Abstract
Next generation sequencing is transforming clinical medicine and genome research, providing a powerful route to establishing molecular diagnoses for genetic conditions; however, challenges remain given the volume and complexity of genetic variation. A number of methods integrate patient phenotype and genotypic data to prioritise variants as potentially causal. Some methods have a clinical focus while others are more research-oriented. With clinical applications in mind we compare results from alternative methods using 21 exomes for which the disease causal variant has been previously established through traditional clinical evaluation. In this case series we find that the PhenIX program is the most effective, ranking the true causal variant at between 1 and 10 in 85% of these cases. This is a significantly higher proportion than the combined results from five alternative methods tested (p = 0.003). The next best method is Exomiser (hiPHIVE), in which the causal variant is ranked 1–10 in 25% of cases. The widely different targets of these methods (more clinical focus, considering known Mendelian genes, in PhenIX, versus gene discovery in Exomiser) is perhaps not fully appreciated but may impact strongly on their utility for molecular diagnosis using clinical exome data.
Similar content being viewed by others
Introduction
Next generation sequencing (NGS) of patient genomes is revolutionising research and medical genetics by establishing molecular diagnoses and identifying novel disease: gene relationships. Whole-exome sequencing (WES), which covers only the protein coding sequence of the genome, is particularly cost-effective and has identified many novel disease genes underlying mostly Mendelian and other monogenic conditions. However WES typically recovers ~30,000 variants of which ~10,000 are predicted to result in nonsynonymous changes, alter conserved splice sites, or represent small insertions or deletions (indels)1. The variant set includes many that are potentially deleterious and therefore detailed and careful analysis is required to identify the most likely candidate variant(s) which best match the clinical phenotypes.
In order to reduce the complexity of WES data, methods exist to filter variant lists. Filters discard variants which fail to meet a set of criteria based on, for example, the predicted functional impact of the variant through changes to the protein or whether a variant has been observed in a disease-free control data set. Examples of variant-based prediction tools include SIFT (Sorting Intolerant From Tolerant)2 and PolyPhen2 (Polymorphism Phenotyping)3, which are concerned with the impact of an amino acid substitution on the structure and function of a protein; GERP++ (Genomic Evolutionary Rate Profiling4) which is concerned with evolutionary conservation of sites; VAAST 2.0 (Variant Annotation, Analysis Search tool5) which incorporates information about phylogenetic conservation and amino acid substitution and CADD (Combined Annotation-Dependent Depletion6) which integrates information from various functional annotations into a single score. Further reduction in the number of candidate variants might be achieved through ‘intersection filtering’7 which considers whether a significant proportion of individuals with a shared phenotype carry a predicted damaging variant in the same gene and whether such a variant is a strong candidate for disease causality. However, each genome contains ~100 loss-of-function variants and has ~20 genes completely inactivated8. Therefore ‘variant based’ methods based only on predicted pathogenicity, combined with intersection filtering, may be insufficient to separate disease mutations from variants with deleterious biochemical effects which are not related to the disease in question. The difficulty is exemplified by the recent whole genome sequencing of 217 Mendelian disease cases with a broad range of disorders for which disease causal variants were, after comprehensive analysis, confirmed in only 34% of cases9. The development and implementation of more powerful strategies which can accelerate the establishment of molecular diagnoses is pressing. Such strategies underlie successful interpretation of cases from the UK 100,000 genomes project (https://www.genomicsengland.co.uk/the-100000-genomes-project/) which is applying NGS to transform patient diagnosis and treatment and rare disease (along with cancer and infectious disease).
Given the difficulty in establishing molecular diagnoses, even for Mendelian forms of disease, a number of tools have been developed which are designed to determine or support the identification of causal variants (Table 1). These methods integrate diverse database information including, for example, phenotypic ontologies, variant pathogenicity scores, insights from model organisms and protein:protein interaction data, with patient phenotypic and genotypic NGS data. To evaluate the utility of these tools for establishing clinical molecular diagnoses we compare results from a range of methods through rank positions for the causal variants in a panel of clinical exomes which have firmly established molecular diagnoses. The tools produce ranked lists of variants but do not report exclusions (i.e. where the causal variant is not within the NGS data file). We compare methods through the ranked position of the causal variant in each case, in particular where a method achieves a rank of 1 for the causal variant or the variant is ranked in the range 1–10. The cases chosen (Supplementary Table 1) form part of a clinical service evaluation of routine NGS diagnostic testing and might be considered representative of cases encountered in a clinical genetics environment.
