Abstract
It has been suggested recently, based on pharmacokinetic-pharmacodynamic modelling exercises, that twice daily dosing of artemisinins increases malaria parasite killing and so could “dramatically enhance and restore drug effectiveness” in artemisinin resistant P. falciparum malaria infections. It was recommended that split dosing should be incorporated into all artemisinin combination regimen designs. To explain why parasite clearance rates were not faster with split dose regimens it was concluded that splenic malaria parasite clearance capacity was readily exceeded, resulting in the accumulation of dead parasites in the circulation, that parasite clearance was therefore an unreliable measure of drug efficacy, and instead that human immunity is the primary determinant of clearance rates. To test these various hypotheses we performed a logistic meta-regression analysis of cure rates from all falciparum malaria treatment trials (n = 40) with monotherapy arms containing artemisinin or a derivative (76 arms). There was no evidence that split dosing enhanced cure rates.
Similar content being viewed by others
Introduction
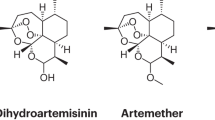
When artemisinin and its derivatives were first evaluated in the treatment of malaria a variety of doses and dosing schedules were assessed. Following single or multiple doses, rates of parasite clearance in falciparum and vivax malaria were faster than observed previously with other classes of antimalarial drug, but satisfactory cure rates with artemisinins alone in falciparum malaria required dosing for more than five days1,2,3,4,5,6,7,8,9,10. The artemisinins are eliminated rapidly (t1/2~1 hour) but giving them twice or even three times in one day did not appear to provide additional benefit over once daily administration, so this became the norm4,5,6,7,8,9,10,11,12,13,14. There were a few exceptions. In uncomplicated malaria artemether-lumefantrine required twice daily administration because of the readily saturated oral absorption of lumefantrine. In severe malaria there was concern that in a highly synchronous infection in which mature schizonts predominated, sub-maximal effects might result from the first parenteral administration so a second dose was given at 12 hours as an “insurance policy”.
Recently, based on pharmacokinetic-pharmacodynamic (PK-PD) modelling studies, it has been suggested that twice daily dosing of artemisinins could increase parasite killing14,15,16,17 and one study went as far as to claim that it could “dramatically enhance and restore drug effectiveness” in artemisinin resistant infections18. The authors further recommended “that twice-daily dosing should be incorporated into all artemisinin combination treatment (ACT) regimen design considerations as a simple and effective way of ensuring the continued long-term effectiveness of ACTs”. The Liverpool group’s strong recommendation for a major change in dosing, which would have a profound effect on current and future practices if followed, was based on PK-PD modelling and was not supported by clinical trial data19. The modelling predicted that splitting current once daily ACT doses into twice per day administration would increase parasite killing enormously (by a factor of 108)16,17,18. So have treatment recommendations been wrong all these years - or is there something wrong with the modelling?
PK-PD modelling
Standard PK-PD models of antimalarial drug concentration-effect relationships generally parameterise the ‘PD’ component (parasite killing) as a sigmoid –Emax relationship driven by plasma concentrations in which parasite numbers decline as a first-order process for a given drug concentration. From observed 48-hour cycle parasite reduction ratios (PRR) and measured plasma concentration profiles in artemisinin treated patients, these models imply that parasite killing rates are very high for a few hours following drug administration, and then decline rapidly as concentrations of artesunate (or artemether) and their main metabolite dihydroartemisinin all fall. It follows logically from this model construct that the effect of each dose is equivalent (in terms of PRR) when suitably spaced out in time, i.e. if the first dose reduced the number of parasites by a factor of 104 then a dose 6–8 hours later would also reduce numbers by 104 fold resulting in a 108 total reduction. However, similar rates of parasitaemia decline (over 48 hours) are observed whether artemisinins are given once, twice or even three times in a day19. Furthermore parasite clearance is actually slower with protracted exposures to the antimalarial peroxides following slowly absorbed intramuscular artemether and slowly eliminated artefenomel than it is with parenteral artesunate which is eliminated very rapidly19,20,21. This may be considered an example of ‘all models are wrong, but some are useful’. The standard PK-PD models are useful for predicting PRR for once daily administration of artemisinin but they fail to predict the observed PRR when more than one dose is given per day. Recent modelling claims to have ‘solved’ this model misfit by hypothesising that the splenic clearance capacity for infected erythrocytes is exceeded by parasite killing by artemisinin antimalarials16,17. It was conjectured that this " saturation" of clearance capacity resulted in the accumulation of dead parasites in the circulation thereby dissociating parasite killing from parasite clearance. Based on this conjecture, it was argued that parasite clearance was an unreliable measure of drug efficacy (as the proportions of live and dead parasites could not be distinguished). Furthermore it was concluded unreservedly that “human immunity is the primary determinant of clearance rates, unless or until artemisinin killing has fallen to near-ineffective levels”22 and more recently that “ the impact of human immunity in clearing erythrocytes containing dead or dying parasites makes parasite clearance rates highly insensitive and non-specific diagnostics of resistance”23. If indeed these conjectures are all true they would deal a serious blow to current epidemiological assessments of artemisinin resistance, which rely heavily on this metric for phenotyping and for validating the parasite genotyping used in molecular surveillance19,24,25,26,27,28. This study examines whether evidence from previous clinical studies of the efficacy of artemisinin and its derivatives supports this hypothesized model structure and the derived therapeutic recommendations.
