Abstract
We investigated (1) the relationship between low-density lipoprotein cholesterol (LDL-C) and vascular function in patients receiving and those not receiving statin therapy and (2) optimal level of LDL-C for maintenance of vascular function. Flow-mediated vasodilation (FMD) and nitroglycerine-induced vasodilation (NID) were inversely correlated with LDL-C in the 957 statin naïve subjects but not in the 392 subjects receiving statin therapy. In statin naïve subjects, non-high LDL-C (≤100 mg/dL) was independently associated with a decrease in adjusted odds ratio of the low tertile of FMD (OR: 0.62, 95% CI: 0.45–0.85; P = 0.003) and NID (OR: 0.69, 95% CI: 0.50–0.96; P = 0.03). Adjusted odds ratio of the low tertile of FMD was significantly lower in the low LDL-C group (≤70 mg/dL) (OR: 0.47, 95% CI, 0.27–0.81; P = 0.006) and in the moderate LDL-C group (70.1–100 mg/dL) (OR: 0.66, 95% CI, 0.48–0.94; P = 0.02) than in the high LDL-C group (>100 mg/dL). There was no significant difference in FMD between the low LDL-C group and moderate LDL-C group. There were significant relationships of FMD and NID with LDL-C levels in statin naïve subjects. In a general population, LDL-C of ≤100 mg/dL may be the optimal target level for maintenance of endothelial function.
Similar content being viewed by others
Introduction
Current evidence indicates that dyslipidemia, including a high level of low-density lipoprotein cholesterol (LDL-C), is a strong predictor of cardiovascular disease1,2,3. Lowering LDL-C by statin therapy or non-statin therapy [e.g., ezetimibe and proprotein convertase subtilisin/kexin type 9 (PCSK9)] reduces major cardiovascular events4,5,6. Several clinical guidelines, but not all of the guidelines, emphasize the importance of achievement of a targeted level of LDL-C by statin therapy7,8,9,10,11. However, the optimal target levels of LDL-C to prevent cardiovascular diseases are different in the guidelines7,8,9,10,11.
Endothelial dysfunction is an initial step of atherosclerosis, leading to cardiovascular diseases12, 13. Measurement of flow-mediated vasodilation (FMD) of the brachial artery as an index of endothelium-dependent vasodilation is a useful method for assessing endothelial function and is an independent predictor of cardiovascular diseases14,15,16,17,18,19,20,21,22,23. Moreover, several lines of evidence suggest that interventions, including pharmacological therapy and life style modification, improve endothelial function24,25,26,27,28,29.
Nitroglycerine-induced vasodilation (NID), an index of endothelium-independent vasodilation, assessed by sublingual administration of a nitroglycerine tablet is usually measured as a control test for FMD measurement to differentiate endothelium-dependent vasodilation from endothelium-independent vasodilation since both endogenous nitric oxide (NO) and administered nitroglycerine act on vascular smooth muscle cells15, 30,31,32. We previously reported that NID as well as FMD significantly correlated with cardiovascular risk factors33. In addition, the combination of measurements of FMD and NID is useful for predicting future cardiovascular events34.
Although it is established that endothelial function assessed by FMD and NID significantly correlate with conventional cardiovascular risk factors, it remains controversial whether elevation of serum levels of LDL-C is independently associated with endothelial dysfunction21, 35, 36. Although the reason for the controversial relationship between LDL-C levels and vascular function is unclear, we hypothesized that the association of LDL-C levels with vascular function might disappear under the influence of cholesterol-lowering therapy, especially statin therapy. In addition, the cutoff level of LDL-C for vascular dysfunction is not determined.
The aims of this study were (1) to determine the association of LDL-C with vascular function in subjects receiving and those not receiving statin therapy, and (2) to determine the optimal cutoff level of LDL-C for maintenance of endothelial function.
