Abstract
Distillers grains are co-products of the corn ethanol industry widely used in animal feed. We examined the effects of erythromycin, penicillin, and virginiamycin at low concentrations reflective of those detected in distillers grains on bacterial resistance selection. At 0.1 µg/ml erythromycin, macrolide-resistant mutants were induced in one Campylobacter coli and one Enterococcus faecium strain, while these strains plus three additional C. coli, one additional E. faecium, and one C. jejuni also developed resistance when exposed to 0.25 µg/ml erythromycin. At 0.5 µg/ml erythromycin, a total of eight strains (four Campylobacter and four Enterococcus) obtained macrolide-resistant mutants, including two strains from each genus that were not selected at lower erythromycin concentrations. For penicillin, three of five E. faecium strains but none of five Enterococcus faecalis strains consistently developed resistance at all three selection concentrations. Virginiamycin at two M1:S1 ratios did not induce resistance development in four out of five E. faecium strains; however, increased resistance was observed in the fifth one under 0.25 and 0.5 µg/ml virginiamycin selections. Although not yet tested in vivo, these findings suggest a potential risk of stimulating bacterial resistance development in the animal gut when distillers grains containing certain antibiotic residues are used in animal feed.
Similar content being viewed by others
Introduction
Distillers grains, co-products of the corn ethanol industry, are widely used animal feed ingredients owing to their abundance and nutritional content1. Over the past 15 years, the expansion of the U.S. domestic ethanol industry has led to an exponential growth in distillers grains feed production2. In 2016, an estimated 42 million metric tons were produced, which were fed, in up to 40% of the ration1, to beef cattle (44%), dairy cattle (30%), swine (16%), poultry (9%), and others (1%)2. Roughly 27% of the total production was exported2.
For at least two decades, antibiotics such as virginiamycin and penicillin have been used to control bacterial contamination of commercial ethanol fermentations1. The steady increase in distillers grains feed production raised growing concerns over this practice3. In two nationwide surveys conducted by the U.S. Food and Drug Administration’s Center for Veterinary Medicine (FDA/CVM), several antibiotics, including virginiamycin, erythromycin, penicillin, and tylosin, have been detected at low concentrations (0.1 to 1.5 ppm) in some of the distillers grains products analyzed4, 5. There is concern that through the feeding of distillers grains, food-producing animals are exposed to these antibiotic residues on a continuous basis, which may give rise to antibiotic-resistant bacteria that could be passed down the food chain3.
Antibiotic resistance is a growing public health threat worldwide6. In the United States, an estimated 2 million illnesses and 23,000 deaths are caused by antibiotic-resistant bacteria each year7. Urgent and multifaceted efforts are therefore needed to curb resistance development in both the human clinical setting and in food production8. Traditionally, selection of resistant mutants occurs at antibiotic concentrations between the minimal inhibitory concentration (MIC) of a susceptible wild-type bacterial population (MICsusc) and that of a resistant one (MICres), i.e., within the mutant selection window9, 10. The effect of lower concentrations of antibiotics such as those detected in distillers grains, at between one-tenth and one-half of the MICsusc or lower, on the selection and enrichment of antibiotic-resistant bacteria is not well understood.
To gain insights into whether low concentrations of erythromycin, penicillin, and virginiamycin may select for resistant bacteria, a preliminary study was carried out at FDA/CVM, subjecting a small number of Campylobacter (tested for erythromycin only) and Enterococcus strains to limited antibiotic selection concentrations and exposure times11. Campylobacter is a leading cause of foodborne illnesses in the United States, and frequently colonizes the intestinal tracts of poultry, swine, and other food-producing animals12. The opportunistic Enterococcus is also highly prevalent in the gut of food-producing animals as well as humans, and is a leading cause of nosocomial infections13. The preliminary study showed that penicillin at 1 µg/ml, virginiamycin at 0.1 and 1 µg/ml, a penicillin/virginiamycin blend at 1/0.075 µg/ml, and erythromycin at 0.1 µg/ml did not select for resistant Enterococcus phenotypes. However, erythromycin at both 0.25 and 0.5 µg/ml stimulated resistance development in Enterococcus. In Campylobacter, 0.5 µg/ml erythromycin (the only concentration tested) did not select for resistant mutants11. Considering the importance of these antibiotics in human and veterinary medicine, these findings support the need for further investigation into the microbiological impact of erythromycin and other residues detected in distillers grains14.
The present study aimed to comprehensively examine the effects of three low concentrations (0.1, 0.25, and 0.5 µg/ml) of erythromycin, penicillin, and virginiamycin (a mixture of two components, virginiamycin M1 and virginiamycin S1) on the development of antibiotic-resistant bacteria. Multiple Campylobacter (tested for erythromycin only) and Enterococcus strains were used as sentinel organisms for Gram-negative and Gram-positive bacteria, respectively.
