Abstract
The present study was to assess the precision (repeatability and reproducibility) of a new optical biometer (OA-2000, Tomey, Japan) based on swept-source optical coherence tomography (SS-OCT) and Placido disk topography in eyes with cataracts. Seventy-eight eyes from seventy-eight patients with cataracts were evaluated. Axial length (AL), anterior chamber depth (ACD), keratometry (K) over a 2.5 mm and 3.0 mm diameter, lens thickness (LT), central corneal thickness (CCT) and white-to-white (WTW) distance were measured by 2 skilled operators. OA-2000 measurements were highly repeatable and reproducible for all parameters (intraclass correlation, 0.925 to 1.000). OA-2000 derived K-values with a diameter of 3.0mm showed narrower 95% limits of agreement (LoA) (SRK/T: −0.18 to 0.16D; Holladay 1: −0.20 to 0.19D; Hoffer Q: −0.22 to 0.20D) than those with a diameter of 2.5 mm for IOL power calculations (SRK/T: −0.20 to 0.20D; Holladay 1: −0.23 to 0.23D; Hoffer Q: −0.25 to 0.25D). The precision (repeatability and reproducibility) of the OA-2000 was excellent for all parameters. The 3.0mm diameter K-readings appear to be the most reliable choice for calculation of IOL power with the OA-2000. In addition, the average values determined from each operator’s 3 consecutive readings were more reproducible.
Similar content being viewed by others
Introduction
Accurate calculation of the intraocular lens (IOL) power is a mandatory step to achieve the desired refractive outcome following cataract surgery. IOL power calculation depends on precise and accurate measurements of the ocular biometric parameters1,2,3. Keratometry (K), i.e. the measurement of corneal curvature and calculation of its power, can be performed by several technologies, whereas axial length (AL) and anterior chamber depth (ACD) are assessed either by ultrasound biometry (preferably with the immersion technique)4,5 and optical biometry. Since the introduction of the IOLMaster (Carl Zeiss Meditec, Germany), optical biometry has gradually replaced traditional ultrasound biometry. IOLMaster applies partial coherence interferometry (PCI) for AL measurements, lateral slit illumination for anterior chamber depth (ACD) measurements and automated keratometry with six peripheral measuring points for corneal curvature estimation6,7,8,9. It is non-contact device and thus does not require topical anesthesia and does not induce any risk of infection. Furthermore, many published studies have indicated that the device shows good repeatability and reproducibility6,10,11,12,13.
Recently, a newly developed optical biometry device (OA-2000, Tomey, Japan), which combines swept source optical coherence tomography (SS-OCT) and Placido disk topography, has been introduced into the market. The new device can measure seven ocular parameters: AL, ACD, K over a 2.5mm and 3.0mm diameter, lens thickness (LT), pupil diameter (PD), central corneal thickness (CCT) and white-to-white (WTW) distance. We recently demonstrated that the OA-2000 SS-OCT biometer and the IOLMaster PCI biometer provided measurements with high agreement for most biometrical parameters14. To our knowledge, however, the precision (repeatability and reproducibility) has not yet been investigated in eyes with cataract, and no studies have assessed whether an average of consecutive readings or a single reading is better. Therefore, the aim of this study was to prospectively evaluate the repeatability and reproducibility of the measurements with this new SS-OCT based biometer in eyes with cataract, test the IOL power calculation obtained with these measurements, and assess whether the average or single measurement is better in clinical practice.
Results
This prospective study compromised randomly 78 right eyes of 78 patients with cataracts (41 men, 37 women).The mean age of the patients was 68.12 ± 8.82 years (range, 45 to 85 years).
Intraoperator repeatability for biometry
The OA-2000 provided highly repeatable measurements for AL, CCT, ACD, LT, WTW and K values, with both operators (Table 1). The ICCs of all ocular components were higher than 0.94, and the CoVs were less than 0.76% except LT (less than 2.07%) and ACD (less than 1.43%). Measurement of the AL provided the highest repeatability as the repeatability limit (r) was lower than 0.05mm and the ICC between 0.999 and 1.0.
