Abstract
The ratio of early diastolic trans-mitral flow velocity to tissue-Doppler mitral annular early diastolic velocity (E/e′), and left ventricular end-diastolic pressure(LVEDP) have been shown to be correlated at rest, provided that patients are not on positive inotropic drugs. Data concerning the latter correlation during exercise stress are conflicting. Therefore, we investigated if use of negative inotropic drugs (NID), impacts the accuracy of E/e′ as a surrogate for LVEDP during low-level exercise. An exercise(50 watts) during cardiac invasive hemodynamic monitoring and an exercise echocardiography were performed prospectively within 24 hours in 54 patients (81%male, 62 ± 9years) with preserved LV Ejection-Fraction. Before exercise, the patients had scattered LVEDP (13.8 ± 5.8 mmHg) and septal E/e′ (8.7 ± 2.7). Half of them were on NID, mainly betablockers(n = 26). The correlation between septal-E/e′ and LVEDP was low for examinations performed at rest (r = 0.35,p = 0.01) with no significant impact of NID. For measurements performed at 50 Watts, NID had a significant impact on the association between septal-E/e′50 watts and LVEDP50 watts (β = −0.28,p = 0.03). Correlation between septal-E/e′50 watts and LVEDP50 watts persisted in patients on NID (r = 0.61,p = 0.001) while it disappeared in the group of patients with no NID (r = 0.15,p = 0.47). NID use is an important confounding factor to take into consideration when assessing exercise LVFP using stress E/e′ in patients with preserved LVEF.
Similar content being viewed by others
Introduction
Cardiac catheterization has demonstrated its usefulness for the diagnosis of early stage of heart failure with preserved ejection fraction (HFpEF), which is characterized by exercise-induced abnormal left ventricular filling pressure (LVFP) despite normal resting values1, 2. However, the invasive nature of this exploration limits its dissemination and echocardiography has been proposed as an alternative method for LVFP monitoring3, 4. The ratio of early diastolic trans-mitral flow velocity to tissue-Doppler mitral annular early diastolic velocity (E/e′) is currently the most widely used Doppler ultrasound parameter to diagnose elevation of LVFP. Several studies have shown a good correlation between E/e′ and LVFP at rest, in patients with chronic heart failure, either with preserved or altered left ventricular ejection fraction (LVEF)5,6,7,8. However, recent data have challenged the validity of this parameter9, 10. In particular, the use of E/e′ during exercise is a matter of debate3, 11,12,13,14. Stress E/e′ has first been validated in a study of small sample size, in patients with heterogeneous LVEF almost all treated with beta-blockers3. However, conflicting results have been reported in other studies assessing E/e′ to evaluate exercise LVFP in various populations with preserved LVEF, including untreated healthy subjects11, 13, 15.
Pulsed-Doppler early diastolic transmitral peak flow velocity (E) is considered to be a composite parameter mainly depending on LVFP and LV relaxation16. Nagueh et al., suggested using the ratio of E to tissue-Doppler mitral annular early diastolic velocity, E/e′, as a surrogate for invasive LVFP. E was estimated to be corrected for the influence of LV relaxation by e′, which was considered a preload-independent index of LV relaxation17. Positive and negative inotropic drugs have been shown to modify LV relaxation18,19,20 and also affect e′ preload-independence in experimental conditions18. In a canine model, when LV relaxation was impaired by beta-blockers use (Tau constant > 65 msec), e′ was preload-independent. In contrast, when dobutamine was used, LV relaxation was enhanced (Tau constant < 50 msec) and e′ lost its preload-independence18. Confirming these non-clinical data, our group and others reported that positive inotropic agents severely impaired the correlation between E/e′ and invasive evaluation of LVFP in patients with decompensated end-stage systolic heart failure21, 22 while this correlation was good in the same type of patients treated by beta-blockers6. We therefore hypothesized that exercise, by releasing endogenous catecholamine23, also alters the correlation between E/e′ and LVFP during stress echocardiography unless patients are concomitantly treated with negative inotropic drugs (NID) such as beta-blockers. In order to test this hypothesis, the aim of this study was to assess the impact of NID use on accuracy of stress E/e′ as a surrogate for exercise LVFP using a direct invasive measurement as the reference method in patients at high risk of heart failure with preserved ejection fraction (HFpEF).