Results
Baseline characteristics
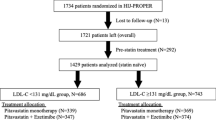
Baseline characteristics of all subjects are summarized in Table 1. Of the 1349 subjects, 787 (58.3%) were men and 562 (41.7%) were women, and 162 (12.0%) had coronary artery disease, 86 (6.4%) had stroke, and 392 (29.1%) were receiving statin therapy. We divided the subjects into 4 groups according to the statin use and level of LDL-C. Baseline characteristics of each group are shown in Table 1. In statin naïve subjects, there were significant differences between the non-high LDL-C (≤100 mg/dL) group and high LDL-C (>100 mg/dL) group in age, gender, body mass index, systolic blood pressure, diastolic blood pressure, total cholesterol, high-density lipoprotein cholesterol, hemoglobin A1c, and prevalence of hypertension and current smoking. FMD and NID were inversely correlated with age, body mass index, systolic blood pressure, diastolic blood pressure, glucose, hemoglobin A1c, and pack years of smoking (Supplementary Table 1). FMD, but not NID, was inversely correlated with total cholesterol and triglycerides.
Relationships between LDL-C and vascular function
There was no significant correlation of FMD or NID with LDL-C in all subjects (Figs 1 and 2). FMD and NID were inversely correlated with LDL-C in subjects not receiving statin therapy (r = -0.11, p = 0.001 and r = -0.09 p = 0.01, respectively) but not in subjects receiving statin therapy (Figs 1 and 2). In statin naïve subjects, there were significant differences in FMD and NID between the non-high LDL-C group and high LDL-C group (4.9 ± 3.3% vs. 3.9 ± 3.0%, p < 0.001 and 13.7 ± 5.6% vs. 12.5 ± 5.5%, p = 0.002, respectively) (Fig. 3). In subjects receiving statin therapy, FMD and NID were similar in the non-high LDL-C group and high LDL-C group (3.5 ± 2.7% vs. 3.7 ± 2.8%, p = 0.56 and 11.3 ± 5.8% vs. 11.1 ± 5.9%, p = 0.72, respectively). In multiple logistic regression analysis, non-high LDL-C in the subjects not receiving statin therapy was independently associated with a low FMD tertile (OR: 0.62, 95% CI: 0.45–0.85; P = 0.003) and a low NID tertile (OR: 0.69, 95% CI: 0.50–0.96; P = 0.03) (Table 2).
Optimal level of LDL-C for maintenance of vascular function
To determine the optimal level of LDL-C for maintenance of vascular function, we divided statin naïve subjects into three groups according to a more intensive cutoff level of LDL-C on the basis of levels recommended in current guidelines: low LDL-C group (≤70 mg/dL), moderate LDL-C group (70.1–100 mg/dL), and high LDL-C group (>100 mg/dL). Baseline clinical characteristics are summarized in Supplementary Table 2. There were significant differences in age, gender, body mass index, systolic blood pressure, diastolic blood pressure, total cholesterol, high-density lipoprotein cholesterol, low-density lipoprotein cholesterol, hemoglobin A1c and presences of hypertension, coronary artery disease and current smoking among the three groups (Supplementary Table 2). FMD was significantly lower in the high LDL-C group than in the moderate LDL-C group (3.9 ± 3.0% vs. 4.9 ± 3.5% p < 0.001) (Fig. 4). NID was significantly lower in the high LDL-C group than in the low LDL-C group (12.5 ± 5.5% vs. 14.7 ± 6.3% p = 0.003) (Fig. 4). There was no significant difference in FMD or NID between the low LDL-C group and moderate LDL-C group.
Using the high LDL-C group as a reference, low LDL-C (OR: 0.47, 95% CI, 0.27–0.81; P = 0.006) and moderate LDL-C (OR: 0.66, 95% CI, 0.48–0.94; P = 0.02) were independently associated with a decrease in the low FMD tertile in multiple logistic regression analysis (Table 3). Using the high LDL-C group as a reference, moderate LDL-C (OR: 0.67, 95% CI, 0.47–0.96; P = 0.03) was independently associated with a decrease in the low NID tertile after multiple logistic regression analysis (Table 3). Multiple logistic regression analysis revealed that there was no significant difference in the low tertile of FMD between low and moderate LDL-C levels and that there was no significant difference in the low tertile of NID between low and moderate LDL-C levels (Table 4).
Discussion
The present study demonstrated that (1) vascular function assessed by FMD and NID was significantly correlated with levels of LDL-C in subjects not receiving statin therapy but not in subjects receiving statin monotherapy and that (2) vascular function in statin naïve subjects was more greatly impaired in subjects with LDL-C of >100 mg/dL than in subjects with LDL-C of ≤100 mg/dL, while an additional benefit was not observed in subjects with LDL-C of ≤70.0 mg/dL compared with subjects with LDL-C of 70.1–100 mg/dL. In the present study, we confirmed, for the first time, a significant correlation between LDL-C and vascular function even in a general population not receiving lipid-lowering therapy.
