Abstract
This study investigated the relationships among plasma biomarkers, regional brain atrophy, and clinical symptoms in patients with Alzheimer’s disease (AD; n = 177), mild cognitive impairment (MCI; N = 60) and controls (n = 108). The Mini-Mental Status Examination (MMSE), Clinical Dementia Rating (CDR), and Neuropsychiatric Inventory (NPI) subscales were administered to subjects. Magnetic resonance imaging was performed and medial temporal atrophy (MTA) and posterior atrophy (PA) were assessed visually. We examined associations among cognition, NPI score, plasma β-amyloid (Aβ) and clusterin levels, and regional brain atrophy in patients with AD by regression analysis. The mean MTA score was associated with the plasma Aβ1-42/Aβ1-40 ratio (r = 0.38, p = 0.01) and with MMSE scores (r = 0.43, p < 0.01). The plasma clusterin level was correlated with CDR sum of box and right-side PA scores (r = 0.28, p = 0.01 and r = 0.30, p = 0.03, respectively). Right-side PA scores were correlated significantly with NPI agitation/aggression (r = 0.30, p = 0.03) subscale scores. In conclusion, the plasma ratio of Aβ1-42/Aβ1-40 and clusterin level may be associated with different patterns of regional brain atrophy, which in turn may account for the clinical symptoms in patients with AD.
Similar content being viewed by others
Introduction
Alzheimer’s disease (AD) is a neurodegenerative disorder characterized by progressive cognitive dysfunction, behavioral changes, and loss of functional ability. The diagnosis of AD relies on the presence of cognitive impairment, namely, episodic memory loss combined with other cognitive deficits. Several cognitive screening tests, including the Mini-Mental State Examination (MMSE) and the DemTect1, 2, have been developed to measure the cognitive deficits in AD. These deficits are correlated with structural changes in the brain3, 4. In addition, 75–90% of patients with AD develop “non-cognitive” behavioral and psychological symptoms of dementia (BPSD), which can be classified using the Neuropsychiatric Inventory (NPI)5,6,7,8. The prevalence of BPSD in patients with early-stage AD ranges from 17% to 46%. Factor analysis can be used to cluster these symptoms into several behavioral groups6, 9, typically consisting of three or four of the following: agitation/aggression (hyperactivity), mood/apathy, frontal symptoms, and psychosis8, 9. Agitation and aggression symptoms are difficult to manage and are especially distressing for patients, caregivers, and medical staff members. The underlying pathophysiological mechanisms of BPSD are not understood, although genetic factors (e.g., apolipoprotein E [ApoE] polymorphism) and certain regional brain dysfunctions have been suggested to play significant roles10,11,12.
Newly developed non-invasive neuroimaging tools, such as brain magnetic resonance imaging (MRI), aid the examination of relationships between cognitive and behavioral symptoms and regional brain dysfunction. From an anatomical point of view, regional brain atrophy is associated with different cognitive symptoms13. In BPSD, gray matter loss in the frontolimbic cortex has been associated with agitation/aggression symptoms12. Atrophy of the lateral frontal, parietal, and anterior cingulate gyrus has been associated with the onset of psychotic symptoms, including delusion, agitation, wandering, and hallucination, and/or the need for chronic use of antipsychotic medication14. In addition, cerebral white matter lesions have been associated independently with BPSD in patients with AD15. Although various brain regions are associated with agitation and aggression symptoms, their relationships to regional brain changes and plasma biomarkers remain unknown.
Plasma amyloid ß peptide (Aß) is a blood-based biomarker used to detect underlying AD pathology16. Increased and decreased plasma amyloid ß peptide 1–40 (Aß1-40) and amyloid ß peptide 1–42 (Aß1-42) levels have been reported in patients with AD17,18,19. Increased plasma Aß1-40 levels have been associated with atrophy of the medial temporal lobe structures in subjects without dementia20. Plasma amyloid levels have also been correlated with cognitive dysfunction in patients with AD21. Plasma clusterin, also known as apolipoprotein J, is a chaperone protein that is expressed widely in brain tissue. This plasma biomarker may also be related to the diagnosis of AD and regional brain atrophy22. In our previous study, right-side posterior atrophy (PA) and medial temporal atrophy (MTA), measured by MRI, were associated with the NPI agitation/aggression subscale score and cognitive impairment in patients with AD11. The current study was conducted to further investigate the relationships among plasma Aß and clusterin levels, atrophy ratings determined by MRI assessment, and clinical symptoms in patients with AD and those with mild cognitive impairment (MCI).