Clinical observations
The radical suggestions of the Liverpool group are not supported by clinical observations. If immunity is the primary determinant of parasite clearance rates it cannot explain why parasite clearance rates are twice as slow in patients of similar age and geographic origin, who have K13 mutant artemisinin-resistant compared with K13 wild type artemisinin-sensitive parasites19,24,25,26,27,28. In studies where the effects of immunity, or age as a surrogate of cumulative exposure, on parasite clearance rates have been quantitated, the effects are much smaller than the effects of artemisinin resistance19,24,29,30. In assessing treatment responses in artemisinin resistant falciparum malaria the hypothesis that human immunity is the primary determinant of parasite clearance rate17 does not fit the facts.
Cure rates following single versus split dosing
If parasite killing substantially exceeds splenic clearance capacity, and giving artemisinins twice daily is so much better than once daily as claimed18, then irrespective of effects on parasite clearance there should be substantial differences in cure rates with twice daily versus once daily administration.
To test this hypothesis we performed a logistic meta-regression analysis of all trials with monotherapy arms containing artemisinin or a derivative. The dependent variable was cure rate, and the independent variables were duration of treatment (in days) and number of artemisinin doses. If the Liverpool group’s hypothesis was correct then the number of doses given should have been a significant covariate. A further meta-regression model was run on all studies of oral artesunate with the mg/kg dose as an independent variable. The logistic meta-regressions were run with a random effect for each study (random intercept term) and fixed effects for the number of doses and duration of treatment (and dose). We fitted the model in R (version 3.1.1) using the function glmer from the lme4 package. The database of extracted study meta-data can be found in the supplementary materials.
Search strategy
We searched the WorldWide Antimalarial Resistance Network (WWARN) Clinical Trials Publication library for eligible studies. This online resource contains all antimalarial clinical efficacy trials conducted and published since 196031. Studies were eligible if once daily or more frequent administration of artemisinin or a derivative was used as monotherapy to treat uncomplicated falciparum malaria and if cure rates at 28 days were reported for each treatment group (PCR adjusted or unadjusted). For two studies the numbers of failures by day 28 were not reported and were requested from the corresponding author.
In early studies where patients were kept in hospital for 28 days to assess cure rate (i.e. reinfection was not possible) the result was combined with later community based studies with PCR adjusted estimates.
Results
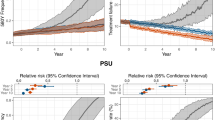
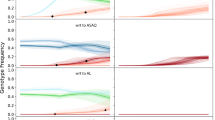
The search identified 40 studies, comprising 76 distinct treatment arms, which met the inclusion criteria (37 from the WWARN database and 3 from secondary searches of references in those articles). The earliest study was reported in 1984, and the most recent in 2016. The majority of studies were performed in Asia (n = 33) with seven reported from Sub-Saharan Africa. Twenty-five studies included participants aged 15 years or older, thirteen enrolled children and adults and for two studies this information was not available. The treatment arms were artesunate (n = 48) artemether (10), artemisinin (10), dihydroartemisinin (7) or beta-cyclodextrin-artemisinin complex (1) all given in a variety of doses, dosing intervals, routes and treatment course durations (Fig. 1).
