Abstract
This study was designed to investigate the associations between TERT overexpression and the clinicopathologic factors of hepatocellular carcinoma (HCC). A total of 291 patients with HCC were enrolled. The site of first recurrence (anywhere in the liver) was classified as intrahepatic recurrence (IHR). Recurrence was then sub classified as either early or late IHR according to whether it was discovered within 2 years of resection, or after, respectively. TERT overexpression was not significantly correlated with previously recognized prognostic factors. During follow-up, early IHR occurred in 126 (63.6%) patients, while late IHR was detected in 59 patients among 145 patients who remained free of HCC recurrence for ≥ 2 years after surgery. Multivariate analysis showed late IHR was significantly correlated with TERT overexpression (P < 0.001, hazard ratio [HR] 2.67, 95% confidence interval [CI] 1.51–4.72). Intrahepatic metastasis (P < 0.001, HR 4.48, 95% CI 2.62–7.65) and TERT overexpression (P < 0.001, HR 1.77, 95% CI 1.28–2.45) were significant prognostic factors for IHR-free survival in both univariate and multivariate analyses. TERT overexpression was the only significant prognostic factor for late IHR in HCC treated with curative resection. And, the statistical significance of TERT overexpression on late IHR was limited to HBsAg-positive patients.
Similar content being viewed by others
Introduction
Hepatocellular carcinoma (HCC) remains one of the most challenging health problems worldwide despite the hepatitis B virus (HBV) vaccine, surveillance in high-risk patients, potent antiviral agents, and imaging and treatment modalities. Currently, HCC is the fifth most common cancer, and the second leading cause of cancer-related death worldwide1.
The Barcelona Clinic Liver Cancer (BCLC) system is the most widely used HCC staging and treatment guideline. According to BCLC, the curative treatments for HCC include liver transplantation (LT), surgical resection, and local ablative therapy, including radiofrequency ablation (RFA)2. One study found that the local control rate of HCC was comparable between surgical resection and RFA3. Surgical resection is generally preferred, if possible, however, because of the difference in overall recurrence after surgery compared to that after other treatment modalities4,5,6. Unfortunately, recurrence is still detected in approximately 50% of patients after surgical resection7. There is no standardized adjuvant treatment modality after HCC surgical resection. Therefore, it is very important to identify reliable biomarkers of recurrence, as well as the most probable sites of recurrence, in order to develop customized management plans.
Telomerase reverse transcriptase (TERT) is a core catalytic component of telomerase that plays a crucial role in maintaining telomere length8. In most somatic cells, TERT expression is suppressed. In contrast, TERT is actively expressed in self-renewing cells, such as stem cells9. Overexpression of TERT and telomere dysfunction is frequently detected in a variety of human cancer specimens, including thyroid cancer10, bladder cancer11, melanoma12, and brain tumors13. This TERT overexpression is detected in up to 90% of cancer cells, compared to in <20% of normal cells14. Evidence has suggested that TERT overexpression in HCC is associated with poor clinical outcomes; however, this hypothesis was based on a small patient population, without consideration of other clinicopathologic factors that might affect clinical outcomes15. Therefore, it is essential to more precisely evaluate the role of TERT overexpression in HCC, as well as that of other clinicopathologic factors in homogenously-treated patients.
We investigated the associations between TERT overexpression and the clinicopathologic factors of HCC in Korean patients mainly caused by HBV infection. We also studied the clinical significance of TERT overexpression with regard to HCC recurrence and survival duration
Results
Patients
The patients and tumor characteristics of the 291 enrolled cases of HCC are displayed in Table 1. The median age was 53 years (range, 17 to 76 years). More than 80% of the patients were male. All but one patient had Child-Pugh class A status. The median alpha-fetoprotein (AFP) level was 169.5 ng/ml (range, 1.0–1667054.0 ng/ml). Approximately one third of the patients (109, 37.5%) were staged as B, while 15 patients (5.2%) were staged as C via the Barcelona Clinic Liver Cancer staging system. According to the Milan criteria, 173 patients were satisfied with the criteria, while 118 patients were not. The median follow-up period was 134.8 months (range, 1.7–193.4 months).