Interoperator reproducibility for biometry
Average of 3 consecutive readings
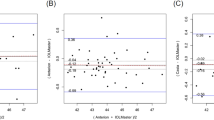
Table 2 shows the interoperator reproducibility of the average measurements for all parameters obtained by averaging each operator’s 3 consecutive readings. There was no statistically significant difference between the two operators’ mean measurements (P > 0.05). All the ICC values were higher than 0.925, demonstrating an excellent reproducibility for all parameters. The Bland-Altman plots showed narrow 95% LoA for the AL, CCT, ACD, K values, and WTW measurements, and a fixed bias was not detected between the two operators. Measurement of the AL provided the highest reproducibility as the ICC between 0.999 and 1.0 and the 95% LoA between −0.02 and 0.03 mm.
Single reading
Table 3 shows the interoperator reproducibility of all parameters obtained from each operator’s first single OA-2000 reading. There was no statistically significant difference between the two operators (P > 0.05). The ICCs for AL, CCT, ACD, K values were more than 0.990, revealing excellent reproducibility. The LT and WTW showed relativity lower but also high reproducibility with ICC were 0.923, 0.897, respectively. The 95% LoA obtained by the first single reading from each operator were statistically wider than those of three consecutive mean readings. The width of the 95% LoA for AL, CCT, LT, Km(2.5), Km(3.0), WTW based on average method were decreased by 44.4%, 35%, 48.3%, 42.2%, 39.2%, 12.5%, respectively (Figs 1–2). These findings indicate that the average measurements achieve a higher reproducibility than does just one single measurement.
Intraoperator repeatability for IOL calculation
Measurements for IOL power calculation performed by both operators are shown in Table 4. Repeatability for IOL power calculation was again excellent for both diameters Ф = 2.5 mm and Ф = 3.0 mm with the ICCs were more than 0.995, the CoVs were less than 0.82%, and repeatability limit (r) values less than 0.45D.
Interoperator reproducibility for IOL calculation
Average of 3 consecutive readings
The average of three successive measurements for IOL power calculation performed by both operators are given in Table 5. There was no statistically significant difference between the two operators’ three consecutive mean measurements for IOL power calculation (P > 0.05). All the ICCs were more than 0.998, demonstrating excellent reproducibility for IOL power calculation. The 95% LoA was wider when using the 2.5 mm diameter for three formulas. And the SRK/T showed the narrowest 95% LOA both using 2.5 mm and 3.0 mm compared to the other two calculation formulas. Overall, agreement between the two operators was higher when the 3.0 mm, rather than the 2.5 mm, diameter was selected on the OA-2000 to measure K.
Single reading
Table 6 shows the interoperator reproducibility of each operators’ first OA-2000 reading for IOL power calculation. All ICCs were over 0.994, revealing excellent reproducibility for three formulas both two diameters. Nevertheless, the 95% LoA were wider than those of three consecutive mean readings (Fig. 3). The width of the 95% LoA that based on the average method using both 2.5 mm and 3.0 mm for SRK/T, Hoffer Q and Holladay I were decreased by 45.2%, 43.9%, 39.3%, 44.3%, 41.8%, 43.2% than those based on the single method, respectively.
Discussion
In the era of refractive cataract surgery, accurate calculation of IOL power requires the most precise and accurate biometric measurements2,3. Anatomical parameters, in particular, axial length and keratometry are fundamental to the accurate determination of the most suitable IOL power at the time of cataract surgery. Inaccurate measurements will result in inaccurate IOL power calculations. The OA-2000 is a new optical device based on SS-OCT and Placido disk topography. There is growing evidence of the potential benefits of this new technology (SS-OCT) particularly in terms of acquisition of axial length measurements in dense cataracts15. Our recent research showed high reliability on healthy eyes for all ocular parameter measurements using the OA-2000. Especially for AL that showed the highest repeatability (Sw, 0.02 mm, repeatability limit (r), 0.07 mm, ICC, 1.0) and reproducibility (ICC, 1.0)14. We also found that the refractive outcomes with IOL power calculation based on the measurements by this device were good16.