Results
Resistance selection at low concentrations of erythromycin
The erythromycin MICs of twenty parent strains ranged from 0.25 to 1 µg/ml for Campylobacter and ≤0.25 to 1 µg/ml for Enterococcus (Table 1). In two independent trials, resistance development was stimulated in some strains of both bacterial genera during culture passages at all three erythromycin selection concentrations, with mutant MICs ranging from 64 to >2048 µg/ml for Campylobacter and 8 to >2048 µg/ml for Enterococcus (Table 2). At 0.1 µg/ml erythromycin, resistant mutants were observed in Campylobacter coli N20290 and Enterococcus faecium N39268 only. The same two strains, plus three additional C. coli, one additional E. faecium, and one C. jejuni strain also developed resistance when exposed to 0.25 µg/ml erythromycin. At 0.5 µg/ml erythromycin, eight strains (three C. coli, one C. jejuni, and two each E. faecalis and E. faecium) obtained resistant mutants, including two from each genus (one C. coli, one C. jejuni, and two E. faecalis) that were not selected at 0.1 and 0.25 µg/ml erythromycin. Notably, E. faecium N39268 mutants were selected at all three erythromycin concentrations, whereas no mutants were selected for three C. jejuni, three E. faecalis, two E. faecium, and the single E. hirae strain. All Campylobacter and E. faecalis mutations occurred at passages 2 or 3. Many mutants were generated outside the mutant selection window, i.e., at erythromycin concentrations lower than parent MICs, therefore with selection ratios (defined as the ratio between antibiotic selection concentration and parent strain MIC, i.e., MICsusc.) less than 1 (Table 2).
Regardless of the erythromycin concentration, selection ratio, and number of passages, Campylobacter strains overall had a higher incidence (70%) of resistance development than Enterococcus (40%) (P > 0.05). The selective effect was more pronounced among C. coli (100%) than C. jejuni (40%) (P < 0.05) and among E. faecium (50%) than E. faecalis (40%) (P > 0.05). Erythromycin at 0.25 and 0.5 µg/ml induced resistance in significantly larger percentages of Campylobacter and Enterococcus strains than those at 0.1 µg/ml (P < 0.05). Notably, resistant mutants of C. jejuni were only obtained at 0.25 and 0.5 µg/ml erythromycin, whereas E. faecalis mutants were only obtained at 0.5 µg/ml erythromycin (Table 3). The selection ratio also played a major role in the process with higher ratios generally associated with stronger selective effects. A selection ratio of 1/4 had the highest frequencies of mutated strains in both Campylobacter and Enterococcus (data not shown). Passages 2 and 3 were linked to stronger selection effect than passage 1, which was statistically significant in Campylobacter (P < 0.05) (data not shown).
Besides erythromycin, some mutants also demonstrated resistance to other macrolides, such as azithromycin in three C. coli strains and tylosin in E. faecalis strain N39462 (Table 3). Co-resistance to telithromycin (a ketolide) and/or clindamycin (a lincosamide) was common among Campylobacter mutants, whereas some E. faecium mutants also showed resistance to nitrofurantoin (a nitrofuran) and non-susceptibility to daptomycin (a lipopeptide) and/or tigecycline (a glycylcycline). Intermediate resistance (MICs above intermediate breakpoint but below resistant breakpoint) to these antibiotics (azithromycin, clindamycin, nitrofurantoin, and telithromycin) was observed as well (Table 3).
Resistance selection at low concentrations of penicillin
The penicillin MICs of ten Enterococcus parent strains ranged from 1 to 4 µg/ml for E. faecalis and ≤0.25 to 4 µg/ml for E. faecium (Table 1). In three independent trials, none of the five E. faecalis strains obtained penicillin-resistant mutants even after 15 passages, and neither did two out of five E. faecium strains. In direct contrast, E. faecium strains N39411, N39482, and N39577 consistently developed penicillin resistance at all three selection concentrations, with mutant MICs ≥ 16 µg/ml. Such difference in resistance selection between the two Enterococcus species was statistically significant (P < 0.05). Most mutants emerged between passages 7 and 10, and some as early as passage 1. Statistical analysis confirmed the link between higher numbers of passages and stronger resistance selection (P < 0.05). Similar to erythromycin, most penicillin mutants were generated outside the mutant selection window, i.e., at selection ratios less than 1 (Table 4). Interesting to note, the three E. faecium strains had parent MICs ranging from ≤0.25 to 1 µg/ml (selection ratios from 1/10 to ≥2) while the other two had parent MICs of 2 and 4 µg/ml (selection ratios from 1/40 to 1/4). This highlights the important role selection ratio played in the process with higher ratios generally associated with stronger selective effects (P < 0.05).
Besides penicillin, three E. faecium N39411 mutants also obtained resistance to erythromycin, to which the parent had an intermediate MIC (Table 5). Similarly, eight E. faecium N39577 mutants developed resistance to ciprofloxacin and/or erythromycin, to which the parent was intermediate. Non-susceptibility to daptomycin and/or tigecycline was observed in some E. faecium N39482 and N39577 mutants (Table 5). The MIC increases for the above mentioned antibiotics were 2–4 fold (data not shown).