Results
Clinical and demographic characteristics
Among the 60 patients initially enrolled in the study, 6 patients had incomplete data during exercise (missing E/e′ for 2; missing hemodynamic data for 4); leaving 54 patients for final analysis. Patients were mainly male (81%) with a mean age of 62 ± 9 years. Sixty-one, 28 and 39% of patients had hypertension, diabetes or history of coronaropathy, respectively. Twenty-seven patients (50%) were treated by a NID, mainly a beta-blocker (n = 26), whose type and doses are detailed in Table 1. One patient received verapamil. Baseline clinical data did not significantly differ between patients with and without NID (Table 2). Previous history of coronaropathy tended to be more frequent in NID vs. no NID subgroups (52% vs 26%, p = 0.09). There was no difference between systolic arterial pressure measured during echocardiography and catheterization at rest (138 ± 19 vs. 140 ± 20 mmHg, ns; respectively), 25 watts (155 ± 21 vs. 161 ± 19 mmHg, ns; respectively) and 50 watts (169 ± 23 vs. 169 ± 24 mmHg, ns; respectively).
Echocardiography and catheterization results
Invasive hemodynamic monitoring data
An example of data acquisition is presented in Fig. 1. Detailed results are provided in Table 2. Our patients had scattered baseline LVEDP at rest (13.8 ± 5.8 mmHg), with 24% having LVEDP >16 mmHg at rest. LVEDP increased at 25 Watts (21.5 ± 7.5 mmHg) and 50 Watts (24 ± 8.1 mmHg), as compared to LVEDP at rest (p < 0.001). During exercise, 57% of all patients had an LVEDP ≥ 25 mmHg, without any influence of NID use (52% in patients without NID and 63% in NID patients, p = 0.58). A total of 41% experienced dyspnea at 50 watts, with no association with NID use (Table 2). LVEDP and heart rate were not significantly associated at any level of the hemodynamic evaluations in subgroups of patients with NID and without NID.
Echocardiography data
The median time between echocardiography and catheterization was 4 hours 49 minutes. There were no significant differences in baseline echocardiographic data according to NID use or not (Table 3). No patient had mitral regurgitation >grade 1. Main diastolic echocardiographic parameters at 25 and 50 watts in both groups are summarized in Table 3. E, lateral and septal e′, and their respective E/e′ values were not significantly different between NID users and non-users at any exercise level. The heart rate tended to be lower in patients with vs. without NID at rest (62.6 ± 11.1 vs. 66.4 ± 9.8bpm, p = 0.19), at 25 watts (82.6 ± 11.8 vs. 88.4 ± 10.5bpm, p = 0.06) and at 50 watts (93.1 ± 11.3 vs. 98.2 ± 12.3bpm, p = 0.12).
Impact of NID on the association between septal E/e′ and LVEDP
A multivariable regression analysis (ANCOVA, n = 54) was performed for determination of LVEDP at rest/25/50 watts as a function of septal E/e′ value, NID use or not, presence of known coronaropathy, heart rate, and indexed left ventricular mass. Septal E/e′ rather than lateral E/e′ was chosen since correlations between septal E/e′ and LVEDP were stronger at rest, 25 and 50 watts (Table 4) than those of lateral E/e′ (Table 4).
At rest, only septal E/e′at rest, was significantly (β = 0.36, p = 0.007) associated with LVEDP at rest without influence of NID. During exercise, at 25 and 50 watts, only septal E/e′at 25/50 Watts (β = 0.43, β = 0.34; respectively, p ≤ 0.01) and NID use or not (β = −0.26, β = −0.28, respectively, p < 0.05) were significantly (p ≤ 0.01) associated with LVEDP at 25/50 Watts. The other parameters tested were not significantly associated to LVEDP value at 25/50 Watts.