Overview of current tools
We consider tools which integrate patient phenotypic information (usually represented in the form of Human Phenotype Ontology, HPO terms; http://human-phenotype-ontology.github.io/about.html) with NGS-derived genotypic data in the form of a VCF file10. Several of the tools are relatively easy to use through online web servers where HPO terms and VCF files containing patient exome data may be uploaded (Table 1). The methods may have a primarily clinical focus, in which known disease genes are targeted, or have a gene discovery emphasis in which novel genes, showing some relationship to known disease associations, are highlighted. The methods include PhenIX 11 which ranks candidate genes in NGS data with a focus on known disease-associated Mendelian genes. Ranking is based on integration of predicted variant pathogenicity with phenotypic similarity of diseases associated with these genes. Exomiser (hiPHIVE) 1 uses the same software framework but also includes multi-species (human, Zebrafish, mouse) ontologies and protein-protein interaction network data. It has a gene discovery focus employing random-walk analyses of multi-species protein interaction networks. Human data come from OMIM and Orphanet12 and the human phenotype comparison considers known disease-gene associations while integration of mouse and zebrafish data targets novel candidate genes. Where genes have no known phenotype associations a random-walk-with-restart algorithm scores proximity to other genes in protein-protein association networks which are implicated in patient phenotypes.
eXtasy 13 employs genomic data fusion to quantify the deleteriousness of nonsynonymous variants which are prioritised dependent on disease phenotypes. eXtasy evaluates patient data against ten measures of variant deleteriousness and a haploinsufficiency prediction score for given gene. The gene prioritisation approach scores genes with mutations according to their similarity with known disease genes. Disease genes previously associated with a HPO term are identified using the Phenomizer algorithm14. Genes containing variants are scored for similarity with this set of genes using Endeavour15, which recognises the high proportion of shared annotations in gene ontology databases. Random Forest learning is used for data integration with the model trained on the Human Gene Mutation Database16 compared to (non-disease) control datasets of common polymorphisms and rare variants.
OMIM Explorer 17 is strongly focussed towards clinical diagnostics by applying transitive prioritization which links phenotypes to variants through medically recognised intermediates. The tool quantifies semantic similarity to compare patient phenotypes with known diseases or syndromes using OMIM as a basis for calculations. Semantic similarity scores and HPO annotations are used to identify similarities of an input query to the set of OMIM-described diseases defined by HPO phenotypes. The interactive user interface guides user input to gradually improve the diagnostic process. Innovative features include an interface for translating clinical notes into HPO terms.
OVA 18 considers genotype and predicted effect on protein sequence to reduce the number of potential candidate variants. OVA firstly excludes likely benign variants (such as synonymous and intronic variants) and then evaluates remaining variants against a multi-ontology annotation. Different ontologies are considered which integrate human and model organism data including: Gene Ontology19, HPO14, Uberon20, Disease Ontology21 and The Pathway Ontology22. Experimental interaction data from mentha23 are also considered. For scoring semantic similarity the query phenotypic descriptors and variant data are evaluated against known phenotype-genotype associations, phenotypes and links across ontologies with the target being the prioritisation of known and novel disease genes. Gene scores are optimised using a Random Forest model to classify each candidate gene and obtain final ranks for candidate genes.
Phen-Gen 24 predicts the damaging impact of coding mutations (nonsynonymous, splice site, and indels) enabling a quantitative comparison between them. Phen-Gen determines potential disease impacts at a locus level (including consideration of non-coding variation) using evolutionary conservation, ENCODE predictions25, and proximity to coding sequence. Phenomizer is used for matching patient HPO terms to known disease-gene associations. Novel candidate genes are assessed as functionally related genes using a random-walk-with-restart algorithm searching gene interaction networks. A Bayesian approach is used to evaluate deleterious variants in the exome to known disease-gene associations.