This is the first study to investigate the repeatability and reproducibility of its measurements in patients with cataract. Excellent repeatability and reproducibility were found for all parameters, with AL showing the highest repeatability and reproducibility, and WTW a slightly lower precision. With regards AL, the intraoperator repeatability limit (r) was 0.05 mm and the 95% interoperator LoA ranged from −0.02 to 0.03 mm. Given that in a normal eye, a 0.10 mm error in AL is equivalent to an error of about 0.27D in the spectacle plane17, we can state that the errors in the refractive prediction due to AL variability are negligible. The high repeatability and reproducibility of ACD measurements mean that formulas based on this parameter (such as the Haigis, Olsen and Barrett formulas) would not be affected by its variability. Several studies had already evaluated the reproducibility of other optical biometers. Results similar to ours have been reported for other optical biometers, like the IOLMaster18, AL-Scan (Nidek Co, Aichi, Japan)19, the Aladdin (Topcon Corp, Tokyo, Japan)20, and the Lenstar (Haag-Streit, Köniz, Switzerland)21,22. K values are one of the main elements for IOL power calculation. The repeatability of Km was slightly better with 3.0 mm readings, but was still very good with 2.5 mm readings too. The repeatability of the OA-2000 K values was similar to that previously reported for other optical biometers, such as the Aladdin20 and the Lenstar22.
In the present study, the repeatability and reproducibility for WTW and LT measurements were high, but lower than those determined for the other parameters. Similar values have been previously reported for LT with other optical biometers22,23. Olsen24 highlighted the influence of LT in the prediction of the postoperative IOL position. However, the clinical impact of LT measurement repeatability is still unknown.
WTW is important for phakic IOL implantation. A relatively low repeatability and reproducibility of WTW (similar to ours) have already been reported for the AL-Scan, IOLMaster, Aladdin and Lenstar20,25,26. The OA-2000 biometer calculates the WTW by distinguishing the light and shade interface between cornea and sclera. It is likely that, due to the high prevalence of arcus senilis in elderly patients with cataracts, the variations in the method of detection may influence the identification of this edge.
CCT has little influence on IOL power, however, it plays an important role in calculating corrected intraocular pressure, completing any preoperative assessment for keratorefractive surgery and diagnosing corneal diseases, such as Fuch’s corneal dystrophy and keratoconus. OA-2000 measurements of CCT are based on SS-OCT, as is also the case for the IOLMaster 700 (Carl Zeiss Meditec AG). Previous studies with the latter optical biometer found results similar to ours27,28,29.
In the present study, we did not only analyze the reproducibility of the mean measurements obtained by two operators but also analyzed the reproducibility of single measurements. We found that the ICCs for the average parameters were higher and the 95% LoA for the average were narrower than those of a single measurement for both 2.5 mm and 3.0 mm diameters. The ICCs for three IOL power calculation formulas based on the average method were higher and the 95% LoA were narrower than those based on a single method. Our findings were in accordance with our recent studies assessing the corneal power measurement of an RTVue Fourier-domain optical coherence tomography (FD-OCT) system (Optovue Inc., Freemont, CA, USA)30. Wang et al.30 also demonstrated that the width of the 95% LoA was reduced using the mean result rather than the first reading of each operator and recommended the mean for clinical application.
This study has some limitations. First, we only assessed the repeatability and reproducibility of measurements with the OA-2000 in patients with cataracts. The findings cannot be applied to patients with other diseases such as keratoconus or contact lens usage or those who had corneal refractive surgery, so further research is necessary to determine those issues. Moreover, we only investigated the new biometer without comparing its results with those provided by similar instruments based on SS-OCT biometers that have already been validated such as the IOLMaster 700.
In summary, the OA-2000 provides highly repeatable and reproducible estimates of AL, CCT, ACD, K, LT, WTW values in patients with cataracts. For IOL power calculation, we suggest using K values measured at a 3.0 mm diameter. Moreover, because the average values determined from each operator’s 3 consecutive readings were more reproducible, we also recommend that clinicians use the mean values.
Subjects and Methods
Patients
Patients with cataracts attending the Eye Hospital of Wenzhou Medical University, Wenzhou, China were invited to participate in this prospective device evaluation study. All patients underwent a complete ophthalmologic examination. Patients with nuclear and cortical score more than 5.0, posterior subcapsular score more than 3.5 based on Lens Opacities Classification System III, previous ocular surgery, trauma, active ocular disease, fundus disease, pre-existing astigmatism >3.0 diopters (D), contact lens usage (within 4 weeks for rigid contact lenses and within 2 weeks for soft contact lenses), poor fixation or significant cognitive impairment were excluded from the study. The study was in compliance with the Declaration of Helsinki. Ethical approval was granted form the ethics committee of the Eye Hospital of Wenzhou Medical University. A written informed consent was obtained from each patient.