Results
Demographic, clinical and plasma biomarker data from study subjects
A total of 345 patients (probable AD, n = 177; MCI, n = 60, control, n = 108) were recruited during the study period. The mean (±standard deviation) ages of patients with AD were 81.0 ± 5.8 and 73.9 ± 8.3 years for patients with MCI and 74.6 ± 7.7 years for controls; 49.2% of patients with AD, 45.2% of patients with MCI and 44.4% controls were women (Table 1). In the AD group, mean NPI agitation/aggression, mood, and frontal symptoms scores were 6.8, 5.5, and 5.5, respectively. Values for plasma Aß1-40 and Aß1-42 levels and the Aß1-42/Aß1-40 ratio were log transformed for further analysis due to the high degree of kurtosis (>3) of data distribution. Plasma Aß1-40 and clusterin levels showed a significant group difference between patients with AD and controls and patients with MCI and controls by t-tests (all p < 0.01; Table 2). In a regression analysis adjusted for age, sex, and ApoE4 carrier status, the significant higher level of in plasma Aß1-40 and clusterin levels were found in patients with AD and MCI than controls (all p < 0.01, respectively). The body mass index (BMI) was not associated with the plasma Aß1-40, Aß1-42, or clusterin level or the Aß1-42/Aß1-40 ratio in the adjusted analysis.
Plasma biomarkers, MRI visual ratings, and clinical symptoms
In patients with AD, the plasma Aß1-40 and clusterin levels were correlated significantly with age (Pearson correlation coefficient = 0.21 and −0.17, respectively, all p < 0.05). The plasma Aß1-42/Aß1-40 ratio was not associated with age, sex, disease duration, BMI, or ApoE4 carrier status, but it was associated weakly with the mean MTA score (Pearson correlation coefficient = −0.16, p = 0.04; Table 3). The clusterin level was associated significantly with the Clinical Dementia Rating sum of box (CDR-SB) score (Pearson correlation coefficient = 0.14, p = 0.04). Plasma Aß1-40 and clusterin levels were not associated with the MMSE score or delayed recall of 12 items memory test.
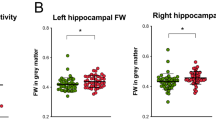
A regression analysis adjusted for age, years of education, sex, and ApoE4 carrier status showed that the Aß1-42/Aß1-40 ratio was moderately significantly correlated with the mean MTA score (r = 0.38, p = 0.01), but not with the PA score, in patients with AD (Table 4). Post-hoc calculation of the statistical power achieved yielded a value of 0.99 under the conditions α = 0.05 and sample size = 170. The Aß1-42/Aß1-40 ratio was not associated with the MMSE score (statistical power = 0.90 under the same conditions). The clusterin level was correlated significantly with the CDR-SB and right-side PA scores after adjustment for multiple covariates (r = 0.28, p < 0.01 and r = 0.30, p = 0.03, respectively; Table 5). It was not correlated with the MMSE, agitation/aggression, frontal symptoms, or mean MTA score (statistical power >0.9 under the conditions α = 0.05 and sample size = 174). No significant association was observed between plasma biomarkers and the white matter hyperintensity (WMH) score. All post-hoc values for the statistical power achieved exceeded 0.80 under the conditions α = 0.05 and sample size = 176. In patients with MCI, no association was found between plasma biomarker, MMSE scores and NPI symptoms.