Resistance selection at low concentrations of virginiamycin
The Q/D MICs of five E. faecium strains used for virginiamycin selection ranged from ≤0.5 to 4 µg/ml (Table 1). In two independent trials, four strains did not develop resistance when exposed to any of the three concentrations of virginiamycin at either M1:S1 ratio (0.5:1 or 5:1). The fifth one, E. faecium N42162, was initially resistant to virginiamycin with Q/D MIC of 4 µg/ml. At 0.5 µg/ml virginiamycin in both trials and 0.25 µg/ml in one trial, E. faecium N42162 mutants with higher Q/D MICs (8–16 µg/ml) were obtained at both M1:S1 ratios. All mutants emerged after passage 7 and were selected outside the mutant selection window (Table 6).
Besides higher Q/D MICs, some E. faecium N42162 mutants also obtained resistance to kanamycin, nitrofurantoin, and tylosin (Table 7), with MICs increasing by 4–8 fold compared to the parent strain (data not shown). It is noted that the parent strain had an intermediate MIC to nitrofurantoin.
Discussion
Much of the literature on antibiotic resistance focuses on tolerance/adaptation to high dosages that typically occur in a clinical setting. The effects of sub-MIC, sub-inhibitory, sub-lethal, or sub-therapeutic concentrations of antibiotics on the evolution of resistant bacteria are just beginning to be understood15,16,17,18,19. One study showed that after exposing 20 independent lineages of Escherichia coli K-12 MG1655 and Salmonella enterica Typhimurium LT2 constantly to 1/10 MIC of ciprofloxacin and 1/4 MIC of streptomycin, respectively, almost all lineages contained resistant subpopulations with MICs several folds higher than the parents17. Another study reported the de novo acquisition of resistance to amoxicillin, enrofloxacin, and tetracycline by E. coli K-12 MG1655 in the presence of sub-lethal antibiotic concentrations19. Nonetheless, most of the studies were carried out in model organisms in molecular biology, such as a single laboratory strain of E. coli. To our knowledge, this is the first study where multiple wild-type Campylobacter and/or Enterococcus strains were used to evaluate the development of resistance against three antibiotics at the concentrations detected in distillers grains.
Our data demonstrate that low concentrations (0.1, 0.25, and 0.5 µg/ml) of erythromycin, penicillin, and virginiamycin can select for resistant Campylobacter and Enterococcus variants, and the selective effects differed among strains, species, and genera. Such discrepancies can be partially explained by the different genetic backgrounds of the strains, resistance characteristics at genus and species levels, types of mutations conferring resistance, and fitness costs (defined as reduced competitiveness in the absence of antibiotics) associated with the mutations20. Historically, the reported frequency of macrolide resistance in C. coli derived from both humans and food animals is much higher than that in C. jejuni 21, 22. Not surprisingly, a significantly higher percentage of C. coli (100%) developed macrolide resistance than C. jejuni (40%) in the present study (P < 0.05). Furthermore, one C. coli strain obtained resistant mutants even at the lowest erythromycin concentration tested, whereas C. jejuni mutants were obtained at 0.25 and 0.5 µg/ml erythromycin only. Our data also suggest that E. faecium had a stronger tendency than E. faecalis to develop erythromycin resistance because E. faecium mutants were selected at all three erythromycin concentrations while E. faecalis only at 0.5 µg/ml. For penicillin, the finding that three E. faecium strains consistently developed resistance agrees with species-specific resistance characteristics: E. faecium is inherently more resistant to β-lactam antibiotics than E. faecalis and now widespread, high-level resistance to ampicillin has been observed among clinical E. faecium isolates23, 24. The differential selection of Q/D-resistant E. faecium mutants by virginiamycin was largely attributable to strain-specific resistance traits, highlighting the importance of using multiple strains in antibiotic selection experiments.
Under our experimental design (a closed system without introducing other strains), gene mutation, either pre-existing or de novo selected, was most likely the single most important route contributing to resistance development, whereas horizontal gene transfer was unlikely to have played a role. Many mutations/genes have been reported that account for resistance to the three antibiotics tested. Macrolide resistance in Campylobacter is mainly associated with point mutations in domain V of the 23 S rRNA and/or ribosomal proteins L4 and L22, active efflux, and rRNA methylation25, 26. In Enterococcus, modification of the 23 S rRNA target confers co-resistance to macrolides, lincosamides, and streptogramin B (quinupristin or virginiamycin S1), known as the MLSB phenotype23, 27. Drug inactivating enzymes and efflux also account for resistance to streptogramin antibiotics23, 27. Enterococcal resistance to β-lactams has been linked to mutations in the low-affinity penicillin binding protein pbp5 gene and/or genes coding for other species-specific proteins involved in cell wall synthesis such as L,D-transpeptidases (Ldt fm ), and β-lactamase27, 28. It is noteworthy that mutants generated in this study had MICs significantly higher (up to 8,192 fold above MICsusc) than the concentrations of antibiotics to which the parent strains were exposed (Tables 2 and 4). Genome-wide identification of resistance determinants among these mutants is currently under way. We anticipate detecting resistance mutations both specific to a particular drug and shared by multiple drugs, such as efflux pumps conferring resistance to multiple antibiotics, and may also include some potential new mechanisms20, 29, which may partly explain the co-resistance observed in some mutants.