Instrument
The OA-2000 (software version 1.0 R) is a non-invasive, high-resolution, biometry instrument, which combines SS-OCT and Placido disk corneal topography. SS-OCT is a subtype of Fourier domain OCT that can measure AL, ACD, CCT, and LT using a wavelength of 1060 nm. It is equipped with a search function—“B-scanning”, that automatically detects a measurable point when the crystalline lens is unclear. The Placido disk corneal topography is used to measure the radius of corneal curvature based on the Placido disk principle. In addition to the 3.0 mm diameter measured by a general keratometer, a 2.5 mm diameter measurement is simultaneously captured. In this study, the flattest K (Kf) and steepest K (Ks) measurements for each of two areas of differing diameter (Kf (Φ = 2.5), Ks (Φ = 2.5), Kf (Φ = 3.0) and Ks (Φ = 3.0)) were averaged and recorded as mean K (Km) (Φ = 2.5) and Km (Φ = 3.0), respectively. Measurements of the ACD are achieved by means of a charge-coupled device (CCD) camera and infrared light illumination. The WTW distance, i.e. the corneal diameter, was obtained according to the captured image. All measurements with suboptimal quality with poor fixation were deleted and retaken.
Measurements
Each subject had 3 consecutive measurements, performed by 2 skilled and experienced operators according to the manufactures’ guidelines. For each patient, only the right eye was examined. The initial examiner was assigned randomly in each case. All measurements were performed between 10:00 and 17:00, and all measurements were acquired within a time period of 20 minutes. In this study the following measurements were evaluated: ACD, CCT, LT, WTW, AL, steep K, flat K, and mean K. All patients were positioned correctly in the headrest and asked to fixate on the target without blinking during the scan. Each patient was then instructed to blink completely so as to spread a smooth tear film over the cornea in between scans. When necessary the lids were gently held open (with care not to exert pressure on the globe) to ensure that the lids did not block the corneal mapping area. The IOL power was calculated using the following three formulas: SRK/T (A-constant = 118.0), Holladay 1 (surgeon factor = 1.22), Hoffer Q (predicted ACD = 4.97).
Statistical Analysis
All data were recorded in a Microsoft Office Excel 2010 (Microsoft Crop, WA, USA) spreadsheet and the statistical analysis was performed using SPSS software for windows V.21 (SPSS Inc. Chicago, Illinois, USA) and MedCalc Statistical Software V16.8 (MedCalc Software, Inc. Belgium). The results of the parameters were expressed by means and standard deviations (SD). The normality of the distribution of data was assessed using the Kolmogorov-Smirnov test (P > 0.05). Repeatability (Sr) equals the within-subject SD (Sw) for repeated measures with the same observer, which is derived by a one-way analysis of variance (ANOVA). The repeatability limit (r) is reported as 1.96√2 × Sr which gives the likely limits within which 95% of measurements should occur. Sr and r were calculated for the repeated measurements with the three scan modes for each observer31. The CoV is defined as the ratio of Sw to the overall mean. A lower CoV is closely related to higher repeatability. The ICC represents the consistency of measurement. The closer the ICC to 1, the better the consistency of measurement is32.
To evaluate interoperator reproducibility, the paired t test was used to test the difference of parameters obtained by two operators. Furthermore, agreement between different operators was analyzed with Bland-Altman plots, and the 95% limits of agreement (LOA) were calculated as the mean difference ± 1.96 SDs33. A P value less than 0.05 was deemed to be statistically significant.
References
Olsen, T. Sources of error in intraocular lens power calculation. J Cataract Refract Surg 18, 125–129 (1992).
Hoffer, K. J. The Hoffer Q formula: a comparison of theoretic and regression formulas. J Cataract Refract Surg 19, 700–712 (1993).
Lee, A. C., Qazi, M. A. & Pepose, J. S. Biometry and intraocular lens power calculation. Curr Opin Ophthalmol 19, 13–17 (2008).