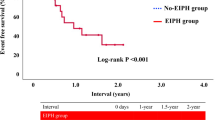
Interestingly, in subgroups analysis, correlation between septal E/e′ at 25 Watts and LVEDP at 25 Watts was slightly better in NID group (r = 0.5, n = 27, p < 0.01) compared to no NID group (r = 0.43, n = 27, p < 0.05). At 50 watts, differences in the correlation between septal E/e′ at 50 Watts and LVEDP at 50 Watts were further improved with good correlation in patients on NID (r = 0.61, n = 27, p < 0.05) while it disappeared (r = 0.15, n = 27, ns) in the no NID group (Fig. 2).
In the group of patients on NID (n = 27), ROC curves analysis for prediction of abnormal stress LVEDP (>16mmHg and ≥25mmHg) from septal E/e′ at 50 Watts showed an area under the curve of 0.8 (p = 0.09) and 0.72 (p ≤ 0.05), respectively. In the group of patients off NID (n = 27), ROC curves analysis for prediction of abnormal stress LVEDP (>16mmHg and ≥25mmHg) from septal E/e′ at 50 Watts were not significant (area under the curve: 0.67 and 0.61, p = ns, respectively).
Discussion
In this prospective study, we evaluated the impact of NID on the accuracy of Doppler echocardiography to assess LVFP in patients with preserved LVEF at risk of developing abnormal exercise LVFP increase at low workload levels as the reflection of early stage HFpEF. We found that NID use had no influence on the association of septal E/e′ with LVEDP at rest. During exercise, the correlation between septal E/e′ and LVEDP persisted only if patients were on NID. These results may explain the conflicting data about the validity of stress E/e′ for the assessment of exercise LVFP in patients with preserved LVEF. This finding may have a clinical significance particularly when considering that NID are frequently withdrawn in routine practice before a stress test.
Controversy about validity of echocardiography for evaluating LVFP during exercise
Several studies found that E/e′ was a better surrogate for LVFP at rest in patients with low LVEF on beta-blockers compared to patients with preserved LVEF5, 8, 24,25,26. Later, it was found that this correlation between E/e′ and LVFP was abolished by catecholamine use both in patients with and without cardiac systolic dysfunction21, 22, 27, 28. In recent years, concerns have been raised about the reliability of echocardiography for estimating LVFP during exercise. A small sample size study found a good correlation between LVEDP and E/e′ in patients with variable LVEF, mostly on beta-blockers3. This finding was also confirmed in another study in patients with advanced HFpEF mostly on betablockers14. In contrast, several recent studies reported the absence of association between LVEDP and E/e′ or their variations during exercise, in untreated patients with preserved LVEF11, 13. In our relatively large and well phenotyped cohort, we found that NID use influences the association between stress E/e′ and the direct invasive measure of LV diastolic pressure as the reference method. Thus, our results give new insight concerning previous discordant results. Moreover, our study emphasizes the importance of NID maintenance for stress echocardiography when performed for diagnosis of HFpEF. Recommendations concerning beta-blockers management before stress echocardiography are lacking in the recently updated guidelines for the evaluation of left ventricular diastolic function by echocardiography4.
Inotropic agents alter the e′ dependence to LVFP
It has been shown in animal models that positive inotropic drugs improve LV relaxation (shortening constant of relaxation Tau) and increase the dependency of e′ on load variations18,19,20. By contrast, e′ variation is little affected by filling pressure and has been validated as a preload-independent index of LV relaxation17 in cases of Tau lengthening, such as that associated with left ventricular systolic dysfunction29 or with NID use such as beta-blockers18. This may explain why use of E/e′ as a surrogate of LVFP has mostly been validated in patients with structural heart diseases, in particular LV systolic dysfunction on beta-blockers25, 26 and not in patients on positive inotropic drugs or during exercise. In fact, exercise is responsible of endogenous release of catecholamine, i.e. positive inotropes23. Therefore, our findings in humans confirm these preclinical findings in canine models where use of inotropes impaired the association between E/e′ and hemodynamic evaluation of LVFP, as opposed to beta-blockers, which improved it18,19,20.