Although LDL-C is known as a strong predictor of cardiovascular events, whether a high level of LDL-C is associated with vascular dysfunction was controversial in previous studies21, 35, 36. Those studies included subjects receiving lipid-lowering therapy. Therefore, LDL-C-lowering therapy might affect vascular function. Recently, several studies have shown that familial hypercholesterolemia on the basis of the level of LDL-C is underdiagnosed37. One possible reason is inferred that cholesterol-lowering therapy hinders accurate diagnosis of familial hypercholesterolemia. In the present study, the association of LDL-C with vascular function was different in subjects receiving and those not receiving statin therapy. The inverse relationship between LDL-C and vascular function may not be evident in subjects receiving statin therapy, suggesting that stain therapy protects against adverse vascular effects of LDL-C through anti-inflammatory effects or other mechanisms.
Endothelial dysfunction is an initial step of atherosclerosis, leading to cardiovascular diseases12, 13. Previous studies showed that LDL-C lowered by statin therapy, but not that lowered by non-statin therapy, improved endothelial function, suggesting that statin therapy-induced improvement of endothelial function is due to pleiotropic effects, not LDL-C-lowering effects per se38,39,40,41. In the present study, a low level of LDL-C was beneficial for endothelial function in statin naïve subjects who had no influence of a statin. To our knowledge, this is the first report showing a correlation between LDL-C and endothelial function in statin naïve patients. Interestingly, NID, as an index of vascular smooth muscle function, was also significantly correlated with LDL-C levels in statin naïve patients. These findings support evidence indicating that non-statin lipid-lowering therapy decreases cardiovascular events, although it is established that statin therapy is beneficial for the prevention of cardiovascular events42,43,44. An interaction of Rho-associated kinase (ROCK) activity and the endothelial NO synthase (eNOS)/NO pathway plays critical roles in vascular function45,46,47. An increase in ROCK activity and a decrease in NO bioavailability independently and cooperatively impair vascular function45,46,47. It is well known that a statin inhibits ROCK activity, upregulates eNOS expression, and increases eNOS bioactivity38, 39. Although we do not know the precise mechanisms underlying the association between LDL-C and vascular function, an increase in ROCK activity and inactivation of NO bioavailability may contribute to vascular dysfunction in subjects with high levels of LDL-C.
There is no consensus among international guidelines on the use of a “treat-to-target” strategy with specific LDL-C goals7,8,9,10,11. Moreover, there are differences in target levels of LDL-C between the guidelines7,8,9,10. In most guidelines, the target LDL-C level for secondary prevention of cardiovascular events is 100 mg/dL or less. Recently, The Improved Reduction of Outcomes: Vytorin Efficacy International Trial demonstrated that in patients with acute coronary syndromes, intensive targeting of LDL-C level of 53.7 mg/dL achieved by treatment with simvastatin in combination of ezetimibe reduced cardiovascular events compared to that with LDL-C level of 69.5 mg/dL achieved by simvastatin monotherapy, suggesting that lower LDL-C levels are better for prevention of cardiovascular events in these patients42. In the present study, in statin naïve subjects, FMD and NID were significantly lower in subjects with LDL-C of >100 mg/dL than in subjects with LDL-C of ≤100 mg/dL. A significant difference in FMD was not observed between subjects with LDL-C of 70 to 100 mg/dL and those with LDL-C of ≤70 mg/dL. Leibowitz et al.48. showed that no additional benefit is obtained by intensive cholesterol lowering to 70 mg/dL or less for secondary prevention in patients with coronary heart disease. Their findings are consistent with our results, indicating that a “treat-to-target” strategy and a target level of LDL-C of 100 md/dL are optimal for maintenance of vascular function. Recently, the Further Cardiovascular Outcomes Research with PCSK9 Inhibition in Subjects with Elevated Risk trial has shown that inhibition of PCSK9 in combination with statin therapy lowers LDL cholesterol level from 70 mg/dL to 30 mg/dL and reduces cardiovascular outcomes in patients with established cardiovascular disease49. These findings suggest that LDL cholesterol-lowering therapy that is more intensive than the current moderate-intensity LDL cholesterol-lowering therapy with a statin would be more effective for prevention of cardiovascular events. From the aspect of vascular function also, low levels of LDL cholesterol of 30 mg/dL or less may be beneficial for endothelial function. In the present study, few subjects had LDL cholesterol levels of 30 mg/dL or less. Future studies are needed to evaluate the effects of more intensive LDL cholesterol-lowering therapy on vascular function in a large population trial.