One especially critical factor for resistance selection at sub-MIC concentrations of antibiotics is the variation in fitness cost incurred by different types of mutations15, 17, 30. Since susceptible bacteria are not killed at such low antibiotic concentrations but only grow slower, mutants will be competitive only when they carry fitness costs lower than the growth reduction in susceptible populations15, 17. A recent study reported fitness costs (measured by mutant growth rate reduction in comparison to the parent) of various resistance mutations in the range of 0.2 to 3% among E. coli and S. Typhimurium mutants selected by ciprofloxacin and streptomycin/tetracycline, respectively16, 30. Therefore, we expect resistant mutants obtained in the present study to carry variable degrees of low-fitness-cost mutations which accumulated and evolved over many generations through the selection process.
Aside from strain parameters, our data show that selective effects also differed by antibiotic selection concentrations and ratios, and number of passages (i.e., exposure time). The level of erythromycin, where no resistance selection occurred among 18 Campylobacter and Enterococcus strains was 0.1 µg/ml, which could be even lower for one C. coli and one E. faecium strain. The level of penicillin where no resistance selection occurred among most Enterococcus was greater than 0.5 µg/ml, while 0.1 µg/ml penicillin still selected for resistance in three E. faecium strains. For virginiamycin, the level where no resistance selection occurred was greater than 0.5 µg/ml for 4 E. faecium strains and 0.1 µg/ml for the fifth one. Taking into consideration the parent MICs (MICsusc.), it is apparent that the selection ratio is a more appropriate parameter in this context. A similar term “minimal selective concentration (MSC)” was coined recently in two pioneering studies as the lowest antibiotic concentration that selects for a given resistance mutation in competition experiments17, 18. In essence, MSC measures the antibiotic concentration needed to overcome the fitness cost of each resistance determinant, i.e., for the mutant strain to be competitive over the susceptible population, and is expressed as a fraction of the MICsusc. The smaller the fitness cost is, the lower the anticipated MSC15, 30. Using slightly different approaches, the two studies reported the MSCs in E. coli for two antibiotics (1/5 of the MICsusc. for ciprofloxacin and 1/20 of the MICsusc. for tetracycline)18 and in E. coli and S. Typhimurium for three antibiotics (1/230 to 1/10 of the MICsusc. for ciprofloxacin in E. coli and 1/4 and 1/100 of the MICsusc. for streptomycin and tetracycline, respectively, in S. Typhimurium)17. In the present study, the lowest selection ratios among those tested that still generated resistant mutants were 1/4 in Campylobacter and 1/10 in Enterococcus for erythromycin (Table 2), and 1/10 and 1/16 in E. faecium for penicillin (Table 4) and virginiamycin (Table 6), respectively. Nonetheless, an optimum selection ratio of 1/4 was noted in erythromycin experiments for both Campylobacter and Enterococcus and penicillin selection showed a strong preference for strains with lower MICsusc. (i.e., higher selection ratio). This suggests that resistance selection at sub-MIC concentrations of antibiotics favors antibiotic concentrations not too distant from the MICsusc., although further studies are warranted to confirm this hypothesis.
The development and dissemination of antibiotic resistance in bacterial pathogens is of significant public health concern globally6. Drug-resistant Campylobacter and vancomycin-resistant Enterococcus are among current resistance threats in the U.S.7. As outlined in FDA’s Guidance for Industry #209, the use of medically important antibiotics, including macrolides, β-lactams, and streptogramins, at sub-therapeutic levels in food animals poses a human health risk due to the potential for resistance development31. The concentrations of antibiotics tested in this study are reflective of those detected in distillers grains products in two nationwide surveys conducted by the FDA/CVM4, 5. Another survey reported the presence of similar low concentrations of antibiotics (erythromycin, mean 0.35 ppm; penicillin G, mean 0.11 ppm) in 12.6% of 159 distillers grain samples collected from 9 states and 43 ethanol plants in the U.S.32. Using various microbiological assays, several studies examined the antimicrobial effects of distillers grains and reported mixed findings32,33,34. In the survey mentioned above, one sample extract (out of 159) inhibited the growth of E. coli at 104 CFU/ml; however, this sample contained no detectable concentrations of antibiotic residues32. A 2015 short communication looking at only one source of commercial dried distillers grains with solubles observed no antimicrobial effect34. There are studies reporting the enzymatic degradation of penicillin and erythromycin and their poor stability in bioethanol fermentations1, 35; however, a very recent study demonstrated that biologically active virginiamycin at low concentrations (0.69 and 8.9 ppm) persisted in distillers grains produced from fermentations treated with virginiamycin33. Several other studies provided evidence that the use of antibiotics such as erythromycin, penicillin, and virginiamycin in ethanol production provides selective pressure for the development of resistant bacteria in the fermentators36,37,38. To our knowledge, there have been three in vivo studies to date evaluating the effect of feeding cattle distillers grains containing antibiotic residues on bacterial resistance development, and all reported minimal effects39,40,41. Notably, Enterococcus isolates from cattle fed monensin or monensin plus tylosin had greater levels of resistance toward macrolides and there was a tendency for a greater proportion of Q/D-resistant Enterococcus in cattle fed distillers grains39. Limitations noted include low statistical power and lack of baseline susceptibility data before feeding distillers grains39,40,41.