Phevor 26 integrates phenotype, gene function, and disease information with genomic data targeting both known variation and disease causing alleles not previously implicated in disease. Phevor combines data from biomedical ontologies with variant prioritization scores. The tool propagates information across and between ontologies to re-prioritize potentially damaging variants given gene function and disease, and phenotype knowledge. Outputs from the NGS annotation tools ANNOVAR27 and VAAST5 are used to rank exome variants. Input patient phenotypes are mapped against a series of ontologies, such as HPO and the Mammalian Phenotype Ontology28, to produce a list of genes known to be associated with these terms. In effect entries in different ontologies are brought together through different annotations of the same gene. Each gene receives a score which is combined with the variant annotation data to produce a final rank.
Results
We examined a total of 21 clinical exomes. In the case of Patient 6, with ‘epileptic encephalopathy, early infantile, 4’ secondary to a mutation in the ARX gene, the known causal variant was not captured by the TruSight One panel, and was therefore not present in the genotype data for this individual. We have therefore excluded this case from the comparison of methods.
Table 2 shows the rank position of the known causal mutation in the set of variants scored by each method. The known pathogenic variant was correctly assigned a rank of 1 in 40% of cases by PhenIX (Table 2, Figs 1 and 2), 20% of cases by Exomiser and 10% of cases by eXtasy (using combined order statistics). OVA and eXtasy (using the maximum score) did not identify the correct variant as rank 1 in any case. Considering the identification of the correct causal variant within a rank of 1–10 the proportion of cases resolved by PhenIX rises to 85% but the proportion remains at 20% for Exomiser and increases slightly to 25% using Exomiser with CADD scores. eXtasy, with combined order statistics, identifies the causal variant with rank 1–10 in 20% of cases. PhenIX places the known causal variant at rank = 1 in 8 cases whereas the five other methods combined (Table 2) identify the known variant at rank = 1 in 5 cases, however, this difference is not significant (p = 0.50, by Fisher’s exact test). Considering the placement of the known causal variant as rank = 1–10, PhenIX achieves this in 17 cases whereas taking the highest rank achieved by any method from the set of five other methods ranks the causal variant as 1–10 for 7 cases (p = 0.003).
For eXtasy the superiority of the combined order statistics over the maximum score is clear (Table 2). The performance of eXtasy using combined order statistics might have improved if a complete set of HPO terms could have been used.
The superiority of PhenIX for this small case series of clinical exomes is clear although it is worth noting that improved prioritisation was achieved by alternative methods for two of the cases. For the mental retardation, autosomal recesive 15 case involving the gene MED13L (patient 4) PhenIX only achieves a rank of 106 for the causal variant compared to a much improved ranking of 10 using Exomiser with CADD. Although it is not possible to draw firm conclusions from one case it is conceivable that in, for example, mental retardation phenotypes where there is extreme phenotypic and genotypic heterogeneity, the integrated phenotypic and interactome analysis provided by Exomiser is more powerful. The other case where there is apparent superiority over PhenIX is for Costello syndrome (patient 16) for which the causal variant in HRAS achieves a rank of 7 under PhenIX but ranked 1 by Exomiser and eXtasy using combined order statistics. The reason for this difference is not understood.
Discussion
Matching by semantic similarity of patient phenotypes with resources such as the Online Mendelian Inheritance in Man (OMIM) disease catalogue is widely employed. A straightforward analysis strategy might filter variant lists by limiting the search for causal variants to genes already known to contain variants associated with a set of phenotypes, for example using lists of genes generated from OMIM. This seems most likely to be effective for conditions with more limited phenotypic and genotypic heterogeneity but, in other cases, using tools such as PhenIX which allows for phenotypic ambiguity through distance measures in the HPO network, as opposed to using semantic absolutes using OMIM, might be advantageous.
Tools which integrate knowledge of existing clinical phenotype and genotype relationships might give misleading results where these relationships are poorly understood. James et al.17, argue that the procedure employed in PhenIX (in which phenotypes are collapsed across the diseases to which a gene’s variants have been associated), can result in overestimation and underestimation of semantic similarity matches of candidate genes to patient phenotypes and limited reporting of ruled-out diseases from further consideration. There is therefore a risk of incorrect phenotypic interpretation given the limitations of current knowledge and over-reliance on this form of matching. However, as we have shown here for cases in a clinical setting, tools which have a gene discovery rather than diagnostic emphasis may give misleading results.
