Abstract
Epilepsy and spreading depolarization (SD) are both episodic brain disorders and often exist together in the same individual. In CA1 pyramidal neurons of mouse hippocampal slices, induction of SD evoked epileptiform activities, including the ictal-like bursts, which occurred during the repolarizing phase of SD, and the subsequent generation of paroxysmal depolarization shifts (PDSs), which are characterized by mild depolarization plateau with overriding spikes. The duration of the ictal-like activity was correlated with both the recovery time and the depolarization potential of SD, whereas the parameters of PDSs were not significantly correlated with the parameters of SD. Moreover, we systematically evaluated the effects of multiple anti-epileptic drugs (AEDs) on SD-induced epileptiform activity. Among the drugs that are known to inhibit voltage-gated sodium channels, carbamazepine, phenytoin, valproate, lamotrigine, and zonisamide reduced the frequency of PDSs and the overriding firing bursts in 20–25 min after the induction of SD. The GABA uptake inhibitor tiagabine exhibited moderate effects and partially limited the incidence of PDSs after SD. AEDs including gabapentin, levetiracetam, ethosuximide, felbamate, and vigabatrin, had no significant effect on SD-induced epileptic activity. Taken together, these results demonstrate the effects of AEDs on SD and the related epileptiform activity at the cellular level.
Similar content being viewed by others
Introduction
Spreading depolarization (SD, also called spreading depression) is a pathophysiological phenomenon that occurs under many neurological conditions, such as traumatic brain injury (TBI), aneurysmal subarachnoid hemorrhage (aSAH), intracerebral hemorrhage, and malignant cerebral infarction1,2. SD is characterized by profound depolarization of neurons and glia, which is accompanied by massive ion exchange across plasma membranes of the affected cells3,4. These electrical and ionic changes cause a disturbance in cell metabolism and might lead to cell death in metabolically compromised brain tissue5. Interestingly, SD is highly associated with the development of epilepsy in patients with aSAH6. In rodent and human brain slices, SD could trigger epileptiform responses that are characterized by ictal-like discharges on the tailing end of the extracellular potential shift of SD7,8. After the membrane potential recovers from the depolarization resulting from the SD, the neuronal activity transforms into epileptic discharge patterns that are characterized by paroxysmal depolarization shifts (PDSs)8.
PDSs are considered to be the manifestation of epileptic interictal spikes at the level of single neurons9. A PDS normally consists of a plateau-like depolarization associated with repetitive discharges of the neuron. The sustained depolarization is initiated by large excitatory postsynaptic potentials (EPSPs)10. The repetitive spikes are mediated by activation of voltage-gated Na+ channels (VGSCs). Activation of voltage-gated, high-threshold Ca2+ conductance and persistent Na+ conductance further contributes to the enhancement of depolarization. The repolarization phase of PDS is normally followed by hyperpolarization that involves a GABAA receptor-mediated Cl− conductance and Ca2+-dependent K+ conductance11. A better understanding of the pharmacological sensitivity of SD-induced PDSs will have implications for the treatment of neurological conditions and complications that are associated with SD.
Anti-epileptic drugs (AEDs) include more than twenty molecular entities that are marketed worldwide. AEDs are effective by different mechanisms of action, including modulation of voltage-gated Na+ channels (VGSCs) and/or voltage-gated Ca2+ channels (VGCCs), enhancement of inhibitory synaptic transmission, or inhibition of excitatory neurotransmission12,13. Activation of VGSCs is crucial for the generation of high-frequency repetitive discharges and PDSs, which are responsible for the generation of the ictal and interictal states of the seizure14. High-voltage activated VGCCs (L-, P/Q-, N- and R-types) are required for presynaptic neurotransmitter release and might modulate neuronal firing patterns, whereas activation of low voltage-activated VGCCs (T-type) are involved in neuronal bursting15. Moreover, some AEDs act at least partially by enhancing GABA transmission or inhibiting ionotropic glutamate receptors to modulate synaptic transmission16,17. Different types of AEDs are used for the treatment of different classifications of seizures. However, which type of AEDs are most effective in preventing epileptiform activity induced by SD remains unknown.
In the present study, we systematically evaluated the inhibitory effects of AEDs on SD-induced epileptic activity. The effects of a range of existing AEDs, including carbamazepine, phenytoin, valproate, lamotrigine, zonisamide, felbamate, gabapentin, levetiracetam, ethosuximide, tiagabine and vigabatrin, were tested on the PDSs following SD induction in hippocampal CA1 pyramidal neurons of mouse brain slices.
Results
SD induction of epileptiform activity
Whole-cell patch clamp recordings were performed in the CA1 pyramidal neurons in mouse hippocampal slices. Under control conditions with physiological levels of extracellular K+ and Mg2+, prolonged epileptiform activity is rarely observed after SD. Previous studies have shown that SD could evoke long-lasting epileptiform activity in partially disinhibited slices, that is, using 1.25 μM bicuculline to partially block GABAA receptors8. This model is, however, not applicable to our study, since AEDs including tiagabine and vigabatrin mainly target on the GABAergic transmission. The network excitability could also be increased by inhibition of certain types of voltage-gated potassium channels with tetraethylammonium (TEA) or Cs+. Considering that bath application of potassium blockers will influence the propagating properties of SD18, we tried intracellular application of Cs+ or TEA, which only modified the excitability of the recorded cell without affecting the propagation of SD or the excitability of the entire circuitry. Intracellular Cs+ increased the basal activities of neurons even without the induction of SD, causing a remarkable upshift of the resting membrane potential and massive spontaneous bursting; whereas intracellular TEA did not dramatically affecting the resting membrane potential or causing spontaneous epileptiform activity. Therefore, we tested whether SD could evoke epileptiform activity under a condition of 1.3 mM [Mg2+]o, 5.0 mM [K+]o and internal TEA. In the current-clamp mode (I = 0), the resting membrane potentials of CA1 neurons were scattered between −52 mV to −62 mV in the recorded cells. Spontaneous neuronal firings with typical waveforms of single action potentials could be observed (Fig. 1A1 ). SD was induced by focal KCl ejection from a glass pipette according to a well-established protocol19,20. The onset of SD was characterized by a profound depolarization of the membrane potential to −3.6 ± 1.0 mV with an averaged half-width duration of 35.8 ± 1.2 sec (n = 40) (Fig. 1A2 ). Such a depolarization phase represents a typical spreading depolarization as previously reported in human and animal models20,21. High frequency spikes at a frequency of 1~5 Hz first appeared during the late repolarization phase of SD8, which resembles the ictaform activity observed in spreading convulsions6. The ictal-like activity normally started in the late phase of repolarization with a mean duration of 79.2 ± 4.3 sec (n = 40). After the membrane potentials recovered to baseline, another form of epileptiform activity that was characterized by PDSs developed from a pattern of broadened action potentials (Fig. 1A3 ). PDSs were characterized by mild but prolonged depolarization with overriding burst of spikes (Fig. 1A4 ). The occurrence of PDSs normally lasted over 30 min from the onset of SD. In a recording period of 20–25 min after the induction of SD, PDSs occurred at a mean frequency of 2.75 ± 0.34 times/min with an overriding burst of 6.18 ± 1.00 action potentials (Fig. 1B,C). These data indicate that SD induces PDSs that reflect epileptiform activity at the single cell level.
