,27. To confirm the essential and protective role of LTB4 in lung infection with A. xylosoxidans, we used two strategies. First, a pharmacological restoration of LTB4 function in the susceptible Alox5 −/− infected mice, which almost abolished mortality induced by infection, promoted efficient clearance of A. xylosoxidans from lungs, and reduced lung oedema. Second, we performed a pharmacological inhibition of LTB4 function in the immune competent 129sv mice by the administration of U-75302, a potent and specific BLT1 receptor antagonist19. Inhibition of LTB4 signalling in A. xylosoxidans-infected 129sv mice significantly dampened the host response against the bacteria, increased mice mortality induced by infection, augmented bacterial load and lung oedema. These data agree with previous reports from our laboratory, demonstrating that the administration of LTB4-loaded microspheres enhances the lung immune response against Histoplasma capsulatum 28. In addition, i.n. administration of soluble LTB4 decreases lung oedema and abrogates mortality induced by scorpion venom19. Several groups, including ours, have postulated that the balance between LTB4 and PGE2 is relevant to the control of infectious and inflammatory diseases19,29,30,31. However, the same process is not apparent during infection with A. xylosoxidans. Indeed, we inhibited PGs production and Cysteinyl leukotrienes (CysLTs) signalling by treating infected mice with indomethacin or montelukast respectively (data not shown). We did not observe differences in the survival of treated mice, suggesting that during infections with A. xylosoxidans, PGs and CysLTs did not contribute to changes in bacterial burden, oedema formation, or to the control of leukocyte effector functions, as reported for other conditions19,32,33. The irrelevance of PGs is also supported in part by our finding that infection with A. xylosoxidans induced PGE2 only in the late stages of infection in 129sv mice, coinciding with mononuclear cell infiltration, a relevant source of this lipid mediator34,35. Overall, these data indicate that LTB4 is the predominant 5-LO product involved in the control of infection by A. xylosoxidans, and suggest that neutrophils and resident macrophages are the major source of this lipid mediator35,36.
The LTB4/BLT1 axis is essential for optimal phagocytosis and killing of H. capsulatum 37 and S. pyogenes by macrophages15. In contrast, LTB4 does not seem to increase the phagocytosis of A. xylosoxidans by alveolar macrophages, since the treatment of AMJ2-C11 cells with exogenous LTB4 did not increase the uptake of FITC-labelled bacteria (Fig. 7a). These contrasting results might result from differences in the receptors involved in the bacterial engulfment by the cells, as previous studies demonstrated a crucial role of LTB4 in FcRγ-mediated phagocytosis37,38,39. Although LTB4 did not affect phagocytosis of non-opsonized A. xylosoxidans by AMJ2-C11, exogenous LTB4 was crucial for clearance of A. xylosoxidans infection at 6 or 24 h post-infection in vitro. These results support our in vivo data and other works showing that LTB4 potentiates macrophage microbicide function15,26,40. Some of these studies associate the LTB4-depedent microbicide capacity with the generation of nitric oxide40, reactive oxygen species15,26,40 or release of AMP18,41. Defensins compose an important family of AMPs, subdivided into two main subfamilies, the α- and the β-defensins produced by polymorphonuclear cells and epithelial cells42,43,44,45. Their synthesis and release are up-regulated by lipopolysaccharide, cytokines, growth factors, among other stimuli44. Alveolar macrophages from rabbits produce α-defensin42, thus we investigated whether the increased microbicide activity of AMJ2-C11 cells conferred by LTB4 was due the secretion of α-defensin-1. In fact, we found that LTB4 increased transcription of Defa1 in infected AMJ2-C11 cells; furthermore, expression of Defa1 was 65% higher in lungs of 129sv mice compared to Alox5 −/− mice. Of interest, LTB4 administration to Alox5 −/− mice restored the expression of Defa1, and at the 3rd day post-infection, BALF of infected and LTB4 treated Alox5 −/− mice exhibits comparable levels of α-defensin-1 to that of 129sv mice. To confirm whether the production of α-defensin-1 is the mechanism by which LTB4 improved the killing capacity of AMJ2-C11 cells, we silenced AMJ2-C11 cells using siRNA against Defa1 and evaluated the killing capacity of LTB4-treated cells. The silencing of α-defensin-1 mRNA completely impaired the killing of A. xylosoxidans induced by LTB4. Thus, we conclude that the microbicide effect observed in LTB4-treated AMJ2-C11 cells was due enhanced production of α-defensin-1 conferred by LTB4 signalling. Finally, we proved that α-defensin-1 is cytotoxic to A. xylosoxidans. Using a low dose of α-defensin-1 we observed significant loss of bacterial wall integrity. The role of α-defensin-1 during viral and bacterial infections was described before18,41. However, ours results are the first to demonstrate that LTB4 increases murine alveolar macrophage effector functions by releasing α-defensin-1. Of note, divalent cations, plasma proteins and salts impair the interaction of defensins with the microbial cell wall, and inhibit cell wall permeabilization44,46. This is of great significance since in CF patients, as the CFTR mutation results in chloride imbalance and dysregulation of ion channels, including impaired sodium transport to extracellular space. These alterations may impair the host defence in CF patients due to inhibition of some defensins activity47. Despite of this fact, we observed that even in non-physiological salt concentration, α-defensin-1 retains its function against A. xylosoxidans (Supplementary Fig. S1a). Our results are first evidence of the role of LTB4 signalling in α-defensin-1 release during an opportunistic bacterial lung infection. In Alox5 −/− mice, A. xylosoxidans may induce mortality due to deficiency and/or impaired activity of α-defensin-1.
