Abstract
Work disability affects quality of life, earnings, and opportunities to contribute to society. Work characteristics, lifestyle and sociodemographic factors have been associated with the risk of work disability, but few multifactorial algorithms exist to identify individuals at risk of future work disability. We developed and validated a parsimonious multifactorial score for the prediction of work disability using individual-level data from 65,775 public-sector employees (development cohort) and 13,527 employed adults from a general population sample (validation cohort), both linked to records of work disability. Candidate predictors for work disability included sociodemographic (3 items), health status and lifestyle (38 items), and work-related (43 items) variables. A parsimonious model, explaining > 99% of the variance of the full model, comprised 8 predictors: age, self-rated health, number of sickness absences in previous year, socioeconomic position, chronic illnesses, sleep problems, body mass index, and smoking. Discriminative ability of a score including these predictors was high: C-index 0.84 in the development and 0.83 in the validation cohort. The corresponding C-indices for a score constructed from work-related predictors (age, sex, socioeconomic position, job strain) were 0.79 and 0.78, respectively. It is possible to identify reliably individuals at high risk of work disability by using a rapidly-administered prediction score.
Similar content being viewed by others
Introduction
According to the International Labour Organization, over a billion people worldwide suffer from a disability and 80% of these persons are of working age1. In OECD countries, 6% of working-age people have exited the labor market due to a disability2. Apart from significant impacts on a person’s life chances, work disability is a problem for the society due to lost productivity. The prevention of work disability is becoming increasingly important due to population aging, as an increasing number of people are spending more years with functional health loss and disability, leading to an absolute expansion of morbidity3.
Recent studies of risk factors for work disability have confirmed the importance of older age4, low socioeconomic status5,6, a history of sickness absences7,8, unhealthy behaviors (smoking and high alcohol consumption)9,10,11, and stressful characteristics of work, such as high job strain and excessive job demands12,13. While these risk factors are useful in evaluating the risk of work disability at a population level, more sensitive and specific prediction instruments are needed to assess an individual’s disability risk. Multifactorial prediction algorithms or scores that take into account the combined effect of multiple risk factors have been used to identify people at high risk of chronic diseases, particularly cardiovascular disease14,15,16, but to date few multifactorial scores are available to identify those at increased risk of work disability. Multifactorial prediction models have been introduced for prediction of work disability in the US Army17 and sickness absence in working populations18. However, we are not aware of any validated multifactorial prediction score for work disability in the general working population. Such scores could facilitate the identification of individuals who are most likely to benefit from targeted interventions.
Using individual-level data on sociodemographic variables, health status and lifestyle, and work-related variables, we developed and validated two parsimonious and rapidly administered prediction algorithms for all-cause work disability, one based on all available data and the other using work-related variables only.
Results
Descriptive characteristics
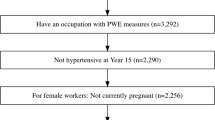
We used data from two large prospective cohort studies, the Finnish Public Sector study (FPS) and the Health and Social Support (HeSSup) study19,20,21. Sample selection and the descriptive characteristics for the development (N = 65,775, mean age 43.7 years, 80% women) and validation (N = 13,527, mean age 39.5 years, 57% women) cohorts are provided in Fig. 1 and Table 1 (see Appendix 1 for the wordings of the questionnaire items). Overall, the development cohort and the validation cohort were quite similar, with the exception of more equal gender distribution and younger participants in the validation cohort. During the mean follow-up of 8.6 years, 5332 (8%) people were granted a disability pension in the development cohort. In the validation cohort mean follow-up was 9.5 years and 877 (6%) participants were granted disability pension. ICD-10 based reasons for granted full disability pensions are shown in Table 2.
Development of prediction score from all available data
We used parametric survival analysis to model the risk of work disability. Based on Akaike’s Information Criterion and graphical evaluation, lognormal distribution showed the best fit for modeling the baseline hazard function, and all models were therefore fitted with the lognormal distribution.
The unadjusted bivariate associations between risk factors and work disability are illustrated in the Manhattan plot of Fig. 2. Nearly all variables were significantly associated with work disability. Age, socioeconomic position, health and disease-related items had the strongest associations. Many of the items related to work characteristics, team climate, and management were associated with work disability, but not as strongly as health-related items. In a redundancy analysis, social capital at work could be predicted with high accuracy with all other available variables and was therefore excluded from all further analysis. There were no other redundant variables.
