Abstract
Inconsistent data from the randomized trials ignites controversy on intensive blood pressure (BP) reduction for acute intracerebral hemorrhage (ICH). This study aims to examine the association between BP lowering and clinical outcomes among patients with acute ICH. We conducted this meta-analysis based on the published randomized controlled trials (RCTs). Data were included from 6 RCTs involving 4412 patients. No significant improvements were observed in hematoma growth at 24 hours, neurologic improvement at 24 hours, hypotension at 72 hours, death or dependency at 90 days, mortality at 90 days, and serious adverse events at 90 days between intensive and conservative BP lowering groups. High heterogeneity was observed between estimates in hematoma growth (I 2 = 49). Univariate meta-regression and subgroup analysis showed that intensive BP lowering showed a significant decrease in hematoma growth in age ≤62 years, time from symptoms onset to treatment ≤6 hours, baseline hematoma volume ≤15 mL, and combined intraventricular hemorrhage ≤25% subgroups. In conclusion, intensive BP management in patients with ICH is safe. Intensive BP lowering could reduce hematoma growth in those patients (≤62 years old) with ICH volume less than 15 mL receiving BP management within 6 hours after randomization.
Similar content being viewed by others
Introduction
Spontaneous intracerebral hemorrhage (ICH) affects 2.5 per 10,000 people worldwide annually1, and is associated with a high mortality that only 38 percent of ICH patients could survive over one year2. Early blood pressure (BP) elevation occurs in more than 90% of affected patients3. Extremely elevated BP is reported to predict hematoma expansion and poor neurological functional outcomes4. Observational data showed a beneficial effect of early intensive BP lowering in patients with ICH5,6. However, it has been reported that excessively low admission systolic BP (SBP) might cause cerebral hypoperfusion and ultimately lead to poor outcomes7. Whether rapid BP lowering in patients with acute ICH would reduce hematoma expansion and improve final outcomes remains on debate.
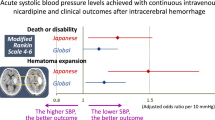
Current AHA/ASA (American Heart Association/American Stroke Association) guidelines recommended that acute lowering of SBP to 140 mm Hg is safe for those ICH patients with SBP between 150 and 220 mm Hg (Class I; Level of Evidence A)8. And it can be effective for improving functional outcome (Class IIa; Level of Evidence B)8. For those ICH patients with SBP >220 mm Hg, aggressive BP reduction should be managed using a continuous intravenous infusion with frequent BP monitoring (Class IIb; Level of Evidence C). These recommendations were based primarily on the data from the phase Intensive Blood Pressure Reduction in Acute Cerebral Hemorrhage II (INTERACT-2) trial enrolling 2839 ICH patients presenting with SBP between 150 and 220 mm Hg within 6 hours9. This trial observed that intensive BP lowering had no effect on reducing the primary outcome of death or major disability, but it could enhance physical functioning compared with conservative BP lowering treatment9. However, this trial was argued for its various use of available antihypertensive drug with different mechanisms, in which the effects might have varied across different agents10. For example, calcium channel blockers could relieve vasospasm to improve cerebral perfusion. In the INTERACT-2 trial, approximately 16.2% of ICH patients received a calcium channel blocker in the intensive BP lowering group compared with 8.5% of ICH patients in the conservative treatment group10. The Antihypertensive Treatment of Acute Cerebral Hemorrhage II (ATACH-2) trial was designed to provide additional information on the efficacy of intravenous nicardipine for intensive BP lowering in patients within 4.5 hours after symptom onset11. However, this trial was discontinued for futility before achieving the target enrollment of 1280 ICH patients11. Moreover, a high occurrence of serious adverse events at 90 days was observed in the intensive BP lowering group in this ATACH-2 trial11.
In consideration of these inconsistent data from the former trials, we aimed to conduct a meta-analysis to examine the association between BP lowering and clinical outcomes among patients with acute ICH.
Methods
This meta-analysis followed the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) format guidelines12.
Search Strategy and Information Sources
All RCTs reporting the efficacy and safety of intensive BP lowering in patients with acute ICH were enrolled from three major databases, MEDLINE, EMBASE, and the Cochrane Library, by two independent investigators (LS and SX). The following search strategy was used in MEDLINE: ((intracranial hemorrhage [Title/Abstract]) OR (intracerebral hemorrhage [Title/Abstract])) AND (blood pressure [Title/Abstract]). Similar search strategy was performed for EMBASE and the Cochrane Library databases from January 2000 to November 2016 without language or other restrictions. In addition, Reference lists of all RCTs, reviews, comments, and meta-analysis were examined to ensure that no relevant studies had been missed by the database search.