In summary, our results demonstrate for the first time the crucial and multifaceted role of LTB4 during infection with A. xylosoxidans. This lipid mediator participates in innate immune response by controlling the α-defensin-1 production and consequent clearance of A. xylosoxidans; and by reducing lung oedema formation. These findings suggest that LTB4 may serve as a potential therapeutic agent against A. xylosoxidans infection, especially in CF patients.
Methods
Mice
Age-matched, (24–26 g) 12–15-wk-old male 5-LO-deficient (Alox5 −/−) and wild-type mouse strains, both from 129sv genetic background, were obtained from the Jackson Laboratory (Bar Harbor, ME, USA) and raised at the Faculdade de Ciências Farmacêuticas de Ribeirão Preto, Universidade de São Paulo (FCFRP/USP). Experiments were approved and conducted in accordance with the guidelines of Universidade de São Paulo for the Use and Care of Animals (Number 14.1.390.53.0).
A. xylosoxidans strain
A. xylosoxidans strain LMG 1863 from the Belgian Co-ordinated Collections of Micro-organisms BCCM/LMG were grown on Brain Heart Infusion (BHI) broth agar (Difco, Detroit, MI, USA) at 37 °C for 18 h. The colonies were resuspended in sterile PBS and the number of bacteria was determined spectrophotometrically (optical density at 600 nm)15.
Determination of sublethal inoculum of A. xylosoxidans
The 129sv mice were anesthetized by intraperitoneal (i.p.) administration of ketamine and xylazine (75 and 10 mg/kg of body weight, respectively) and infected intratracheally (i.t.) with 100 µL of increasing inoculums of A. xylosoxidans (2 × 108; 4 × 108; 8 × 108 and 16 × 108). Mortality rate and sublethal inoculum were estimated using the moving average interpolation method20,21. Infected mice were monitored daily and mortality was recorded during the next 14 days. The median lethal and sublethal doses were estimated as 6.2 × 108 and 2 × 108 bacilli, respectively (Supplementary Table 1).
Intratracheal infection and treatments
Both wt and Alox5 −/− mice were anesthetized and i.t. infected with sublethal inoculums of A. xylosoxidans as described above. When necessary, Alox5 −/− mice were treated with LTB4 (Cayman, Ann Arbor, MI, USA) (50 ng/animal in 20 µL in PBS, thrice daily at 8 h intervals) and 129sv mice were intranasally (i.n.) treated with U-75302 (a BLT1 antagonist; Cayman, Ann Arbor, MI, USA) (50 ng/animal in 20 µL in PBS, thrice daily at 8 h intervals). The treatments started one day before infection with A. xylosoxidans. Vehicle-infected or treated (i.t and/or i.n.) mice were used as negative controls.