SD induced epileptiform activity in CA1 pyramidal neurons in mouse hippocampal slices. (A) A representative trace showing that SD induced PDSs that were sustained for over 30 min in a hippocampal CA1 pyramidal neuron. The changes in the membrane potential over time in the dotted squares are expanded in (A1–A4). (A1) shows that spontaneous firing of action potentials could be recorded before the induction of SD. (A2) shows the induction of SD. The application of the high KCl solution from the ejection pipette is indicated by the arrow. The waveform of the SD is characterized by prolonged depolarization for tens of seconds and profound depolarization in the membrane potential. Ictal-like discharges normally appears during the repolarization phase of SD. (A3) shows that PDSs instead of action potentials starts to appear after the membrane potential recovered from the depolarization caused by SD. (A4) shows further broadening of PDSs and an increased number of spikes during each PDS. (B) Quantitative results showing the frequency of PDSs before and after the induction of SD. (C) Quantitative results showing the number of spikes during each PDS before and after the induction of SD.
Relationships among SD characteristics, SD-induced ictal-like activity, and PDSs
As a first step towards a better understanding of the associations between SD and the epileptiform activity, we measured the 50% (τ50) and 90% recovery time (τ90) of SD, considering that the ictal-like activity normally started in the late repolarization phase of SD. τ50 and τ90 were determined by the duration from the time of the peak depolarization potential to the time at which the membrane potential reaches the 50% and 90% of full recovery, respectively. τ90 was measured instead of the full recovery time because τ90 is easier and more reliable to be defined. Our results showed that SD recovered with a mean τ50 = 26.5 ± 1.1 sec and a mean 90 = 85.0 ± 5.4 sec (n = 40). The relationship between τ50/τ90 and other parameters of SD was assessed by two-tailed Pearson’s correlation analysis. The results show that τ50 is highly correlated with the half-width duration of SD (Fig. 2A); interestingly, however, τ90 has no significant correlation with the half-width duration (Fig. 2B). Furthermore, the peak depolarization potential was significantly correlated with τ90 but not τ50 (Fig. 2C,D). These data suggest that the time required for the near complete recovery was highly dependent upon the extent of membrane potential depolarization of the SD, whereas τ50 is not directly associated with the depolarization potential.
Correlation of parameters of SD. Each point represents a pair of parameters of SD from a recorded neuron (n = 40). (A and B) The half-width durations of SD are significantly correlated with the τ50 (A) but not the τ90 (B) of SD. (C and D) The peak depolarization potential is not correlated with τ50 (C) but is rather correlated with the τ90 (D) of SD. r2, R-squared from linear regression analysis; ρ, Pearson’s correlation coefficient; *P < 0.05; **P < 0.01.
Considering that the ictal-like activity unusually occurred during the late repolarization phase of SD, it would be interesting to examine its relationships to the SD depolarization potential and recovery time. The results showed that duration of the ictal-like activity was significantly correlated with τ50, τ90, and the peak depolarization potential of SD (n = 40, Fig. 3). These data suggest that higher extent of membrane depolarization likely facilitates a longer period of ictaform events following SD.
Correlation of ictaform duration and parameters of SD. Each point represents a pair of ictaform duration and a parameter of SD from a recorded neuron (n = 40). The durations of ictal-like activity are significantly correlated with the τ50 (A), τ90 (B) and the peak depolarization potential of SD (C). r2, R-squared from linear regression analysis; ρ, Pearson’s correlation coefficient; *P < 0.05; **P < 0.01.
Correlation analysis of the parameters of PDS showed that the number of PDSs and the number of spikes per PDS are significantly correlated (n = 40, Fig. 4A). However, the PDSs appeared to be independent from the ictal-like activity, since no significant correlation was found between the PDS parameters and the ictal duration (Fig. 4B,C). The PDS parameters did not exhibit any significant correlation with τ50, τ90, or the peak depolarization potential of SD, either (Fig. 4D–I). Taken together, these results indicate that the amplitude and recovery of SD have an influence on the following ictaform activity rather than the later-generated PDSs.
Correlation of PDS parameters, ictaform durations, and parameters of SD. The PDS parameter, the ictaform duration, and the SD parameter from a recorded neuron are graphed in all pairwise combinations (n = 40). (A) The number of PDSs (as the total PDSs calculated in the 20-25 min after SD induction) is significantly correlated with the spike numbers during each PDS. (B and C) Neither the number of PDSs (B) or the number of spikes (C) is significantly with the duration of ictal-like duration. (D and F) There is no significant correlation between the number of PDSs and the parameters of SD. (G and I) There is no significant correlation between the spike number per PDS and the parameters of SD. r2, R-squared from linear regression analysis; ρ, Pearson’s correlation coefficient; *P < 0.05; **P < 0.01.
Influence of AEDs on the electrophysiological properties of the SD waveform
Next, we tested the effects of a range of AEDs on SD parameters and SD-induced epileptiform activity. The tested AEDs include carbamazepine, phenytoin, valproate, lamotrigine, zonisamide, felbamate, gabapentin, levetiracetam, ethosuximide, tiagabine and vigabatrin. The concentration used for each compound was selected as medium to high doses according to previous in vitro studies (Table 1). We first examined whether the AEDs tested in our study have a direct modulatory effect on the electrophysiological parameters of SD. Table 2 summarizes τ50, τ90, and the peak depolarization potential after different AED treatments. Among the 11 tested AEDs, felbamate, tiagabine, and vigabatrin significantly increased τ50 of SD, suggesting that these drugs delay the early repolarization phase of SD (Table 2). However, when τ90 was measured, only felbamate and vigabatrin caused a significant increase. Treating with the other AEDs did not significantly change the τ90 of SD (Table 2). Moreover, phenytoin significantly suppressed the peak depolarization potential, whereas the other AEDs did not influence the extent of depolarization during SD (Table 2).