Study Selection and Data Collection
Only studies with acute ICH patients who randomly assigned to receive intensive or conservative BP reduction treatment were included in this meta-analysis. Two independent investigators (LS and SX) scanned all studies to select applicable studies. Case reports or series, retrospective or prospective observational studies, and RCTs without control groups were excluded from the final analysis. Data on eligibility criteria, study design, baseline characteristics of the participants, and outcome assessments from the included trials were extracted independently by two investigators (LS and SX).
Outcomes Definition and Quality Assessment
Short-term outcomes were assessed with hematoma growth and neurologic improvement at 24 hours, and hypotension at 72 hours. Hematoma growth was defined as the proportion of acute ICH patients with ≥33% hematoma expansion on the computed tomography (CT) scan at 24 hours compared with the admission scan. Neurologic improvement was defined as an increase of ≥2 points in the Glasgow Coma Score (GCS) or a decrease of ≥4 points in the National Institutes of Health Stroke Scale (NIHSS), which was sustained for at least 8 hours within 24 hours after randomization. Hypotension was defined as the proportion of participants who required therapy with intravenous vasopressor drugs within 72 hours after randomization.
Long-term outcomes were included death or dependency, mortality, and serious adverse events at 90 days. Modified Rankin scale (mRS) runs from 0 to 6 scores in consistent with perfect health without symptoms to death13. Dependency was defined as a score of 3 to 5 on the mRS scale at 90 days after randomization. Serious adverse events were included renal failure, recurrent stroke, acute coronary event, severe hypotension, and other life-threatening events.
Biases of the included trials were assessed by 2 independent investigators (LS and SX) using a 7-point quality control recommended by Cochrane Handbook14. The items contained selection bias, performance bias, detection bias, attrition bias, reporting bias, and other potential biases. Each items was categorized as high, low, or unclear risks.
Data Synthesis and Analysis
All data were calculated by STATA (Version 12.0). Odds ratios (ORs) and 95% credibility interval (CI) were calculated to express the safety and effect of intensive BP reduction in patients with acute ICH compared with conservative BP lowering treatment. A random-effects model and z test were used to calculate the pooled ORs. A P value of less than 0.05 was considered statistically significant. Heterogeneity was assessed with the Cochran Q and I 2 statistics. High heterogeneity was defined as I 2 values of ≥50%. Univariate meta-regression (Method of Moments) and subgroup analysis were performed to evaluate sources of heterogeneity. Publication bias was assessed using Egger’s funnel plot with pseudo 95% confidence limits.
Results
Study Selection and Characteristics
MEDLINE, EMBASE and Cochrane Library databases were searched for all records reporting the efficacy and safety of intensive BP lowering in patients with acute ICH, from which we obtained 35 records without duplicates. Protocols, post-hoc analyses studies, meta-analysis, comments, and reviews were excluded after assessing full-text articles. Ultimately, six studies (ATACH-2 201611, GONG 201515, INTERACT-2 20139, ADAPT 201316, INTERACT 200817, and KOCH 200818) were included in quantitative synthesis (Fig. 1). The characteristics of the included trials are summarized in Table 1.
Overall and subgroup analysis
For long-term outcomes, intensive BP reduction showed no significant differences in death or dependency at 90 days (OR 0.91, 95% CI 0.80 to 1.02, P = 0.11; Fig. 2A), mortality at 90 days (OR 0.98, 95% CI 0.81 to 1.19, P = 0.86; Fig. 2B), and serious adverse events at 90 days (OR 1.10, 95% CI 0.87 to 1.38, P = 0.44; Fig. 2C) compared with conservative BP lowering treatment in patients with acute ICH. No evidence of heterogeneities were observed between estimates in death or dependency at 90 days (I 2 = 0%; P = 0.67) and mortality at 90 days (I 2 = 0%; P = 0.89). But a moderate heterogeneity was observed in serious adverse events at 90 days (I 2 = 47%; P = 0.15).
For short-term outcomes, no significant differences were observed between intensive and conservative BP lowering groups in hematoma growth at 24 hours (OR 0.78, 95% CI 0.56 to 1.09, P = 0.14; Fig. 3A), neurologic deterioration at 24 hours (OR 1.04, 95% CI 0.87 to 1.24, P = 0.66; Fig. 3B), and hypotension at 72 hours (OR 1.20, 95% CI 0.60 to 2.42, P = 0.61; Fig. 3C). No evidence of heterogeneities were observed between estimates in neurologic deterioration at 24 hours (I 2 = 0%; P = 0.45) and hypotension at 72 hours (I 2 = 0%; P = 0.65). But a moderate heterogeneity was observed in hematoma growth at 24 hours (I 2 = 49%; P = 0.08).