In conclusion, our in vitro study demonstrates that bacterial resistance evolution at sub-MIC concentrations of antibiotics involves a complex interplay between the specific drug, bacterial genetics, and culturing conditions42, 43. Further genome-wide identification of resistance determinants among mutants obtained in this study may shed some light on the dynamic mechanisms involved in the process. Although not yet tested in vivo, findings from this study suggest the potential risk of stimulating bacterial resistance development when distillers grains containing certain antibiotic residues are used in animal feed. Considering the mixed findings in the literature on this topic and the degradation of antibiotics following fermentation and distillation process, future in vivo studies are warranted in order to evaluate such effects in specific food-producing animal species fed commercially produced distillers grains.
Methods
Bacterial strains and growth conditions
Ten Campylobacter and fifteen Enterococcus strains were used as parent strains for mutant selection (Table 1). The strains were recovered from retail meats (ground beef, chicken breast, pork chop, and ground turkey) between 2006 and 2012 by the National Antimicrobial Resistance Monitoring System (NARMS)44. Among them, 10 strains from each genus representing five species (C. coli, C. jejuni, E. faecalis, E. faecium, and E. hirae) were tested against erythromycin, 10 strains of Enterococcus were tested against penicillin, and 5 strains of E. faecium were tested against virginiamycin (a mixture of two components, virginiamycin M1 and virginiamycin S1). Campylobacter was not tested against penicillin or virginiamycin because neither antibiotic is effective against Campylobacter 45. Only E. faecium strains were used in virginiamycin experiments due to the intrinsic resistance of E. faecalis to streptogramin antibiotics such as quinupristin/dalfopristin (Q/D) and virginiamycin46.
Campylobacter strains were cultured on blood agar prepared in-house using trypticase soy agar (BD Diagnostic Systems, Sparks, MD) supplemented with 5% horse blood (Remel Products, Lenexa, KS) or in Mueller-Hinton (MH) broth (BD Diagnostic Systems) at 42 °C under microaerophilic conditions (85% N2, 10% CO2, and 5% O2). When organisms were grown in MH broth, 25-cm2 tissue culture flasks with vented caps (Corning Inc., Corning, NY) were used. Enterococcus strains were grown on MH agar (BD Diagnostic Systems) or in broth at 37 °C.
Antibiotics and antibiotic-containing media preparation
Erythromycin, penicillin G potassium, and virginiamycin M1 and S1 were obtained from Sigma-Aldrich (St. Louis, MO). Virginiamycin complex (75% M1, 20% S1, and 5% other minor analogs) was procured from Santa Cruz Biotechnology, Inc. (Dallas, TX). Antibiotic stock solutions were prepared and stored following guidelines of the Clinical and Laboratory Standards Institute (CLSI)47, and aliquots were added to MH broth to obtain three low concentrations (0.1, 0.25, and 0.5 µg/ml) used for mutant selection. Virginiamycin M1 and S1 were mixed at two ratios (0.5:1 and 5:1) in broths. Aliquots were also added to agar plates (blood agar for Campylobacter and MH agar for Enterococcus) at or near clinical resistant breakpoint concentrations (see the section below) to screen for resistant mutants at each culture passage. The virginiamycin complex was used to make virginiamycin-containing MH agar plates.
Mutant selection experiments
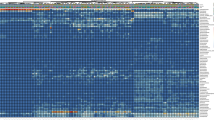
The procedure used in the FDA/CVM’s preliminary study11 was adopted with some modifications. All experiments were independently repeated twice (three times for penicillin). A schematic diagram for erythromycin selection experiments is shown (Fig. 1). Briefly, Campylobacter (tested for erythromycin only) and Enterococcus (for all three antibiotics) parent strains (Table 1) were cultured overnight in 5 ml of MH broth without antibiotics. Aliquots (100 µl) of the overnight cultures (ca. 109 CFU/ml) were transferred to fresh 5 ml of MH broth containing 0, 0.1, 0.25, or 0.5 µg/ml erythromycin, penicillin, or virginiamycin (at M1:S1 ratios of 0.5:1 and 5:1). After 24 h incubation (approximately 5–6 generations), 100 µl of the cultures were transferred again to fresh MH broth containing the same concentrations and ratios (in the case of virginiamycin) of antibiotics and incubated for 24 h. A total of 3 culture passages were performed for erythromycin, 10–15 for penicillin, and 10 for virginiamycin. For penicillin, strains that did not develop resistance after 10 passages were subject to an additional 5 passages. At each passage, excluding passages 5, 6, 12, and 13 which fell on weekends, the cultures were examined for resistance development by spreading 100-µl aliquots on agar plates (blood agar for Campylobacter and MH agar for Enterococcus) containing 8 and 16 µg/ml erythromycin, 16 and 32 µg/ml penicillin, or 4 µg/ml virginiamycin complex. Cultures were also plated on respective agar plates without antibiotics. Colonies were enumerated after 24-h incubation for Enterococcus and 48-h incubation for Campylobacter. Presumptive mutants (2 colonies per selective plate) were subcultured twice on blood agar and stored at −80 °C in brucella broth (BD Diagnostic Systems) containing 20% glycerol.