There were several limitations in the present study. First, the cross-sectional design did not allow us to establish a definitive causal relationship between LDL-C and vascular function. Future prospective and interventional studies are needed to establish more specific conclusions as to whether elevation of serum levels of LDL-C is associated with vascular dysfunction.
Second, in the present study, a significant correlation was not found between LDL-C and FMD in subjects receiving statin monotherapy, while a low level of LDL-C achieved by cholesterol-lowering therapy has been established to be essential for prevention of cardiovascular disease. In the subjects receiving statin monotherapy, the percentage of subjects who had a history of previous cardiovascular diseases progressively increased from the high LDL-C group to the low LDL-C group (Supplementary Table 2). Thus, we cannot rule out the possibility that there were differences in baseline characteristics among the groups. In addition, the intensity of the statin per se and dosages of statins were not considered. It is necessary to adjust baseline characteristics and the intensity, treatment period, and dosage of statins for assessment of vascular function in patients receiving statin therapy. Even after adjustment of these parameters, it would be difficult to assess vascular function under the condition of statin treatment.
In conclusion, LDL-C is an independent risk factor for vascular dysfunction in statin naïve individuals but not in individuals receiving statin monotherapy. In a general population not receiving lipid-lowering therapy, LDL-C of 100 mg/dL may be optimal as a cutoff level for maintenance of vascular function.
Methods
Subjects
A total of 1349 subjects were recruited from people who underwent a health check up at Hiroshima University Hospital between August 2007 and August 2016. Subjects were excluded if they were newly prescribed a statin or changed statin doses within 6 months. In order to focus on statin user and statin naïve patients, subjects were also excluded if they were receiving non-statin therapy: ezetimibe, PCSK9 inhibitor, bile acid sequestrants, fibrates, and niacin. Patients with hypertension were defined as those taking oral antihypertensive agents or with systolic blood pressure of more than 140 mm Hg or diastolic blood pressure of more than 90 mm Hg measured in a sitting position on at least 3 different occasions. Diabetes mellitus was defined according to the American Diabetes Association recommendation50. Dyslipidemia was defined according to the third report of the National Cholesterol Education Program51. Smokers were defined as those who were current smokers. One pack-year was equivalent to 20 cigarettes per day for 1 year. Coronary heart disease included angina pectoris, myocardial infarction, and unstable angina. Cerebrovascular disease included ischemic stroke, hemorrhagic stroke, and transient ischemic attack. Cardiovascular disease was defined as coronary heart disease and cerebrovascular disease. LDL-C concentration was calculated directly for subjects with triglycerides of >400 mg/dL. The Friedewald equation was used for other subjects.
In a primary analysis, we defined the target level of LDL-C as 100 mg/dL and divided the subjects into the two groups: a non-high group (LDL-C of ≤100 mg/dL) and a high group (LDL-C of >100 mg/dL). In a secondary analysis, the subjects were divided into the three groups to investigate whether an additional benefit is achieved in the lower level of LDL-C: a low group (LDL-C of ≤70 mg/dL), moderate group (LDL-C of 70.1–100 mg/dL), and high group (LDL-C of >100 mg/dL).
All methods were carried out in accordance with relevant guidelines and regulations. The Ethics Review Board of Hiroshima University approved the study protocol. Written informed consent for participation in the study was obtained from all of the subjects. All methods were performed in accordance with the relevant guidelines and regulations overseen by the Ethical Committee.
Study protocol
All subjects were assessed vascular function and structure using measurement of FMD and NID in brachial artery. The subjects fasted overnight for at least 12 hours and the study began at 08:30 hours, and remained supine in a quiet, dark, air-conditioned room (constant temperature of 22 °C to 25 °C) throughout the study. A 23-gauge polyethylene catheter was inserted into the left deep antecubital vein to obtain blood samples. At 30 minutes of maintaining a supine position, FMD and NID were measured. The observers were blind to the form of examination.