The logistic meta-regression model estimated that the duration of treatment was the main determinant of efficacy (95% confidence interval did not contain zero) and that the number of doses explained none of the residual variance (95% confidence interval was centred approximately at 0). Thus for regimens of artemisinins that were sub-optimal (i.e. gave sub-maximal cure rates), having more than one dose per day provided no benefit over once daily administration. To check the assumption that each dose administered in these various studies produces the maximum parasiticidal effect a logistic meta-regression was performed using only studies with the most frequently evaluated drug, oral artesunate, (n = 39). This found that the dose in mg/kg was not a significant predictor of efficacy (lowest doses were 1.6 mg/kg). This confirms that ~2 mg/kg gives almost maximum antiparasitic effects in artemisinin-sensitive P. falciparum infections.
Discussion
For antimalarial treatments with artemisinin or its derivatives there is no evidence that split dosing either accelerates parasite clearance or augments cure rates significantly. In those studies where cure rates were sub-maximal, and the conjectured “dramatic enhancement of drug effectiveness” should have been evident, none was found. An effect of dose frequency on treatment efficacy was observed in a small study of 43 patients in which once daily artemether-lumefantrine was compared with standard twice daily dosing. In that study PCR adjusted cure rates were 85.1% and 94.4% respectively but this difference was explained entirely by 30% lower lumefantrine levels in the former group since lumefantrine exposure is the principal determinant of cure following treatment with this ACT32. In studies of artemisinin monotherapies where twice or thrice daily administration has been evaluated, and in contemporary or sequential comparisons with once daily administration there is no evidence that cure rates are substantially higher with more than once daily dosing1,3,4,5,6,7,8,9,10,11,12,13,33,34,35,36,37,38.
Furthermore there is no evidence that splenic clearance functions are as low as the values needed to sustain this hypothesis16,18,39. Taken together there is no clinical support for these PK-PD modelling predictions, which appear to be wrong. The fundamental problem is probably the modelling of parasite killing and clearance in falciparum malaria as a simple first order process14,18,39. Whilst the decline in parasite densities is log linear, and can therefore be described as a first order process, it seems that once daily exposures to artemisinin or its derivatives produce maximum effects in the majority of patients. The kinetics of malaria parasite killing and parasite recovery are more complex than currently modelled.
Data availability statement
The data are uploaded as a supplementary file.
References
Qinghaosu Antimalarial Coordinating Research Group. Antimalaria studies on Qinghaosu. Chinese Medical Journal 92, 811–816 (1979).
Jiang, J. B., Li, G. Q., Guo, X. B., Kong, Y. C. & Arnold, K. Antimalarial activity of mefloquine and qinghaosu. Lancet 2, 285–288 (1982).
Li, G. Q. et al. Clinical studies on treatment of cerebral malaria with qinghaosu and its derivatives. Journal of Traditional Chinese Medicine=Chung i tsa chih ying wen pan 2, 125–130 (1982).
Bunnag, D., Viravan, C., Looareesuwan, S., Karbwang, J. & Harinasuta, T. Double blind randomised clinical trial of oral artesunate at once or twice daily dose in falciparum malaria. The Southeast Asian Journal of Tropical Medicine and Public Health 22, 539–543 (1991).
Bunnag, D., Viravan, C., Looareesuwan, S., Karbwang, J. & Harinasuta, T. Clinical trial of artesunate and artemether on multidrug resistant falciparum malaria in Thailand. A preliminary report. The Southeast Asian Journal of Tropical Medicine and Public Health 22, 380–385 (1991).
Bunnag, D., Viravan, C., Looareesuwan, S., Karbwang, J. & Harinasuta, T. Double blind randomised clinical trial of two different regimens of oral artesunate in falciparum malaria. The Southeast Asian Journal of Tropical Medicine and Public Health 22, 534–538 (1991).
Bunnag, D., Karbwang, J. & Harinasuta, T. Artemether in the treatment of multiple drug resistant falciparum malaria. The Southeast Asian Journal of Tropical Medicine and Public Health 23, 762–767 (1992).
Looareesuwan, S. Overview of clinical studies on artemisinin derivatives in Thailand. Transactions of the Royal Society of Tropical Medicine and Hygiene 88(Suppl 1), S9–11 (1994).