Limitations
Heart catheterization and trans-thoracic echocardiography were not performed at exactly the same time and this may have contributed to decrease the magnitude of correlations between LVEDP and E/e′. However, good quality echocardiographic exams are difficult to obtain in catheterization laboratories and can lead to acquisitions of poor quality. Moreover, this methodological choice ensured that echocardiographic acquisitions and analyses of the data were made blindly of invasive measurements. The patients were investigated using exactly the same exercise protocol and without any modification of their drug treatments.
In patients treated with NID, treatment strategies were highly heterogeneous, with various doses and types of NID used, potentially leading to different effects on heart and vascular function. Too few patients were included in this study for additional multivariable analyses to be performed to assess any influence of type and dose of NID. Of note, in current clinical practice, strictly identical echocardiographic parameters are used for the estimation of LVFP in patients with different type and doses of NID or either without NID.
Since the non-invasive diagnosis of early stage HFpEF remains a major clinical challenge, we decided to focus our investigations on patients with preserved LVEF. The assessment of the influence of NID on stress E/e′ diagnostic accuracy in patients with altered LVEF deserves further investigations. In these latter patients, a focus on several comprehensive evaluations after careful beta-blocker dose up-titration is needed, seeking for dose-effect impact of NID on the relationship between E/e′ and LVFP.
Methods
Study
This study was ancillary to the PREFFORT study (NCT01714752)30. The study protocol and all methods applied were approved by the Committee for the Protection of Human Subjects of Pitié-Salpétière (Paris, France) and prior written informed consent was obtained from all subjects after being fully informed regarding the nature and risks of the study. We did the study in accordance with the principles of the international conference on harmonization guidelines on good clinical practice and the world medical association declaration of Helsinki.
Patient selection
The methods was previously described in details elsewhere30. Briefly, we prospectively enrolled 60 patients, among those admitted to the Pitié-Salpêtrière hospital in Paris, France, between 12/2012 and 07/2013, for clinically indicated left heart catheterization. Included patients had to undergo invasive and non-invasive assessments of LVFP within 24 hours, without change to their medications during that interval.
All included patients fulfilled the following criteria: (1) in sinus rhythm with LVEF >50%; (2) without any significant valve disease, hypertrophic cardiomyopathy, heart transplantation, atrial fibrillation, severe mitral annular calcification, LV thrombus, severe renal failure and (3) without any acute coronary syndrome in the previous 3 months or angiographic diagnosis of a stenosis requiring a percutaneous coronary intervention.
The risk factors of coronary artery disease, especially age, hypertension and diabetes, are also recognized as risk factors of HFpEF2. Thus, the patients referred for coronary angiography were also at high risk of developing abnormal exercise LVFP as the reflection of early stage HFpEF2.
Clinical data
On admission, demographic data (age, sex, previous coronaropathy, diabetes, hypertension, other comorbid conditions), baseline clinical data, type of NID (non-dihydropyridine calcium channel blockers, beta-blockers) and of other current treatments were collected prospectively. The type and dose of NID were left at the discretion of the treating physician.
Invasive hemodynamic assessment
After realization of the coronary angiography for diagnostic purpose, a fluid-filled pigtail catheter introduced through the radial artery was positioned in the mid-LV cavity using fluoroscopy, with the patient in the supine position. This catheter was connected to a strain-gauge pressure transducer positioned at right atrium level and zeroed before measurement. LV pressure tracings were recorded at baseline and during exercise. Measurements were made off-line, blindly from echocardiographic and clinical data by two experienced physicians. LVEDP measurement was averaged over five cardiac cycles. A hemodynamic LV end-diastolic pressure (LVEDP) ≤16 mmHg was defined as normal at rest. An increase of LVEDP >16 mmHg (moderate), and to a further extent ≥25 mmHg (important), was considered abnormal during stress1, 30, 31.