Univariate meta-regression showed no independent predictor (P > 0.05) of hematoma growth (Table 2). In subsequent subgroup analysis, intensive BP reduction was associated with a great reduction of hematoma growth in age ≤62 years (OR 0.66, 95% CI 0.51 to 0.86, P = 0.002), time from symptoms onset to treatment ≤6 hours (OR 0.72, 95% CI 0.51 to 1.01, P = 0.05), baseline hematoma volume ≤ 15 mL (OR 0.66, 95% CI 0.51 to 0.86, P = 0.002), and combined intraventricular hemorrhage (IVH) ≤ 25% (OR 0.68, 95% CI 0.52 to 0.90, P = 0.007) subgroups (Fig. 4).
Risk of bias for independent studies
Risk of bias in the included studies is summarized in Fig. 5. All the included trials were open-label RCTs. Except for the GONG 2015 trial15, all trials stated that they were blind to assess outcomes. The KOCH 200818 and GONG 201515 trials were lack of data on adverse events at 90 days after randomization. Publication bias was detected using Egger’s funnel plot with pseudo 95% confidence limits, which showed low risks (data not shown).
Discussion
The data from the present meta-analysis showing similar incidence of 72-hour hypotension and 3-month serious adverse events between intensive and conservative BP reduction groups, indicated that intensive BP lowering treatment was safe (target SBP <140 mm Hg or Mean Arterial Blood Pressure [MAP] <110 mm Hg) in patients with acute ICH. Intensive BP lowering therapy did not appear to have curative effects on either 24-hour neurologic improvement or 3-month functional outcome (death or dependency). But it might have a considerable attenuation of hematoma growth in those patients (≤62 years old) with ICH volume less than 15 mL receiving BP management within 6 hours.
The first issue is the safety of intensive BP lowering in patients with acute ICH. The evidence from the present meta-analysis is reassuring. However, the heterogeneity of 3-month serious adverse events was 47% with P value of 0.15. Univariate meta regression or subgroup analysis was not applicable due to the limited included trials. The ATACH-2 trial observed a higher occurrence of 7-day renal adverse events and 3-month serious adverse events in those patients assigned to the intensive lowering group than those assigned to the conservative BP lowering group11. Renal adverse events might be associated with hypoperfusion, although the occurrence of 72-hour hypotension showed no significant difference between intensive and conservative BP lowering groups11. In view of these former data, intensive BP lowering treatment is acceptable for those patients with acute ICH.
The second question is the efficacy of lowering BP in improving the functional outcomes. The raise in BP levels is very common after acute ICH onset. Several potential mechanisms have been involved in this pathological process, including increase intracranial pressure, premorbid hypertension, neuro-endocrine, and activation of neuro-vegetative signaling pathways19. High BP levels in acute ICH patients have been associated with intracranial pressure elevation, cerebral edema formation, and hematoma expansion20,21. Hematoma expansion in the early phase of ICH strongly predicted poor long-term outcomes22. Intensive BP lowering was regarded as an effective management for controlling hematoma expansion5,6. However, this used to be a concern whether rapid BP lowering in patients with acute ICH would cause global or regional cerebral hypoperfusion, especially in the perihematoma. The ADAPT trial found that intensive BP lowering has no significant impact on perihematoma cerebral blood flow16, which was also consistent with previous observational studies23. The results of the present meta-analysis indicated that intensive BP reduction has no significant effect on either 24-hour hematoma growth or 3-month functional outcome. Subgroup analysis indicated that age, therapeutic time window, baseline hematoma volume, and combined with IVH were associated with hematoma expansion at 24 hours after randomization. Among these factors, age was reported as an independent predictor of neurologic recovery24. In the univariate meta-regression analysis, only age showed a potential association with hematoma expansion (P = 0.05). Larger volume of baseline hematoma combined with IVH showed worse outcomes. Analysis of previous available data indicated that each 1 mL growth in hematoma might increase a 7% risk of death or disability25. Spontaneous ICH combined IVH showed 51% risk of death compared to 20% without IVH26. Our findings supported the hypothesis that there is a time-dependent loss of benefit in the intensive BP lowering treatment. ICH might have a wider therapeutic window than acute ischemic stroke, due to its lack of ischemic penumbra27. The ADAPT trial16 indicated a similar effect of intensive BP lowering on hematoma expansion between ≤3 hours and ≤ 4.5 hours. Our data showed that intensive BP lowering could reduce hematoma growth within 6 hours after randomization. In addition, previous meta-analysis including four trials9,16,17,18 indicated that baseline NIHSS score was an independent predictor of 3-month unfavorable outcome (death or dependency)28. However, in the present univariate meta-regression analysis, baseline NIHSS score was not associated with hematoma expansion.
