Abstract
The determination of the chronic toxicity is time-consumed and costly, so it’s of great interest to predict the chronic toxicity based on acute data. Current methods include the acute to chronic ratios (ACRs) and the QSTR models, both of which have some usage limitations. In this paper, the acute and chronic mixture toxicity of three types of antibiotics, namely sulfonamides, sulfonamide potentiators and tetracyclines, were determined by a bioluminescence inhibition test. A novel QSTR model was developed for predicting the chronic mixture toxicity using the acute data and docking-based descriptors. This model revealed a complex relationship between the acute and chronic toxicity, i.e. a linear correlation between the acute and chronic lg(−lgEC50)s, rather than the simple EC50s or −lgEC50s. In particular, the interaction energies (Ebind) of the chemicals with luciferase and LitR in the bacterial quorum sensing systems were introduced to represent their acute and chronic actions, respectively, regardless of their defined toxic mechanisms. Therefore, the present QSTR model can apply to the chemicals with distinct toxic mechanisms, as well as those with undefined mechanism. This study provides a novel idea for the acute to chronic toxicity extrapolation, which may benefit the environmental risk assessment on the pollutants.
Similar content being viewed by others
Introduction
The chronic toxicity can better reflect the environmental risks of pollutants than the acute toxicity, since the organisms in the real environment are commonly subjected to long-term exposure of pollutants. However, it remains challenging to obtain the chronic toxicity directly through experimental methods, comparing to a flood of acute toxicity data that have been collected. This is because the chronic tests are usually characterized by long test cycle, complicated operation and high cost1. An effective solution to these problems is to extrapolate the chronic toxicity from the acute data that are easily obtained experimentally2, 3. Therefore, the underlying difference and connection between the chronic and acute toxicity should be investigated, which may provide easy and quick methods for acute to chronic toxicity extrapolation, and help establish chronic toxicity database for the environmental risk assessment.
At present, the acute to chronic toxicity ratios (ACRs) are commonly used for acute to chronic toxicity extrapolation. The ACR of a chemical is obtained as the ratio of the median lethal concentration (LC50) and the chronic maximum acceptable toxicant concentration (MATC)1,2,3. It is assumed that the ACR of a certain chemical is a constant for different species, which is calculated using the observed acute and chronic toxicity data with one species and then used to predict the chronic toxicity for another that is exposed to the same chemical4. This method is easy to perform and has been used in deriving US National Ambient Water Quality Criteria (NAWQC)5 as well as in risk assessments in many countries6. However, this method is problematic, for the ACR of a chemical may vary with many factors, such as the chemical modes of action (MOA), the model organisms and the experimental conditions3. Only when the MOA of a chemical is narcotic, can its ACR be a constant7, 8. Otherwise, the ACRs of the chemicals (i.e. the reactive compounds) can vary in a wide range (up to four orders of magnitude difference)2, 3, which makes it difficult to choose an appropriate ACR value for the chronic toxicity extrapolation and sometimes results in a under- or over-estimation of the chronic toxicity.
Quantitative structure-toxicity relationships (QSTR) severs as an important tool for the chronic toxicity prediction in risk assessment9. To date, a great many QSTR models have been reported for the chronic toxicity prediction, covering a variety of organisms and chemicals10,11,12,13. And various chemical properties have been introduced as the molecular descriptors for the QSTR models, such as logKow 8, 10, ELUMO 14, 15 and EHOMO 16, 17. In particular, the acute toxicity of chemicals was involved as one of the molecular descriptors in some QSTR models. For instance, Jiang et al.18 developed a chronic QSTR model that linked the 24 h toxicity [lg(1/EC50–24 h)] of antibiotics on luminescent bacteria to the 30 min toxicity [lg(1/EC50–30 min)] and other five descriptors. Likewise, in the report of Zou et al.19, the lg(1/EC50–24 h) of antibiotics on the luminescent bacteria can also be related to the lg(1/EC50–30 min). However, the QSTR model predictions also have some limitations, for instance, they can only apply to the chemicals with the similar structures or the same action mechanisms20. Moreover, few of the researches consider the chronic effects at the population level from the chemical ecology perspective, e.g. the potential effects of the chemicals on the bacterial quorum sensing (QS) systems.
QS is a cell-cell communication by which bacteria coordinate the expression of certain genes using small signal molecules (autoinducers, AIs)21. During their normal physiological process, the bacteria secrete AIs into the surrounding environment, which accumulate to a threshold concentration and then re-enter the bacterial cells, regulating gene expression and a series of bacterial behaviors, such as the biofilm formation22 and luminescence23. The acute toxicity test with the luminescent bacteria usually takes only 15 to 30 min, while the chronic toxicity test takes 24 hours or even longer. Therefore, during the acute test, the action of the chemicals on the bacterial QS systems can be neglected, whereas during the chronic test, the chemicals may exert considerable effects on the bacterial QS systems and thereby the bacterial behaviors. So we assume that the acute toxicity on the bacteria is caused by the interference with the structures and functions of the biomolecules, while the chronic toxicity should include the effects on the bacterial QS communications. This assumption provides a possibility to extrapolate the chronic toxicity data from the acute ones by using parameters that are concerning the bacterial QS systems. This is what we are going to explore in the present paper.
In this study, the acute (15 min) and chronic (24 h) toxicity of fifteen antibiotics, inclusive of sulfonamides (SAs), sulfonamide potentiators (SAPs) and tetracyclines (TCs), were determined by a bioluminescence inhibition test based on Vibrio fischeri (V. fischeri), both individually and in combination. The differences between the mechanisms of the acute and chronic toxicity were explained from the perspective of bacterial QS communication. A QSTR prediction model was then constructed for the chronic toxicity, by using the acute toxicity and the molecular docking-based descriptors. The current study provides a novel method in predicting the chronic toxicity of antibiotics, which may help make environmental risk assessment on the pollutants.