Echocardiographic assessment
Transthoracic echocardiography was performed using a Vivid 9 (GE Healthcare; Horten, Norway) by an experienced physician blinded to clinical and invasive data. Images were transferred to a workstation equipped with the Echopac PC software version 12.0 (GE Vingmed Ultrasound®; Horten, Norway). All examinations were analyzed off-line. All measurements were averaged over 3 to 6 cardiac cycles.
The following measurements were performed according to current guidelines32: LV internal diameter, inter-ventricular septal and posterior wall thicknesses at end diastole from M-mode. LV mass was derived. Left atrial maximal volume was measured in 2-dimensional mode at the end of ventricular systole just before opening of the mitral valve by biplane Simpson method from apical four and two-chamber views. LV volumes and LVEF were measured using the biplane Simpson method. When appropriate, preceding measures were indexed to body surface area. Trans-mitral E and A were determined by pulsed-Doppler echography. Using tissue-Doppler data, we acquired e′ in early diastole, in spectral mode, for both the basal septal and lateral segments, using the four-chamber apical view (Fig. 1). The calculated variables were lateral E/e′ and septal E/e′. Intra and inter-observer variabilities of E/e′ measurements at rest and during exercise were excellent (intra-class correlation coefficient ≥0.94 and ≥0.86, respectively)30.
Exercise Protocol
The same two-leg pedaling exercise was performed within 24 hours in catheterization laboratory using a cycle ergometer ERG 911 BP/XRAY (Schiller®, Switzerland) and then, in echocardiography laboratory using ERG 911 L/LS ergometer (Schiller®, Switzerland). Patients pedaled (50–60 cycles/minute) in the supine position, beginning at a workload of 25 Watts for 3 minutes, then at 50 Watts for another 3 minutes. Heart rate, blood pressure, invasive hemodynamic and non-invasive echocardiographic data were collected at baseline and during the last minute of each level of exercise, i.e. 25 and 50 Watts (Fig. 1). Continuous electrocardiographic monitoring was undertaken throughout the examination. The patient medications, including NID type and doses were unchanged between the invasive and non-invasive evaluations. Patients were asked at the end of the 50 Watts exercise if they had experienced dyspnea during the effort. Adequate mitral inflow, tissue Doppler signals and hemodynamic variables were obtained for all patients at baseline. E/e′ could not be measured accurately during exercise in two patients and hemodynamic data at exercise were missing in 4 patients, leaving 54 patients for final analysis.
Statistical analysis
For quantitative variables, mean and standard deviations (SD) were calculated. Discrete variables are presented as percentages. Continuous variables were compared with unpaired t tests for normally distributed variables. Fischer’s exact test was used for categorical variables. Statistical significance was defined as P < 0.05. All tests were two-tailed. Repeated measure two-ways ANOVA with Sidak post-test were performed to compare changes in LVEDP between rest, 25 and 50 Watts, as a function of NID use or not. The correlation between variables was assessed by calculating Pearson’s or Spearman’s coefficient (r), as appropriate. Multiple regression analysis (ANCOVA) was used to study association between LVEDP and E/e′, considering other covariates such as NID use (XLStat, Addinsoft®), at rest, 25 and 50 Watts. The choice of using septal or lateral E/e′ for these analyses was determined by the strength of their respective correlation with LVEDP. Receiver-operator characteristics (ROC) curves were plotted to determine diagnostic properties of E/e′ value to predict exercise LVEDP >16 mmHg and ≥25 mmHg, as a function of NID use (GraphPad 6 Software, San Diego, USA).
Conclusion
NID use is an important confounding factor to be taken into account when assessing exercise LVFP using stress E/e′ in patients with preserved LVEF.
References
Borlaug, B. A., Nishimura, R. A., Sorajja, P., Lam, C. S. & Redfield, M. M. Exercise hemodynamics enhance diagnosis of early heart failure with preserved ejection fraction. Circ Heart Fail 3, 588–595 (2010).