The full model including all the non-redundant variables explained 21.7% of the variance in work disability. We then used backward stepwise regression analyses to obtain a more parsimonious prediction model, and found that almost all the variance (>99%) of the full model was captured by 8 variables: age, self-rated health, the number of long sickness absences in the previous year, socioeconomic position, chronic illnesses, sleep disturbance as indicated by the Jenkins scale, BMI and smoking. To determine which specific items of the Jenkins scale predicted work disability, we specified a new full model that included all the individual items instead of the summary variable. Only the item assessing difficulty falling asleep remained as a robust predictor and thus replaced the Jenkins scale in the parsimonious prediction model. Appendix 2 shows coefficients for the full model with all individual items from Jenkins scale, and the final model with 8 predictors. Adding specific chronic conditions, instead of the composite of having a history of any chronic disease, in the model as predictors did not improve the variance explained.
To refine the parsimonious prediction model to a multifactorial prediction score that allows linear and non-linear associations between the predictors and work disability, all the 8 continuous predictors were transformed into categorical variables. We categorized age into 5-year bands from 35 to 55 years plus a category of over 55 years. BMI was categorized according to the WHO classification22 into underweight (BMI < 18.5 kg/m2), normal weight (BMI = 18.5–24.9 kg/m2), overweight (BMI = 25–29.9 kg/m2) and obese (BMI ≥ 30 kg/m2). All the 6 other predictors were categorized according to their response options. We then fitted a model with the 8 categorical predictors (Table 3). While most of the associations between the predictors and work disability were linear or nearly linear, this was not the case for BMI, as both obesity and underweight were associated with an elevated risk of work disability. To assess internal validity, we fitted the 8-factor model separately for the two subsamples of FPS. The hazard ratios were similar in both subsamples in addition to the final combined sample, suggesting that the model was internally valid and reproducible (Table 3). As a sensitivity analysis, we also compared the hazard ratios of the final prediction score from the three best performing parametric models to those from Cox regression model. The log-normal model was again the closest match to the Cox model (Appendix 3).
Figure 3 shows a nomogram of the weights and points of the 8-factor prediction score allowing estimation of an individual’s risk manually without having to resort to the actual formula (for details of the nomogram, see Appendix 4). To illustrate risk accumulation, Fig. 4 shows how each additional risk factor increases the absolute risk of disability starting from a risk profile with minimum risk factors at age 45–49 years. In that group, the risk of disability was 1.5%. The risk increased after each additional risk factor, being 2.1% if the person smoked, 3.0% if also obese, 4.5% if having trouble falling asleep, 10.5% with prevalent chronic disease, 24.1% if socioeconomic position was additionally low, and 59.3% with a history of 3 or more sickness absence during the preceding 12 months. For a person with all these risk factors plus poor self-rated health, the risk of work disability during the next 10 years was as high as 93.3%.
Validation of the 8-factor prediction score
Further internal validation in the combined FPS sample supported the high predictive performance of the score. The C-index was 0.840 (95% confidence interval: 0.834 to 0.845) and internal validation with bootstrapping indicated minimal over-fitting with the optimism-corrected C-index being 0.838.
External validation was done using data from the HeSSup survey which did not include exactly the same questions as those used in the survey of the development sample (for the wordings of the questionnaire items, see Appendix 1). The main differences were in the questions on socioeconomic position and sleep problems. In HeSSup, socioeconomic position was assessed by educational level (1 = university degree, 7 = no vocational degree), and sleep by the question “How well do you usually sleep?” (1 = well, 4 = poorly). Responses for educational level in the validation cohort were treated as equal to those of socioeconomic position in the development cohort. As the response format for the sleep question was a 4-rather than 6-point scale, the responses were rescaled to a 6-point scale using rounding to the closest integer. Despite these minor differences, the 8-item score yielded a high C-index of 0.828 (95% confidence interval: 0.815 to 0.841) in the independent validation sample.
The absolute accuracy of the prediction score was then evaluated using calibration plots. As shown in Fig. 5, these plots suggested a high correspondence between the predicted and the observed risk both in the development and validation cohorts. For example, in the bottom two deciles of the score the predicted risks were 0.4% and 0.9% and the observed risks 0.5% and 0.8% in the development sample. In the validation sample, the corresponding predicted risks were 0.4% and 0.6% and the observed risks 0.2% and 0.4%, respectively. The predicted risk in the top decile was slightly overestimated: in development sample the predicted risk for that decile was 43.0%, whereas the observed risk was 44.6%. In the validation sample the corresponding risks for the same decile were 30.9% and 30.7%, respectively.