Several limitations of this meta-analysis need to be acknowledged. The first issue is high selection and performance biases that all the included trials were open-label RCTs. Although five of all the included trials were outcome-blinded, performance biases still cannot be ruled out. The limited trials including in this meta-analysis made it impossible to perform multivariate meta regression analysis to detect the interaction among these influential factors. Variable antihypertensive medications with different mechanisms were used in the included trials. In addition, the large size of the INTERACT-2 trial results in disproportional weights in effect sizes.
In conclusion, the present meta-analysis indicated that intensive BP management in patients with ICH is safe, but has no contribution to 90-day neurological functional recovery. Intensive BP lowering could reduce hematoma growth in those patients (≤62 years old) with ICH volume less than 15 mL receiving BP management within 6 hours after randomization.
References
Liu, M. et al. Stroke in China: epidemiology, prevention, and management strategies. Lancet Neurol 6, 456–464, https://doi.org/10.1016/S1474-4422(07)70004-2 (2007).
Qureshi, A. I. et al. Spontaneous intracerebral hemorrhage. N Engl J Med 344, 1450–1460, https://doi.org/10.1056/NEJM200105103441907 (2001).
Asdaghi, N., Manawadu, D. & Butcher, K. Therapeutic management of acute intracerebral haemorrhage. Expert Opin Pharmacother 8, 3097–3116, https://doi.org/10.1517/14656566.8.18.3097 (2007).
Qureshi, A. I. The importance of acute hypertensive response in ICH. Stroke 44, S67–69, https://doi.org/10.1161/STROKEAHA.111.000758 (2013).
Okumura, K. et al. Effects of blood pressure levels on case fatality after acute stroke. J Hypertens 23, 1217–1223, https://doi.org/10.1097/01.hjh.0000170385.76826.4a (2005).
Terayama, Y., Tanahashi, N., Fukuuchi, Y. & Gotoh, F. Prognostic value of admission blood pressure in patients with intracerebral hemorrhage. Keio Cooperative Stroke Study. Stroke 28, 1185-1188, WOS:A1997XC72400016 (1997).
Vemmos, K. N. et al. U-shaped relationship between mortality and admission blood pressure in patients with acute stroke. J Intern Med 255, 257–265, https://doi.org/10.1046/j.1365-2796.2003.01291.x (2004).
Hemphill, J. C. III et al. Guidelines for the Management of Spontaneous Intracerebral Hemorrhage: A Guideline for Healthcare Professionals From the American Heart Association/American Stroke Association. Stroke 46, 2032–2060, https://doi.org/10.1161/STR.0000000000000069 (2015).
Anderson, C. S. et al. Rapid blood-pressure lowering in patients with acute intracerebral hemorrhage. N Engl J Med 368, 2355–2365, https://doi.org/10.1056/NEJMoa1214609 (2013).
Keller, D. L. Blood-pressure lowering in acute intracerebral hemorrhage. N Engl J Med 369, 1273, https://doi.org/10.1056/NEJMc1309586#SA1 (2013).
Qureshi, A. I. et al. Intensive Blood-Pressure Lowering in Patients with Acute Cerebral Hemorrhage. N Engl J Med 375, 1033–1043, https://doi.org/10.1056/NEJMoa1603460 (2016).
Liberati, A. et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. J Clin Epidemiol 62, e1–34, https://doi.org/10.1016/j.jclinepi.2009.06.006 (2009).
Bruno, A. et al. Improving modified Rankin Scale assessment with a simplified questionnaire. Stroke 41, 1048–1050, https://doi.org/10.1161/STROKEAHA.109.571562 (2010).
Higgins, J. P. et al. The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ 343, d5928, https://doi.org/10.1136/bmj.d5928 (2011).
Gong, F.T., et al. Blood pressure control in ultra-early basal ganglia intracerebral hemorrhage. Eur Rev Med Pharmacol Sci 19, 412–415, WOS:000351491800015 (2015).
Butcher, K. S. et al. The Intracerebral Hemorrhage Acutely Decreasing Arterial Pressure Trial. Stroke 44, 620–626, https://doi.org/10.1161/STROKEAHA.111.000188 (2013).