Correlation between TERT messenger ribonucleic acid (RNA) expression and clinicopathologic variables
Gene expression analysis using quantitative Reverse-Transcriptase Polymerase Chain Reaction (qRT-PCR) revealed that TERT messenger RNA (mRNA) expression was significantly higher in HCC tissues than it was in background, non-tumor liver tissue (at least 2 cm from the HCC) and normal liver tissues. Normal liver tissue was obtained from patients who underwent hepatectomy due to pathologically-confirmed metastatic colon cancer to the liver without a history of viral hepatitis or alcohol use (P < 0.001, Fig. 1). The median value of normalized TERT mRNA expression values was 0.46 (range, 0.00–908.87). A TERT mRNA value of 0.3 was defined as the cut-off point for high expression of overall recurrence in this present study. This value was based on the highest Youden index values of 1.3147 and 1.3195 with TERT mRNA values of 0.317 and 0.297 (P-values 0.0006 for both cut-off points). Diagnostic accuracy of TERT mRNA of 0.3 to predict recurrence and survival was displayed in Supplementary Table 1. And, the sensitivity, specificity, positive predictive value, negative predictive value, positive likelihood ratio, and negative likelihood ratio of TERT mRNA value of 0.3 was 71.3%, 45.6%, 12.6%, 93.5%, 1.31 and 0.63 at 3-year IHR, respectively. For internal validation of the estimated cut-off value of TERT expression, the median of the estimated cut-off values of 1000 bootstrap samples was 0.3 with a 95% confidence interval of 0.3.
TERT mRNA expression in normal and HCC tissues: TERT mRNA expression (measured using quantitative RT-PCR) was significantly higher in HCC tissues than in adjacent, normal liver tissues (at least 2 cm from the HCC) and in normal liver tissues (obtained from patients after hepatectomy performed for pathology-confirmed metastatic colon cancer of the liver in the absence of viral hepatitis and history of alcohol use).
The correlations between elevated TERT mRNA expression and clinicopathologic variables are displayed in Supplementary Table 2. High TERT expression was not significantly associated with any other factors, including well-known prognostic factors for HCC recurrence after surgical resection. These factors for HCC recurrence include Edmonson grade (P = 0.67), microvascular invasion (P = 0.91), intrahepatic metastasis (P = 0.40), and background liver status (P = 0.89).
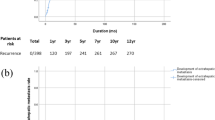
Recurrence patterns and clinicopathologic variables
During the follow-up period, overall recurrence was detected in 198 (68.0%) patients. Among them, 103 (35.4%) patients had isolated intrahepatic recurrence (IHR), 82 (28.2%) had both IHR and distant metastases (DM), and the remaining 13 (4.5%) had isolated DM. Among all of the patients with IHR (with or without DM), early IHR developed in 126 (63.6%) patients. In contrast, late IHR was detected in 59 of the 145 patients that were followed for over 2 years. The estimated recurrence rate (per month) after surgical resection is displayed in Fig. 2A. The highest recurrence rate was detected within 6 months of resection, and decreased gradually thereafter. There was a relatively stable rate of recurrence after 3 years postoperatively, at approximately 0.005% per month.
The results of univariate and multivariate analyses of clinicopathologic variables and early/late IHR are displayed in Tables 2 and 3. Multivariate analysis showed early IHR was significantly correlated with tumors ≥ 5 cm in size (P = 0.02, hazard ratio [HR] 2.81, 95% confidence interval [CI] 1.20–6.60), and intrahepatic metastasis (P < 0.001, HR 5.27, 95% CI 2.81–9.87). Early IHR was somewhat related to TERT expression, although the trend was not statistically significant (P = 0.08, HR 1.41, 95% CI 0.96–2.08).
In contrast, late IHR was not significantly correlated with any variables, including those known to be significant prognostic factors of HCC, including microvascular invasion (P = 0.72), intrahepatic metastasis (P = 0.75), and BCLC stage (P = 0.33). Multivariate analysis showed TERT expression (P < 0.001, HR 2.67, 95% CI 1.51–4.72) and HBsAg (P = 0.02, HR 2.27, 95% CI 1.16–4.46) were the only significant prognostic factors for late IHR. In the subgroup analysis by HBsAg status, late IHR was significantly associated with TERT overexpression in HBsAg-positive patients (P = 0.002, HR 2.77, 95% CI 1.44–5.34), but not in HBsAg-negative patients (P = 0.22, HR 2.70, 95% CI 0.55–13.25). The monthly IHR rate according to probable prognostic clinicopathologic factors is displayed in Fig. 2B–D. Even after two years, the IHR curve for TERT overexpression was maintained at a higher level compared to that of non-TERT overexpression.