Li, G. Q., Guo, X. B., Fu, L. C., Jian, H. X. & Wang, X. H. Clinical trials of artemisinin and its derivatives in the treatment of malaria in China. Transactions of the Royal Society of Tropical Medicine and Hygiene 88(Suppl 1), S5–6 (1994).
Hien, T. T. An overview of the clinical use of artemisinin and its derivatives in the treatment of falciparum malaria in Viet Nam. Transactions of the Royal Society of Tropical Medicine and Hygiene 88(Suppl 1), S7–8 (1994).
Nosten, F. et al. Treatment of multidrug-resistant Plasmodium falciparum malaria with 3-day artesunate-mefloquine combination. The Journal of Infectious Diseases 170, 971–977 (1994).
Luxemburger, C. et al. Single day mefloquine-artesunate combination in the treatment of multi-drug resistant falciparum malaria. Transactions of the Royal Society of Tropical Medicine and Hygiene 88, 213–217 (1994).
McIntosh, H. M. & Olliaro, P. Artemisinin derivatives for treating uncomplicated malaria. The Cochrane database of systematic reviews, CD000256. https://doi.org/10.1002/14651858.CD000256 (2000).
Saralamba, S. et al. Intrahost modeling of artemisinin resistance in Plasmodium falciparum. Proceedings of the National Academy of Sciences of the United States of America 108, 397–402, https://doi.org/10.1073/pnas.1006113108 (2011).
Dogovski, C. et al. Targeting the cell stress response of Plasmodium falciparum to overcome artemisinin resistance. PLoS Biology 13, e1002132, https://doi.org/10.1371/journal.pbio.1002132 (2015).
Kay, K. & Hastings, I. M. Improving pharmacokinetic-pharmacodynamic modeling to investigate anti-infective chemotherapy with application to the current generation of antimalarial drugs. PLoS Computational Biology 9, e1003151, https://doi.org/10.1371/journal.pcbi.1003151 (2013).
Hastings, I. M., Kay, K. & Hodel, E. M. How Robust Are Malaria Parasite Clearance Rates as Indicators of Drug Effectiveness and Resistance? Antimicrobial Agents and Chemotherapy 59, 6428–6436, https://doi.org/10.1128/AAC.00481-15 (2015).
Kay, K., Hodel, E. M. & Hastings, I. M. Altering Antimalarial Drug Regimens May Dramatically Enhance and Restore Drug Effectiveness. Antimicrobial Agents and Chemotherapy 59, 6419–6427, https://doi.org/10.1128/AAC.00482-15 (2015).
WWARN Parasite Clearance Study Group et al. Baseline data of parasite clearance in patients with falciparum malaria treated with an artemisinin derivative: an individual patient data meta-analysis. Malaria Journal 14, 359, doi:https://doi.org/10.1186/s12936-015-0874-1 (2015).
Phu, N. H. et al. Randomized controlled trial of artesunate or artemether in Vietnamese adults with severe falciparum malaria. Malaria Journal 9, 97, https://doi.org/10.1186/1475-2875-9-97 (2010).
Phyo, A. P. et al. Antimalarial activity of artefenomel (OZ439), a novel synthetic antimalarial endoperoxide, in patients with Plasmodium falciparum and Plasmodium vivax malaria: an open-label phase 2 trial. The Lancet Infectious Diseases 16, 61–69, https://doi.org/10.1016/S1473-3099(15)00320-5 (2016).
Gordi, T., Xie, R. & Jusko, W. J. Semi-mechanistic pharmacokinetic/pharmacodynamic modelling of the antimalarial effect of artemisinin. British Journal of Clinical Pharmacology 60, 594–604, https://doi.org/10.1111/j.1365-2125.2005.02508.x (2005).
Hastings, I. M., Hodel, E. M. & Kay, K. Quantifying the pharmacology of antimalarial drug combination therapy. Scientific Reports 6, 32762, https://doi.org/10.1038/srep32762 (2016).
Stepniewska, K. et al. In vivo parasitological measures of artemisinin susceptibility. The Journal of Infectious Diseases 201, 570–579, https://doi.org/10.1086/650301 (2010).
Kyaw, M. P. et al. Reduced susceptibility of Plasmodium falciparum to artesunate in southern Myanmar. PloS One 8, e57689, https://doi.org/10.1371/journal.pone.0057689 (2013).