Measurements of FMD and NID
We evaluated the vascular response to reactive hyperemia in the brachial artery for assessment of endothelium-dependent FMD. A high resolution linear artery transducer was coupled to computer assisted analysis software (UNEX18 G, UNEX Co, Nagoya, Japan) that used an automated edge detection system for measurement of brachial artery diameter. A blood pressure cuff was placed around the forearm. The brachial artery was scanned longitudinally 5–10 cm above the elbow. When the clearest B-mode image of the anterior and posterior intimal interfaces between the lumen and vessel wall was obtained, the transducer was held at the same point throughout the scan by a special probe holder (UNEX Co) to ensure consistency of the image. Depth and gain settings were set to optimize the images of the arterial lumen wall interface. When the tracking gate was placed on the intima, the artery diameter was automatically tracked, and the waveform of diameter changes over the cardiac cycle was displayed in real time using the FMD mode of the tracking system. This allowed the ultrasound images to be optimized at the start of the scan and the transducer position to be adjusted immediately for optimal tracking performance throughout the scan. Pulsed Doppler flow was assessed at baseline and during peak hyperemic flow, which was confirmed to occur within 15 seconds after cuff deflation. Blood flow velocity was calculated from the Doppler data and was displayed as a waveform in real time. The baseline longitudinal image of the artery was acquired for 30 seconds, and then the blood pressure cuff was inflated to 50 mm Hg above systolic pressure for 5 minutes. The longitudinal images of the artery was recorded continuously until 5 minutes after cuff deflation. Pulsed Doppler velocity signals were obtained for 20 seconds at baseline and for 10 seconds immediately after cuff deflation. Changes in brachial artery diameter were immediately expressed as the percentage change relative to the vessel diameter before cuff inflation. FMD was automatically calculated as the percentage change in peak vessel diameter from the baseline value. Percentage of FMD [(Peak diameter–Base line diameter)/Baseline diameter] was used for analysis. Blood flow volume was calculated by multiplying the Doppler flow velocity (corrected for the angle) by the heart rate and vessel cross-sectional area (−r2). Reactive hyperemia was calculated as the maximum percentage increase in flow after cuff deflation compared with baseline flow.
The response to nitroglycerine was used for assessment of endothelium-independent vasodilation33. After acquiring baseline rest image for 30 seconds, a sublingual tablet (nitroglycerine 75 μg) was given and imaging of the artery was done continuously for 5 minutes. NID was automatically calculated as a percentage change in peak vessel diameter from the baseline. Percentage of NID [(Peak diameter–Baseline diameter)/Baseline diameter] was used for analysis. In our laboratory, the coefficient of variation for the baseline diameter was 2.9%.
Statistical analysis
Results are presented as means ± SD. All reported probability values were 2-sided, and a probability value of <0.05 was considered statistically significant. Categorical values were compared by means of the chi-square test. Continuous variables were compared by using ANOVA multiple groups. Comparisons between the groups categorized according to the serum LDL-C were carried out using repeated measures ANOVA with tukey’s post hoc test. Multiple logistic regression analysis was performed to identify independent variables associated with low tertiles of FMD (<2.7%) and NID (<10.6%). Age, sex, body mass index, and presences of current smoking, hypertension and diabetes mellitus were entered into the multiple logistic regression analysis. The data were processed using the software package Stata version 9 (Stata Co. College Station, Texas, USA).
Clinical Trial Registration Information
URL for Clinical Trial: http://UMIN; Registration Number for Clinical Trial: UMIN000003409.
References
Lloyd-Jones, D. M. et al. Lifetime risk of coronary heart disease by cholesterol levels at selected ages. Arch. Intern. Med. 163, 1966–1972, doi:10.1001/archinte.163.16.1966 (2003).
Yusuf, S. et al. Effect of potentially modifiable risk factors associated with myocardial infarction in 52 countries (the INTERHEART study): case-control study. Lancet 364, 937–952, doi:10.1016/s0140-6736(04)17018-9 (2004).
Nilsson, P. M., Nilsson, J. A. & Berglund, G. Population-attributable risk of coronary heart disease risk factors during long-term follow-up: the Malmo Preventive Project. J. Intern. Med. 260, 134–141, doi:10.1111/j.1365-2796.2006.01671.x (2006).
Baigent, C. et al. Efficacy and safety of cholesterol-lowering treatment: prospective meta-analysis of data from 90,056 participants in 14 randomised trials of statins. Lancet 366, 1267–1278, doi:10.1016/s0140-6736(05)67394-1 (2005).