Survival outcomes and probable prognostic factors
Table 4 summarizes the univariate analysis results of overall IHR-free survival (IHRFS), DM-free survival (DMFS), and recurrence-free survival (RFS) according to probable prognostic factors.
Multivariate analysis (Table 5) showed statistical significance only for TERT overexpression (P < 0.001, HR 1.77, 95% CI 1.28–2.45, Fig. 3A) and intrahepatic metastasis (P < 0.001, HR 4.48, 95% CI 2.62–7.65, Fig. 3B) on overall IHRFS. ALBI grade was marginally significant (P = 0.05, HR 1.42, 95% CI 0.99–2.04, Fig. 3C). In the DMFS, intrahepatic metastasis (P = 0.02, HR 2.50, 95% CI 1.14–5.47, Supplementary Fig. 1A) was the only significant prognostic factor, while Edmonson grade was marginally significant (P = 0.06, HR 1.79, 95% CI 0.97–3.30, Supplementary Fig. 1B). In addition, DMFS did not vary according to TERT expression (P = 0.86, Supplementary Fig. 1C). Finally, RFS was significantly affected by intrahepatic metastasis (P < 0.001, HR 3.33, 95% CI 1.93–5.77, Fig. 1D) and marginally by ALBI grade (P = 0.06, HR 1.39, 95% CI 0.99–1.97, Fig. 3D). TERT expression did not affect RFS (P = 0.56, HR 1.12, 95% CI 0.77–1.65); however, the effect of TERT expression (P = 0.005, HR 1.01, 95% CI 1.00–1.02) on RFS increased with time.
Kaplan-Meier survival curves according to probable prognostic factors: TERT overexpression (A) and intrahepatic metastasis (B) were significant prognostic factors of IHRFS and ALBI grade (C) was marginally significant on multivariate analysis. Intrahepatic metastasis (D) was also a significant prognostic factor for RFS.
We performed predictive grouping of IHRFS according to the significant or marginally significant factors (ALBI grade, intrahepatic metastasis and TERT overexpression) using the following criteria: group 1, no risk factor; group 2, one risk factor; group 3, two risk factors; and group 4, all three risk factors. The curves for IHRFS, DMFS, RFS, and overall survival (OS) according to the risk groupings are shown in Fig. 4. Although the survival curves are significantly different according to group (all P < 0.001), an even clearer stratification was identified for IHRFS and RFS. According to the risk grouping, the median IHRFS was not reached in group 1, was 50.3 months (95% CI, 29.4–71.3 months) in group 2, 10.3 months (95% CI, 5.5–15.1 months) in group 3, and 3.4 months in group 4 (95% CI, 0.3–6.4 months). Similarly, RFS was not reached in group 1, but was 42.5 months (95% CI, 19.6–65.4 months) in group 2, 9.4 months (95% CI, 4.9–13.9 months) in group 3, and 3.41 months in group 4 (95% CI, 2.1–4.1 months).
Discussion
In this study, we evaluated the correlation between clinicopathologic variables and the prognostic significance of TERT overexpression in HCC treated with curative surgical resection. Interestingly, TERT overexpression was not related to other clinicopathologic variables, including well-known prognostic factors for HCC. Instead, TERT overexpression was significantly correlated with late IHR (occurring two years or later after surgical resection). The previously identified prognostic factors for HCC were only related to early IHR in our study. Furthermore, the prognostic significance of TERT overexpression on overall IHRFS was maintained in multivariate analysis.
The TERT is the most important unit of the telomerase complex, which allows potentially unlimited cell proliferation through the addition of repeated TTAGGG sequences and subsequent telomere maintenance16. In most normal somatic cells, TERT expression is suppressed and strictly controlled by transcriptional regulation; in some self-renewing cells such as stem cells and/or reproductive cells, however, TERT is expressed more ubiquitously9. There has been a lot of interest in understanding the pivotal role of increased TERT-mediated telomere maintenance in HCC carcinogenesis17. The mechanisms by which TERT expression is increased in HCC may include TERT gene amplification18, and TERT promoter mutations19,20.
In addition to HCC carcinogenesis17, TERT abnormalities also have prognostic significance in thyroid cancer10, bladder cancer21, and brain tumors13. In HCC, however, there are few studies defining the role of TERT expression as a prognosticator for the disease. It also remains to be determined whether TERT expression during recurrence reflects metastasis or a new primary lesion. Therefore, understanding the crucial role of TERT expression in HCC carcinogenesis17, as well as its clinical significance on metastasis and/or de novo primary HCC is extremely important for optimizing HCC management.