The anti-epileptic effects of older generation of AEDs that influence Na+ channels
The first generation of AEDs are widely used in clinic due to their well-documented pharmacokinetics profiles. Among these drugs, carbamazepine, phenytoin, and valproate are known to prevent epilepsy by inhibition of VGSC activity22,23,24,25. We first tested the effects of high concentrations of the three AEDs on SD-induced ictal duration and PDS parameters (Fig. 5). Our results show that 50 μM phenytoin significantly reduced the duration of ictaform discharges that occurred at the late repolarization phase of SD (28.7 ± 11.9 s, n = 6, p = <0.05 compared with control: 79.2 ± 4.3 s, n = 40), whereas carbamazepine (50 μM, 71.3 ± 18.7 s, n = 6, p = 0.97) or valproate (1 mM, 88.7 ± 10.3 s, n = 6, p = 0.83) did not show a significant effect. Next, we examined the effects of these AEDs on SD-induced PDSs. The three tested AEDs at high concentrations all potently inhibited the induction of PDSs after SD. There were no PDSs after treatment with carbamazepine (n = 6) or phenytoin (n = 6). Valproate strongly decreased frequency of PDSs (0.16 ± 0.07 times/min, n = 5, p < 0.001) and spike number per PDS (2.2 ± 1.0, n = 5, p = 0.13). Since high doses of carbamazepine and phenytoin showed a complete block on PDSs, we further tested if the lower concentrations of these AEDs were also effective. Our data showed that carbamazepine still completely blocked the generation of PDS after SD at a concentration of 5 μM, but failed to produce a significant effect at 1 μM (1.3 ± 0.8 PDS/min for the frequency of PDSs, p = 0.70; and 3.2 ± 1.0 for the number of spikes/PDS, p = 0.43; n = 5). Phenytoin at a lower concentration of 5 μM still significantly inhibited the generation of PDSs after SD (0.04 ± 0.04 times/min for the frequency of PDSs, p < 0.001; and 0.6 ± 0.6 for the number of spikes/PDS, p < 0.001; n = 5). Taken together, these results indicate that carbamazepine, phenytoin, and valproate are effective in suppressing the SD-induced epileptiform activity.
The effects of carbamazepine, phenytoin, and valproate on SD-induced epileptiform activity. (A) Representative traces showing the changes in the membrane potential after treatment with carbamazepine (50 μM), phenytoin (50 μM), or valproate (1 mM). (B) Quantitative results showing the effects of AEDs on the duration of ictal-like activity. (C) Quantitative results showing the frequency of PDSs after treatment with carbamazepine (1–50 μM), phenytoin (5-50 μM), or valproate (1 mM) than in control. (D) Quantitative results showing the number of spikes per PDS after treatment with carbamazepine (1–50 μM), phenytoin (5–50 μM), or valproate (1 mM) than in control. Significance differences were determined by a One-way ANOVA with the Games-Howell post hoc test and were defined as *P < 0.05; **P < 0.01; ***P < 0.001.
The anti-epileptic effects of newer generation of AEDs that possibly influence Na+ channels
The newer generation of AEDs has shown improved tolerability and safety. Among these drugs, lamotrigine, zonisamide, and felbamate have been reported to modulate VGSC-mediated neuronal responses26,27,28. Figure 6 summarizes the effects of these drugs on SD-induced epileptiform activity. Among the tested AEDs, only lamotrigine (60 μM; 25.1 ± 12.8 s, n = 5, p < 0.05) significantly inhibited the duration of SD-induced ictal-like discharges, whereas zonisamide (50 μM; 86.3 ± 13.0 s, n = 9, p = 0.95) or felbamate (100 μM; 115.7 ± 23.6 s, n = 8, p = 0.47) did not show a significant effect. Both lamotrigine and zonisamide significantly reduced the frequency of PDS generation after SD (0.12 ± 0.12, n = 5, p < 0.001 after treatment with lamotrigine; 0.04 ± 0.04, n = 9, p < 0.001 after treatment with zonisamide). The number of discharges during each PDS was also decreased after treatment with lamotrigine (0.8 ± 0.8, n = 5, p < 0.01) or zonisamide (0.4 ± 0.4, n = 9, p < 0.001). The treatment with 100 μM felbamate failed to influence the frequency of the PDSs (1.98 ± 0.80, n = 8, p = 0.81) or the spike numbers during the PDSs (4.01 ± 0.90, n = 8, p = 0.39). These data indicate that both lamotrigine and zonisamide effectively attenuated the SD-induced generation of PDSs, whereas felbamate had no significant effect.
The effects of lamotrigine, zonisamide, and felbamate on SD-induced epileptiform activity. (A) Representative traces showing the changes in the membrane potential after treatment with lamotrigine (60 μM) and zonisamide (50 μM) or felbamate (100 μM). (B) Quantitative results showing the effects of AEDs on the duration of ictal-like activity. (C) Quantitative results showing the frequency of PDSs after treatment with lamotrigine (60 μM) and zonisamide (50 μM), or felbamate (100 μM) compared to that of control. (D) Quantitative results showing the number of spikes per PDS after treatment with lamotrigine (60 μM) and zonisamide (50 μM) or felbamate (100 μM) compared to control. Significance differences were determined by a One-way ANOVA with the Games-Howell post hoc test and were defined as *P < 0.05; **P < 0.01; ***P < 0.001.