Results
Individual toxicity of the antibiotics
Comparison between the acute and chronic toxicity of individual antibiotics
The acute and chronic toxicity (−lgEC50) of the individual antibiotics were listed in Table 1. In general, the chronic −lgEC50s were greater than the acute ones, indicating a greater action of the antibiotics on the bacteria during the chronic test. Moreover, the differences between the acute and chronic −lgEC50s varied with the chemical type. The largest differences between the acute and chronic −lgEC50s were observed with the two SAPs, i.e. OMP and TMP. Their acute −lgEC50s were 3.29 and 3.22, while the chronic −lgEC50s were 6.51 and 6.48. The differences between the acute and chronic −lgEC50s for them were 3.12 and 3.26, respectively. With respect to SAs, the differences between the acute and chronic −lgEC50s were moderate, ranging from 0.41 (SDX) to 1.81 (SMP); whereas for TCs, only slight difference were observed between the acute and chronic −lgEC50s, ranging from 0.11 (MH) to 0.71 (CH).
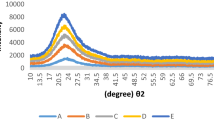
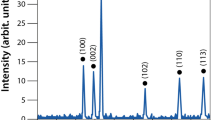
Figure 1 shows the comparisons of the dose-response curves for the acute and chronic toxicity. In particular, the antibiotics at low concentrations presented stimulatory effects on the bioluminescence in chronic test, which manifested hormetic characteristics24. Besides, the slope for the chronic toxicity (Kc) was significantly greater than that for the acute toxicity (Ka), which suggested that the effects of the antibiotics in the chronic test varied from no observed effect to complete (100%) inhibition within a narrow concentration range. For example, in the chronic test, the effects of TMP (Fig. 1j) on V. fischeri varied from no observed effect to complete inhibition with the concentration increasing by only 1.30 × 10−7 mol/L; while in the acute test, the concentration increase for TMP was almost two orders of magnitude, with the log concentration ranging from −4.5 to −2.5 (Fig. 1j). Although Kc was greater than Ka for all of the chemicals, their absolute values varied vastly with the chemical type (see Fig. 2A). For SAs, Ka values distributed within 37.71–71.35, while Kc values ranged from 243.47 to 350.84. With respect to SAPs and TCs, the Ka values fell in the range of 100–200, whereas the Kc values were greater than 1000, with only one exception MH (the Ka and Kc were 89.23 and 834.02, respectively).
The differences between the acute and chronic −lgEC50s, as well as Ka and Kc reflected varying responses of V. fischeri to the antibiotics in the acute and chronic test, implying a much greater susceptibility to the chronic exposure than to the acute exposure. At least two reasons may account for these differences, one is the exposure time, and the other is the varying toxic mechanisms in the acute and chronic actions.
Mechanisms for the acute and chronic toxicity of individual antibiotics
The acute test in the current research takes only 15 min, therefore the acute toxicity of the antibiotics was primarily due to their interference with the light emitting process, and the luciferase might act as the main target of antibiotics25, as shown in Fig. 3B. While the chronic test takes 24 h, during which the bacteria grow from extremely low density to high density (stationary phase), as shown in Figure S1 in the supporting information. During this period, the antibiotics could on the one hand bind with their target proteins26 (DHPS, DHFR and 16S rRNA, respectively), killing or inhibiting the bacterial growth, on the other hand affect the bacterial QS communications (see Figure S2 for detailed information on QS of V. fischeri).
Mechanisms for the acute and chronic toxicity of individual chemicals. (A) The luminescence curves of V. fischeri during 0–24 h. From 0–10 h, there was no QS communication among the bacteria, since the bacteria and the AIs were at low concentrations. After 10 h, the AIs around the bacteria achieved the threshold concentration and triggered on the bacterial QS communication. (B) In the acute test, the antibiotics primarily target the luciferase (Luc) to inhibit the bioluminescence. (C) In the chronic test, the antibiotics acted on LitR to inhibit the QS communication and thereby the bioluminescence.
The expression of the QS-related genes was determined upon exposure to SCP in the chronic toxicity, in order to investigate its influence on the bacterial QS communication. As depicted in Fig. 4, SCP presented concentration-dependent inhibition on the expression of litR, luxR, and dhps. This suggested that the bacterial QS communication were considerably influenced by the exogenous drugs. The decrease in the luxR mRNA expression was probably induced by the depression on the litR expression, since the litR locates in the upstream of lux genes. In light of this, the actions on the LitR proteins by the antibiotics were actually prior to their actions on the LuxR (Fig. 3C). Therefore, the influences of the antibiotics on the LuxR proteins can be represented by the influences on the LitR. In addition, the expression of dhps mRNA was also inhibited by SCP in a similar concentration-dependent mode (Fig. 4). The same change trend of litR and dhps with the SCP concentration indicated that LitR probably participates in regulating the dhps expression. Therefore, the influences of the antibiotics on their target proteins can also be related to their actions on LitR (Fig. 3C).
Quantitative relation between Ka and Kc for individual antibiotics
Based on the above analysis, the antibiotics primarily target luciferase in acute actions, while may influence both their target proteins and the bacterial QS systems in chronic actions. Therefore, the higher sensitivity of V. fischeri in the chronic test was probably due to the interference of antibiotics with the bacterial QS communication, and the differences between Ka and Kc can be explained by the interaction between the antibiotics and the QS-related proteins.
Herein, we introduced lgKc/Ka to represent the difference between Kc and Ka. This parameter may reflect the difference of the V. fischeri sensitivity to the antibiotics in acute and chronic test. A greater value of lgKc/Ka suggested a larger difference in the sensitivities between acute and chronic test. It was then found that lgKc/Ka for the individual antibiotics showed a good correlation (R2 = 0.827) with ELuc and ELitR (Equation 1) through the multiple linear regression analysis.
n = 15, R2 = 0.827, RMSE = 0.053, F = 28.696, P = 0.000, \({{\rm{Q}}}_{{\rm{loo}}}^{2}\) = 0.748, RMSEloo = 0.057, \({{\rm{Q}}}_{{\rm{lto}}}^{2}\) = 0.742, RMSElto = 0.058.