This study reveals the prognostic significance of TERT expression on IHRFS. With the exception of other potential confounders during multivariate analysis, TERT expression demonstrated an HR of 1.78 on overall IHRFS. Although the HR of TERT expression on IHRFS was lower than that of intrahepatic metastasis (HR 4.22), it still suggests that it is an independent prognostic factor for overall IHRFS. There was no statistically significant correlation between intrahepatic metastasis and TERT expression (Supplementary Table 2).
With the exception of HBsAg status, TERT was the only significant prognostic factor for late IHR. As displayed in Fig. 3, most cases of IHR developed within 2 years of initial resection in patients with intrahepatic metastasis. In those with TERT expression, more than half of the IHR cases were detected more than 2 years after initial resection. This finding suggests that TERT expression is more closely related to de novo primary HCC, rather than recurrence, in patients initially treated with curative surgical resection.
The subgroup analysis by HBsAg status revealed that a statistically significant association between late IHR and TERT overexpression was limited to HBsAg-positive patients. The most frequent mechanism by which HBV infection leads to TERT overexpression is related to insertional mutagenesis by the virus itself rather than promoter mutations or gene amplification, which is seen in other liver diseases including HCV infection18,20,22,23. Integration of HBV was seen in 22% of the HBV positive patients whereas gene amplification was seen in 6.7%18. Although it is assumed that HBV integration would be a major cause of TERT overexpression in our samples, we cannot rule out the possibility of other genetic alterations that are involved in the TERT overexpression. Future work is needed to uncover the molecular mechanism underlying the overexpression of TERT and the correlation with late IHR.
Prior research has found that TERT expression induced by TERT promoter mutations is one of the earliest genetic events identified in pre-neoplastic lesions in cirrhotic livers17. Therefore, high TERT expression in resected HCC might reflect potential cancer development in the surrounding liver. If this were true, then one could hypothesize that there would be a higher incidence of de novo primary HCC lesions in patients who had TERT expression after hepatic resection. Like other studies in which genetic factors were associated with late tumor recurrence in HCC24,25, TERT expression was significantly correlated with late IHR in this study. Patients with high TERT expression, therefore, may require more intensive follow-up after surgical resection. In addition, considering that DMFS was unaffected by TERT expression, it may be important to consider LT, rather than liver resection, in order to improve clinical outcomes in these patients. Further evaluation is needed to clarify the clinical significance of TERT expression in the patients treated with LT.
The role of ALBI grade as a prognosticator for OS is well recognized in HCC, including in patients treated with curative surgical resection26,27,28,29. Although one group found a slightly higher tendency of recurrence in ALBI grade II than in grade I, some have suggested that ALBI grade is not a significant prognostic factor for HCC recurrence after curative liver resection26. Interestingly, however, ALBI grade itself had a marginally significant role as a prognostic factor in this study. There was a marginal survival difference between RFS and IHRFS according to ALBI grade. Correlation analysis showed ALBI grade was significantly related to background liver status and marginally related to HBsAg status (Supplementary Table 3). Therefore, ALBI grade could predict IHR by reflecting the status of the surrounding liver. Regardless, a larger study is needed to evaluate the role of the ALBI grade as a prognostic factor for HCC recurrence.
This study has several limitations that warrant consideration. First, we evaluated the expression of TERT mRNA, but not of TERT promoter mutations and telomere lengthening. However, there is a well-recognized correlation between TERT promotor mutations, TERT expression, and telomere lengthening in other studies. Second, this study has unavoidable selection bias given that it was a single institution, retrospective study. Third, diagnostic performance of TERT mRNA value of 0.3 was not sufficiently high as 61.9 to 71.3% of sensitivity and it has never been validated by independent external data. Finally, we only included patients who had undergone curative surgical resection for HCC. Therefore, our results ought to be interpreted with caution, as they may not be generalizable to HCC patients treated with other modalities. To apply the outcomes of the present study in clinical practice, it is essential to reproduce the results through prospectively designed independent multicenter studies. Future research with larger, prospective studies is needed to substantiate the clinical significance of TERT expression in HCC recurrence.