Effects of AEDs that affects VGCCs
Gabapentin, levetiracetam, and ethosuximide are AEDs that are thought to mainly inhibit VGCCs. Gabapentin and levetiracetam mainly target the high-voltage activated Ca2+ channels29,30, while ethosuximide is a specific drug for absent seizures that works by blocking T-type VGCCs in the thalamus31. The duration of ictaform discharges immediately following SD was not affected by gabapentin (50 μM; 78.3 ± 16.6 s, n = 5, p = 1.00), levetiracetam (100 μM; 62.2 ± 19.0 s, n = 5, p = 0.82), or ethosuximide (500 μM; 60.3 ± 18.1 s, n = 5, p = 0.75). The frequency of PDSs was 0.76 ± 0.62 time/min (n = 5, p = 0.10) after treatment with gabapentin, 5.24 ± 2.47 time/min (n = 5, p = 0.76) after levetiracetam, and 2.52 ± 0.94 time/min (n = 5, p = 0.99) after ethosuximide. The number of spikes per PDS was 3.92 ± 3.15 (n = 5, p = 0.90) after treatment with gabapentin, 5.13 ± 1.55 (n = 5, p = 0.94) after levetiracetam, and 6.22 ± 0.80 (n = 5, p = 1.00) after ethosuximide. Therefore, none of these AEDs induced a significant inhibition on either the ictaform activity or the PDSs after SD (Fig. 7). These data suggest that SD-induced epileptiform activity is not sensitive to AEDs that modulate Ca2+ currents.
The effects of gabapentin, levetiracetam, and ethosuximide on SD-induced epileptiform activity. (A) Representative traces showing the changes in the membrane potential after treatment with gabapentin (50 μM), levetiracetam (100 μM), and ethosuximide (500 μM). (B) Quantitative results showing the effects of AEDs on the duration of ictal-like activity. (C) Quantitative results showing the frequency of PDSs after treatment with gabapentin (50 μM), levetiracetam (100 μM), and ethosuximide (500 μM) compared to that of control. (D) Quantitative results showing the number of spikes per PDS after treatment with gabapentin (50 μM), levetiracetam (100 μM), and ethosuximide (500 μM) compared to that of control. Significance differences were determined by a One-way ANOVA with the Games-Howell post hoc test and were defined as *P < 0.05; **P < 0.01; ***P < 0.001.
Effects of AEDs that modulate GABAergic transmission
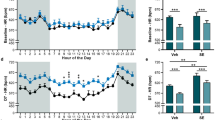
The anticonvulsant actions of tiagabine and vigabatrin are mainly through the potentiation of GABAergic signaling. Tiagabine potentiates GABA-mediated synaptic responses by inhibiting GABA uptake transporters32. Vigabatrin is a GABA analogue that irreversibly inhibits GABA transaminase and increases the extracellular GABA concentration and tonic inhibition33. Our results showed that the duration of ictaform activity was not affected by tiagabine (30 μM; 59.9 ± 19.6 s, n = 7, p = 0.63) or vigabatrin (200 μM, 64.5 ± 15.9 s, n = 6, p = 0.67). Tiagabine significantly reduced the number of PDSs (0.69 ± 0.50 time/min, n = 7, p < 0.05) and the spike number per PDS (1.98 ± 0.96, n = 7, p < 0.05). Vigabatrin produced a reducing trend on the frequency of PDSs (1.00 ± 0.62 time/min, n = 7); however, no statistical significant was reached for either PDS frequency (p = 0.08) or the number of spikes per PDS (3.80 ± 2.49, n = 7, p = 0.66) (Fig. 8). These results suggest that tiagabine rather than vigabatrin has an inhibitory effect on SD-induced PSDs.
The effects of tiagabine and vigabatrin on SD-induced epileptiform activity. (A) Representative traces showing the changes in the membrane potential after treatment with tiagabine (30 μM) and vigabatrin (200 μM). (B) Quantitative results showing the effects of AEDs on the duration of ictal-like activity. (C) Quantitative results showing the frequency of PDSs after treatment with tiagabine (30 μM) and vigabatrin (200 μM) compared to that of control. (D) Quantitative results showing the number spikes per PDS after treatment with tiagabine (30 μM) and vigabatrin (200 μM) compared to that of control. Significance differences were determined by a One-way ANOVA with the Games-Howell post hoc test and were defined as *P < 0.05; **P < 0.01; ***P < 0.001.
Discussion
SD and epilepsy are both episodic disorders caused by brain hyperexcitation or damage. They share many clinical features as well as some underlying mechanisms34 and could co-occur in the cerebral cortex7,35. In rat hippocampal slices, both SD and epilepsy could be induced by repetitive stimulation, especially under conditions of low extracellular Mg2+ concentrations36. In human slices, SD enhanced the repetition rate and amplitude of spontaneous seizure-like activity37. Instances of both SD and epilepsy implicated the role of ionotropic glutamate receptors. Moreover, the results from clinical studies suggest that the occurrence of seizures is highly associated with SD after acute brain injury38. The ictal epileptic field potentials in particularly could start at the end of the potential change of SD in aSAH patients6. Epilepsy is a well-recognized complication that occurs after acute brain injuries, especially including hemorrhagic stroke and TBI39,40. Many types of AEDs have been used as prophylaxis to prevent the onset of seizures and late seizures after brain injury conditions41. For example, phenytoin, carbamazepine and valproate are traditionally used as the primary choice of prophylactic drugs after aSAH; newer AEDs, such as levetiracetam, lamotrigine, gabapentin, and zonisamide, have also been used because of their better side effect profiles39. However, the effects of these AEDs are uncertain due to the lack of randomized and placebo controlled trials. The mechanisms of epileptogenesis after brain injury also remain largely unclear. Some studies have demonstrated that one contributing factor is the disruption of the blood-brain barrier after these conditions42. Functional changes in astrocytes could also enhance hyperexcitability and hyper-synchronization among neurons43. The alterations in the blood-brain barrier and glial cells could be further aggravated by epilepsy and SD44,45,46. Moreover, electrocorticography (ECoG) recordings showing that SD precedes ictal discharges in some aSAH patients suggest that SD could directly or indirectly increase the susceptibility to seizures under the condition of brain damage6. Effective attenuation of epileptiform activity after SD may help to reduce seizures in these patients.