Development of an alternative score using work-related variables
As workplace questionnaire surveys often include only questions on basic demographic characteristics and work-related issues, we created another prediction model using only age, sex, socioeconomic status, and all work-related factors as candidate variables. Model development was based on following the same procedure as with our main prediction model. Factors explaining 99% of the variance of full model were age, socioeconomic position and job strain scale. C-index in internal validation was 0.784 (95% confidence interval: 0.778 to 0.789). External validation with the data from the HeSSup survey yielded a C-index of 0.774 (95% confidence interval: 0.760 to 0.789) (for model coefficients, see Appendix 5). Other work-related factors, such as shift work and scales of effort-reward imbalance at work, procedural and relational justice, team climate inventory, including participatory safety, support for innovation, vision, and task orientation, did not improve prediction. We then examined whether the predictive ability of work-related score can be improved by disaggregating the job strain subscales and developing a prediction algorithm using items that are most strongly related to work disability. Using this procedure, one item from both the job demand (“I am expected to do unreasonable amount of work”) and job control (“My work involves a lot of repetitive tasks”) scales were chosen. The C-index for a model including these 2 items in addition to age and socioeconomic position was 0.788 (95% confidence interval: 0.782 to 0.793) in internal validation and 0.780 (95% confidence interval: 0.765 to 0.794) in external validation. Figure 6 shows the related nomogram (for coefficients and calibration plots, see Appendix 6).
Finally, we developed a prediction model from a pool of demographic variables and all work-related items (rather than scales). In this analysis, a parsimonious model included the following 4 statements or questions in addition to age and socioeconomic position: “I am expected to do unreasonable amount of work”, “My work involves a lot of repetitive tasks”, “I have a say in the tasks included in my work”, and “Your supervisor shows concern for your rights as an employee”. The C-index did not improve (0.789; 95% confidence interval: 0.783 to 0.795). This model could not be externally validated as data on one of the items were not available in the validation cohort.
Internet-based tool to estimate the risk of work disability
As way to disseminate these findings, we developed a web-based questionnaire for the calculation of a personalized 10-year work disability risk based on the validated 8-factor score and the validated score using work-related variables (available as an online appendix in the journal’s web-page: https://doi.org/10.1038/s41598-017-13892-1).
Discussion
We developed and validated, internally and externally, a new risk prediction score for work disability. The score is based on eight variables: age, self-rated health, number of sickness absences in the previous year, socioeconomic position, presence of chronic illnesses, having difficulty falling asleep, BMI, and smoking. The score performed well in the development cohort and in the independent validation cohort, with discriminative ability of 0.84 and 0.83, respectively. In addition, the predicted risks were in accordance with the observed risks through all risk deciles in both cohorts and the score captured a wide range of absolute risks. In the age group of 45 to 49-years, for example, absolute risk of work disability was 1.5% for a person with optimal risk profile and 93.3% for one with all measured risk markers. Alternative risk prediction scores, based on demographic characteristics and work-related factors, had more modest predictive abilities, although the observed c-statistics in the range of 0.70 to 0.80 are still considered to indicate acceptable discrimination.
All variables included in the prediction scores have previously been associated with disability pension. Poor self-rated health, for example, predicted disability pension from any cause even after controlling for various health and working conditions related factors23. Earlier findings have also identified age and a history of sickness absences as predictors of disability pension24,25. Similarly smoking and obesity have been associated with an increased risk of early exit from workforce9,26. The predictive performance of our 8-factor score, which is applicable across occupations or branches of occupation, is comparable to that for the 15-factor soldiers’ disability risk, the C-index being 0.828 in the present study and 0.860 for soldiers’ score in a US army population. The predictive performance of our score was at the same level as those for standard prediction scores for chronic conditions that are currently recommended internationally for disease prevention in clinical practice27,28. The C-statistics for the widely used U.S. Framingham Cardiovascular Risk Scores29,30 the European equivalent, SCORE predictor14, and the UK QD-Score for prediction of diabetes15, for example, have been slightly above and below 0.8. This supports the feasibility of our score in real-life settings.
There is a large body of research on work characteristics and work disability. In the present study, a wide range of validated questionnaire scales on work-related stress, team working, leadership and organizational justice were included in the baseline assessment31,32,33,34. Interestingly, these work characteristics were not retained in our final 8-factor prediction algorithm, suggesting that work characteristics may be more distal in the causal pathway and not as strongly predictive of an individual’s risk of work disability compared to more proximal risk factors such as health status, lifestyle habits and socioeconomic position. Of the multiple work-related concepts, job strain, the most widely used model of psychosocial work stress32 had better predictive capacity than more recent derived characteristics, such as effort-reward imbalance34, procedural and relational justice35, and team climate36.
It is important to make a distinction between risk prediction and targets of intervention to prevent work disability. The purpose of risk prediction in this context is to identify a group of people at increased risk of work disability. The items in the multifactorial score are not necessarily the best targets for prevention; indeed, they can even be risk markers (e.g., HDL-cholesterol is a component of the Framingham risk score for prediction of cardiovascular disease, but reduction of LDL-cholesterol is the main target of lipid-lowering treatments). Further research is needed to develop effective, cost-effective and safe measures to reduce the occurrence of work disability in groups at risk.