Anderson, C. S. et al. Intensive blood pressure reduction in acute cerebral haemorrhage trial (INTERACT): a randomised pilot trial. Lancet Neurol 7, 391–399, https://doi.org/10.1016/S1474-4422(08)70069-3 (2008).
Koch, S., Romano, J. G., Forteza, A. M., Otero, C. M. & Rabinstein, A. A. Rapid blood pressure reduction in acute intracerebral hemorrhage: feasibility and safety. Neurocrit Care 8, 316–321, https://doi.org/10.1007/s12028-008-9085-8 (2008).
Lattanzi, S. & Silvestrini, M. Blood pressure in acute intra-cerebral hemorrhage. Ann Transl Med 4, 320, https://doi.org/10.21037/atm.2016.08.04 (2016).
Vemmos, K. N. et al. Association between 24-h blood pressure monitoring variables and brain oedema in patients with hyperacute stroke. J Hypertens 21, 2167–2173, https://doi.org/10.1097/01.hjh.0000084798.73547.0c (2003).
Vemmos, K. N. et al. Factors influencing acute blood pressure values in stroke subtypes. J Hum Hypertens 18, 253–259, https://doi.org/10.1038/sj.jhh.1001662 (2004).
Chang, G.Y. Hematoma growth is a determinant of mortality and poor outcome after intracerebral hemorrhage. Neurology 68, 471–472; author reply472, https://doi.org/10.1212/01.wnl.0000256290.15120.37 (2007).
Powers, W.J., et al. Autoregulation of cerebral blood flow surrounding acute (6 to 22 hours) intracerebral hemorrhage. Neurology 57, 18–24, WOS:000169702500005 (2001).
Broderick, J.P., Brott, T.G., Duldner, J.E., Tomsick, T. & Huster, G. Volume of intracerebral hemorrhage. A powerful and easy-to-use predictor of 30-day mortality. Stroke 24, 987–993, WOS:A1993LK32800009 (1993).
Davis, S. M. et al. Hematoma growth is a determinant of mortality and poor outcome after intracerebral hemorrhage. Neurology 66, 1175–1181, https://doi.org/10.1212/01.wnl.0000208408.98482.99 (2006).
Gaberel, T., Magheru, C.& Emery, E. Management of non-traumatic intraventricular hemorrhage. Neurosurg Rev 35, 485–494; discussion 494–485, https://doi.org/10.1007/s10143-012-0399-9 (2012).
Zazulia, A. R. et al. Hypoperfusion without ischemia surrounding acute intracerebral hemorrhage. J Cereb Blood Flow Metab 21, 804–810, https://doi.org/10.1097/00004647-200107000-00005 (2001).
Tsivgoulis, G. et al. Intensive blood pressure reduction in acute intracerebral hemorrhage: a meta-analysis. Neurology 83, 1523–1529, https://doi.org/10.1212/WNL.0000000000000917 (2014).
Acknowledgements
This study was supported by a grant from the National Natural Science Foundation of China (81671131) awarded to Jing Xu. The authors report no financial or other relationship relevant to the subject of this article.
Author information
Authors and Affiliations
Contributions
J.M. Zhang is the principal investigator. L.G. Shi and J. Xu designed the study and developed the analysis plan. S.B. Xu and L.G. Shi analyzed the data and performed meta-analysis. L.G. Shi contributed in writing of the article. J.W. Zheng revised the manuscript and polish the language.
Corresponding authors
Ethics declarations
Competing Interests
The authors declare that they have no competing interests.
Additional information
Publisher's note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Shi, L., Xu, S., Zheng, J. et al. Blood Pressure Management for Acute Intracerebral Hemorrhage: A Meta-Analysis. Sci Rep 7, 14345 (2017). https://doi.org/10.1038/s41598-017-13111-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-017-13111-x
This article is cited by
-
Diagnostic test accuracy of machine learning algorithms for the detection intracranial hemorrhage: a systematic review and meta-analysis study
BioMedical Engineering OnLine (2023)
-
Nonpharmacological Treatments for Hospitalized Patients with Stroke: A Nuanced Approach to Prescribing Early Activity
Neurotherapeutics (2023)
-
Proper timing of control of hypertension and outcome in acute spontaneous intracerebral hemorrhage
The Egyptian Journal of Neurology, Psychiatry and Neurosurgery (2020)
-
The Unsolved Conundrum of Optimal Blood Pressure Target During Acute Haemorrhagic Stroke: A Comprehensive Analysis
High Blood Pressure & Cardiovascular Prevention (2019)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.