In the present study, we showed that epileptiform activity could be induced by SD under a condition of increased neuronal excitability, since internal TEA could enhance EPSP, increase membrane input resistance, and produce a slight membrane depolarization47,48. Under these conditions, SD first induced a phase of ictaform events that occurred at the late repolarization phase. The duration of the ictaform discharges are significantly correlated with τ50, τ90, and the peak potentiation potential of SD, suggesting that a longer recovery time and a more depolarized state of SD favors the occurrence of ictal-like activity. In the present model, SD also induced a prolonged phase of interictal-like activity, which was shown as the PDSs. SD-induced PDSs have also been observed in previous studies, in which PDS persisted for ~1 h in rat neocortical and hippocampal slices under a condition of 1.25 µM bicuculline that leads to partial disinhibition. However, the mechanism for the generation of PDSs remains unknown. Our results showed that the parameters of PDSs, including the frequency and spike numbers per PDS, were not significantly correlated with the parameters of SD or the parameter of ictaform activity. It is possible that the SD-triggered strong ionic and metabolic responses disrupt the balance between neural excitation and inhibition. Under a condition of partial disinhibition, PDSs could be evoked when SD nudges this balance towards hyper-excitation.
Carbamazepine, phenytoin, lamotrigine, valproate, and zonisamide are potent VGSC inhibitors. These AEDs block high-frequency repetitive spike discharges without significantly affecting physiological action potentials12,49. In this study, carbamazepine, phenytoin, lamotrigine, valproate, and zonisamide reduced not only the number of overriding action potentials during the PDS but also the incidence of PDSs after SD. This could be due to multiple mechanisms of actions of these AEDs. First, VGSC-targeting AEDs, such as phenytoin and lamotrigine, produce a tonic inhibition on VGSCs by voltage-dependent and use-dependent manners22,50. They preferentially bind to the inactivated conformation of the channel and exhibited stronger inhibition when the depolarization state was prolonged and accumulated26,49. During the PDSs, the prolonged depolarization of the neuronal membrane causes repetitive discharges, which are sensitive to AED blockade11. Second, the binding and unbinding kinetics of these AEDs are slow51,52. In our experiments, the onset of SD is accompanied by a sustained depolarization of the membrane potential that reaches ~0 mV and lasts for tens of seconds. Such a condition already favors the binding of AEDs and therefore prevents the generation of PDSs. Third, some AEDs might also inhibit the persistent Na+ currents. Persistent Na+ currents contribute to the initiation and enhancement of PDSs when the PDS is induced by an EPSP11,53. Therefore, inhibition of persistent Na+ currents could reduce the extent of depolarization during the PDS. Together, these properties of VGSC-targeting AEDs might contribute to the suppression of both the incidence of PDSs and the overriding discharges induced by SD.
We also tested VGCC-targeting AEDs including gabapentin, levetiracetam, and ethosuximide, for their ability to affect epileptiform activity after SD. Blocking Ca2+ channels could inhibit the release of neurotransmitters and attenuate postsynaptic excitability54. Gabapentin and levetiracetam are thought to modulate high voltage-activated Ca2+ channels, whereas ethosuximide mainly inhibits T-type Ca2+ channels. However, the pharmacological mechanisms of these AEDs are complex. For example, levetiracetam is known to modulate N-type Ca2+ channels30, and it also binds to the synaptic vesicle protein SV2A to modulate neurotransmitter release and stabilizes GABAA receptors to facilitate inhibition55,56. In our study, gabapentin, levetiracetam, and ethosuximide did not show significant inhibition of the generation of PDSs, suggesting that SD-induced epileptiform activity was relatively insensitive to this type of AED. In a previous study, however, levetiracetam could reduce the duration and depolarization magnitude of PDSs induced by Mg2+-free solutions containing 4-aminopyridine and bicuculline57. This could largely result from the difference in the condition of the induction of epilepsy: in the study by Pisani et al., GABAergic transmission was blocked and NMDA receptors were potentiated. Such a condition could be more favorable to the generation of PDSs that are initiated by the largely enhanced excitatory synaptic transmission10. The increased synaptic release and the resulting PDSs therefore largely depend on activation of VGCCs and are sensitive to levetiracetam.
The GABAergic transmission is also involved the SD-induced epileptiform activity. The slices are more susceptible to generate epilepsy after SD when low concentrations of GABAA receptor antagonists were applied8. It has been reported that SD causes changes in receptor binding sites of both glutamate and GABA receptors and leads to an imbalance between excitatory and inhibitory inputs during the late phase58,59. The spontaneous and miniature inhibitory postsynaptic currents exhibited decreased frequency and increased amplitude after SD60. Therefore, the altered GABAergic transmission might contribute to epileptogenesis after SD. In this study, we show that the frequency of PDSs induced by SD was reduced by tiagabine. Tiagabine is a potent and selective inhibitor of the GABA uptake transporter GAT132, which is responsible for removing GABA from the synaptic cleft. Tiagabine can slow the reuptake of GABA from synapses and prolong the inhibitory postsynaptic potential. Our results suggest that enhancing GABA inhibition might attenuate SD-induced epileptiform activity.
In conclusion, our study reveals that AEDs that mainly target VGSCs, including carbamazepine, phenytoin, valproate, lamotrigine, and zonisamide, are potent inhibitors of SD-induced epileptiform activity. Tiagabine, which mainly modulates GABAergic transmission, also exhibits moderate inhibitory effects. AEDs that inhibit VGCCs, including gabapentin, levetiracetam, and ethosuximide, do not significantly affect the generation of PDSs after SD. These data will have implications for the therapy of epilepsy as a complication of SD-related neurological disorders.
Methods
Preparation of brain slices
All experimental procedures were in accordance with the Institutional Guidelines of China Medical University for the Care and Use of Experimental Animals (IGCMU-CUEA) and were approved by the Institutional Animal Care and Use Committee (IACUC) of China Medical University. Hippocampal slices were prepared from 12 to 21-day-old ICR mice of either sex. Mice were anaesthetized with urethane and decapitated. Brains were removed and placed in ice-cold artificial cerebrospinal fluid (ACSF) containing the following (in mM): 126 NaCl, 2.5 KCl, 2.0 MgCl2, 2.0 CaCl2, 1.25 NaH2PO4, 26 NaHCO3, and 10 D-glucose. Then, 350 μm-thick transverse hemi-sections from the hippocampus were sliced (Leica vibratome). The slices were incubated at room temperature for >1 h before recording. The slices were then transferred to the recording chamber with fresh ACSF containing the following (in mM): 125 NaCl, 5.0 KCl, 1.3 MgCl2, 2.0 CaCl2, 1.25 NaH2PO4, 26 NaHCO3, and 10 D-glucose. All solutions were saturated with 95% O2/5% CO2. In all pharmacological experiments, slices were pre-treated with chemicals for 20 min before SD induction unless specifically mentioned otherwise.