In vitro antimicrobial susceptibility testing
The minimal inhibitory concentration (MIC) for a panel of antimicrobial agents was determined for each parent and all presumptive mutants. The MICs were determined by broth microdilution using Sensititre NARMS Gram-positive (CMV3AGPF) and Campylobacter (CAMPY) MIC plates (TREK Diagnostic Systems, Oakwood Village, OH) for Enterococcus and Campylobacter, respectively44. Q/D was tested as a proxy for virginiamycin. Confirmed erythromycin-resistant mutants were further tested for erythromycin MICs using agar dilution because many had MIC values outside of the test ranges for erythromycin on the Sensititre MIC plates. Campylobacter jejuni ATCC 33560 and Enterococcus faecalis ATCC 29212 were used as quality control organisms. Susceptibility testing and data interpretation followed CLSI guidelines47, 48. Specifically, resistant breakpoints for erythromycin were ≥32 µg/ml and ≥8 µg/ml, respectively, for Campylobacter spp. and Enterococcus spp. For penicillin, a resistant breakpoint of ≥16 µg/ml was used and for quinupristin/dalfopristin, which was tested as a proxy for virginiamycin, a resistant breakpoint of ≥4 µg/ml was used.
Statistical analysis
Data on the frequencies of bacterial resistance development were sorted by antibiotic used for selection, bacterial genus, species, strain, antibiotic selection concentration, selection ratio (defined as the ratio between antibiotic selection concentration and parent strain MIC, i.e., MICsusc.), and number of passages. These data were compared using Chi-square and analysis of variance (ANOVA) (SAS for Windows, version 9.4; SAS Institute Inc., Cary, NC). Differences between the mean values were considered significant when P < 0.05.
Data availability statement
All data generated or analyzed during this study are included in this published article.
References
U.S. Grains Council. A guide to distiller’s dried grains with solubles (DDGS) – 3 rd Edition, http://www.grains.org/sites/default/files/ddgs-handbook/Complete%202012%20DDGS%20Handbook.pdf (2012).
Renewable Fuels Association. Building partnerships growing markets: 2017 ethanol industry outlook, http://www.ethanolrfa.org/wp-content/uploads/2017/02/Ethanol-Industry-Outlook-2017.pdf (2017).
Olmstead, J. Bugs in the system, https://www.iatp.org/sites/default/files/2012_05_02_AntibioticsInEthanol_JO_0.pdf (2012).
Luther, M. Report of FY 2008 nationwide survey of distillers products for antibiotic residues, http://www.fda.gov/AnimalVeterinary/Products/AnimalFoodFeeds/Contaminants/ucm331189.htm (2012).
Luther, M. Report of FY 2010 nationwide survey of distillers products for antibiotic residues, http://www.fda.gov/AnimalVeterinary/Products/AnimalFoodFeeds/Contaminants/ucm300126.htm (2012).
WHO. Antimicrobial resistance: global report on surveillance, 2014, http://apps.who.int/iris/bitstream/10665/112642/1/9789241564748_eng.pdf (2014).
CDC. Antibiotic resistance threats in the United States, 2013, https://www.cdc.gov/drugresistance/pdf/ar-threats-2013-508.pdf (2013).
The White House. National action plan for combating antibiotic-resistant bacteria, 2015, https://obamawhitehouse.archives.gov/sites/default/files/docs/national_action_plan_for_combating_antibotic-resistant_bacteria.pdf (2015).
Zhao, X. & Drlica, K. Restricting the selection of antibiotic-resistant mutant bacteria: measurement and potential use of the mutant selection window. J Infect Dis 185, 561–565, doi:10.1086/338571 (2002).
Drlica, K. & Zhao, X. Mutant selection window hypothesis updated. Clin Infect Dis 44, 681–688, doi: 10.1086/511642 (2007).
Blickenstaff, K. et al. In 34th Symposium on Biotechnology for Fuels and Chemicals (New Orleans, LA, 2012).
Scallan, E. et al. Foodborne illness acquired in the United States-major pathogens. Emerg Infect Dis 17, 7–15, doi:10.3201/eid1701.P11101(2011).
Lebreton, F., Willems, R. J. L. & Gilmore, M. S. Enterococcus diversity, origins in nature, and gut colonization. In Enterococci: From Commensals to Leading Causes of Drug Resistant Infection (eds M. S. Gilmore, D. B. Clewell, Y. Ike, & N. Shankar) (Massachusetts Eye and Ear Infirmary, Boston, MA, 2014).
FDA. Guidance for industry #152: Evaluating the safety of antimicrobial new animal drugs with regard to their microbiological effects on bacteria of human health concern, http://www.fda.gov/downloads/AnimalVeterinary/GuidanceComplianceEnforcement/GuidanceforIndustry/ucm052519.pdf (2003).
Andersson, D. I. & Hughes, D. Microbiological effects of sublethal levels of antibiotics. Nat Rev Microbiol 12, 465–478, doi:10.1038/nrmicro3270 (2014).