Experimental design and analyses
In specific experiments, infected 129sv and Alox5 −/− mice, treated or not, were monitored for 14 days to mortality rate determination. For kinetic experiments, anesthetized mice were euthanized by cervical dislocation exsanguinated by cardiac puncture and the bronchoalveolar lavage fluid (BALF) was collected at 1, 3 and 7 days post-infection for total and differential leukocytes counts25 and total protein measurements in the BALF supernatant (Coomassie reagent, Pierce Chemical, Rockford, IL, USA). In another set of experiments, lungs from all groups were collected at the above-mentioned time points without performing a BAL. After weighting and fractionating the lungs, the left upper lobe was processed for bacterial burden15 plating four serial 0.05 mL dilutions on BHI broth agar and incubating at 37 °C for 36 h. Results were expressed as colony forming units (CFU) per gram of lung. The right middle lobe was used for histological analyses following haematoxylin and eosin (HE) staining. ImageJ software (U.S. NIH, Bethesda, MD, USA) was used to calculate the lung area covered by infiltrating cells in five random photomicrograph sections (100x resolution), and tissue damage was calculated as described48. The right upper lobe was homogenized, and the supernatant used (Mixer Homogenizer IKA Labortechnik, Staufen, Germany)17 for TNF-α, IL-1α, monocyte chemoattractant protein-1 (MCP-1) and macrophage inflammatory protein-1α (MIP-1α) quantification by ELISA (R&D Systems, Minneapolis, MN, USA). The right lower lobe was homogenized in 1 mL of ultra-pure water (v/v), followed by the addition of 1 mL of methanol and the supernatant was diluted in 9 mL of ultra-pure water prior to purification using Sep-Pak C18 column (Waters, Milford, MA, USA). The eluted fraction was used for LTB4 and PGE2 quantification using EIA (Enzo Life Science, Farmingdale, NY, USA)19.
Cell culture
Alveolar macrophages, AMJ2-C11 cell lineage was acquired from the Rio de Janeiro Cell Bank, Rio de Janeiro Federal University (BCRJ code 0039). The cells were maintained in DMEM supplemented with 10% SBF and 1% gentamicin and grown at 37 °C, 5% CO2. Prior to experiments the cells were removed using cell scrapers and the total numbers of cells were determined in a Neubauer chamber in trypan-blue 0.4% (Sigma-Aldrich, St. Louis, MO, USA).
Phagocytosis, bacterial killing and gene expression assay
To perform phagocytosis assay, 2 × 108 A. xylosoxidans were labelled with Fluorescein isothiocyanate (FITC) (Amresco, Solon, OH, USA) at 0.1 mg/ml and washed twice with sterile PBS 1x 17,39. 1 × 106 AMJ2-C11 cells were plated on 24 wells culture plates, pre-treated for 15 minutes with LTB4 (1, 10 or 100 nM), infected with FITC-labelled A. xylosoxidans (multiplicity of infection - MOI 50:1 bacilli per macrophage) and incubated at 37 °C, 5% of CO2 for 2 h. After this period, the cells were transferred for a cytometry tubes on ice and washed with cold and sterile PBS 1x. At the time of data acquisition, the cells were mixed with 0.9 mL of trypan blue (4 mg/mL, sodium citrate 14.7 mg/mL, pH 4.4) to chelate fluorescence of non-ingested bacteria. Samples were analysed using a FACSCanto Flow Cytometer (BD Bioscience, San Jose, CA, USA), and the percentage and MFI of FITC+ cells were estimated using the FACSDiva software (BD Bioscience, San Jose, CA, USA). To perform killing assay 2 × 105 AMJ2-C11 cells were plated on 96 wells culture plates, pre-treated for 15 minutes with LTB4 (1, 10 or 100 nM), infected with A. xylosoxidans (MOI 5:1 bacilli per macrophage) and incubated at 37 °C, 5% of CO2 for 6 or 24 h. Then, the cells were lysed with saponin (0.05%) and mixed with 10 μL of a resazurin solution (0.5 mg/mL) (Sigma-Aldrich, St. Louis, MO, USA). The plate was incubated for 8 h at 37 °C, 5% of CO2. The relative fluorescence unit (RFU) was measured by a fluorimeter microplate reader (SpectraMax Paradigm, Molecular Devices, Sunnyvale, CA) at 560–590 nm. The RFU of untreated and infected cells were considered 100% bacterial recovery and the other groups were calculated relative to this group49. For gene expression assays, 5 × 105 cells were plated on 24 wells culture plates, pre-treated for 15 minutes with LTB4 (1, 10 or 100 nm), infected with A. xylosoxidans (MOI 30:1 bacilli per macrophage) and incubated at 37 °C, 5% of CO2 for 30, 120 and 360 minutes. After this period the plate was centrifuged, the supernatant was removed, and the cells stored at −80 °C until RNA isolation.