Whole-cell patch clamp recordings
Whole-cell patch clamp recordings were performed in CA1 pyramidal neurons using a MultiClamp 700B amplifier. The membrane potential was acquired under current-clamp mode without any holding current applied (I = 0 mode). Patch electrodes (3–7 MΩ) were pulled from 1.5-mm outer diameter thin-walled glass capillaries in three stages and were filled with intracellular solutions containing the following (in mM): 98 K-gluconate, 17 KCl, 10 HEPES, 1.1 EGTA, 0.1 CaCl2, 25 TEA-Cl, and 2 Na2-ATP, pH 7.25, osmolarity 290–300. Input resistance was obtained before and after each recording and recordings with a >25% change in input resistance were discarded. Signals were acquired via a Digidata 1440 A analog-to-digital interface and were low-pass filtered at 2 kHz and digitized at 10 kHz.
Induction and acquisition of SD and SD-associated epileptiform activity
Individual slices were transferred to a recording chamber (Fast Exchange Diamond Bath Chamber from Warner Instruments, Hamden, CT, USA) perfused with oxygenated ACSF at room temperature. SD was induced with a brief focal ejection of 2.5 M KCl from a glass pipette (resistance ~1–3 MΩ). The puffing pipette was placed close to the surface of the slice (z < 5 μm) in the CA3 stratum radiatum. Whole-cell recordings were made from CA1 pyramidal neurons at locations >200 μm from the KCl ejection site. One neuron was recorded in each slice, and a fresh slice was used for each new trial. The onset of SD was indicated by the well-established electrophysiological criteria for an SD: abruptly developing depolarization of neuronal membrane potential to nearly 0 mV61. Under a condition of 1.3 mM extracellular Mg2+, 5.0 mM extracellular K+ and intracellular TEA that helps to enhance excitability of the recorded neuron, intensive ictal-like activity occur in the repolarizing phase of SD. The peak depolarization potential was measured as the highest value of the absolute membrane potential reached during the SD. The half-width duration of the SD was measured at the half-maximum of the potential shifts. τ50 and τ90 were determined by measuring the time intervals from the peak depolarization potential to the point when membrane potential returns to 50% and 90% of resting membrane potentials, respectively. The duration of ictal-like activity was measured by the duration of continuous bursts (1~5 Hz) that occurred during the repolarization phase of SD. PDSs normally appeared after the ictal-like activity had stopped and were identified by a prolonged depolarization plateau with overriding repetitive discharges (>=3) with a frequency of >=5 Hz. Depolarization shifts with 2 spikes (and less) may represent the physiological firing pattern of “early-bursting pyramidal neurons” and thereby were not considered as PDSs62. The frequency of PDS was calculated as times/min. The spike number was calculated as the number of repetitive spikes during each PDS. If there was no PDS occurred, the frequency of PDS and the spike number/PDS were both considered 0. The frequency of PDS and spike number were analyzed as a mean value each min during the 20–25 min after the onset of SD in Figs 5–8.
Chemicals
Phenytoin, levetiracetam, ethosuximide, and tiagabine were obtained from Sigma-Aldrich (St. Louis, MO, USA). Carbamazepine, valproate, lamotrigine, zonisamide, felbamate, gabapentin, and vigabatrin were obtained from Tocris (Avonmouth, Bristol, UK).
Data analysis
Data in all figures are reported as the mean ± standard error of mean (s.e.m.). Statistical analysis was performed using the Statistical Product and Service Solutions (SPSS, IBM). One-way analysis of variance with the Games-Howell post hoc test or the two-tailed Dunnett-t post hoc test was used for statistical comparisons of multiple groups. Pearson’s correlation coefficient (ρ) was used for correlation analysis. Statistical significance was defined as *p < 0.05; **p < 0.01; ***P < 0.001.
References
Lauritzen, M. et al. Clinical relevance of cortical spreading depression in neurological disorders: migraine, malignant stroke, subarachnoid and intracranial hemorrhage, and traumatic brain injury. J Cereb Blood Flow Metab 31, 17–35 (2011).
Dreier, J. P. et al. Recording, analysis, and interpretation of spreading depolarizations in neurointensive care: Review and recommendations of the COSBID research group. J Cereb Blood Flow Metab 37, 1595–1625 (2017).
Somjen, G. G. Mechanisms of spreading depression and hypoxic spreading depression-like depolarization. Physiol Rev 81, 1065–1096 (2001).
Hartings, J. A. et al. The continuum of spreading depolarizations in acute cortical lesion development: Examining Leao’s legacy. J Cereb Blood Flow Metab (2016).
Dreier, J. P. The role of spreading depression, spreading depolarization and spreading ischemia in neurological disease. Nat Med 17, 439–447 (2011).
Dreier, J. P. et al. Spreading convulsions, spreading depolarization and epileptogenesis in human cerebral cortex. Brain 135, 259–275 (2012).
Van Harreveld, A. & Stamm, J. S. Spreading cortical convulsions and depressions. J Neurophysiol 16, 352–366 (1953).
Eickhoff, M. et al. Spreading depression triggers ictaform activity in partially disinhibited neuronal tissues. Exp Neurol 253, 1–15 (2014).
McCormick, D. A. & Contreras, D. On the cellular and network bases of epileptic seizures. Annu Rev Physiol 63, 815–846 (2001).
Johnston, D. & Brown, T. H. Giant synaptic potential hypothesis for epileptiform activity. Science 211, 294–297 (1981).
Timofeev, I., Grenier, F. & Steriade, M. Contribution of intrinsic neuronal factors in the generation of cortically driven electrographic seizures. J Neurophysiol 92, 1133–1143 (2004).
Rogawski, M. A. & Loscher, W. The neurobiology of antiepileptic drugs. Nat Rev Neurosci 5, 553–564 (2004).
Bialer, M. & White, H. S. Key factors in the discovery and development of new antiepileptic drugs. Nature reviews Drug discovery 9, 68–82 (2010).
Mantegazza, M., Curia, G., Biagini, G., Ragsdale, D. S. & Avoli, M. Voltage-gated sodium channels as therapeutic targets in epilepsy and other neurological disorders. Lancet Neurol 9, 413–424 (2010).