\({{\rm{Q}}}_{{\rm{loo}}}^{2}\) and \({{\rm{Q}}}_{{\rm{lto}}}^{2}\) are the cross-validated squared correlation coefficients from leave-one-out (LOO) and leave-two-out (LTO) cross-validation, respectively. The high \({{\rm{Q}}}_{{\rm{loo}}}^{2}\) = 0.748 and \({{\rm{Q}}}_{{\rm{lto}}}^{2}\) = 0.742 suggested a good internal validation. (The external validation was not performed for the individual toxicity data due to the limited size of the data).
Besides, it was found that the lgKc/Ka also had a good correlation with ELuc and ET (Ebind with the respective targets). As indicated by Equation 2, the determination coefficient (R2) of this model was 0.819, which was slightly lower than that of Equation 1.
n = 15, R2 = 0.819, RMSE = 0.054, F = 27.150, P = 0.000, \({{\rm{Q}}}_{{\rm{loo}}}^{2}\) = 0.725, RMSEloo = 0.059, \({{\rm{Q}}}_{{\rm{lto}}}^{2}\) = 0.718, RMSElto = 0.060.
It should be noticed that ET in Equation 2 was obtained with distinct proteins for different drugs, namely DHPS for SAs, DHFR for SAPs and 30 s subunit of ribosomes for TCs, respectively. Therefore, the ET values varied with not only the composition of the chemicals but also the target proteins. For this reason, the ET in Equation 2 will not be able to discriminate the toxic effect of a defined drug when the target protein varied. In this sense, the moving average approach27,28,29,30 was employed to generate new descriptors ΔE ij , as follows:
In this equation, E i denotes the interaction energy of drug i with the protein, j denotes the target (e.g., DHPS and DHF), and (E ij ) avg is the average value of Ebind for all drugs with the same j. Using this new descriptor, another QSAR model for lgKc/Ka was obtained with high R2 (0.803) as below:
n = 15, R2 = 0.803, RMSE = 0.056, F = 24.490, P = 0.000, \({{\rm{Q}}}_{{\rm{loo}}}^{2}\) = 0.715, RMSEloo = 0.060, \({{\rm{Q}}}_{{\rm{lto}}}^{2}\) = 0.709, RMSElto = 0.061.
In Equations 1, 2 and 4, ELuc represents the effects of antibiotics on luciferase in acute test, while ELitR and ET reflect the effects of antibiotics in chronic actions. The good relationships between them and lgKc/Ka suggested that the distinct targets in the acute and chronic test may account for the differences between Ka and Kc. Furthermore, as noted above, LitR may involve in regulating dhps genes, so the bind of the antibiotics with LitR may affect their actions on the target proteins (Fig. 3C). Consequently, the interaction between the antibiotics and the target proteins (i.e., ET) can be represented by ELitR.
In Equation 1, it was seen that the lgKc/Ka values were negatively correlated to ELitR. This is likely because the lower Ebind values represented stronger interaction between the drugs and the proteins, which resulted in larger differences between the acute and chronic actions. Based on the above analysis, it can be deduced that the difference between Kc and Ka for individual antibiotics was due to the distinct targets in acute and chronic test, and their difference (represented by lgKc/Ka) can be quantitatively characterized by their interaction energy with the proteins (Ebind).
Combined toxicity of the binary antibiotic mixtures
Different joint effects of the antibiotic mixtures
The combined toxicity of the binary mixtures of SA-SA, SA-SAP and SA-TC were determined in both acute and chronic test, the TU of the mixtures were listed in Table S1 in Supporting Information. According to Table S1, all of the mixtures presented antagonistic joint effects in the acute toxicity test, with TU values greater than 1.2. The results were consistent with the findings of Zou et al.19, in which SAs and TMP showed antagonistic joint effects on the bioluminescence of Photobacterium phosphoreum (15 min) with TU ranging from 1.44 to 4.54. This was because the components in the mixtures both target the luciferase in the acute actions (as depicted in Figure S3), and the competition between them may hamper their interaction with the proteins and thus reduced their inhibition on the bioluminescence. In the chronic test, the joint effects of the antibiotic mixtures varied with the type of the components, exhibiting either synergism or addition. For the mixtures of SA-SA, TU values varied from 0.8 to 1.19, suggesting simply additive effects between the two components. This is similar to the results in Fang et al.31 that the binary mixtures of SAs presented additive effects on E. coli (12 h) and B. subtilis (24 h) in chronic test. Unlike SA-SA mixtures, strong synergism was observed with SA-SAP, with TU ranging from 0.37–0.55. The synergistic effects between SAs and SAPs were due to their double blocking effects on the folate metabolism pathways (Figure S3). In detail, SAs inhibited the activity of DHPS, blocking the generation of dihydrofolate; while SAPs interfered with the activity of DHFR and blocked the biosynthesis of tetrahydrofolic acid. As a result, the SA-SAP mixtures lead to increased inhibition on the bacteria. With respect to the mixtures of SA-TC and SAP-TC, antagonistic effects were generally observed, which was in agreement with the results of the acute test. The antagonist effects of SA-TC and SAP-TC in the chronic test were probably due to the mutual effect of the two components. As noted in the study of Long et al.26, TCs can inhibit the protein synthesis and decrease the amount of intracellular DHPS or DHFR accordingly, which led to the decrease of the acting sites of SAs or SAPs and thus weakened their toxicity.
Quantitative relation between Ka and Kc for antibiotic mixtures
The Ka and Kc values for the binary antibiotic mixtures were calculated and the comparisons between them were shown in Fig. 2B. Similarly to the single toxicity, Kc for the mixtures was significantly greater than Ka. Notably, mixtures of SA-SAP that presented synergistic joint effects showed the largest differences between Ka and Kc, with Ka/Kc ranging from 500 to 1500. For the mixtures of SA-TC that are antagonistic, the differences between Ka and Kc were relatively lower, which varied between 100 to 800 fold; while for SA-SA mixtures that showed additive effects, the differences between Ka and Kc were about 300 times.