Most tools (eXtasy, Phevor, Phen-Gen, OVA and Exomiser hiPHIVE) integrate human and non-human genomic data which underlies their gene discovery focus. Our analyses, which utilise clinical exome data with known molecular causes, suggest that these tools may not reliably identify known disease:gene relationships. The most striking example is in the comparison of PhenIX and Exomiser (hiPHIVE) which share the same software framework but have widely differing performance (ranking the causal variant 1–10, in 17 cases by PhenIX, compared to 5 cases by Exomiser, p = 0.0003). This comparison suggests that the integration of model organism data (as in Exomiser) may be less useful in prioritising established human phenotype: genotype relationships which underlie many clinical genetics applications. However, where there is high phenotypic and genotypic heterogeneity, such as in the case of mental retardation phenotypes, tools which encompass a wider range of predictors may be more useful.
Beyond the questions of diagnostic accuracy, there are also other potential factors which would need to be considered prior to the implementation of these tools in a diagnostic setting. Amenability to high throughput use, and ability to integrate with existing software used would greatly reduce the ‘hands on’ time required for using these tools, as well as reducing the potential for user input error. Furthermore, care must be taken regarding data protection. Tools which provide only a website to which patient data is uploaded (for instance OMIMExplorer) will likely raise more concerns than a tool which can be run locally without data leaving the lab (such as the Exomiser software package).
The use of these software tools will obviously fail to correctly identify the pathogenic variant in cases where the pathogenic variant is not present in the sequencing data (as seen in patient 6 with a pathogenic ARX variant). Some consideration should also be given to the use of a priori candidate gene sets identified using HPO terms (for example by using the Phenomizer platform14). Here, candidate genes worthy of sequencing may be identified and this information can impact the choice of panel for the planned sequencing experiment.
It must be noted that this investigation considers only a small sample size, although they represent well characterised clinical cases. Although a total of 20 exomes contribute to the final analyses, it is noteworthy that the statistical superiority of PhenIX in these data has been demonstrated. It is likely that these data are not representative of the substantial variety of exome samples that will be seen in clinical practice, though they do represent an unbiased selection of exomes which were clinically resolvable through traditional genetic investigations. Whilst resolving clinically tractable exomes is perhaps not the area for which these tools offer the biggest gain, they have the potential to help streamline diagnostic processes if used routinely for diagnostic applications. It is therefore important to understand situations in which some of the tools may be sub-optimal. We have shown that this may be the case with hiPHIVE for clinically ‘simple’ cases, and further work is required to confirm this evidence to inform clinical practice as NGS and HPO analyses become increasingly mainstream.
Materials and Methods
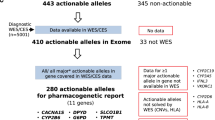
We consider 21 exome samples collected during a regional clinical exome service evaluation project in the UK. These cases have a previously established, clinically confirmed molecular diagnosis determined through traditional testing. Phenotypes from each case were described through comprehensive sets of HPO terms (Supplementary Table 1); HPO terms were selected based upon review of the clinical notes, identifying unambiguous physical features, as well as those reported by multiple clinicians. Samples were sequenced following capture using the TruSight One sequencing panel (Illumina, San Diego, CA, USA). The TruSight One panel captures the exonic regions of 4,813 genes that are known to be implicated in the development of human disease.
For the tools we were able to compare we retained default parameters throughout and used the same HPO terms and VCF files as input in each case, with the following tool-specific differences: eXtasy could not utilise all current HPO terms because its internally held database of HPO terms has not been fully updated since the original publication of the eXtasy program. We consider two alternative statistics for the eXtasy software. Because each variant may be associated with different phenotypes eXtasy can report a maximum score (‘combined max’) across phenotypes13 and, alternatively, it may report Order Statistics (‘combined order statistics’)15 which combines ranking from separate data sources effectively reducing to a combined rank across all separate ranks. PhenIX was run utilising the available web server (http://compbio.charite.de/PhenIX/), whilst hiPhive was run using the downloaded Exomiser package. For hiPHIVE and PhenIX, we specified a 0.1% allele frequency cutoff. Exomiser (hiPHIVE) does not include CADD scores as a default but has the option to include them if downloaded locally. We compare both the default program and the program with the addition of CADD scores. We scored the rank position determined by each method tested for the known causal variant in every case (Table 2, Fig. 1).