Zamponi, G. W., Lory, P. & Perez-Reyes, E. Role of voltage-gated calcium channels in epilepsy. Pflugers Arch 460, 395–403 (2010).
Avoli, M., Louvel, J., Pumain, R. & Kohling, R. Cellular and molecular mechanisms of epilepsy in the human brain. Prog Neurobiol 77, 166–200 (2005).
Braat, S. & Kooy, R. F. The GABAA Receptor as a Therapeutic Target for Neurodevelopmental Disorders. Neuron 86, 1119–1130 (2015).
Aitken, P. G., Jing, J., Young, J. & Somjen, G. G. Ion channel involvement in hypoxia-induced spreading depression in hippocampal slices. Brain Res 541, 7–11 (1991).
Ayata, C. Pearls and pitfalls in experimental models of spreading depression. Cephalalgia 33, 604–613 (2013).
Aiba, I. & Shuttleworth, C. W. Sustained NMDA receptor activation by spreading depolarizations can initiate excitotoxic injury in metabolically compromised neurons. J Physiol 590, 5877–5893 (2012).
Gorji, A. et al. Spreading depression in human neocortical slices. Brain Res 906, 74–83 (2001).
Ragsdale, D. S., Scheuer, T. & Catterall, W. A. Frequency and voltage-dependent inhibition of type IIA Na+ channels, expressed in a mammalian cell line, by local anesthetic, antiarrhythmic, and anticonvulsant drugs. Mol Pharmacol 40, 756–765 (1991).
Willow, M., Gonoi, T. & Catterall, W. A. Voltage clamp analysis of the inhibitory actions of diphenylhydantoin and carbamazepine on voltage-sensitive sodium channels in neuroblastoma cells. Mol Pharmacol 27, 549–558 (1985).
Van den Berg, R. J., Kok, P. & Voskuyl, R. A. Valproate and sodium currents in cultured hippocampal neurons. Exp Brain Res 93, 279–287 (1993).
Taverna, S., Mantegazza, M., Franceschetti, S. & Avanzini, G. Valproate selectively reduces the persistent fraction of Na+ current in neocortical neurons. Epilepsy Res 32, 304–308 (1998).
Xie, X. et al. Electrophysiological and pharmacological properties of the human brain type IIA Na+ channel expressed in a stable mammalian cell line. Pflugers Arch 441, 425–433 (2001).
Schauf, C. L. Zonisamide enhances slow sodium inactivation in Myxicola. Brain Res 413, 185–188 (1987).
Taglialatela, M., Ongini, E., Brown, A. M., Di Renzo, G. & Annunziato, L. Felbamate inhibits cloned voltage-dependent Na+ channels from human and rat brain. Eur J Pharmacol 316, 373–377 (1996).
Gee, N. S. et al. The novel anticonvulsant drug, gabapentin (Neurontin), binds to the alpha2delta subunit of a calcium channel. J Biol Chem 271, 5768–5776 (1996).
Lukyanetz, E. A., Shkryl, V. M. & Kostyuk, P. G. Selective blockade of N-type calcium channels by levetiracetam. Epilepsia 43, 9–18 (2002).
Coulter, D. A., Huguenard, J. R. & Prince, D. A. Characterization of ethosuximide reduction of low-threshold calcium current in thalamic neurons. Ann Neurol 25, 582–593 (1989).
Suzdak, P. D. & Jansen, J. A. A review of the preclinical pharmacology of tiagabine: a potent and selective anticonvulsant GABA uptake inhibitor. Epilepsia 36, 612–626 (1995).
De Biase, D., Barra, D., Bossa, F., Pucci, P. & John, R. A. Chemistry of the inactivation of 4-aminobutyrate aminotransferase by the antiepileptic drug vigabatrin. J Biol Chem 266, 20056–20061 (1991).
Rogawski, M. A. In Jasper’s Basic Mechanisms of the Epilepsies (eds J. L. Noebels et al.) (Oxford, 2012).
Koroleva, V. I. & Bures, J. Cortical penicillin focus as a generator of repetitive spike-triggered waves of spreading depression in rats. Exp Brain Res 51, 291–297 (1983).
Mody, I., Lambert, J. D. & Heinemann, U. Low extracellular magnesium induces epileptiform activity and spreading depression in rat hippocampal slices. J Neurophysiol 57, 869–888 (1987).
Gorji, A. & Speckmann, E. J. Spreading depression enhances the spontaneous epileptiform activity in human neocortical tissues. European Journal of Neuroscience 19, 3371–3374 (2004).
Fabricius, M. et al. Association of seizures with cortical spreading depression and peri-infarct depolarisations in the acutely injured human brain. Clin Neurophysiol 119, 1973–1984 (2008).
Gilmore, E., Choi, H. A., Hirsch, L. J. & Claassen, J. Seizures and CNS hemorrhage: spontaneous intracerebral and aneurysmal subarachnoid hemorrhage. Neurologist 16, 165–175 (2010).
Pitkanen, A. et al. Posttraumatic epilepsy - disease or comorbidity? Epilepsy Behav 38, 19–24 (2014).
Marigold, R., Gunther, A., Tiwari, D. & Kwan, J. Antiepileptic drugs for the primary and secondary prevention of seizures after subarachnoid haemorrhage. Cochrane Database Syst Rev 6, CD008710 (2013).
Shlosberg, D., Benifla, M., Kaufer, D. & Friedman, A. Blood-brain barrier breakdown as a therapeutic target in traumatic brain injury. Nat Rev Neurol 6, 393–403 (2010).
Robel, S. et al. Reactive astrogliosis causes the development of spontaneous seizures. J Neurosci 35, 3330–3345 (2015).
Lapilover, E. G. et al. Peri-infarct blood-brain barrier dysfunction facilitates induction of spreading depolarization associated with epileptiform discharges. Neurobiol Dis 48, 495–506 (2012).
Wetherington, J., Serrano, G. & Dingledine, R. Astrocytes in the epileptic brain. Neuron 58, 168–178 (2008).
Petito, C. K., Schaefer, J. A. & Plum, F. Ultrastructural characteristics of the brain and blood-brain barrier in experimental seizures. Brain Res 127, 251–267 (1977).
Nowak, L. M. & Macdonald, R. L. Substance P: ionic basis for depolarizing responses of mouse spinal cord neurons in cell culture. J Neurosci 2, 1119–1128 (1982).