LaRosa, J. C. et al. Intensive lipid lowering with atorvastatin in patients with stable coronary disease. N. Engl. J. Med. 352, 1425–1435, doi:10.1056/NEJMoa050461 (2005).
Silverman, M. G. et al. Association Between Lowering LDL-C and Cardiovascular Risk Reduction Among Different Therapeutic Interventions: A Systematic Review and Meta-analysis. JAMA 316, 1289–1297, doi:10.1001/jama.2016.13985 (2016).
Nayor, M. & Vasan, R. S. Recent Update to the US Cholesterol Treatment Guidelines: A Comparison With International Guidelines. Circulation 133, 1795–1806, doi:10.1161/circulationaha.116.021407 (2016).
Reiner, Z. et al. ESC/EAS Guidelines for the management of dyslipidaemias: the Task Force for the management of dyslipidaemias of the European Society of Cardiology (ESC) and the European Atherosclerosis Society (EAS). Eur. Heart J. 32, 1769–1818, doi:10.1093/eurheartj/ehr158 (2011).
Steg, P. G. et al. ESC Guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation. Eur. Heart J. 33, 2569–2619, doi:10.1093/eurheartj/ehs215 (2012).
Anderson, T. J. et al. 2012 update of the Canadian Cardiovascular Society guidelines for the diagnosis and treatment of dyslipidemia for the prevention of cardiovascular disease in the adult. Can. J. Cardiol. 29, 151–167, doi:10.1016/j.cjca.2012.11.032 (2013).
Stone, N. J. et al. 2013 ACC/AHA guideline on the treatment of blood cholesterol to reduce atherosclerotic cardiovascular risk in adults: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Circulation 129, S1–45, doi:10.1161/01.cir.0000437738.63853.7a (2014).
Ross, R. Atherosclerosis: an inflammatory disease. N. Engl. J. Med. 340, 115–126, doi:10.1056/nejm199901143400207 (1999).
Higashi, Y., Noma, K., Yoshizumi, M. & Kihara, Y. Endothelial function and oxidative stress in cardiovascular diseases. Circ. J. 73, 411–418 (2009).
Celermajer, D. S. et al. Non-invasive detection of endothelial dysfunction in children and adults at risk of atherosclerosis. Lancet 340, 1111–1115 (1992).
Corretti, M. C. et al. Guidelines for the ultrasound assessment of endothelial-dependent flow-mediated vasodilation of the brachial artery: a report of the International Brachial Artery Reactivity Task Force. J. Am. Coll. Cardiol. 39, 257–265 (2002).
Benjamin, E. J. et al. Clinical correlates and heritability of flow-mediated dilation in the community: the Framingham Heart Study. Circulation 109, 613–619, doi:10.1161/01.cir.0000112565.60887.1e (2004).
Donald, A. E. et al. Methodological approaches to optimize reproducibility and power in clinical studies of flow-mediated dilation. J. Am. Coll. Cardiol. 51, 1959–1964, doi:10.1016/j.jacc.2008.02.044 (2008).
Modena, M. G., Bonetti, L., Coppi, F., Bursi, F. & Rossi, R. Prognostic role of reversible endothelial dysfunction in hypertensive postmenopausal women. J. Am. Coll. Cardiol. 40, 505–510 (2002).
Schachinger, V., Britten, M. B. & Zeiher, A. M. Prognostic impact of coronary vasodilator dysfunction on adverse long-term outcome of coronary heart disease. Circulation 101, 1899–1906 (2000).
Neunteufl, T. et al. Late prognostic value of flow-mediated dilation in the brachial artery of patients with chest pain. Am. J. Cardiol. 86, 207–210 (2000).
Yeboah, J. et al. Predictive value of brachial flow-mediated dilation for incident cardiovascular events in a population-based study: the multi-ethnic study of atherosclerosis. Circulation 120, 502–509, doi:10.1161/circulationaha.109.864801 (2009).
Gokce, N. et al. Risk stratification for postoperative cardiovascular events via noninvasive assessment of endothelial function: a prospective study. Circulation 105, 1567–1572 (2002).
Suzuki, T. et al. Metabolic syndrome, endothelial dysfunction, and risk of cardiovascular events: the Northern Manhattan Study (NOMAS). Am. Heart J. 156, 405–410, doi:10.1016/j.ahj.2008.02.022 (2008).