This research was performed in accordance with the relevant guidelines for research within the National Health Service.
Data availability
We are unable to make the genomic data on which these analyses are based available.
References
Robinson, P. N., Köhler, S., Oellrich, A. et al. Improved exome prioritization of disease genes through cross-species phenotype comparison. Genome research 24(2), 340–348 (2014).
Ng, P. C. & Henikoff, S. SIFT: Predicting amino acid changes that affect protein function. Nucleic acids research 31(13), 3812–3814 (2003).
Adzhubei, I., Jordan, D. M. & Sunyaev, S. R. Predicting functional effect of human missense mutations using PolyPhen2. Current protocols in human genetics 7–20 (2013).
Davydov, E. V., Goode, D. L., Sirota, M. et al. Identifying a high fraction of the human genome to be under selective constraint using GERP++. PLoS Comput Biol. 6(12), e1001025 (2010).
Hu, H., Huff, C. D., Moore, B. et al. VAAST 2.0: Improved variant classification and disease gene identification using a conservation controlled amino acid substitution matrix. Genetic epidemiology 37(6), 622–634 (2013).
Kircher, M., Witten, D. M., Jain, P. et al. A general framework for estimating the relative pathogenicity of human genetic variants. Nature genetics 46(3), 310 (2014).
Dand, N., Schulz, R., Weale, M. E. et al. Network-Informed Gene Ranking Tackles Genetic Heterogeneity in Exome Sequencing Studies of Monogenic Disease. Human mutation 36(12), 1135–1144 (2015).
MacArthur, D. G., Balasubramanian, S., Frankish, A. et al. A systematic survey of loss-of-function variants in human protein-coding genes. Science 335(6070), 823–828 (2012).
Taylor, J. C., Martin, H. C., Lise, S. et al. Factors influencing success of clinical genome sequencing across a broad spectrum of disorders. Nature genetics 47(7), 717–726 (2015).
Danecek, P., Auton, A., Abecasis, G. et al. The variant call format and VCFtools. Bioinformatics 27(15), 2156–8 (2011).
Zemojtel, T., Köhler, S., Mackenroth, L. et al. Effective diagnosis of genetic disease by computational phenotype analysis of the disease-associated genome. Science translational medicine 6(252), 252ra123 (2014).
Rath, A., Olry, A., Dhombres, F. et al. Representation of rare diseases in health information systems: the Orphanet approach to serve a wide range of end users. Human Mutation 33, 803–808 (2012).
Sifrim, A., Popovic, D., Tranchevent, L. C. et al. eXtasy: variant prioritization by genomic data fusion. Nature methods 10(11), 1083–1084 (2013).
Köhler, S., Schulz, M. H., Krawitz, P. et al. Clinical diagnostics in human genetics with semantic similarity searches in ontologies. The American Journal of Human Genetics 85(4), 457–464 (2009).
Aerts, S., Lambrechts, D., Maity, S. et al. Gene prioritization through genomic data fusion. Nature biotechnology 24(5), 537–544 (2006).
Stenson, P. D., Ball, E. V., Mort, M. et al. The Human Gene Mutation Database (HGMD) and its exploitation in the fields of personalized genomics and molecular evolution. Current protocols in bioinformatics 1–3 (2012).
James, R. A., Campbell, I. M., Chen, E. S. et al. A visual and curatorial approach to clinical variant prioritization and disease gene discovery in genome-wide diagnostics. Genome Medicine 8(1), 1 (2016).
Antanaviciute, A., Watson, C. M., Harrison, S. M. et al. OVA: integrating molecular and physical phenotype data from multiple biomedical domain ontologies with variant filtering for enhanced variant prioritization. Bioinformatics btv473 (2015).