Clements, J. D., Nelson, P. G. & Redman, S. J. Intracellular tetraethylammonium ions enhance group Ia excitatory post-synaptic potentials evoked in cat motoneurones. J Physiol 377, 267–282 (1986).
Xie, X., Lancaster, B., Peakman, T. & Garthwaite, J. Interaction of the antiepileptic drug lamotrigine with recombinant rat brain type IIA Na+ channels and with native Na+ channels in rat hippocampal neurones. Pflugers Arch 430, 437–446 (1995).
Matsuki, N., Quandt, F. N., Ten Eick, R. E. & Yeh, J. Z. Characterization of the block of sodium channels by phenytoin in mouse neuroblastoma cells. J Pharmacol Exp Ther 228, 523–530 (1984).
Kuo, C. C. & Bean, B. P. Slow binding of phenytoin to inactivated sodium channels in rat hippocampal neurons. Mol Pharmacol 46, 716–725 (1994).
Kuo, C. C. & Lu, L. Characterization of lamotrigine inhibition of Na+ channels in rat hippocampal neurones. Br J Pharmacol 121, 1231–1238 (1997).
Timofeev, I., Bazhenov, M., Sejnowski, T. & Steriade, M. Cortical hyperpolarization-activated depolarizing current takes part in the generation of focal paroxysmal activities. Proc Natl Acad Sci USA 99, 9533–9537 (2002).
Zamponi, G. W. Targeting voltage-gated calcium channels in neurological and psychiatric diseases. Nat Rev Drug Discov 15, 19–34 (2016).
Lynch, B. A. et al. The synaptic vesicle protein SV2A is the binding site for the antiepileptic drug levetiracetam. Proc Natl Acad Sci USA 101, 9861–9866 (2004).
Palma, E. et al. The antiepileptic drug levetiracetam stabilizes the human epileptic GABAA receptors upon repetitive activation. Epilepsia 48, 1842–1849 (2007).
Pisani, A. et al. Intracellular calcium increase in epileptiform activity: modulation by levetiracetam and lamotrigine. Epilepsia 45, 719–728 (2004).
Haghir, H., Kovac, S., Speckmann, E. J., Zilles, K. & Gorji, A. Patterns of neurotransmitter receptor distributions following cortical spreading depression. Neuroscience 163, 1340–1352 (2009).
Aiba, I. & Shuttleworth, C. W. Characterization of inhibitory GABA-A receptor activation during spreading depolarization in brain slice. PLoS One 9, e110849 (2014).
Sawant-Pokam, P. M., Suryavanshi, P., Mendez, J. M., Dudek, F. E. & Brennan, K. C. Mechanisms of Neuronal Silencing After Cortical Spreading Depression. Cereb Cortex 27, 1311–1325 (2017).
Collewijn, H. & Harreveld, A. V. Membrane potential of cerebral cortical cells during reading depression and asyxia. Exp Neurol 15, 425–436 (1966).
Graves, A. R. et al. Hippocampal pyramidal neurons comprise two distinct cell types that are countermodulated by metabotropic receptors. Neuron 76, 776–789 (2012).
Goldenberg, M. M. Overview of drugs used for epilepsy and seizures: etiology, diagnosis, and treatment. P T 35, 392–415 (2010).
Kito, M., Maehara, M. & Watanabe, K. Mechanisms of T-type calcium channel blockade by zonisamide. Seizure 5, 115–119 (1996).
Pisani, A. et al. Electrophysiological actions of felbamate on rat striatal neurones. Br J Pharmacol 116, 2053–2061 (1995).
Sutton, K. G., Martin, D. J., Pinnock, R. D., Lee, K. & Scott, R. H. Gabapentin inhibits high-threshold calcium channel currents in cultured rat dorsal root ganglion neurones. Br J Pharmacol 135, 257–265 (2002).
Niespodziany, I., Klitgaard, H. & Margineanu, D. G. Levetiracetam inhibits the high-voltage-activated Ca(2+) current in pyramidal neurones of rat hippocampal slices. Neurosci Lett 306, 5–8 (2001).
Gomora, J. C., Daud, A. N., Weiergraber, M. & Perez-Reyes, E. Block of cloned human T-type calcium channels by succinimide antiepileptic drugs. Mol Pharmacol 60, 1121–1132 (2001).
Thompson, S. M. & Gahwiler, B. H. Effects of the GABA uptake inhibitor tiagabine on inhibitory synaptic potentials in rat hippocampal slice cultures. J Neurophysiol 67, 1698–1701 (1992).
Errante, L. D., Williamson, A., Spencer, D. D. & Petroff, O. A. Gabapentin and vigabatrin increase GABA in the human neocortical slice. Epilepsy Res 49, 203–210 (2002).
Wu, Y., Wang, W. & Richerson, G. B. Vigabatrin induces tonic inhibition via GABA transporter reversal without increasing vesicular GABA release. J Neurophysiol 89, 2021–2034 (2003).
Acknowledgements
This study was supported by grants from the Ministry of Science and Technology (MOST 103-2320-B-039–033, MOST 104-2320-B-039-045-MY3, MOST 104-2320-B-039-048-MY3, MOST 106-2314-B-006-034, MOST 106-2320-B-006 -055, and MOST 105-2632-B-039-002), China Medical University Hospital (DMR-106-170) and I-Da Hospital (NCKUEDA 10405), and in part by the Taiwan Ministry of Health and Welfare Clinical Trial and Research Center (MOHW105-TDU-B-212-133019).
Author information
Authors and Affiliations
Contributions
S.-P.H., C.-W.H., D.C.W. and N.Z. designed the study and coordinated the project, C.-H.L., T.-C.C., and M.-L.S. carried out the experiments, C.-H.L., S.-P.H., T.-C.C. and M.-H.L. analyzed data, Y.-C.C. and I.-H.H. contributed to slice preparation, C.-W.H., D.C.W. and N.Z. wrote the manuscript with the input of remaining authors.
Corresponding authors
Ethics declarations
Competing Interests
The authors declare that they have no competing interests.
Additional information
Publisher's note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Lin, CH., Hsu, SP., Cheng, TC. et al. Effects of anti-epileptic drugs on spreading depolarization-induced epileptiform activity in mouse hippocampal slices. Sci Rep 7, 11884 (2017). https://doi.org/10.1038/s41598-017-12346-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-017-12346-y
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.