Quantitative polymerase chain reaction with reverse transcription
Total RNA was extracted according to manufacturer’s recommendations (Purelink, Ambion Invitrogen, Carlsbad, CA, USA), quantified by fluorometric method (Qbit, Invitrogen, Carlsbad, CA, USA) and the complimentary DNA (cDNA) was synthesized from 1 μg of total RNA (High Quality cDNA Reverse Transcriptase Kit, Applied Biosystems, Carlsbad, CA, USA). Fifty nanograms (in vivo) or a hundred nanograms (in vitro) of total cDNA was amplified by quantitative reverse transcriptase-polymerase chain reaction (qRT–PCR) using TaqMan primers for Defa1 (Mm02524428_g1), in a StepOne Plus machine (Applied Biosystems, Foster City, CA, USA). Gapdh (Mm99999915_g1) and Actb (Mm00607939_s1) were used as reference genes (TaqMan® Gene Expression Assay, Applied Biosystems, Carlsbad, CA, USA). Reaction conditions were applied as previously described19. The gene expression was normalized to the expression levels of Actb and Gapdh and the ΔΔCt method was used for the data analysis. The expression data was presented as n-fold difference relative to the control group and their average values were set as 119,49.
RNA interference using silencing RNA (siRNA)
1 × 104 AMJ2-C11 were plated on 96 wells culture plate and maintained at 37 °C, 5% CO2 in serum and antibiotic free DMEM medium until 80% confluence (18–24 h). The cells were transfected with 40 pmol of α-defensin siRNA (m) (sc-40476) or control siRNA-A (sc-37007) using transfection reagent and Opti-MEM reduced serum medium (Santa Cruz biotechnology, Santa Cruz, CA, USA). After 36 h of transfection, cells were pre-treated or not with LTB4 (1, 10 or 100 nM; Cayman, Ann Arbor, MI, USA) for 15 minutes and then infected with A. xylosoxidans (MOI 5:1) for evaluation of killing for 6 h, as described above on killing assay. Efficiency of transfection was 85% for α-defensin, as determined by qRT–PCR. Controls included non-targeting siRNA (scrambled and fluorescent) and no siRNA (with and without lipofectamine).
ELISA for mouse α-defensin-1 detection
The supernatant of BALF from 129sv, Alox5 −/− and Alox5 −/− treated with LTB4, uninfected and infected with A. xylosoxidans at 1 and 3 days post-infection were stored at −80 °C until performed the assay. At the day of quantification, 100 µl of BALF were added in respectively well and the assay was performed according to the manufacturer’s recommendations (SEB705Mu – Cloud-Clone Corp. Houston, TX, USA).
Antimicrobial assay
105 CFU of A. xylosoxidans were incubated with crescent concentrations (5, 50 and 500 pg) of recombinant α-defensin-1 peptide standard from ELISA kit (SEB705Mu – Cloud-Clone Corp. Houston, TX, USA), in PBS 1x supplemented or not with NaCl (150 mM) containing 1% (v/v) BHI (Difco, Detroit, MI, USA) in 96 well plate for 3 h at 37 °C. Then, we added 10 μL of a resazurin solution (0.5 mg/mL) (Sigma, St. Louis, MO, USA) (VF = 200 µl) and we incubated the plate at 37 °C for 8 h. The RFU was measured by fluorimeter microplate reader (560–590 nm) (SpectraMax Paradigm, Molecular Devices, Sunnyvale, CA, USA)49.
Transmission electron microscopy of bacteria
109 CFU of A. xylosoxidans were treated with 500 pg of recombinant α-defensin-1 peptide standard from ELISA kit (SEB705Mu—Cloud-Clone Corp. Houston, TX, USA), in 0.5 ml of PBS 1x containing 1% (v/v) BHI for 2 h at 37 °C. Next steps were performed as previously described50. Bacteria were examined with JEM-100CX II electron microscope (JEOL, Peabody, MA, USA).
Statistical analyses
Data were tested for Gaussian distribution using the D’Agostino-Pearson normality test. Mean values were compared between groups by a one-way or two-way analysis of variance followed by Newman-Keuls or Bonferroni multiple comparison tests. In some cases, student’s t-test was used. Survival differences between groups were calculated using a log-rank test. Analyses were performed using the Prism 6 software (GraphPad Prism, La Jolla, CA, USA). Significances are indicated for p < 0.05.