Similarly, the docking-based descriptors were also employed to construct the QSTR model for \({\rm{lg}}({{\rm{K}}}_{{\rm{c}}}^{{\rm{m}}}/{{\rm{K}}}_{{\rm{a}}}^{{\rm{m}}})\), i.e., the differences between Ka and Kc for the mixtures (\({{\rm{K}}}_{{\rm{c}}}^{{\rm{m}}}\,\)and \({{\rm{K}}}_{{\rm{a}}}^{{\rm{m}}}\)). The total mixture data (81) were split into training (80%, 64 data) and test (20%, 17 data) subsets randomly (see Tables S2 and S3, respectively). A model for \({\rm{lg}}({{\rm{K}}}_{{\rm{c}}}^{{\rm{m}}}/{{\rm{K}}}_{{\rm{a}}}^{{\rm{m}}})\) was developed based on training set using Ebind as the descriptors and the linear equation was as follows:
n = 64, R2 = 0.831, RMSE = 0.031, F = 72.657, P = 0.000, \({{\rm{Q}}}_{{\rm{loo}}}^{2}\) = 0.793, RMSEloo = 0.033, \({{\rm{Q}}}_{{\rm{lmo}}}^{2}\) = 0.792, RMSElmo = 0.033, \({{\rm{Q}}}_{{\rm{F}}1}^{2}\) = 0.789, RMSEP = 0.016.
As seen from Equation 5, the \({\rm{lg}}({{\rm{K}}}_{{\rm{c}}}^{{\rm{m}}}/{{\rm{K}}}_{{\rm{a}}}^{{\rm{m}}})\) values were correlated with four docking-based descriptors, i.e., the ELuc and ELitR of each component (A and B). The four descriptors represent the actions of component A and B in acute and chronic test, respectively. In this equation, \({{\rm{C}}}_{{\rm{A}}}^{{\rm{a}}}\) and \({{\rm{C}}}_{{\rm{B}}}^{{\rm{a}}}\) represented the acute EC50s of component A and B, while \({{\rm{C}}}_{{\rm{A}}}^{{\rm{c}}}\) and \({{\rm{C}}}_{{\rm{B}}}^{{\rm{c}}}\) denoted the chronic EC50s. The parameter \({C}_{i}/\sum C\) indicated the apparent concentration proportion of component i in the mixtures, which was proposed by Zou et al.19 and have been introduced for the QSTR model constructions for mixtures26, 31. This parameter was involved in this model to reflect the varying contribution of drug i in different mixtures. R2 = 0.831 of this model indicated high goodness-of-fit of the training set. Internal validation was carried out using leave-one-out (LOO) and leave-many-out (LMO) method. For the latter case, a group of data including 20% of the training set were left out and predicted later by the model obtained with the remaining 80% of the data. The higher \({{\rm{Q}}}_{{\rm{loo}}}^{2}\) (0.793) and \({{\rm{Q}}}_{{\rm{lmo}}}^{2}\) (0.792) suggested good robustness and stability of this model. The external predictive performance of this model was assessed by \({{\rm{Q}}}_{{\rm{F}}1}^{2}\) 32. The high value of \({{\rm{Q}}}_{{\rm{F}}1}^{2}\) suggested that the constructed model have good predictive performance. Plots of the experimental versus predicted \({\rm{lg}}({{\rm{K}}}_{{\rm{c}}}^{{\rm{m}}}/{{\rm{K}}}_{{\rm{a}}}^{{\rm{m}}})\) were presented in Fig. 5A. It can be seen that the predicted \({\rm{lg}}({{\rm{K}}}_{{\rm{c}}}^{{\rm{m}}}/{{\rm{K}}}_{{\rm{a}}}^{{\rm{m}}})\) values were in good correlation with the experimental values, for both the training and test set. The applicability domain (AD) for this model was characterized by the leverage approach33. A Williams plot of the leverage values versus standardized residuals for every data was obtained, as depicted in Fig. 5B. The Williams plot allows a graphical detection of both the outliers and the influential chemicals in a model34. According to Fig. 5B, all of the leverage values were less than the warning leverage (in this case h* = 0.237 as indicated by the vertical dash line), and there were no outlier data with standard residuals >3δ (indicated by the horizontal dash lines) for both the training and test sets. This suggested that all of the data fall inside the AD of the model, and the model can thus be utilized to predict the \({\rm{lg}}({{\rm{K}}}_{{\rm{c}}}^{{\rm{m}}}/{{\rm{K}}}_{{\rm{a}}}^{{\rm{m}}})\) values.
(A) Plots of experimental versus predicted \({\rm{lg}}({{\rm{K}}}_{{\rm{c}}}^{{\rm{m}}}/{{\rm{K}}}_{{\rm{a}}}^{{\rm{m}}})\) values. (B) Williams plot of the training and test sets with a warning leverage h* = 0.237. h* was calculated by h* = 3(m + 1)/n, where m is the number of the descriptors, and n is the number of the data.
Other functional forms and descriptors were also investigated for the possibility to construct a QSTR model for the \({\rm{lg}}({{\rm{K}}}_{{\rm{c}}}^{{\rm{m}}}/{{\rm{K}}}_{{\rm{a}}}^{{\rm{m}}})\) values. For example, we used the moving average descriptors (ΔE ij ) to construct a model as follows:
n = 64, R2 = 0.292, RMSE = 0.064, F = 6.093, P = 0.000
R2 = 0.292 indicated bad fitting of this model, therefore the moving average descriptors may not apply to the QSTR model construction for the mixture data.
QSTR models for acute to chronic toxicity extrapolation
As depicted in Figure S4, the equation of the linear regression for the dose-response curves is denoted as:
K is the slope of the fitting curve, and b denotes the intercept. Based on this equation, we can obtain the −lgEC50 for the acute and chronic toxicity:
Then, the ratio of −\({{\rm{lgEC}}}_{50}^{{\rm{a}}}\) to −\({{\rm{lgEC}}}_{50}^{{\rm{c}}}\) can be calculated:
Equation 9 can be transformed by taking the logarithm values of the two sides of the equation:
Particularly, we fitted \({\rm{lg}}\,\frac{{{\rm{K}}}_{{\rm{c}}}}{{{\rm{K}}}_{{\rm{a}}}}\) with \({\rm{lg}}\,\frac{50-{b}_{a}}{50-{b}_{c}}\) and found a good correlation between them:
n = 15, R2 = 0.703, RMSE = 0.198, F = 30.724, P = 0.000.