Strengths and limitations
To the best of our knowledge, our 8-factor model is the first internally and externally validated multifactorial prediction score for work disability. That the variables included in the model can be easily assessed by health care professionals or by the individuals themselves facilitates the use of the score in multiple settings ranging from occupational and primary health care to web-based applications. Early detection of individuals at high risk is a precondition to effective targeted interventions to prevent work disability and a basis for developing cost-effective strategies to lengthening work career. Our validated score for 10-year prediction of work disability could serve as a screening tool for clinicians and occupational health professionals in identifying those at the greatest risk for work disability. Such instruments are needed in the process of work disability evaluation, which has been demonstrated to show high variability and low reliability37, especially in cases were no such instruments are used. Further research is needed to evaluate potential benefits and harms of the usage of the screening tool in diverse working populations and the feasibility of our score as a web-based tool to enable employees’ self-evaluation of their risk for work disability.
The present study has some limitations. Both the development and validation cohorts were based in Finland where ascertainment of work disability was possible with linkage to comprehensive records from the national pension register with virtually full coverage on all gainful employment38. However, the generalizability of our score should be tested in other settings. Even though the calibration of the prediction score proved to be high across the observed risk range, most of those risks were small −70% of the risks in the development cohort were smaller or equal to 10% risk of work disability in 10 years. A lifetime prediction model would identify are large proportion of people at high risk, although the predictive validity of short scores for longer prediction windows is likely to be lower.
Also, the validation cohort differed from the development cohort on the assessment of socioeconomic position and sleep disturbances. In the development cohort socioeconomic position was measured using current occupational status, whereas in the validation cohort the measure was occupational education. The measures might capture different parts of the underlying concept. However, the validation study showed that both measures of socioeconomic position performed equally well. Similarly, the questions on sleep relate to slightly different features of sleep in the two cohorts, although the weight given to sleep problems in the model was modest and therefore such differences are unlikely to affect the results in a significant way.
Finally, the process of evaluating work disability by local authorities may affect the generalizability of our findings. Although work disability is defined by impairment, unlike commonly used clinical outcomes, such as adverse cardiac/cerebrovascular events and mortality, receipt of a disability pension is additionally dependent on non-medical factors, such as disability pension regulations, the work environment, the nature of the job, and the extent to which the workplace is prepared to accommodate the disability. There is a need for further research to examine the predictive validity of our score across populations and countries with different labor market regulations.
Conclusions
We developed and validated internally and externally a new 10-year prediction score for work disability which included information from sociodemographic and lifestyle factors. The 8-item score showed high predictive performance and discriminative ability in two large independent samples from Finland. An alternative score including only demographic and work-related items had slightly lower discriminative ability. As easy-to use scores, these measures could be valuable screening tools for identifying those at most risk of health-related early exit from the workforce, but further research is needed on benefits and harms and generalizability across different labor market settings.
Data and Methods
Study design and participants
We used individual-level data from the Finnish Public Sector study (FPS) for the development of the prediction score (‘development’ cohort). We then validated this score in an independent, population-based cohort study, the Health and Social Support study (HeSSup) (‘validation’ cohort). Both studies have been described in detail elsewhere19,20,21.
Briefly, the participants of FPS were employees in the municipal service of 10 Finnish towns and 21 public hospitals, including a range of professions (city mayors, teachers, cleaners, construction workers, and so on). The study was approved by the Ethic committee of the Hospital District of Helsinki and Uusimaa. A wide set of potential predictors of work disability was assessed using a standardized survey in 2000–2002 when 48,598 participants responded (response 68%) and in 2004 when 48,076 responded (response 66%). We excluded participants who were on a long-term sickness absence (≥90 days), disability pension, or retired at the time of responding (N = 478 in 2000–2002 and N = 578 in 2004) as well as those missing the personal identification number used for data linkage (N = 595 in 2000–2002 and N = 481 in 2004). We also excluded those participants from the second survey who had taken part in the first survey (N = 28,767). Thus, the sample of the 2000–2002 survey included 47,525 employees (subsample 1), and the 2004 survey included 18,250 employees (subsample 2). We combined the subsamples to form the final development sample. The combined sample included 65,775 employees. We linked these participants to the electronic records of work disability, sickness absence, statutory retirement and mortality registers until the end of 2011 using personal identification numbers assigned to all Finnish citizens, an exercise that was successful for all participants. A flow chart of the sample selection is shown in Fig. 1.