References
Cohen, T. S. & Prince, A. Cystic fibrosis: a mucosal immunodeficiency syndrome. Nat. Med. 18, 509–519 (2012).
Tummler, B. & Kiewitz, C. Cystic fibrosis: an inherited susceptibility to bacterial respiratory infections. Mol. Med. Today. 5, 351–358 (1999).
Green, H. & Jones, A. M. The microbiome and emerging pathogens in cystic fibrosis and non-cystic fibrosis bronchiectasis. Semin. Respir. Crit. Care Med. 36, 225–235 (2015).
Ronne Hansen, C., Pressler, T., Hoiby, N. & Gormsen, M. Chronic infection with Achromobacter xylosoxidans in cystic fibrosis patients; a retrospective case control study. J. Cyst. Fibros. 5, 245–251 (2006).
Swenson, C. E. & Sadikot, R. T. Achromobacter respiratory infections. Ann. Am. Thorac. Soc. 12, 252–258 (2015).
Carpagnano, G. E., Barnes, P. J., Geddes, D. M., Hodson, M. E. & Kharitonov, S. A. Increased leukotriene B4 and interleukin-6 in exhaled breath condensate in cystic fibrosis. Am. J. Respir. Crit. Care Med. 167, 1109–1112 (2003).
Hansen, C. R. et al. Inflammation in Achromobacter xylosoxidans infected cystic fibrosis patients. J. Cyst. Fibros. 9, 51–58 (2010).
Jabr, S. et al. Quantification of major urinary metabolites of PGE2 and PGD2 in cystic fibrosis: correlation with disease severity. Prostaglandins Leukot. Essent. Fatty Acids. 89, 121–126 (2013).
Mantovani, R. P., Levy, C. E. & Yano, T. A heat-stable cytotoxic factor produced by Achromobacter xylosoxidans isolated from Brazilian patients with CF is associated with in vitro increased proinflammatory cytokines. J. Cyst. Fibros. 11, 305–311 (2012).
Kawai, Y. et al. A typical bacterial ornithine-containing lipid Nalpha-(D)-[3-(hexadecanoyloxy)hexadecanoyl]-ornithine is a strong stimulant for macrophages and a useful adjuvant. FEMS Immunol. Med. Microbiol. 23, 67–73 (1999).
Hutchison, M. L., Bonell, E. C., Poxton, I. R. & Govan, J. R. Endotoxic activity of lipopolysaccharides isolated from emergent potential cystic fibrosis pathogens. FEMS Immunol. Med. Microbiol. 27, 73–77 (2000).
Dennis, E. A. & Norris, P. C. Eicosanoid storm in infection and inflammation. Nat. Rev. Immunol. 15, 511–523 (2015).
Bailie, M. B. et al. Leukotriene-deficient mice manifest enhanced lethality from Klebsiella pneumonia in association with decreased alveolar macrophage phagocytic and bactericidal activities. J. Immunol. 157, 5221–5224 (1996).
Peres, C. M. et al. Inhibition of leukotriene biosynthesis abrogates the host control of Mycobacterium tuberculosis. Microbes Infect. 9, 483–489 (2007).
Soares, E. M. et al. Leukotriene B4 enhances innate immune defense against the puerperal sepsis agent Streptococcus pyogenes. J. Immunol. 190, 1614–1622 (2013).
Medeiros, A. I., Silva, C. L., Malheiro, A., Maffei, C. M. & Faccioli, L. H. Leukotrienes are involved in leukocyte recruitment induced by live Histoplasma capsulatum or by the beta-glucan present in their cell wall. Br. J. Pharmacol. 128, 1529–1537 (1999).
Secatto, A. et al. 5-Lipoxygenase deficiency impairs innate and adaptive immune responses during fungal infection. PLoS One 7, e31701 (2012).
Flamand, L., Tremblay, M. J. & Borgeat, P. Leukotriene B4 triggers the in vitro and in vivo release of potent antimicrobial agents. J. Immunol. 178, 8036–8045 (2007).
Zoccal, K. F. et al. Opposing roles of LTB4 and PGE2 in regulating the inflammasome-dependent scorpion venom-induced mortality. Nat. Commun. 7, 10760 (2016).
Welkos, S. & O’Brien, A. Determination of median lethal and infectious doses in animal model systems. Methods Enzymol. 235, 29–39 (1994).