Butcher, J. M. & O’Brien, C. The reproducibility of biometry and keratometry measurements. Eye 5(Pt 6), 708–711 (1991).
Raj, P. S., Ilango, B. & Watson, A. Measurement of axial length in the calculation of intraocular lens power. Eye 12(Pt 2), 227–229 (1998).
Lam, A. K., Chan, R. & Pang, P. C. The repeatability and accuracy of axial length and anterior chamber depth measurements from the IOLMaster. Ophthalmic Physiol Opt 21, 477–483 (2001).
Olsen, T. Improved accuracy of intraocular lens power calculation with the Zeiss IOLMaster. Acta Ophthalmol Scand 85, 84–87 (2007).
Goebels, S. et al. Comparison of 3 biometry devices in cataract patients. J Cataract Refract Surg 41, 2387–2393 (2015).
Holzer, M. P., Mamusa, M. & Auffarth, G. U. Accuracy of a new partial coherence interferometry analyser for biometric measurements. Brit J Ophthalmol 93, 807–810 (2009).
Kunavisarut, P., Poopattanakul, P., Intarated, C. & Pathanapitoon, K. Accuracy and reliability of IOL master and A-scan immersion biometry in silicone oil-filled eyes. Eye (Lond) 26, 1344–1348 (2012).
Rabsilber, T. M., Jepsen, C., Auffarth, G. U. & Holzer, M. P. Intraocular lens power calculation: clinical comparison of 2 optical biometry devices. J Cataract Refract Surg 36, 230–234 (2010).
Vogel, A., Dick, H. B. & Krummenauer, F. Reproducibility of optical biometry using partial coherence interferometry: intraobserver and interobserver reliability. J Cataract Refract Surg 27, 1961–1968 (2001).
Bueno-Gimeno, I., Espana-Gregori, E., Gene-Sampedro, A., Lanzagorta-Aresti, A. & Pinero-Llorens, D. P. Relationship among corneal biomechanics, refractive error, and axial length. Optometry and vision science: official publication of the American Academy of Optometry 91, 507–513 (2014).
Huang, J. et al. Repeatability and interobserver reproducibility of a new optical biometer based on swept-source optical coherence tomography and comparison with IOLMaster. Br J Ophthalmol 101, 493–498 (2017).
McAlinden, C. et al. Axial Length Measurement Failure Rates With Biometers Using Swept-Source Optical Coherence Tomography Compared to Partial-Coherence Interferometry and Optical Low-Coherence Interferometry. Am J Ophthalmol 173, 64–69 (2017).
Savini, G. et al. Accuracy of a new swept-source optical coherence tomography biometer for IOL power calculation and comparison to IOLMaster. J Refract Surg in press (2017).
Olsen, T. Calculation of intraocular lens power: a review. Acta Ophthalmol Scand 85, 472–485 (2007).
Shammas, H. J. & Chan, S. Precision of biometry, keratometry, and refractive measurements with a partial coherence interferometry-keratometry device. Journal of cataract and refractive surgery 36, 1474–1478 (2010).
Huang, J. et al. Evaluation of a new optical biometry device for measurements of ocular components and its comparison with IOLMaster. Br J Ophthalmol 98, 1277–1281 (2014).
Huang, J. et al. Repeatability and reproducibility of ocular biometry using a new noncontact optical low-coherence interferometer. Journal of cataract and refractive surgery 41, 2233–2241 (2015).
Chen, W. et al. Scheimpflug-Placido topographer and optical low-coherence reflectometry biometer: repeatability and agreement. J Cataract Refract Surg 38, 1626–1632 (2012).
Shammas, H. J. & Hoffer, K. J. Repeatability and reproducibility of biometry and keratometry measurements using a noncontact optical low-coherence reflectometer and keratometer. Am J Ophthalmol 153, 55–61 e52 (2012).
Kunert, K. S. et al. Repeatability and agreement in optical biometry of a new swept-source optical coherence tomography-based biometer versus partial coherence interferometry and optical low-coherence reflectometry. J Cataract Refract Surg 42, 76–83 (2016).
Olsen, T. & Hoffmann, P. C constant: new concept for ray tracing-assisted intraocular lens power calculation. J Cataract Refract Surg 40, 764–773 (2014).