Borlaug, B. A. The pathophysiology of heart failure with preserved ejection fraction. Nat Rev Cardiol 11, 507–515 (2014).
Burgess, M. I., Jenkins, C., Sharman, J. E. & Marwick, T. H. Diastolic stress echocardiography: hemodynamic validation and clinical significance of estimation of ventricular filling pressure with exercise. J Am Coll Cardiol 47, 1891–1900 (2006).
Nagueh, S. F. et al. Recommendations for the Evaluation of Left Ventricular Diastolic Function by Echocardiography: An Update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. Eur Heart J Cardiovasc Imaging 17, 1321–1360 (2016).
Kasner, M. et al. Utility of Doppler echocardiography and tissue Doppler imaging in the estimation of diastolic function in heart failure with normal ejection fraction: a comparative Doppler-conductance catheterization study. Circulation 116, 637–647 (2007).
Nagueh, S. F. et al. Echocardiographic evaluation of hemodynamics in patients with decompensated systolic heart failure. Circ Cardiovasc Imaging 4, 220–227 (2011).
Nagueh, S. F. et al. Doppler Estimation of Left Ventricular Filling Pressure in Sinus Tachycardia: A New Application of Tissue Doppler Imaging. Circulation 98, 1644–1650 (1998).
Rivas-Gotz, C., Manolios, M., Thohan, V. & Nagueh, S. F. Impact of left ventricular ejection fraction on estimation of left ventricular filling pressures using tissue Doppler and flow propagation velocity. The American Journal of Cardiology 91, 780–784 (2003).
Marchandise, S. et al. Usefulness of tissue Doppler imaging to evaluate pulmonary capillary wedge pressure during exercise in patients with reduced left ventricular ejection fraction. Am J Cardiol 113, 2036–2044 (2014).
Santos, M. et al. E/e′ Ratio in Patients With Unexplained Dyspnea: Lack of Accuracy in Estimating Left Ventricular Filling Pressure. Circ Heart Fail 8, 749–756 (2015).
Bhella, P. S. et al. Echocardiographic indices do not reliably track changes in left-sided filling pressure in healthy subjects or patients with heart failure with preserved ejection fraction. Circ Cardiovasc Imaging 4, 482–489 (2011).
Hammoudi, N., Achkar, M. & Isnard, R. Exercise E/e′ for the assessment of left ventricular filling pressures: with caution in clinical practice? J Am Soc Echocardiogr 28, 376–377 (2015).
Maeder, M. T., Thompson, B. R., Brunner-La Rocca, H. P. & Kaye, D. M. Hemodynamic basis of exercise limitation in patients with heart failure and normal ejection fraction. J Am Coll Cardiol 56, 855–863 (2010).
Obokata, M. et al. Role of Diastolic Stress Testing in the Evaluation for Heart Failure With Preserved Ejection Fraction: A Simultaneous Invasive-Echocardiographic Study. Circulation 135, 825–838 (2017).
Talreja, D. R., Nishimura, R. A. & Oh, J. K. Estimation of left ventricular filling pressure with exercise by Doppler echocardiography in patients with normal systolic function: a simultaneous echocardiographic-cardiac catheterization study. J Am Soc Echocardiogr 20, 477–479 (2007).
Courtois, M., Mechem, C. J., Barzilai, B. & Ludbrook, P. A. Factors related to end-systolic volume are important determinants of peak early diastolic transmitral flow velocity. Circulation 85, 1132–1138 (1992).
Nagueh, S. F., Middleton, K. J., Kopelen, H. A., Zoghbi, W. A. & Quinones, M. A. Doppler tissue imaging: a noninvasive technique for evaluation of left ventricular relaxation and estimation of filling pressures. J Am Coll Cardiol 30, 1527–1533 (1997).
Firstenberg, M. S. et al. Determinants of diastolic myocardial tissue Doppler velocities: influences of relaxation and preload. J Appl Physiol (1985) 90, 299–307 (2001).