Weil, C. S. Tables for convenient calculation of Median-Effective Dose (LD50 or ED50) and Instructions for their use. Biometrics. 8, 395–401 (1952).
Medzhitov, R. Origin and physiological roles of inflammation. Nature. 454, 428–435 (2008).
Parker, J. C. & Townsley, M. I. Evaluation of lung injury in rats and mice. Am. J. Physiol. Lung Cell Mol. Physiol. 286, L231–246 (2004).
Widegren, H. et al. LTB4 increases nasal neutrophil activity and conditions neutrophils to exert antiviral effects. Respir. Med. 105, 997–1006 (2011).
Medeiros, A. I. et al. Blockade of endogenous leukotrienes exacerbates pulmonary histoplasmosis. Infect. Immun. 72, 1637–1644 (2004).
Serezani, C. H., Aronoff, D. M., Jancar, S., Mancuso, P. & Peters-Golden, M. Leukotrienes enhance the bactericidal activity of alveolar macrophages against Klebsiella pneumoniae through the activation of NADPH oxidase. Blood. 106, 1067–1075 (2005).
Machado, E. R. et al. Leukotrienes play a role in the control of parasite burden in murine strongyloidiasis. J. Immunol. 175, 3892–3899 (2005).
Nicolete, R., Secatto, A., Pereira, P. A., Soares, E. G. & Faccioli, L. H. Leukotriene B4-loaded microspheres as a new approach to enhance antimicrobial responses in Histoplasma capsulatum-infected mice. Int. J. Antimicrob. Agents. 34, 365–369 (2009).
Peres-Buzalaf, C. et al. Control of experimental pulmonary tuberculosis depends more on immunostimulatory leukotrienes than on the absence of immunosuppressive prostaglandins. Prostaglandins Leukot. Essent. Fatty Acids. 85, 75–81 (2011).
Pedruzzi, G., Das, P. N., Rao, K. V. & Chatterjee, S. Understanding PGE2, LXA4 and LTB4 balance during Mycobacterium tuberculosis infection through mathematical model. J. Theor. Biol. 389, 159–170 (2016).
Lee, S. P., Serezani, C. H., Medeiros, A. I., Ballinger, M. N. & Peters-Golden, M. Crosstalk between prostaglandin E2 and leukotriene B4 regulates phagocytosis in alveolar macrophages via combinatorial effects on cyclic AMP. J. Immunol. 182, 530–537 (2009).
Pereira, P. A. et al. Celecoxib improves host defense through prostaglandin inhibition during Histoplasma capsulatum infection. Mediators Inflamm. 2013, 950981 (2013).
Cabrera, G. et al. Leukotriene C4 increases the susceptibility of adult mice to Shiga toxin-producing Escherichia coli infection. Int. J. Med. Microbiol. 305, 910–917 (2015).
Medeiros, A., Peres-Buzalaf, C., Fortino Verdan, F. & Serezani, C. H. Prostaglandin E2 and the suppression of phagocyte innate immune responses in different organs. Mediators Inflamm. 2012, 327568 (2012).
Sorgi, C. A. et al. Dormant 5-lipoxygenase in inflammatory macrophages is triggered by exogenous arachidonic acid. Sci. Rep. 7, 10981 (2017).
Marleau, S. et al. Role of 5-lipoxygenase products in the local accumulation of neutrophils in dermal inflammation in the rabbit. J. Immunol. 163, 3449–3458 (1999).
Secatto, A. et al. The leukotriene B(4)/BLT(1) axis is a key determinant in susceptibility and resistance to histoplasmosis. PLoS One. 9, e85083 (2014).
Mancuso, P. & Peters-Golden, M. Modulation of alveolar macrophage phagocytosis by leukotrienes is Fc receptor-mediated and protein kinase C-dependent. Am. J. Respir. Cell Mol. Biol. 23, 727–733 (2000).
Peres, C. M. et al. Specific leukotriene receptors couple to distinct G proteins to effect stimulation of alveolar macrophage host defense functions. J. Immunol. 179, 5454–5461 (2007).
Santos, P. C. et al. The pivotal role of 5-lipoxygenase-derived LTB4 in controlling pulmonary paracoccidioidomycosis. PLoS Negl. Trop. Dis. 7, e2390 (2013).
Gaudreault, E. & Gosselin, J. Leukotriene B4 induces release of antimicrobial peptides in lungs of virally infected mice. J. Immunol. 180, 6211–6221 (2008).