HeSSup is a prospective cohort study that began in 199820 and targeted a population sample representative of the Finnish population in four age groups: 20–24, 30–34, 40–44, 50–54 years at baseline. The study was approved by the Turku University Central Hospital’s Ethics Committee. A total of 25,898 people participated in the baseline survey, of whom 14,683 were employed. Of them, we excluded those who did not give consent to link their responses to electronic records of work disability (N = 1055), or were on a long-term sickness absence ( ≥ 90 days), disability pension or retired at the time of responding or died before the start of the follow-up (N = 101). Thus, the final validation data included 13,527 participants who were linked to records of disability pension, sickness absence, retirement and death until 31 December 2008.
All participants provided written informed consent. Further, this study and its methods were conducted according to the guidelines of the Helsinki declaration.
Measurement of predictors of work disability
The FPS survey included 82 questions assessing participants’ sociodemographic characteristics, health status, lifestyle, and working conditions. For a full list of the items see Appendix 1. These questions relate to the following 23 single- or multi-item candidate predictors.
Sociodemographic factors were derived from employers’ registers and included sex, age, and socioeconomic position. Socioeconomic position was derived from the participants’ job titles using the International Standard Classification of Occupations (ISCO). The ISCO has ten categories ranging from 1 (managers) to 9 (elementary occupations) with a separate category for armed force occupations. With categories 6–8 (skilled agricultural workers, craft and trade workers, plant and machine operations) referring to similar skill level occupations, and relatively few participants falling into those categories, they were combined to form a single “process worker” category. Further, none of the participants were employed in armed forces, so the final measure for socioeconomic position was (1–7): 1 = manager/higher official, 2 = senior specialist, 3 = specialist, 4 = office worker, 5 = service worker, 6 = process worker, and 7 = other/elementary occupations.
Chronic diseases
Participants were asked to report physician-diagnosed diseases from a list of common ailments. We matched the diseases with the 30 leading contributors of global disability-adjusted life years3. The list of diseases included bronchial asthma, myocardial infarction, angina pectoris, cerebrovascular diseases, migraine, depression, and diabetes. Diseases that were among the leading causes, but not asked in the survey, included diseases such as sense organ diseases, lung cancer, and a range of severe communicable diseases. We formed a new variable for chronic diseases by summing the number of reported chronic diseases. The number ranged from 0 to 7 with 180 individuals reporting 4 or more (who were collapsed to the category of “3 or more”).
Health status and health behaviors
Self-rated health was assessed using a 5-point scale (1 = good, 2 = rather good, 3 = moderate, 4 = rather poor, 5 = poor). The 12-item general health questionnaire (GHQ) was used to assess psychological distress39. Responses for GHQ were given on a 4-points Likert scale (i.e., 1 = better than usual, 4 = much worse than usual) and a mean response was used in analyses. Sleep problems were assessed using the four item Jenkins sleep problem scale40 and responses were given on a 6-point Likert scale (i.e., 1 = never, 6 = almost every night). Alcohol consumption was assessed with question on how much beer, wine, and spirits the participants consumed in a week. The average for each beverage was transformed into units of alcohol per week (range from 0 to 226 units a week and a median of 3) and the variable was truncated from the top to interquartile range (IQR) + IQR*3, so that the range was from 0 to 21. Other measures included smoking (0 = non-smoker/former smoker, 1 = current smoker) and leisure-time physical inactivity (0 = active, 1 = sedentary). Self-reported height and weight were used to calculate body mass index (BMI; weight in kilograms divided by height in meters squared). All spells of sickness absences longer than 9 days during the previous year were obtained from electronic health records curated by the Social Insurance Institution of Finland. The number of sickness absences had a range from 0 to 5 with 68 individuals reporting 4 or 5 spells of absence. Observations measuring 4 or over were recoded as 3, resulting in a range from 0 to 3.
Work-related factors
The FPS questionnaire included questions about shift work (0 = no, 1 = yes), night shift (0 = no, 1 = yes), and multi-item scales of job demand (a 3-item scale), job control (a 6-item scale), job effort (1 items) and job reward (a 3-item scale) with a 5-point Likert scale as the response format. The partial scales used for job demand and job control have been shown to be in high agreement with the full scales41. The mean score of job demand and job control scales were used to construct a measure of job strain42. Job strain was defined as 1, if job demand was above the median and job control below the median, and 0 otherwise. For job rewards we averaged the responses and the ratio of effort to rewards was used to form a dichotomized measure of effort-reward imbalance at work, with value 1 if the ratio was over 1, and 0 otherwise43.
Team work and management
These measures included procedural (7 items) and relational justice (6 items)35, and a short version of team climate inventory (TCI)44 which includes four subscales labelled as participatory safety (4 items), support for innovation (3 items), vision (4 items), and task orientation (3 items). Also included was a scale for social capital at work (8 items), which consisted of a combination of items from the four TCI scales. Responses to the items of procedural and relational justice, and TCI scales were given using a 5-point Likert scale. The mean of the responses on each scale were used in analysis.