Gullberg, E., Albrecht, L. M., Karlsson, C., Sandegren, L. & Andersson, D. I. Selection of a multidrug resistance plasmid by sublethal levels of antibiotics and heavy metals. mBio 5, e01918–01914, doi:10.1128/mBio.01918-14 (2014).
Gullberg, E. et al. Selection of resistant bacteria at very low antibiotic concentrations. PLoS Pathog 7, e1002158, doi:10.1371/journal.ppat.1002158 (2011).
Liu, A. et al. Selective advantage of resistant strains at trace levels of antibiotics: a simple and ultrasensitive color test for detection of antibiotics and genotoxic agents. Antimicrob Agents Chemother 55, 1204–1210, doi:10.1128/AAC.01182-10 (2011).
van der Horst, M. A., Schuurmans, J. M., Smid, M. C., Koenders, B. B. & ter Kuile, B. H. De novo acquisition of resistance to three antibiotics by Escherichia coli. Microb Drug Resist 17, 141–147, doi:10.1089/mdr.2010.0101 (2011).
Andersson, D. I. & Hughes, D. Evolution of antibiotic resistance at non-lethal drug concentrations. Drug Resist Update 15, 162–172, doi:10.1016/j.drup.2012.03.005 (2012).
Belanger, A. E. & Shryock, T. R. Macrolide-resistant Campylobacter: the meat of the matter. J Antimicrob Chemother 60, 715–723, doi:10.1093/jac/dkm300 (2007).
FDA. 2014 NARMS Intregrated Report, https://www.fda.gov/AnimalVeterinary/SafetyHealth/AntimicrobialResistance/NationalAntimicrobialResistanceMonitoringSystem/ucm059103.htm (2016).
Kristich, C. J., Rice, L. B. & Arias, C. A. Enterococcal infection—treatment and antibiotic resistance. In Enterococci: From Commensals to Leading Causes of Drug Resistant Infection (eds M. S. Gilmore, D. B. Clewell, Y. Ike, & N. Shankar) (Massachusetts Eye and Ear Infirmary, Boston, MA, 2014).
Zhang, X. et al. Genome-wide identification of ampicillin resistance determinants in Enterococcus faecium. PLoS Genet 8, e1002804, doi:10.1371/journal.pgen.1002804 (2012).
Luangtongkum, T. et al. Antibiotic resistance in Campylobacter: emergence, transmission and persistence. Future Microbiol 4, 189–200, doi:10.2217/17460913.4.2.189 (2009).
Wang, Y. et al. Emergence of multidrug-resistant Campylobacter species isolates with a horizontally acquired rRNA methylase. Antimicrob Agents Chemother 58, 5405–5412, doi:10.1128/AAC.03039-14 (2014).
Miller, W. R., Munita, J. M. & Arias, C. A. Mechanisms of antibiotic resistance in enterococci. Expert Rev Anti Infect Ther 12, 1221–1236, doi:10.1586/14787210.2014.956092 (2014).
Novais, C. et al. Co-diversification of Enterococcus faecium core genomes and PBP5: evidences of pbp5 horizontal transfer. Front Microbiol 7, doi:10.3389/fmicb.2016.01581 (2016).
Toprak, E. et al. Evolutionary paths to antibiotic resistance under dynamically sustained drug selection. Nat Genet 44, 101–105, doi:10.1038/ng.1034 (2011).
Sandegren, L. Selection of antibiotic resistance at very low antibiotic concentrations. Ups J Med Sci 119, 103–107, doi:10.3109/03009734.2014.904457 (2014).
FDA. Guide for industry #209: The judicious use of medically important antimicrobial drugs in food-producing animals, https://www.fda.gov/downloads/AnimalVeterinary/GuidanceComplianceEnforcement/GuidanceforIndustry/UCM216936.pdf (2012).
Compart, D. M. et al. Presence and biological activity of antibiotics used in fuel ethanol and corn co-product production. J Anim Sci 91, 2395–2404, doi:10.2527/jas.2012-5714 (2013).
Bischoff, K. M., Zhang, Y. & Rich, J. O. Fate of virginiamycin through the fuel ethanol production process. World J Microbiol Biotechnol 32, 76, doi:10.1007/s11274-016-2026-3 (2016).
Sankarlal, V. M., Testroet, E. D., Beitz, D. C. & Clark, S. Short communication: No antimicrobial effects from one source of commercial dried distillers grains with solubles. J Dairy Sci 98, 8554–8559, doi:10.3168/jds.2015-9932 (2015).
Muthaiyan, A., Limayem, A. & Ricke, S. C. Antimicrobial strategies for limiting bacterial contaminants in fuel bioethanol fermentations. Prog Energ Combust 37, 351–370, doi:10.1016/j.pecs.2010.06.005 (2011).
Bischoff, K. M. & Skinner-Nemec, K. A. & Leathers, T. D. Antimicrobial susceptibility of Lactobacillus species isolated from commercial ethanol plants. J Ind Microbiol Biotechnol 34, 739–744, doi:10.1007/s10295-007-0250-4 (2007).