Ashburner, M., Ball, C. A., Blake, J. A. et al. Gene ontology: tool for the unification of biology. The Gene Ontology Consortium. Nature Genetics 25, 25–29 (2000).
Mungall, C. J., Torniai, C., Gkoutos, G. V. et al. Uberon, an integrative multi-species anatomy ontology. Genome Biology 13, R5 (2012).
Kibbe, W. A., Arze, C., Felix, V. et al. Disease Ontology 2015 update: an expanded and updated database of human diseases for linking biomedical knowledge through disease data. Nucleic Acids Research 43, D1071–D1078 (2015).
Petri, V., Jayaraman, P., Tutaj, M. et al. The pathway ontology - updates and applications. J. Biomed. Semantics 5, 7 (2014).
Calderone, A., Castagnoli, L. & Cesareni, G. mentha: a resource for browsing integrated protein-interaction networks. Nature Methods 10, 690–691 (2013).
Javed, A., Agrawal, S. & Ng, P. C. Phen-Gen: combining phenotype and genotype to analyze rare disorders. Nature methods 11(9), 935–937 (2014).
ENCODE Project Consortium. The ENCODE (ENCyclopedia of DNA elements) project. Science. 306(5696), 636–640 (2004).
Singleton, M. V., Guthery, S. L., Voelkerding, K. V. et al. Phevor combines multiple biomedical ontologies for accurate identification of disease-causing alleles in single individuals and small nuclear families. The American Journal of Human Genetics 94(4), 599–610 (2014).
Wang, K., Li, M. & Hakonarson, H. ANNOVAR: functional annotation of genetic variants from high-throughput sequencing data. Nucleic acids research 38(16), e164 (2010).
Smith, C. L. & Eppig, J. T. The mammalian phenotype ontology: enabling robust annotation and comparative analysis. Wiley Interdisciplinary Reviews: Systems Biology and Medicine 1(3), 390–399 (2009).
Smedley, D., Jacobsen, J. O., Jäger, M. et al. Next-generation diagnostics and disease-gene discovery with the Exomiser. Nature protocols 10(12), 2004–2015 (2015).
Haendel, M. A., Vasilevsky, N., Brush, M. et al. Disease insights through cross-species phenotype comparisons. Mammalian Genome 26(9–10), 548–555 (2015).
Smedley, D., Köhler, S., Czeschik, J. C. et al. Walking the interactome for candidate prioritization in exome sequencing studies of Mendelian diseases. Bioinformatics 30(22), 3215–3222 (2014).
Acknowledgements
TA was supported by the Nuffield Foundation. The Wessex Clinical Exome Pilot is supported by the University of Southampton, University Hospital Southampton NHS Foundation Trust, Salisbury NHS Foundation Trust and the Academic Health Sciences Network.
Author information
Authors and Affiliations
Contributions
R.J.P. and A.C. performed and supervised data analysis and wrote the manuscript, T.A. performed data analysis, Z.Z. collected and analysed data, D.H. and S.E. supervised and performed data collection and analysis.
Corresponding author
Ethics declarations
Competing Interests
The authors declare that they have no competing interests.
Additional information
Publisher's note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Pengelly, R.J., Alom, T., Zhang, Z. et al. Evaluating phenotype-driven approaches for genetic diagnoses from exomes in a clinical setting. Sci Rep 7, 13509 (2017). https://doi.org/10.1038/s41598-017-13841-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-017-13841-y
This article is cited by
-
An AI-based approach driven by genotypes and phenotypes to uplift the diagnostic yield of genetic diseases
Human Genetics (2024)
-
High-Resolution and Multidimensional Phenotypes Can Complement Genomics Data to Diagnose Diseases in the Neonatal Population
Phenomics (2023)
-
Early illustrations of the importance of systematic phenotyping
European Journal of Human Genetics (2022)
-
Clinical and genotypic analysis in determining dystonia non-motor phenotypic heterogeneity: a UK Biobank study
Journal of Neurology (2022)
-
Predicting genes from phenotypes using human phenotype ontology (HPO) terms
Human Genetics (2022)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.