Ascertainment of work disability
In Finland, earnings-related pension security covers almost all gainful employment. We obtained records of the starting date and type of all pensions from the national register of the Finnish Centre of Pensions38. The Finnish Centre of Pensions has a statutory obligation to keep records of pensions and produce statistics from all registries and pension providers in Finland. A full disability pension can be granted for a person whose capacity for work is severely impaired by at least 60% due to a disease, injury or handicap. These records have been widely used in a research context11,45,46. All the employees in both studies were insured in some pension scheme and therefore disability pension records were available for all study participants. The examined outcome was full time disability pensions that could be temporary or permanent.
Statistical Analysis
We combined the two FPS subsamples to form the development cohort of 65,775 employees. We imputed missing data (2.8% of all observations) on predictors using single imputation with predictive mean matching47.
We used Akaike’s Information Criterion and graphical evaluation to compare how well different parametric distribution fit the baseline hazard function. Then we examined bivariate associations between all the predictor items and summary variables using parametric survival models. Reducing the number of predictors based on unadjusted association with the outcome is not recommended by the TRIPOD statement, as it may lead to rejection of important predictors based on nuances in the data48. Therefore we included all the variables in the following analyses, even if there was no significant association in the bivariate analysis. Before further model specification, we ran a redundancy analysis to exclude variables that could be readily predicted using all other variables. Following the procedure of Hijazi and colleagues49, we specified a parametric survival model that included all 23 candidate variables as predictors (‘full model’). To obtain a more parsimonious model, we derived the model-predicted work disability risks for each individual based on the full model. We then used backward stepwise ordinary least squares regression in which we predicted risks derived from the full model. In the first step all original variables used in the full model were retained in the model, and R2 equals unity by design. We then removed as many variables as possible, while retaining a R2 value close to 100%. The satisfactory level of R2 obtained this way is a balance between a model that explains most of the variance of the full model (more variables leads to higher R2) and the number of variables retained in the final model (fewer variables leads to a more parsimonious model). If any summary variables were left in the model after the backward stepwise regression analysis, we defined the full model again with the summary variable(s) broken down to individual items. We then repeated the analysis as described above. This allowed us to identify the individual items that explained most of the variance of the full model and enabled us to form a parsimonious model. The predictors that were left in the model after these steps formed the final multifactorial prediction score – again, a parametric survival model.
The performance of the final prediction score was evaluated using Harrell’s C-index, which is the concordance between predicted and observed survival47. To estimate the degree of overfitting, the model was first internally validated using the bootstrapping method48, and then externally validated by assessing the performance of the score in the HeSSup cohort study. Calibration of the model - how accurately the predicted absolute risks correspond to observed absolute risks - was assessed using calibration plots, separately for the development data and validation data. All analyses were performed using R 3.2.3 (packages: mice, rms and Hmisc).
Data sharing
Statistical syntax and anonymized data on predictors are available for bona fide researchers. Individual-level data on disability pensions are owned by the Finnish Institute of Occupational Health and University of Helsinki; no sharing of those data are permitted.
Change history
16 November 2018
A correction to this article has been published and is linked from the HTML and PDF versions of this paper. The error has not been fixed in the paper.
References
ILO. Disability Inclusion Strategy and Action Plan 2014–17 (2015).
OECD. Sickness, Disability and Work: Breaking the Barriers: A Synthesis of Findings across OECD Countries. (OECD Publishing, 2009). https://doi.org/10.1111/j.1468-246X.2011.01406.x.
Kassebaum, N. J. et al. Global, regional, and national disability-adjusted life-years (DALYs) for 315 diseases and injuries and healthy life expectancy (HALE), 1990–2015: a systematic analysis for the Global Burden of Disease Study 2015. Lancet 388, 1603–1658 (2016).
Mykletun, A. et al. A population-based cohort study of the effect of common mental disorders on disability pension awards. Am. J. Psychiatry 163, 1412–8 (2006).
Mansson, N. O., Rastam, L., Eriksson, K. F. & Israelsson, B. Socioeconomic inequalities and disability pension in middle-aged men. Int. J. Epidemiol. 27, 1019–1025 (1998).
Stronks, K., van de Mheen, H., van den Bos, J. & Mackenback, J. P. The interrelationship between income, health and emplyment status. Int. J. Epidemiol. 26, 592–600 (1997).
Alexanderson, K. et al. Diagnosis-specific sick leave as a long-term predictor of disability pension: a 13-year follow-up of the GAZEL cohort study. J. Epidemiol. Community Health 66, 155–9 (2012).