Nevertheless, this study provides valuable information that is relevant for further study and consequent modifications of HCC management. TERT expression was a significant prognostic factor for IHRFS and RFS. In addition, TERT expression was the only significant factor for late IHR in patients treated with curative hepatic resection. Therefore, close follow-up and/or treatment modifications for resectable HCC according to TERT expression might improve clinical outcomes in these patients.
Conclusions
In this study conducted in the HBV endemic area, TERT overexpression was not related to previously known HCC prognostic factors treated with curative surgical resection. Known HCC prognostic factors were correlated with early IHR, while TERT overexpression was the only significant prognostic factor for late IHR. Besides TERT overexpression, ALBI grade and presence of intrahepatic metastasis also had prognostic significance in IHRFS and RFS. Further research is needed to substantiate these findings.
Materials and Methods
Patients
Cancer tissue from patients with histologically confirmed HCC at Samsung Medical Center (Seoul, Korea) between July 2000 and May 2006 was used in this present study. Patients were eligible if they underwent complete surgical resection with curative intent. Complete resection was defined as the removal of all hepatic tumor nodules with microscopic clear resection margins. Any patients who received neoadjuvant or adjuvant treatments were excluded. The Institutional Review Board at Samsung Medical Center approved this study, and waived informed consent.
Prior to surgery, patients underwent a work-up of their liver function and HCC status. This examination included the following: comprehensive history, patient demographics, viral marker, chest X-ray, complete blood count, chemistry profile, liver function test, indocyanin green retention test, AFP level, and contrast enhanced liver CT and/or magnetic resonance imaging (MRI) of the abdomen and pelvis. Chest CT and whole body bone scan were performed to rule out distant metastasis. Positron emission tomography (PET)-CT was alternatively used for the same purpose at the physician’s discretion.
Patients were generally followed every two to three months after surgical resection. During the follow-up period, evaluations included physical examinations, laboratory tests (including liver function tests and AFP), chest X-rays, and CT of the abdomen and pelvis. Patients with suspicious imaging findings and/or continuously elevated AFP levels were further evaluated with PET-CT and/or MRI.
Based on the Liver Cancer Study Group of Japan guidelines, the following histological parameters were postoperatively assessed: largest tumor diameter, number of tumors, microvascular invasion, and intrahepatic metastasis16. The resected HCC tissues were graded according to the Edmonson and Steiner grading system: grade I (well differentiated), grade II (moderately differentiated), or grade III (poorly differentiated)30.
RNA extraction and qRT-PCR
The total RNA was isolated from fresh samples using the ReliaPrepTM FFPE Total RNA Miniprep System (Promega, Madison, WI). RNA was reverse transcribed using a high-capacity, complementary deoxyrinuleic acid (cDNA) Reverse Transcription Kit (Life Technologies, Invitrogen, Carlsbad, CA) according to the manufacturer’s instructions. The expression of TERT was measured using a gene expression assay containing forward and reverse primers, and a FAM-labeled MGB TaqMan probe from Applied Biosystems (assay ID; Hs00972650_m1, Thermo-Fisher Scientific, Waltham, MA) for the detection of overlap at the exon 3-exon 4 junctions. GAPDH was used as an endogenous control (assay ID; Hs99999905_m1, Thermo-Fisher Scientific). The PCR reaction mixture contained TaqMan Universal PCR master mix with AmpErase UNG (Applied Biosystems, Foster City, CA), 900-nM primers (forward and reverse), 250 nM TaqMan probe, and 5 μl of cDNA sample for a total reaction volume of 20 μl. The PCR conditions were as follows: 95 °C for 10 min followed by 40 cycles of amplification at 95 °C for 15 s, and 60 °C for 1 min using the ABI PRISM 7500HT Fast Real-time PCR system (Applied Biosystems). The threshold cycle (Ct), which is the fractional cycle number at which the amount of amplified target reached a fixed threshold, was determined. The relative changes in gene expression were measured using the 2−ΔΔCt (ΔΔCt = ΔCttarget gene − ΔCtGAPDH) method.
Definition of recurrence and statistical analysis
Recurrence was generally diagnosed using radiologic examinations without histologic confirmation, except in patients for whom further surgical resection or liver transplantation was indicated. The site of first recurrence was classified as IHR, which is defined as recurrence occurring anywhere inside the entire liver. The IHR was sub classified as either early recurrence or late recurrence according to whether it was detected <2 years or ≥2 years after the initial surgery, respectively. This cut-off point was based on the study by Imamura et al.31. All other sites of recurrence were defined as DM.