Taking Equations 1 and 11 into Equation 10, we finally obtained the prediction model for the acute to chronic toxicity extrapolation for individual antibiotics:
For antibiotic mixtures, \(\mathrm{lg}\,\frac{{K}_{{\rm{c}}}^{{\rm{m}}}}{{K}_{{\rm{a}}}^{{\rm{m}}}}\) and \(\mathrm{lg}\,\frac{50-{b}_{{\rm{a}}}^{{\rm{m}}}}{50-{b}_{{\rm{c}}}^{{\rm{m}}}}\) also had a good correlation, which was as follows:
n = 64, R2 = 0.971, RMSE = 0.075, F = 2099.31, P = 0.000, \({{\rm{Q}}}_{{\rm{loo}}}^{2}\) = 0.969, RMSEloo = 0.076, \({{\rm{Q}}}_{{\rm{lmo}}}^{2}\) = 0.969, RMSElmo = 0.076, \({{\rm{Q}}}_{{\rm{F}}1}^{2}\) = 0.969, RMSEP = 0.040.
The plots of the experimental versus predicted \({\rm{lg}}\,\frac{50-{b}_{a}^{m}}{50-{b}_{c}^{m}}\) values and the Williams plots of this model were depicted in Fig. 6A and B, respectively. The internal (\({{\rm{Q}}}_{{\rm{loo}}}^{2}\) = 0.969 and \({{\rm{Q}}}_{{\rm{lmo}}}^{2}\) = 0.969) and external validation (\({{\rm{Q}}}_{{\rm{F}}1}^{2}\) = 0.969) and the Williams plot of this model all confirm that this model could be utilized to predict the \({\rm{lg}}\,\frac{50-{b}_{a}^{m}}{50-{b}_{c}^{m}}\) values.
Likewise, taking Equations 5 and 13 into Equation 10, we obtained the final chronic toxicity extrapolation model for the mixtures:
This model was derived from model 5 and 13 that have been well established and validated. This model established a linkage between the chronic and acute mixture toxicity using the docking-based descriptors. Based on this model, we calculated the predicted −\({{\rm{lgEC}}}_{50}^{{\rm{m}},{\rm{c}}}\) and plotted them versus the experimental −\({{\rm{lgEC}}}_{50}^{{\rm{m}},{\rm{c}}}\) values, as shown in Fig. 7. It can be seen from Fig. 7 that there was satisfactory agreement between the observed and predicted values, which suggested that the model could be used to predict the mixture chronic toxicity of the antibiotics.
Moreover, in this model, \(\mathrm{lg}(-{{\rm{lgEC}}}_{50}^{{\rm{c}}})\) is linearly related to \(\,\mathrm{lg}(-{{\rm{lgEC}}}_{50}^{{\rm{a}}})\), which is different from the ACR model that describes a simple linear relationship between \({{\rm{EC}}}_{50}^{{\rm{c}}}\) and \({\,\text{EC}}_{50}^{{\rm{a}}}\). In addition, model 14 also differs from the model proposed by Zou et al.19, in which −\({{\rm{lgEC}}}_{50}^{{\rm{c}}}\) was linearly correlated with −\({{\rm{lgEC}}}_{50}^{{\rm{a}}}\). The complex relationship between \({{\rm{EC}}}_{50}^{{\rm{c}}}\) and \({\,\text{EC}}_{50}^{{\rm{a}}}\) as indicated by model 14 might be the reason for which the predecessors were not able to exactly extrapolate the chronic toxicity from corresponding acute data.
Discussion
In this paper, we put forward a new model (Equation 12) for predicting the chronic toxicity of mixtures based on their acute toxicity. This model reflected a nonlinear correlation between the acute and chronic toxicity, which suggested that the lg(−lgEC50)s for the acute and chronic toxicity presented a good correlation. Compared to previous prediction models, this model was improved with regard to the following aspects.
The present model was based on a good understanding on the toxic mechanisms
The previous models were usually based on a simple safety coefficient for the acute to chronic toxicity extrapolation, without considering the different toxicity mechanisms between the acute and the chronic toxicity. As a consequence, these methods can only apply to the narcotic compounds, whose toxicity effects are merely the baseline toxicity that is related to the lipid solubility as characterized by lgKow. For example, Blaschke et al.35 found that the acute and chronic toxicity of narcotic compounds towards Vibrio fischeri both had a good correlation with lgKow, with determination coefficients up to 0.95 and 0.94, respectively. In this sense, the ACRs for the narcotic compounds are usually constant, because their acute and chronic toxicity shared the same mechanism. Whereas, the ACRs for the reactive compounds (specific acting) may vary vastly (10–10000), because their acute and chronic toxic effects are induced by completely different mechanisms. For instance, Ahlers et al.3 discovered that the variations in ACRs of different reactive compounds can reach 5–6 orders of magnitude, even for the same species. Therefore, it is quite unreliable to simply extrapolate the chronic toxicity of reactive chemicals from the acute data by taking ACRs as a constant value.
In this study, we constructed the prediction model based on the premise that the targets of the chemicals in acute and chronic actions were identified, i.e., luciferase and LitR respectively. The toxic effects of the chemicals in acute and chronic actions were represented by their binding energies with the target proteins, which were used for building the prediction model. This mechanism-based extrapolation was proven to have good predictive capacity.
The present model can apply to compounds with different action mechanisms
Zou et al.19 have developed a QSTR model for predicting the chronic mixture toxicity of SAs and TMP. In Zou’s model, the binding energies of SAs and TMP with luciferase were employed to represent their acute toxicity, while their binding energies with DHPS and DHFR were employed for their chronic toxicity, respectively. We attempted to verify Zou’s model for its ability to predict the chronic mixture toxicity of SAs and TCs, by replacing the binding energies of TMP (with DHFR) with the binding energies of TCs (with 30 s subunit), as indicated by Equation S1 in supporting information.
The comparison between the predicted and experimental values was shown in Figure S5, from which we can see that the predicted −lgEC50s were significantly greater than the experimental values. Therefore, Zou’s model is not suitable for predicting the chronic mixture toxicity of SAs and TCs, though it may have good predictive ability for SA-TMP mixtures. This limitation of Zou’s model is also the problem with many QSTR models, that is, a QSTR model can only apply to the compounds with the same action mechanism, while for compounds with different action mechanisms it may not work20.