Labriola, M. & Lund, T. Self-reported sickness absence as a risk marker of future disability pension. Prospective findings from the DWECS/DREAM study 1990-2004. Int. J. Med. Sci. 4, 153–158 (2007).
Korhonen, T., Smeds, E., Silventoinen, K., Heikkilä, K. & Kaprio, J. Cigarette smoking and alcohol use as predictors of disability retirement: A population-based cohort study. Drug Alcohol Depend. 155, 260–266 (2015).
Lallukka, T., Rahkonen, O., Lahelma, E. & Lahti, J. Joint associations of smoking and physical activity with disability retirement: a register-linked cohort study. BMJ Open 5, e006988 (2015).
Salonsalmi, A., Laaksonen, M., Lahelma, E. & Rahkonen, O. Drinking habits and disability retirement. Addiction 107, 2128–2136 (2012).
Canivet, C. et al. Can high psychological job demands, low decision latitude, and high job strain predict disability pensions? A 12-year follow-up of middle-aged Swedish workers. Int. Arch. Occup. Environ. Health 86, 307–319 (2013).
Lahelma, E. et al. Working conditions as risk factors for disability retirement: a longitudinal register linkage study. BMC Public Health 12, 309 (2012).
Conroy, R. M. et al. Estimation of ten-year risk of fatal cardiovascular disease in Europe: The SCORE project. Eur. Heart J. 24, 987–1003 (2003).
Hippisley-Cox, J., Coupland, C., Robson, J., Sheikh, A. & Brindle, P. Predicting risk of type 2 diabetes in England and Wales: prospective derivation and validation of QDScore. Bmj 338, b880–b880 (2009).
Sullivan, L. M. & Wilson, P. Validation of the Framingham Coronary Heart Disease prediction score. Jama 286, 180–187 (2001).
Nelson, D. A., Wolcott, V. L. & Kurina, L. M. Prediction of all-cause occupational disability among US Army soldiers. Occup. Environ. Med. 73, 442–451 (2016).
Roelen, C. et al. Development and validation of a prediction model for long-term sickness absence based on occupational health survey variables. Disabil. Rehabil. 8288, 1–8 (2016).
Kivimäki, M. et al. Socioeconomic position, co-occurrence of behavior-related risk factors, and coronary heart Disease: The finnish public sector study. Am. J. Public Health 97, 874–879 (2007).
Korkeila, K., Suominen, S., Ahvenainen, J., Ojanlatva, A. & Helenius, H. Non-response and related factors in a nation-wide health survey. Eur. J. Epidemiol. 17, 991–999 (2001).
Vahtera, J. et al. Organisational downsizing, sickness absence, and mortality: 10-town prospective cohort study. Bmj 328, 555–0 (2004).
WHO. Obesity: Preventing and Managing the Global Epidemic. (2000).
Pietiläinen, O., Laaksonen, M., Rahkonen, O. & Lahelma, E. Self-rated health as a predictor of disability retirement - the contribution of ill-health and working conditions. PLoS One 6, (2011).
Ishtiak-Ahmed, K., Perski, A. & Mittendorfer-Rutz, E. Risk markers of all-cause and diagnosis-specific disability pension–a prospective cohort study of individuals sickness absent due to stress-related mental disorders. BMC Public Health 14, 12 (2014).
Wallman, T. et al. Sick-leave track record and other potential predictors of a disability pension. A population based study of 8,218 men and women followed for 16 years. BMC Public Health 9, 104 (2009).
Robroek, S. J. W. et al. The contribution of overweight, obesity, and lack of physical activity to exit from paid employment: A meta-analysis. Scand. J. Work. Environ. Heal. 39, 233–240 (2013).
Piepoli, M. F. et al. European Guidelines on cardiovascular disease prevention in clinical practice. Eur. Heart J. 37, 2315–2381 (2016).
Goff, D. C. et al. ACC/AHA guideline on the assessment of cardiovascular risk: A report of the American college of cardiology/American heart association task force on practice guidelines. J. Am. Coll. Cardiol. 63, 2935–2959 (2014).
Wilson, P. W. F. et al. Prediction of coronary heart disease using risk factor categories. Circulation 97, 1837–1847 (1998).
Anderson, K. M., Odell, P. M., Wilson, P. W. F. & Kannel, W. B. Cardiovascular disease risk profiles. Am. Heart J. 121, 293–298 (1991).
Greenberg, J. A Taxonomy of Organizational Justice Theories. Acad. Manag. Rev. 12, 9–22 (1987).
Karasek, R. A. Job Demands, Job De- cision Latitude, and MentalStrain: Implica- tions for Job Redesign. Adm. Sci. Q. 24, 285–308 (1979).