Dondorp, A. M. et al. Artemisinin resistance in Plasmodium falciparum malaria. The New England Journal of Medicine 361, 455–467, https://doi.org/10.1056/NEJMoa0808859 (2009).
Ashley, E. A. et al. Spread of artemisinin resistance in Plasmodium falciparum malaria. The New England Journal of Medicine 371, 411–423, https://doi.org/10.1056/NEJMoa1314981 (2014).
Nkhoma, S. C. et al. Genetic evaluation of the performance of malaria parasite clearance rate metrics. The Journal of Infectious Diseases 208, 346–350, https://doi.org/10.1093/infdis/jit165 (2013).
Ataide, R. et al. Host immunity to Plasmodium falciparum and the assessment of emerging artemisinin resistance in a multinational cohort. Proceedings of the National Academy of Sciences of the United States of America 114, 3515–3520, https://doi.org/10.1073/pnas.1615875114 (2017).
WWARN Artemisinin based Combination Therapy Africa Baseline Study Group et al. Clinical determinants of early parasitological response to ACTs in African patients with uncomplicated falciparum malaria: a literature review and meta-analysis of individual patient data. BMC medicine 13, 212, doi:https://doi.org/10.1186/s12916-015-0445-x (2015).
WorldWide Antimalarial Resistance Network. WWARN Clinical Trials Publication library., http://www.wwarn.org/tools-resources/literature-reviews/wwarn-clinical-trials-publication-library (2017).
Ashley, E. A. et al. Pharmacokinetic study of artemether-lumefantrine given once daily for the treatment of uncomplicated multidrug-resistant falciparum malaria. Tropical Medicine & International Health: TM & IH 12, 201–208, https://doi.org/10.1111/j.1365-3156.2006.01785.x (2007).
Ramharter, M. et al. Artesunate-clindamycin versus quinine-clindamycin in the treatment of Plasmodium falciparum malaria: a randomized controlled trial. Clinical Infectious Diseases 40, 1777–1784, https://doi.org/10.1086/430309 (2005).
Ashley, E. A. et al. A randomized, controlled study of a simple, once-daily regimen of dihydroartemisinin-piperaquine for the treatment of uncomplicated, multidrug-resistant falciparum malaria. Clinical Infectious Diseases 41, 425–432, https://doi.org/10.1086/432011 (2005).
Noedl, H. et al. Artemisinin resistance in Cambodia: a clinical trial designed to address an emerging problem in Southeast Asia. Clinical Infectious Diseases 51, e82–89, https://doi.org/10.1086/657120 (2010).
Das, D. et al. Effect of high-dose or split-dose artesunate on parasite clearance in artemisinin-resistant falciparum malaria. Clinical Infectious Diseases 56, e48–58, https://doi.org/10.1093/cid/cis958 (2013).
Kremsner, P. G. et al. Intramuscular Artesunate for Severe Malaria in African Children: A Multicenter Randomized Controlled Trial. PLoS Medicine 13, e1001938, https://doi.org/10.1371/journal.pmed.1001938 (2016).
Looareesuwan, S. et al. Open randomized trial of oral artemether alone and a sequential combination with mefloquine for acute uncomplicated falciparum malaria. The American Journal of Tropical Medicine and Hygiene 56, 613–617 (1997).
White, N. J. Malaria parasite clearance. Malaria Journal 16, 88, https://doi.org/10.1186/s12936-017-1731-1 (2017).
Acknowledgements
This investigation was part of the Mahidol -Oxford Tropical Medicine Research Unit activities supported by the Wellcome Trust of Great Britain.
Author information
Authors and Affiliations
Contributions
E.A. performed the literature search, J.W. analysed the data, N.J.W. conceived the investigation and wrote the first draft of the manuscript. All authors contributed to the design, data interpretation and content of the submitted version.
Corresponding author
Ethics declarations
Competing Interests
The authors declare that they have no competing interests.
Additional information
Publisher's note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
White, N.J., Watson, J. & Ashley, E.A. Split dosing of artemisinins does not improve antimalarial therapeutic efficacy. Sci Rep 7, 12132 (2017). https://doi.org/10.1038/s41598-017-12483-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-017-12483-4
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.