Bjelos Roncevic, M. et al. Comparison of optical low-coherence reflectometry and applanation ultrasound biometry on intraocular lens power calculation. Graefes Arch Clin Exp Ophthalmol 249, 69–75 (2011).
Srivannaboon, S., Chirapapaisan, C., Chonpimai, P. & Koodkaew, S. Comparison of ocular biometry and intraocular lens power using a new biometer and a standard biometer. Journal of cataract and refractive surgery 40, 709–715 (2014).
Srivannaboon, S., Chirapapaisan, C., Chonpimai, P. & Loket, S. Clinical comparison of a new swept-source optical coherence tomography-based optical biometer and a time-domain optical coherence tomography-based optical biometer. Journal of cataract and refractive surgery 41, 2224–2232 (2015).
Garza-Leon, M., Fuentes-de la Fuente, H. A. & Garcia-Trevino, A. V. Repeatability of ocular biometry with IOLMaster 700 in subjects with clear lens. International ophthalmology (2016).
Arriola-Villalobos, P. et al. Effect of pharmacological pupil dilation on measurements and iol power calculation made using the new swept-source optical coherence tomography-based optical biometer. Journal francais d’ophtalmologie 39, 859–865 (2016).
Wang, Q. et al. Corneal Power Measurement Obtained by Fourier-Domain Optical Coherence Tomography: Repeatability, Reproducibility, and Comparison With Scheimpflug and Automated Keratometry Measurements. Cornea 34, 1266–1271 (2015).
McAlinden, C., Khadka, J. & Pesudovs, K. Precision (repeatability and reproducibility) studies and sample-size calculation. J Cataract Refract Surg 41, 2598–2604 (2015).
Muller, R. & Buttner, P. A critical discussion of intraclass correlation coefficients. Stat Med 13, 2465–2476 (1994).
McAlinden, C., Khadka, J. & Pesudovs, K. Statistical methods for conducting agreement (comparison of clinical tests) and precision (repeatability or reproducibility) studies in optometry and ophthalmology. Ophthalmic Physiol Opt 31, 330–338 (2011).
Acknowledgements
Supported in part by the National Natural Science Foundation of China (81300807); Foundation of Wenzhou City Science & Technology Bureau (J20140014, Y20150076); Medical and Health Science and Technology Program of Zhejiang Province (2016RCB013); Zhejiang Provincial & Ministry of Health Research Fund For Medical Sciences (WKJ-ZJ-1530); The National Key Research and Development Program of China (2016YFC0100200, 2016YFC0100201). The contribution of G.B. Bietti Foundation IRCCS was supported by the Italian Ministry of Health and Fondazione Roma.
Author information
Authors and Affiliations
Contributions
Concept and design W.W., Y.M., G.S., J.H., Q.W.; data collection Y.M., Q.H.; statistical expertise C.M., G.S.; literature research G.S., H.C., J.H., Q.W.; administrative, technical or logistic support J.H., Q.W.; analysis and interpretation W.W., Y.M., G.S., H.C., J.H., Q.W.; writing the article G.S., C.M., J.H., Q.W.; critical revision of the article W.W., Y.M., G.S., J.H., Q.W.; final approval of the article W.W., Y.M., G.S., C.M., H.C., J.H., Q.W.; All authors reviewed the manuscript.
Corresponding authors
Ethics declarations
Competing Interests
The authors declare that they have no competing interests.
Additional information
Publisher's note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Wang, W., Miao, Y., Savini, G. et al. Precision of a new ocular biometer in eyes with cataract using swept source optical coherence tomography combined with Placido-disk corneal topography. Sci Rep 7, 13736 (2017). https://doi.org/10.1038/s41598-017-13800-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-017-13800-7
This article is cited by
-
Evaluation of the repeatability of optical coherence tomography in patients with age-related cataract associated with dry eye
International Ophthalmology (2022)
-
Effect of orthokeratology on precision and agreement assessment of a new swept-source optical coherence tomography biometer
Eye and Vision (2020)
-
Estimation of intraocular lens position from full crystalline lens geometry: towards a new generation of intraocular lens power calculation formulas
Scientific Reports (2018)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.