Anderson, N. & West, M. Measuring climate for work group innovation:development and validation of the team climate inventory. J. Organ. Behav. 19, 235–258 (1998).
Siegrist, J. Adverse health effects of high-effort / low-reward conditions. J. Occup. Health Psychol. 1, 27–41 (1996).
Moorman, R. H. Relationship Between Organizational Justice and Organizational Citizenship Behaviors: Do Fairness Perception Influence Employee Citizenship? J. Appl. Psychol. 76, 845–855 (1991).
West, M. & Anderson, N. Innovation in top management teams. J. Appl. Psychol. 81, 680–693 (1996).
Barth, J. et al. Inter-rater agreement in evaluation of disability: systematic review of reproducibility studies. Bmj j14, https://doi.org/10.1136/bmj.j14 (2017).
Finnish C for Pensions. Finnish Centre for Pensions. Available at: http://www.etk.fi/en/statistics-2/statistics/producer-of-statistics/. (Accessed: 1st December 2016).
Goldberg, D. P. et al. The validity of two versions of the GHQ in the WHO study of mental illness in general health care. Psychol. Med. 27, 191–197 (1997).
Jenkins, C. D., Stanton, B. A., Niemcryk, S. J. & Rose, R. M. A scale for the estimation of sleep problems in clinical research. J. Clin. Epidemiol. 41, 313–321 (1988).
Fransson, E. I. et al. Comparison of alternative versions of the job demand-control scales in 17 European cohort studies: the IPD-Work consortium. BMC Public Health 12, 62 (2012).
Karasek, R. & Theorell, T. Healthy work: stress, productivity, and the reconstruction of working life. (Basic Books, 1990).
Siegrist, J. et al. The measurement of effort-reward imbalance at work: European comparisons. Soc. Sci. Med. 58, 1483–1499 (2004).
Kivimaki, M. & Elovainio, M. A short version of the Team Climate Inventory: Development and psychometric properties. J. Occup. Organ. Psychol. 241–246, https://doi.org/10.1348/096317999166644 (1999).
Lahti, J., Holstila, A., Mänty, M., Lahelma, E. & Rahkonen, O. Changes in leisure time physical activity and subsequent disability retirement: A register-linked cohort study. Int. J. Behav. Nutr. Phys. Act. 13, 99 (2016).
Von Bondorff, M. B. et al. Early life origins of all-cause and cause-specific disability pension: Findings from the Helsinki birth cohort study. PLoS One 10, 1–12 (2015).
Harrell, F. E. Regression Modeling Strategies: With Applications to Linear Models, Logistic and Ordinal Regression, and Survival Analysis. (Springer, 2015).
Moons, K. G. M. et al. Transparent Reporting of a multivariable prediction model for Individual Prognosis Or Diagnosis (TRIPOD): Explanation and Elaboration. Ann. Intern. Med. 162, W1–W73 (2015).
Hijazi, Z. et al. The novel biomarker-based ABC (age, biomarkers, clinical history)-bleeding risk score for patients with atrial fibrillation: a derivation and validation study. Lancet 6736, 1–10 (2016).
Acknowledgements
J Airaksinen was supported by the Finnish Work Environment Fund (No. 115421). M Kivimäki was supported by the UK Medical Research Council (K013351), NordForsk and the Academy of Finland (311492).
Author information
Authors and Affiliations
Contributions
M.K., M.J., and J.A. were responsible for conception/design of the study. M.K., J.V., and J.P. were responsible for data acquisition. J.A. performed all the analysis. J.A., M.J., M.V., T.O., J.P., J.V., Ma.K., I.K., G.D.B., and M.K. were involved in interpretation of data. J.A., M.K., and M.J. were involved in drafting the manuscript, and M.V., T.O., J.P., J.V., Ma.K., I.K., and G.D.B. critically revised it for important intellectual content. J.A. is the guarantor.
Corresponding author
Ethics declarations
Competing Interests
The authors declare that they have no competing interests.
Additional information
Publisher's note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Airaksinen, J., Jokela, M., Virtanen, M. et al. Development and validation of a risk prediction model for work disability: multicohort study. Sci Rep 7, 13578 (2017). https://doi.org/10.1038/s41598-017-13892-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-017-13892-1
Keywords
This article is cited by
-
Predicting work disability among people with chronic conditions: a prospective cohort study
Scientific Reports (2023)
-
Association between work ability and work stressors: cross-sectional survey of elderly services and health and social care service employees
Archives of Public Health (2022)
-
The influence of antidepressant and psychotherapy treatment adherence on future work leaves for patients with major depressive disorder
BMC Psychiatry (2020)
-
Sleep problem but not chronotype is associated with retirement from shift work: a cross-sectional retrospective study
Sleep and Biological Rhythms (2019)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.