In this research, the three types of antibiotics, i.e., SAs, SAPs and TCs, acted through different mechanisms during chronic test by targeting DHPS, DHFR and 30 s subunit, respectively. But in constructing the QSTR models for their binary mixture toxicity, we used their binding energies with LitR to substitute for the binding energies with their respective target proteins. This is feasible because LitR is likely involved in regulating the bacterial growth and thereby the production of the proteins including DHPS, DHFR and 30 s subunit. Particularly, we found a good correlation between the Ebind with LitR (ELitR) and the Ebind with the target proteins (ET) for the three types of antibiotics. As shown in Equation 15, the determination coefficient was up to 0.805.
n = 15, R2 = 0.805, RMSE = 0.016, F = 46.796, P = 0.000.
Therefore, the ELitR can be used to substitute for the ET in constructing the QSTR models. By doing so, we obtained the prediction model that can apply to the compounds with distinct mechanisms.
In particular, our model can be applicable for predicting the chronic toxicity of chemicals with unknown action mechanism, which is also another distinctive advantage of this model. Because this model utilizes Ebind with LitR as the characterization of chronic toxicity without considering the particular targets of the compounds, which makes the prediction model stand a good chance of applying to chemicals with unknown action mechanism.
Limitations of the present model
All prediction models may have some intrinsic limitations from various aspects, and the limitations of this approach can be concluded as follows: firstly, this model can merely apply to binary mixtures at equitoxic ratio. The case of multicomponent mixtures with non-equitoxic ratio should be considered in the following research. What’s more, our model needs to be validated by a large amount of experimental data before it can be put into application confidently.
Materials and Methods
Chemicals and organisms
All of the chemicals were purchased from Aladdin Sigma-Aldrich (St. Louis, MO, USA) (purity ≥99%), as listed in Table 1. V. fischeri (AS 1.3842) was purchased from Species Conservation Center of Chinese Academy of Sciences.
Toxicity test
The acute and chronic toxicity of the chemicals were determined based on a bioluminescence inhibition test, the detailed procedure was as follows: first, the chemicals were prepared into a series of solutions (in 2% NaCl) and added into the diluted bacteria suspension that has been cultured to exponential growth phase. DMSO was added to the chemical solutions with a final concentration of 0.5% v/v in order to enhance the dissolution of the chemicals. The 0.5% v/v DMSO induced no adverse effects on the bacterial growth and the bioluminescence36. For the chronic test, sufficient culture medium was added to support the growth of the bacteria; while in the acute test, the culture medium was replaced with 2% NaCl. After completely mixed, the bacteria suspensions were incubated at 20 °C for 15 min (acute) and 24 h (chronic) respectively. Afterwards, the inhibition rate of chemicals to the bacteria was calculated by the following equation:
where L 0 represents the light intensity of the control group, and L i denotes the light intensity of the exposed group i. Then the dose-response curve was plotted with the compounds’ concentration and their inhibition on the bioluminescence, and the EC50 for acute toxicity of each compound was calculated.
For the mixture toxicity test, the binary mixtures were prepared at equitoxic ratio according to the individual EC50s of the components. Then the mixture toxicity was determined based on the above method and the EC50 for the mixtures (EC50m) were obtained. The joint effects of the antibiotic mixtures are characterized by the total toxicity unit (TU) as calculated by \({\rm{TU}}=\sum \frac{{{\rm{C}}}_{{\rm{i}}}}{{{\rm{EC}}}_{50,{\rm{i}}}}\), where C i was the concentration of each component when the inhibition rate of the mixture achieved 50%; EC50,i represented EC50 of the individual component i. TU ranging from 0.8 to 1.2 represents additive joint effect, while TU > 1.2 indicates antagonism and TU < 0.8 synergism37.
Homology Modeling
The crystal structures of the proteins are required for the protein-chemical docking studies. For luciferase, LitR and the 30 s subunit of ribosomes, their crystal structures (3FGC, 3WHP and 4U1U, respectively) were directly obtained from the protein data bank (PDB, http://www.pdb.org). While the crystal structures of dihydropteroate synthase (DHPS) and dihydrofolate reductase (DHFR) were constructed using Homology Modeling module in Discovery Studio 3.1 (DS3.1, Accelrys Software Inc., San Diego, CA). The protein sequences YP_203863.1 (DHPS) and Q5E7M1 (DHFR) were obtained from NCBI (https://www.ncbi.nlm.nih.gov), which were selected as the target sequences for the homology modeling. BLAST (Basic Local Alignment Search Tool) at the NCBI website (http://blast.ncbi.nlm.nih.gov/Blast.cgi) was then run with the two sequences over the protein database bank, based on which 1AJ0 and 3TYU were selected as the templates for DHPS and DHFR, respectively. Afterwards, Align Sequence to the Templates wizard was performed on DS3.1, followed by the Building Homology Model. The “copy ligand” function was employed during the modeling, which embedded the ligand of the templates into the modeled proteins. In the Building Homology Model protocol, the number of models was set as 20, which generates 20 modeled structures for each protein. These structures were then subjected to Verify Protein (MODELER), and the structure with the highest Verify Score was chosen for the docking studies after the Loop Refinement (MODDLER).
Molecular Docking
Molecular Docking was performed by CDOCKER module in DS3.1. The crystal structures of the proteins are in complex with their ligands. Their active sites were defined by selecting the ligands as the centers with the radius of the site sphere at 11.0 Å. Prior to the docking work, the proteins were prepared by the protein preparation wizard, and the chemicals were subjected to the energy minimization. Then the CDOCKER docking was performed with the default parameters. The CDOCKER used the soft-core potentials with an optional grid representation to dock ligands into the active site of the receptor. 10 random conformers were generated for each compound, and the lowest CDOCKER interaction energy (Ebind) was selected to represent its binding affinity with the receptor.