Ghiadoni, L., Virdis, A., Magagna, A., Taddei, S. & Salvetti, A. Effect of the angiotensin II type 1 receptor blocker candesartan on endothelial function in patients with essential hypertension. Hypertension 35, 501–506 (2000).
Wolfrum, S., Jensen, K. S. & Liao, J. K. Endothelium-dependent effects of statins. Arterioscler. Thromb. Vasc. Biol. 23, 729–736, doi:10.1161/01.atv.0000063385.12476.a7 (2003).
Martens, F. M., Rabelink, T. J., op ‘t Roodt, J., de Koning, E. J. & Visseren, F. L. TNF-alpha induces endothelial dysfunction in diabetic adults, an effect reversible by the PPAR-gamma agonist pioglitazone. Eur. Heart J. 27, 1605–1609, doi:10.1093/eurheartj/ehl079 (2006).
Higashi, Y. et al. Effects of L-arginine infusion on renal hemodynamics in patients with mild essential hypertension. Hypertension 25, 898–902 (1995).
Sanada, M. et al. Relationship between the angiotensin-converting enzyme genotype and the forearm vasodilator response to estrogen replacement therapy in postmenopausal women. J. Am. Coll. Cardiol. 37, 1529–1535 (2001).
Goto, C. et al. Effect of different intensities of exercise on endothelium-dependent vasodilation in humans: role of endothelium-dependent nitric oxide and oxidative stress. Circulation 108, 530–535, doi:10.1161/01.cir.0000080893.55729.28 (2003).
Inoue, T. et al. Flow-mediated vasodilation as a diagnostic modality for vascular failure. Hypertens. Res. 31, 2105–2113, doi:10.1291/hypres.31.2105 (2008).
Adams, M. R. et al. Smooth muscle dysfunction occurs independently of impaired endothelium-dependent dilation in adults at risk of atherosclerosis. J. Am. Coll. Cardiol. 32, 123–127 (1998).
Raitakari, O. T., Seale, J. P. & Celermajer, D. S. Impaired vascular responses to nitroglycerin in subjects with coronary atherosclerosis. Am. J. Cardiol. 87, 217-219, a218 (2001).
Maruhashi, T. et al. Nitroglycerine-induced vasodilation for assessment of vascular function: a comparison with flow-mediated vasodilation. Arterioscler. Thromb. Vasc. Biol. 33, 1401–1408, doi:10.1161/atvbaha.112.300934 (2013).
Kajikawa, M. et al. Combination of Flow-Mediated Vasodilation and Nitroglycerine-Induced Vasodilation Is More Effective for Prediction of Cardiovascular Events. Hypertension 67, 1045–1052, doi:10.1161/hypertensionaha.115.06839 (2016).
Maruhashi, T. et al. Relationship between flow-mediated vasodilation and cardiovascular risk factors in a large community-based study. Heart 99, 1837–1842, doi:10.1136/heartjnl-2013-304739 (2013).
Kajikawa, M. et al. Relationship between serum triglyceride levels and endothelial function in a large community-based study. Atherosclerosis 249, 70–75, doi:10.1016/j.atherosclerosis.2016.03.035 (2016).
Nordestgaard, B. G. et al. Familial hypercholesterolaemia is underdiagnosed and undertreated in the general population: guidance for clinicians to prevent coronary heart disease: consensus statement of the European Atherosclerosis Society. Eur. Heart J. 34, 3478–3490a, doi:10.1093/eurheartj/eht273 (2013).
Laufs, U., La Fata, V., Plutzky, J. & Liao, J. K. Upregulation of endothelial nitric oxide synthase by HMG CoA reductase inhibitors. Circulation 97, 1129–1135 (1998).
Kureishi, Y. et al. The HMG-CoA reductase inhibitor simvastatin activates the protein kinase Akt and promotes angiogenesis in normocholesterolemic animals. Nat. Med 6, 1004–1010, doi:10.1038/79510 (2000).
Fichtlscherer, S. et al. Differential effects of short-term lipid lowering with ezetimibe and statins on endothelial function in patients with CAD: clinical evidence for ‘pleiotropic’ functions of statin therapy. Eur. Heart J. 27, 1182–1190, doi:10.1093/eurheartj/ehi881 (2006).