Ganz, T. et al. The structure of the rabbit macrophage defensin genes and their organ-specific expression. J. Immunol. 143, 1358–1365 (1989).
Lehrer, R. I., Ladra, K. M. & Hake, R. B. Nonoxidative fungicidal mechanisms of mammalian granulocytes: demonstration of components with candidacidal activity in human, rabbit, and guinea pig leukocytes. Infect. Immun. 11, 1226–1234 (1975).
Ganz, T. Defensins: antimicrobial peptides of innate immunity. Nat. Rev. Immunol. 3, 710–720 (2003).
Ouellette, A. J. et al. Developmental regulation of cryptdin, a corticostatin/defensin precursor mRNA in mouse small intestinal crypt epithelium. J. Cell Biol. 108, 1687–1695 (1989).
Lehrer, R. I. & Lu, W. alpha-Defensins in human innate immunity. Immunol. Rev. 245, 84–112 (2012).
Smith, J. J., Travis, S. M., Greenberg, E. P. & Welsh, M. J. Cystic fibrosis airway epithelia fail to kill bacteria because of abnormal airway surface fluid. Cell. 85, 229–236 (1996).
Lemos, M. P., McKinney, J. & Rhee, K. Y. Dispensability of surfactant proteins A and D in immune control of Mycobacterium tuberculosis infection following aerosol challenge of mice. Infect. Immun. 79, 1077–1085 (2011).
Assis, P. A. et al. Mycobacterium tuberculosis expressing phospholipase C subverts PGE2 synthesis and induces necrosis in alveolar macrophages. BMC Microbiol. 14, 128 (2014).
Harder, J., Bartels, J., Christophers, E. & Schroder, J. M. Isolation and characterization of human beta -defensin-3, a novel human inducible peptide antibiotic. J. Biol. Chem. 276, 5707–5713 (2001).
Acknowledgements
The authors thank Alyne F. Galvão-Meirelles (Faculdade de Ciências Farmacêuticas de Ribeirão Preto/USP), Elaine M. Floriano (Departamento de Patologia e Medicina Legal, Faculdade de Medicina de Ribeirão Preto/USP), Fabiana R. Morais (Centro Multiusuário de Citometria de Fluxo - Faculdade de Ciências Farmacêuticas de Ribeirão Preto/USP) and José A. Maulin, Maria Teresa P. Maglia and Maria Dolores S. Ferreira (Laboratório Multiusuário de Microscopia Eletrônica – LMME, Departamento de Biologia Celular e Molecular e Bioagentes Patogênicos – FMRP/USP) for technical support. For assistance in the image analyses using Image J. we are grateful to PhD Liliana Moura Massis (Departamento de Biologia Celular e Molecular e Bioagentes Patogênicos – FMRP/USP). This work was supported by grants from São Paulo Research Foundation (FAPESP; grant #2014/07125-6), from Conselho Nacional de Desenvolvimento Científico e Tecnológico (CNPq) and Coordenação de Aperfeiçoamento de Pessoal de Nível Superior (CAPES).
Author information
Authors and Affiliations
Contributions
M.K.B.P. planned and performed the experiments, analysed the data, organized the figures and wrote the manuscript. G.A.L., K.F.Z., F.W.G.P., C.F., J.C.F. and P.A.T.P. helped to execute the experiments and analysed the data. L.G.G. helped with the data interpretation and wrote the manuscript. C.A.S. helped with the data interpretation, data analysis and wrote the manuscript. S.G.R. and A.L.C.D. were implicated in the design of the study and analysis of the data. L.H.F. conceived and supervised the project, designed the experiments, helped with the data interpretation, participated in the data analysis and wrote the manuscript. All authors reviewed the manuscript.
Corresponding author
Ethics declarations
Competing Interests
The authors declare that they have no competing interests.
Additional information
Publisher's note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Prado, M.K.B., Locachevic, G.A., Zoccal, K.F. et al. Leukotriene B4 is essential for lung host defence and alpha-defensin-1 production during Achromobacter xylosoxidans infection. Sci Rep 7, 17658 (2017). https://doi.org/10.1038/s41598-017-17993-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-017-17993-9
This article is cited by
-
CD14 signaling mediates lung immunopathology and mice mortality induced by Achromobacter xylosoxidans
Inflammation Research (2022)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.