Data Analysis
Multiple linear regressions were performed using SPSS 18.0 (SPSS Inc.). The statistical quality of the fitted models was evaluated by the square of the correlation coefficient (R2), root mean standard error (RMSE), Fischer ratio (F), and the significant level (P). Cross-validation was employed for the internal validation of the constructed models using LOO (\({{\rm{Q}}}_{{\rm{loo}}}^{2}\)), LTO (\({{\rm{Q}}}_{{\rm{lto}}}^{2}\)) and LMO (\({{\rm{Q}}}_{{\rm{lmo}}}^{2}\)) methods. In the cross-validation, different proportions of data (one, two and many for LOO, LTO and LMO, respectively) are iteratively held-out from the training set and predicted as new by the developed model in order to verify internal “predictivity”38. Q2 was calculated by the following equation:
where y i , and \(\overline{{y}_{i}}\) are the actual and predicted values of the dependent variables in the training set, respectively; y mean is the average value of all the dependent variables in the training set. The external validation of the model was characterized by \({{\rm{Q}}}_{{\rm{F}}1}^{2}\) 39, which was calculated as follows:
where Y i and \(\overline{{Y}_{i}}\) are the actual and predicted values of the dependent variables in the test set, respectively; y mean is the average value of all the dependent variables in the training set.
Conclusion
In the current work, a QSTR model was built for predicting the chronic mixture toxicity of antibiotics on bioluminescence based on the acute data and the docking-based descriptors. This model revealed a complex relationship between the acute and chronic toxicity, i.e. the lg(−lgEC50)s for the acute and chronic toxicity were linearly correlated. This is different from the ACR prediction method that describes a simple linear relationship between EC50s for the acute and chronic toxicity. The present model was based on a good understanding on the differences between the acute and chronic action mechanisms. In particular, the interaction energies (Ebind) of the chemicals with LitR, rather than their respective target proteins, were introduced to represent their toxic effects in the chronic test. Therefore, the present model could probably apply to chemicals with distinct toxic mechanisms as well as those with undefined toxic mechanism. This breaks the limitation of the traditional QSTR models that can only apply to chemicals with similar structures or the same toxic mechanisms. Although the prediction capacity of the present model still needs further validation, it may provide a novel idea for the acute to chronic toxicity extrapolation studies, which may help with the environmental risk assessment on the pollutants.
References
Sun, K., Krause, G. F., Mayer, F. L., Ellersieck, M. R. & Basu, A. P. Predicting chronic lethality of chemicals to fishes from acute toxicity test data: Theory of accelerated life testing. Environ. Toxicol. Chem. 14, 1745–1752 (1995).
Kenaga, E. E. Predictability of chronic toxicity from acute toxicity of chemicals in fish and aquatic invertebrates. Environ. Toxicol. Chem. 1, 347–358 (1982).
Ahlers, J. et al. Acute to chronic ratios in aquatic toxicity—variation across trophic levels and relationship with chemical structure. Environ. Toxicol. Chem. 25, 2937–2945 (2006).
Hoff, D. et al. Predicting the toxicities of chemicals to aquatic animal species. US Environ. Prot. Agency, Washington, DC (2010).
Stephen, C. E. et al. Guidelines for deriving numerical national water quality criteria for the protection of aquatic organisms and their uses. US EPA, Off. Water Regul. Stand. Criteria, Washingt. DC PB85-227049 (1985).
Barron, M. G. & Wharton, S. R. Survey of methodologies for developing media screening values for ecological risk assessment. Integr. Environ. Assess. Manag. 1, 320–332 (2005).
Verhaar, H. J. M., Van Leeuwen, C. J. & Hermens, J. L. M. Classifying environmental pollutants. Chemosphere 25, 471–491 (1992).
Niederlehner, B. R., Cairns, J. & Smith, E. P. Modeling Acute and Chronic Toxicity of Nonpolar Narcotic Chemicals and Mixtures toCeriodaphnia dubia. Ecotoxicol. Environ. Saf. 39, 136–146 (1998).
Bradbury, S. P. Quantitative Structure-Activity-Relationships and Ecological Risk Assessment-An Overview of Predictive Aquatic Toxicology Research. Toxicol. Lett. 79, 229–237 (1995).
Wang, C., Lu, G. H. & Li, Y. M. QSARs for the Chronic Toxicity of Halogenated Benzenes to Bacteria in Natural Waters. Bull. Environ. Contam. Toxicol. 75, 102–108 (2005).
Fan, D. et al. Development of Quantitative Structure–Activity Relationship Models for Predicting Chronic Toxicity of Substituted Benzenes to Daphnia Magna. Bull. Environ. Contam. Toxicol. 96, 664–670 (2016).
McCarty, L. S., Hodson, P. V., Craig, G. R. & Kaiser, K. L. E. The use of quantitative structure-activity relationships to predict the acute and chronic toxicities of organic chemicals to fish. Environ. Toxicol. Chem. 4, 595–606 (1985).
Cronin, M. T. D. & Dearden, J. C. QSAR in Toxicology. 3. Prediction of Chronic Toxicities. Quant. Struct. Relationships 14, 329–334 (1995).
Tuppurainen, K., Lötjönen, S., Laatikainen, R. & Vartiainen, T. Structural and electronic properties of MX compounds related to TA100 mutagenicity. A semi-empirical molecular orbital QSAR study. Mutat. Res. Mol. Mech. Mutagen. 266, 181–188 (1992).
Debnath, A. K., Lopez de Compadre, R. L., Debnath, G., Shusterman, A. J. & Hansch, C. Structure-activity relationship of mutagenic aromatic and heteroaromatic nitro compounds. Correlation with molecular orbital energies and hydrophobicity. J. Med. Chem. 34, 786–797 (1991).
Zhang, L., Sannes, K., Shusterman, A. J. & Hansch, C. The structure-activity relationship of skin carcinogenicity of aromatic hydrocarbons and heterocycles. Chem. Biol. Interact. 81, 149–180 (1992).
Brown, L. P., Lewis, D. F. V., Flint, O. P., Orton, T. C. & Gibson, G. G. Teratogenicity of phenylhydantoins in an in vitro system: Molecular orbital-generated quantitative structure-toxicity relationships. Xenobiotica 19, 1471–1481 (1989).