The duration of IHRFS, DMFS, RFS, and OS were calculated from the date of surgical resection to the date of each event, or the last day of follow-up.
The cut-off value of TERT mRNA expression on overall recurrence was determined using the log-rank test and the minimum p-value approach. For internal validation of the estimated cut-off value of TERT expression level, the distribution of the cut-off values was examined using 1000 bootstrap samples with replacement from the study data. P-values < 0.05 were considered statistically significant in two-tailed tests. The correlation between high TERT expression or intrahepatic metastasis and other clinicopathologic variables was evaluated using the Chi-square or Fisher’s exact tests. Univariate analysis was performed using the Cox proportional hazard model or the time-dependent Cox model according to satisfaction of the proportional hazard assumption for each variable. The proportional hazard assumption was confirmed using the correlation between partial residuals from the estimated Cox proportional hazard model and the time to the event. Variables with P < 0.1 in univariate analysis were included in the multivariate analysis. Multivariate analysis was conducted using a time-dependent Cox model, because some variables included in the multivariate analysis were against the proportional hazard assumption. Multicollinearity was identified by a Variance Inflation Factor (VIF) > 4.0. Some of those variables were excluded from the multivariate analysis. Statistical analyses were performed using SAS version 9.4 (SAS Institute, Cary, NC). Variable risk was expressed as an HR with corresponding 95% CI.
References
Torre, L. A. et al. Global cancer statistics, 2012. CA Cancer J. Clin. 65, 87–108 (2015).
Forner, A., Llovet, J. M. & Bruix, J. Hepatocellular carcinoma. Lancet 379, 1245–1255 (2012).
Huang, J. et al. A randomized trial comparing radiofrequency ablation and surgical resection for HCC conforming to the Milan criteria. Ann. Surg. 252, 903–912 (2010).
Fu, C. et al. Radiofrequency ablation vs. surgical resection on the treatment of patients with small hepatocellular carcinoma: a system review and meta-analysis of five randomized controlled trials. Hepatogastroenterology 61, 1722–1729 (2014).
Gory, I. et al. Radiofrequency ablation versus resection for the treatment of early stage hepatocellular carcinoma: a multicenter Australian study. Scand. J. Gastroenterol. 50, 567–576 (2015).
Liu, H. et al. Randomized clinical trial of chemoembolization plus radiofrequency ablation versus partial hepatectomy for hepatocellular carcinoma within the Milan criteria. Br. J. Surg. 103, 348–356 (2016).
Sposito, C. et al. Propensity score analysis of outcomes following laparoscopic or open liver resection for hepatocellular carcinoma. Br. J. Surg. 103, 871–880 (2016).
Smogorzewska, A. & de Lange, T. Regulation of telomerase by telomeric proteins. Annu. Rev. Biochem. 73, 177–208 (2004).
Blasco, M. A. Telomeres and human disease: ageing, cancer and beyond. Nat. Rev. Genet. 6, 611–622 (2005).
Xing, M. et al. BRAF V600E and TERT promoter mutations cooperatively identify the most aggressive papillary thyroid cancer with highest recurrence. J. Clin. Oncol. 32, 2718–2726 (2014).
Li, C. et al. The C228T mutation of TERT promoter frequently occurs in bladder cancer stem cells and contributes to tumorigenesis of bladder cancer. Oncotarget 6, 19542–19551 (2015).
Shain, A. H. et al. The Genetic Evolution of Melanoma from Precursor Lesions. N. Engl. J. Med. 373, 1926–1936 (2015).
Yang, P. et al. Classification based on mutations of TERT promoter and IDH characterizes subtypes in grade II/III gliomas. Neuro Oncol. 18, 1099–1108 (2016).
Kim, N. W. et al. Specific association of human telomerase activity with immortal cells and cancer. Science 266, 2011–2015 (1994).
Ko, E., Seo, H. W., Jung, E. S., Kim, B. H. & Jung, G. The TERT promoter SNP rs2853669 decreases E2F1 transcription factor binding and increases mortality and recurrence risks in liver cancer. Oncotarget 7, 684-699 (2016).
Morin, G. B. The human telomere terminal transferase enzyme is a ribonucleoprotein that synthesizes TTAGGG repeats. Cell 59, 521–529 (1989).
Nault, J. C. et al. Telomerase reverse transcriptase promoter mutation is an early somatic genetic alteration in the transformation of premalignant nodules in hepatocellular carcinoma on cirrhosis. Hepatology 60, 1983–1992 (2014).