Murphree, C. A., Heist, E. P. & Moe, L. A. Antibiotic resistance among cultured bacterial isolates from bioethanol fermentation facilities across the United States. Curr Microbiol 69, 277–285, doi:10.1007/s00284-014-0583-y (2014).
Murphree, C. A., Li, Q., Heist, E. P. & Moe, L. A. A multiple antibiotic-resistant Enterobacter cloacae strain isolated from a bioethanol fermentation facility. Microbes Environ 29, 322–325, doi:10.1264/jsme2.ME13162 (2014).
Jacob, M. E. et al. Effects of feeding wet corn distillers grains with solubles with or without monensin and tylosin on the prevalence and antimicrobial susceptibilities of fecal foodborne pathogenic and commensal bacteria in feedlot cattle. J Anim Sci 86, 1182–1190, doi: 10.2527/jas.2007-0091 (2008).
Edrington, T. S., Bischoff, K. M., Loneragan, G. H. & Nisbet, D. J. Evaluation of feeding distiller’s grains, containing virginiamycin, on antimicrobial susceptibilities in fecal isolates of Enterococcus and Escherichia coli and prevalence of resistance genes in cattle. J Anim Sci 92, 1144–1149, doi:10.2527/jas.2013-6954 (2014).
Edrington, T. S. et al. Influence of wet distiller’s grains on prevalence of Escherichia coli O157:H7 and Salmonella in feedlot cattle and antimicrobial susceptibility of generic Escherichia coli isolates. Foodborne Pathog Dis 7, 605–608, doi:10.1089/fpd.2009.0417 (2010).
MacLean, R. C., Hall, A. R., Perron, G. G. & Buckling, A. The population genetics of antibiotic resistance: integrating molecular mechanisms and treatment contexts. Nat Rev Genet 11, 405–414, doi:10.1038/nrg2778 (2010).
Chait, R., Palmer, A. C., Yelin, I. & Kishony, R. Pervasive selection for and against antibiotic resistance in inhomogeneous multistress environments. Nat Commun 7, 10333, doi:10.1038/ncomms10333 (2016).
FDA/CDC/USDA. National Antimicrobial Resistance Monitoring System, http://www.fda.gov/AnimalVeterinary/SafetyHealth/AntimicrobialResistance/NationalAntimicrobialResistanceMonitoringSystem/default.htm (2017).
Lewis, J. S. & Bush, K. Antibacterial agents. In Manual of Clinical Microbiology, Eleventh Edition Vol. 1 (eds J. H. Jorgensen et al.) (ASM Press, Washington, DC, 2015).
Singh, K. V., Weinstock, G. M. & Murray, B. E. An Enterococcus faecalis ABC homologue (Lsa) is required for the resistance of this species to clindamycin and quinupristin-dalfopristin. Antimicrob Agents Chemother 46, 1845–1850, doi:10.1128/AAC.46.6.1845-1850.2002 (2002).
CLSI. Methods for Dilution Antimicrobial Susceptibility Tests for Bacteria That Grow Aerobically; Approved Standard-Eighth Edition (M7-A9). (Clinical and Laboratory Standards Institute, Wayne, PA, 2012).
CLSI. Performance Standards for Antimicrobial Susceptibility Testing; Twentieth Informational Supplement (M100-S22). (Clinical and Laboratory Standards Institute, Wayne, PA, 2012).
Acknowledgements
We thank Sherry L. Ayers and Jonathan L. Sabo for technical assistance. We are also grateful to Linda A. Benjamin, Maureen K. Davidson, Ron A. Miller, and Gregory H. Tyson for critical reading of the manuscript, and Steve Yan and Ruby Singh for stimulating discussions. The views expressed in this article are those of the authors and do not necessarily reflect the official policy of the Department of Health and Human Services, the U.S. Food and Drug Administration, or the U.S. Government. Reference to any commercial materials, equipment, or process does not in any way constitute approval, endorsement, or recommendation by the Food and Drug Administration.
Author information
Authors and Affiliations
Contributions
B.G., M.W.K., X.L., S.A.P., B.M.W., H.C.H., and J.M.G. conceived the experiments, B.G., K.J.D., Q.Y. developed the experimental set-up, K.J.D., Q.Y., S.R.Y., C.L.R., S.M.B., and S.A.G. conducted the experiments, B.G., K.J.D., Q.Y. analysed the results and wrote the manuscript, and all authors reviewed the manuscript.
Corresponding author
Ethics declarations
Competing Interests
The authors declare that they have no competing interests.
Additional information
Publisher's note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Ge, B., Domesle, K.J., Yang, Q. et al. Effects of low concentrations of erythromycin, penicillin, and virginiamycin on bacterial resistance development in vitro . Sci Rep 7, 11017 (2017). https://doi.org/10.1038/s41598-017-09593-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-017-09593-4
This article is cited by
-
Novel endolysin LysMP for control of Limosilactobacillus fermentum contamination in small-scale corn mash fermentation
Biotechnology for Biofuels and Bioproducts (2023)
-
Progress in the development of methods used for the abatement of microbial contaminants in ethanol fermentations: a review
Reviews in Environmental Science and Bio/Technology (2019)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.