Jiang, L., Lin, Z., Hu, X. & Yin, D. Toxicity Prediction of Antibiotics on Luminescent Bacteria, Photobacterium phosphoreum, Based on Their Quantitative Structure–Activity Relationship Models. Bull. Environ. Contam. Toxicol. 85, 550–555 (2010).
Zou, X., Lin, Z., Deng, Z., Yin, D. & Zhang, Y. The joint effects of sulfonamides and their potentiator on Photobacterium phosphoreum: Differences between the acute and chronic mixture toxicity mechanisms. Chemosphere 86, 30–35 (2012).
Harder, A., Escher, B. I. & Schwarzenbach, R. P. Applicability and Limitation of QSARs for the Toxicity of Electrophilic Chemicals. Environ. Sci. Technol. 37, 4955–4961 (2003).
Bassler, B. L. & Miller, M. B. In (eds Rosenberg, E., DeLong, E. F., Lory, S., Stackebrandt, E. & Thompson, F.) 495–509, doi:10.1007/978-3-642-30123-0_60 (Springer Berlin Heidelberg, 2013).
Parsek, M. R. & Greenberg, E. P. Sociomicrobiology: the connections between quorum sensing and biofilms. Trends Microbiol. 13, 27–33 (2005).
Henke, J. M. & Bassler, B. L. Three Parallel Quorum-Sensing Systems Regulate Gene Expression in Vibrio harveyi. J. Bacteriol. 186, 6902–6914 (2004).
Calabrese, E. J. Hormesis is central to toxicology, pharmacology and risk assessment. Hum. Exp. Toxicol. 29, 249–261 (2010).
Ma, X. Y. et al. Bioassay based luminescent bacteria: Interferences, improvements, and applications. Sci. Total Environ. 468–469, 1–11 (2014).
Long, X. et al. The mixture toxicity of environmental contaminants containing sulfonamides and other antibiotics in Escherichia coli: Differences in both the special target proteins of individual chemicals and their effective combined concentration. Chemosphere 158, 193–203 (2016).
Kleandrova, V. V. et al. Computational ecotoxicology: Simultaneous prediction of ecotoxic effects of nanoparticles under different experimental conditions. Environ. Int. 73, 288–294 (2014).
Luan, F. et al. Computer-aided nanotoxicology: Assessing cytotoxicity of nanoparticles under diverse experimental conditions by using a novel QSTR-perturbation approach. Nanoscale 6, 10623–10630 (2014).
Kleandrova, V. V. et al. Computational tool for risk assessment of nanomaterials: Novel QSTR-perturbation model for simultaneous prediction of ecotoxicity and cytotoxicity of uncoated and coated nanoparticles under multiple experimental conditions. Environ. Sci. Technol. 48, 14686–14694 (2014).
Ran, T. et al. Gastrointestinal Spatiotemporal mRNA Expression of Ghrelin vs Growth Hormone Receptor and New Growth Yield Machine Learning Model Based on Perturbation Theory. Nat. Publ. Gr. 1–14, doi:10.1038/srep30174 (2016).
Fang, S. et al. Similarities and differences in combined toxicity of sulfonamides and other antibiotics towards bacteria for environmental risk assessment. Environ. Monit. Assess. 188 (2016).
Tropsha, A., Gramatica, P. & Gombar, V. K. The Importance of Being Earnest: Validation is the Absolute Essential for Successful Application and Interpretation of QSPR Models. QSAR Comb. Sci. 22, 69–77 (2003).
Eriksson, L. et al. Methods for reliability and uncertainty assessment and for applicability evaluations of classification- and regression-based QSARs. Environ. Health Perspect. 111, 1361–1375 (2003).
Pourbasheer, E., Aalizadeh, R., Ganjali, M. R., Norouzi, P. & Shadmanesh, J. QSAR study of ACK1 inhibitors by genetic algorithm-multiple linear regression (GA-MLR). J. Saudi Chem. Soc. 18, 681–688 (2014).
Blaschke, U., Paschke, A., Rensch, I. & Schüürmann, G. Acute and Chronic Toxicity toward the Bacteria Vibrio fischeri of Organic Narcotics and Epoxides: Structural Alerts for Epoxide Excess Toxicity. Chem. Res. Toxicol. 23, 1936–1946 (2010).
Fernández-Alba, A. R., Hernando, M. D., Piedra, L. & Chisti, Y. Toxicity evaluation of single and mixed antifouling biocides measured with acute toxicity bioassays. Anal. Chim. Acta 456, 303–312 (2002).
Broderius, S. J., Kahl, M. D. & Hoglund, M. D. Use of joint toxic response to define the primary mode of toxic action for diverse industrial organic chemicals. Environ. Toxicol. Chem. 14, 1591–1605 (1995).
Gramatica, P. Principles of QSAR models validation: Internal and external. QSAR Comb. Sci. 26, 694–701 (2007).
Gramatica, P. & Sangion, A. A Historical Excursus on the Statistical Validation Parameters for QSAR Models: A Clarification Concerning Metrics and Terminology. J. Chem. Inf. Model. 56, 1127–1131 (2016).
Acknowledgements
This work was funded by the State Key Laboratory of Pollution Control and Resource Reuse Foundation (PCRRK16007), the National Natural Science Foundation of China (21377096, 21577105), “Climbing” Program of Tongji university (0400219287), the 111 Project, Science & Technology Commission of Shanghai Municipality (14DZ2261100), Shanghai Municipal Committee of Science and Technology (17DZ1200100), China Postdoctoral Science Foundation (2016M600332).
Author information
Authors and Affiliations
Contributions
Dali Wang and Zhifen Lin performed and designed the experiments. Yue Gu analyzed the experimental data. Dali Wang wrote the manuscript and Zhifen Lin revised the manuscript. Min Zheng, Wei Zhang and Ying Liu helped with the experiment.
Corresponding author
Ethics declarations
Competing Interests
The authors declare that they have no competing interests.
Additional information
Publisher's note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Wang, D., Gu, Y., Zheng, M. et al. A Mechanism-based QSTR Model for Acute to Chronic Toxicity Extrapolation: A Case Study of Antibiotics on Luminous Bacteria. Sci Rep 7, 6022 (2017). https://doi.org/10.1038/s41598-017-06384-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-017-06384-9
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.