Hittinger, L. et al. Isoproterenol-induced alterations in myocardial blood flow, systolic and diastolic function in conscious dogs with heart failure. Circulation 80, 658–668 (1989).
Nagueh, S. F., Sun, H., Kopelen, H. A., Middleton, K. J. & Khoury, D. S. Hemodynamic determinants of the mitral annulus diastolic velocities by tissue Doppler. J Am Coll Cardiol 37, 278–285 (2001).
Mullens, W., Borowski, A. G., Curtin, R. J., Thomas, J. D. & Tang, W. H. Tissue Doppler imaging in the estimation of intracardiac filling pressure in decompensated patients with advanced systolic heart failure. Circulation 119, 62–70 (2009).
Salem, J. E. et al. Impact of inodilator drugs on echocardiographic assessments of left ventricular filling pressure in patients with decompensated end-stage heart failure*. Crit Care Med 42, 2508–2517 (2014).
Dimsdale, J. E. & Moss, J. Plasma catecholamines in stress and exercise. JAMA 243, 340–342 (1980).
Firstenberg, M. S. et al. Relationship of echocardiographic indices to pulmonary capillary wedge pressures in healthy volunteers. J Am Coll Cardiol 36, 1664–1669 (2000).
Kim, Y.-J. & Sohn, D.-W. Mitral annulus velocity in the estimation of left ventricular filling pressure: Prospective study in 200 patients. Journal of the American Society of Echocardiography 13, 980–985 (2000).
Ommen, S. R. et al. Clinical Utility of Doppler Echocardiography and Tissue Doppler Imaging in the Estimation of Left Ventricular Filling Pressures: A Comparative Simultaneous Doppler-Catheterization Study. Circulation 102, 1788–1794 (2000).
Chan, A. K. et al. Dobutamine stress echocardiography Doppler estimation of cardiac diastolic function: a simultaneous catheterization correlation study. Echocardiography 28, 442–447 (2011).
Egstrup, M. et al. Haemodynamic response during low-dose dobutamine infusion in patients with chronic systolic heart failure: comparison of echocardiographic and invasive measurements. Eur Heart J Cardiovasc Imaging 14, 659–667 (2013).
Popovic, Z. B. et al. Predictors of mitral annulus early diastolic velocity: impact of long-axis function, ventricular filling pattern, and relaxation. Eur J Echocardiogr 12, 818–825 (2011).
Hammoudi, N. et al. Low level exercise echocardiography helps diagnose early stage heart failure with preserved ejection fraction: a study of echocardiography versus catheterization. Clin Res Cardiol 106, 192–201 (2017).
Borlaug, B. A. Exercise haemodynamics and outcome in patients with dyspnoea. Eur Heart J 35, 3085–3087 (2014).
Lang, R. M. et al. Recommendations for cardiac chamber quantification by echocardiography in adults: an update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. Eur Heart J Cardiovasc Imaging 16, 233–270 (2015).
Acknowledgements
This project was supported by the French Federation of Cardiology and by the French Society of Cardiology.
Author information
Authors and Affiliations
Contributions
J.E.S. and N.H. had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis. J.E.S., N.H. and R.I. contributed to the conception and design of the study. F.L., A.C., A.M., O.B., G.H., C.L.F. and N.H. contributed to data collection. J.E.S., J.S.H., C.F.B., R.I. and N.H. contributed to analysis and/or interpretation of the data. J.E.S., C.F.B., and N.H. contributed to drafting the manuscript. All authors contributed to revision of the manuscript and accepted the submitted version.
Corresponding author
Ethics declarations
Competing Interests
FL was supported by a one-year research grant from the French Federation of Cardiology. The other authors have no conflict of interest to declare related to the present study.
Additional information
Publisher's note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Salem, JE., Laveau, F., Ceccaldi, A. et al. Impact of negative inotropic drugs on accuracy of diastolic stress echocardiography for evaluation of left ventricular filling pressure. Sci Rep 7, 9537 (2017). https://doi.org/10.1038/s41598-017-10301-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-017-10301-5
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.