Liu, P. Y., Liu, Y. W., Lin, L. J., Chen, J. H. & Liao, J. K. Evidence for statin pleiotropy in humans: differential effects of statins and ezetimibe on rho-associated coiled-coil containing protein kinase activity, endothelial function, and inflammation. Circulation 119, 131–138, doi:10.1161/circulationaha.108.813311 (2009).
Cannon, C. P. et al. Ezetimibe Added to Statin Therapy after Acute Coronary Syndromes. N. Engl. J. Med. 372, 2387–2397, doi:10.1056/NEJMoa1410489 (2015).
Robinson, J. G. et al. Efficacy and safety of alirocumab in reducing lipids and cardiovascular events. N. Engl. J. Med. 372, 1489–1499, doi:10.1056/NEJMoa1501031 (2015).
Sabatine, M. S. et al. Efficacy and safety of evolocumab in reducing lipids and cardiovascular events. N. Engl. J. Med. 372, 1500–1509, doi:10.1056/NEJMoa1500858 (2015).
Soga, J. et al. Rho-associated kinase activity, endothelial function, and cardiovascular risk factors. Arterioscler. Thromb. Vasc. Biol. 31, 2353–2359, doi:10.1161/atvbaha.111.227892 (2011).
Wang, P., Ba, Z. F. & Chaudry, I. H. Administration of tumor necrosis factor-alpha in vivo depresses endothelium-dependent relaxation. Am. J. Physiol. 266, H2535–2541 (1994).
Venugopal, S. K., Devaraj, S., Yuhanna, I., Shaul, P. & Jialal, I. Demonstration that C-reactive protein decreases eNOS expression and bioactivity in human aortic endothelial cells. Circulation 106, 1439–1441 (2002).
Leibowitz, M. et al. Association Between Achieved Low-Density Lipoprotein Levels and Major Adverse Cardiac Events in Patients With Stable Ischemic Heart Disease Taking Statin Treatment. JAMA Intern Med 176, 1105–1113, doi:10.1001/jamainternmed.2016.2751 (2016).
Sabatine, M. S. et al. Evolocumab and Clinical Outcomes in Patients with Cardiovascular Disease. N. Engl. J. Med. 376, 1713–1722, doi:10.1056/NEJMoa1615664 (2017).
Diagnosis and classification of diabetes mellitus. Diabetes Care 37 Suppl 1, S81–90, doi:10.2337/dc14-S081 (2014).
Executive Summary of The Third Report of The National Cholesterol Education Program (NCEP). Expert Panel on Detection, Evaluation, And Treatment of High Blood Cholesterol In Adults (Adult Treatment Panel III). JAMA 285, 2486–2497 (2001).
Acknowledgements
We thank Miki Kumiji, Megumi Wakisaka, Ki-ichiro Kawano and Satoko Michiyama for their excellent secretarial assistance. This study was supported in part by a Grant-in-Aid for Scientific Research from the Ministry of Education, Science and Culture of Japan (18590815 and 21590898).
Author information
Authors and Affiliations
Contributions
S.M. and Y.H.: drafting the article and conception of this study; M.K., T.M., Y.I., A.I., N.O., S.K., T.H., C.G., Y.A., A.N., F.Y. and K.N. acquiring subjects and/or data; E.H., K.C. and Y.K., revising the article critically for important intellectual content. Y.H. is the guarantor of this work and, as such, had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Corresponding author
Ethics declarations
Competing Interests
The authors declare that they have no competing interests.
Additional information
Publisher's note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Matsui, S., Kajikawa, M., Hida, E. et al. Optimal Target Level of Low-density Lipoprotein Cholesterol for Vascular Function in Statin Naïve Individuals. Sci Rep 7, 8422 (2017). https://doi.org/10.1038/s41598-017-09043-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-017-09043-1
This article is cited by
-
Relationship between lipid parameters and vascular mechanical characteristics among a normotensive population without diabetes mellitus residing at the Qinghai–Tibet plateau: a cross-sectional study
BMC Cardiovascular Disorders (2022)
-
White blood cell count is not associated with flow-mediated vasodilation or nitroglycerine-induced vasodilation
Scientific Reports (2022)
-
Self-reported total sitting time on a non-working day is associated with blunted flow-mediated vasodilation and blunted nitroglycerine-induced vasodilation
Scientific Reports (2022)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.