Totoki, Y. et al. Trans-ancestry mutational landscape of hepatocellular carcinoma genomes. Nat. Genet. 46, 1267–1273 (2014).
Schulze, K. et al. Exome sequencing of hepatocellular carcinomas identifies new mutational signatures and potential therapeutic targets. Nat. Genet. 47, 505–511 (2015).
Sung, W. K. et al. Genome-wide survey of recurrent HBV integration in hepatocellular carcinoma. Nat. Genet. 44, 765–769 (2012).
Wang, K. et al. TERT promoter mutations are associated with distant metastases in upper tract urothelial carcinomas and serve as urinary biomarkers detected by a sensitive castPCR. Oncotarget 5, 12428–12439 (2014).
Donati, B. & Valenti, L. Telomeres, NAFLD and Chronic Liver Disease. International journal of molecular sciences 17, 383 (2016).
Paterlini-Brechot, P. et al. Hepatitis B virus-related insertional mutagenesis occurs frequently in human liver cancers and recurrently targets human telomerase gene. Oncogene 22, 3911–3916 (2003). 24.
Chan, A. W. et al. Steatotic hepatocellular carcinoma: a variant associated with metabolic factors and late tumour relapse. Histopathology 69, 971–984 (2016).
Kim, J. H. et al. Genomic predictors for recurrence patterns of hepatocellular carcinoma: model derivation and validation. PLoS Med 11, e1001770 (2014).
Chan, A. W. et al. Incorporating albumin-bilirubin grade into the cancer of the liver Italian program system for hepatocellular carcinoma. J. Gastroenterol. Hepatol. 32, 221–228 (2017).
Hiraoka, A. et al. Usefulness of albumin-bilirubin grade for evaluation of prognosis of 2584 Japanese patients with hepatocellular carcinoma. J. Gastroenterol. Hepatol. 31, 1031–1036 (2016).
Johnson, P. J. et al. Assessment of liver function in patients with hepatocellular carcinoma: a new evidence-based approach-the ALBI grade. J. Clin. Oncol. 33, 550–558 (2015).
Wang, Y. Y. et al. Albumin-bilirubin versus Child-Pugh score as a predictor of outcome after liver resection for hepatocellular carcinoma. Br. J. Surg. 103, 725–734 (2016).
Edmondson, H. A. & Steiner, P. E. Primary carcinoma of the liver: a study of 100 cases among 48,900 necropsies. Cancer 7, 462–503 (1954).
Imamura, H. et al. Risk factors contributing to early and late phase intrahepatic recurrence of hepatocellular carcinoma after hepatectomy. J. Hepatol. 38, 200–207 (2003).
Acknowledgements
This research was supported by a grant from Samsung Medical Center (GFO02160081), and a grant from the Marine Biotechnology Program (20150220) funded by the Ministry of Oceans and Fisheries, Korea.
Author information
Authors and Affiliations
Contributions
Conception and design: J.I. Yu, C. Choi, S.Y. Ha, H.C. Park, C.K. Park. Development of methodology: J.I. Yu, C. Choi, S.Y. Kang, S.Y. Ha, S. Kim, M. Kim, H.C. Park, C.K. Park. Acquisition of data: J.I. Yu, C. Choi, S.Y. Ha, H.C. Park, C.K. Park, J.W. Joh, S.W. Paik, S.H. Jung. Analysis and interpretation of data (e.g., statistical analysis, biostatistics, computational analysis): J.I. Yu, C. Choi, S. Kim, M. Kim. Writing, review, and/or revision of the manuscript: all authors.
Corresponding authors
Ethics declarations
Competing Interests
The authors declare that they have no competing interests.
Additional information
Publisher's note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Yu, J.I., Choi, C., Ha, S.Y. et al. Clinical importance of TERT overexpression in hepatocellular carcinoma treated with curative surgical resection in HBV endemic area. Sci Rep 7, 12258 (2017). https://doi.org/10.1038/s41598-017-12469-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-017-12469-2
This article is cited by
-
Genomic Landscape of HCC
Current Hepatology Reports (2020)
-
The role of telomeres and telomerase in cirrhosis and liver cancer
Nature Reviews Gastroenterology & Hepatology (2019)
-
Prognostic significance of miR-122 expression after curative resection in patients with hepatocellular carcinoma
Scientific Reports (2019)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.