MRI rating and clinical measurements in patients with AD
In patients with AD, MTA and PA scores within each hemisphere were not correlated (right side: r = 0.08, p = 0.32; left side: 0.10, p = 0.20). Regression analysis with adjustment for age, years of education, sex, and ApoE4 carrier status showed that the mean MTA score was moderately significantly correlated with the MMSE score in patients with AD (r = 0.43, p < 0.01). The post-hoc calculation of the statistical power achieved yielded a value of 0.99 under the conditions α = 0.05 and sample size = 177. We also observed a significant association between the CDR-SB and mean MTA scores (r = 0.30, p < 0.01). The mean PA score was not correlated significantly with the MMSE score after adjustment for age and years of education (statistical power = 0.89 under the conditions α = 0.05 and sample size = 176). The right-side PA score, but not the left-side PA or MTA score, was moderately significantly associated with the NPI agitation/aggression (r = 0.30, p = 0.03) and frontal symptoms (r = 0.31, p < 0.01) subscale scores after adjustment for multiple covariates. All post-hoc values for the statistical power achieved exceeded 0.90 under the conditions α = 0.05 and sample size = 176. In patients with MCI, no association was found between MRI visual rating scores, MMSE scores and NPI symptoms.
Discussion
In this study, we investigated the relationships among plasma biomarkers, cognitive function, agitation/aggression symptoms, frontal symptoms, and MRI-based visual ratings in patients with AD and those with MCI. First, our results demonstrated that the plasma clusterin level was correlated with the severity of AD, as measured by the CDR-SB scale, even after adjustment for multiple covariates. Second, the plasma Aß1-42/Aß1-40 ratio was correlated with the mean MTA score, and the clusterin level was correlated with the right-side PA score, in patients with AD. Third, regional brain atrophy, as measured by the MTA score, was associated with MMSE and CDR-SB scores, and the right-side PA score was associated with the NPI agitation/aggression and frontal symptoms scores. These results suggest that different plasma biomarkers were linked individually to regional brain atrophy and that these changes were correspondingly associated with clinical symptoms in patients with AD.
Plasma Aß levels, cognition, and brain structure
In patients with AD, increased plasma Aß1-40 or Aß1-42 levels have been reported23, 24. Other studies have shown no difference or even decreases in the Aß1-42 level21, 25. This wide variation in plasma Aß levels and the use of different assay techniques among studies have contributed substantially to discrepancies among findings26. In general, the broad overlap in plasma Aß levels between patients with AD and controls indicates that these levels cannot differentiate cases of sporadic AD from control cases. High plasma concentrations of Aß1-40 and low plasma concentrations of Aß1-42 indicate an increased risk of dementia27. In some studies, plasma Aß levels and the Aß1-42/Aß1-40 ratio have been associated significantly with MMSE and memory scores21, 28. However, other studies have found no association between plasma Aß levels and MMSE scores, leading the authors to conclude that age, rather than the AD diagnosis, was the main predictor of these levels29. These findings are consistent with our results: although the plasma Aß1-40 level of patients with AD was significantly higher than that of controls, even after adjustment for multiple covariates, the plasma Aß1-40 level and the Aß1-42/Aß1-40 ratio were not associated with the MMSE score. Our statistical power calculation confirmed that our sample size was sufficient to support the validity of these findings.
Findings regarding the relationships of plasma Aß levels to brain structure parameters are more consistent. In dementia-free subjects, a high plasma Aß1-40 level and low plasma ratio of Aß1-42/Aß1-40 were associated with smaller hippocampal volume and accelerated global and regional brain atrophy, respectively20. Sotolongo-Grau et al.30 also reported that the left hippocampal volume was associated strongly with cell-bound Aß1-40 in blood in patients with AD. The relationships of plasma Aß levels to regional brain atrophy could be attributed to Aß deposition in the brain. A low plasma Aß1-42/Aß1-40 ratio has been linked to increased Aß deposition in the brain parenchyma, which induces brain atrophy, as determined by amyloid positron emission tomography25.
The plasma clusterin level, dementia severity, and the right-side PA score
Several studies have documented increased plasma clusterin levels in patients with AD, although other studies have produced negative findings22, 31, 32. Previous studies have also revealed associations between the plasma clusterin level and AD severity and entorhinal cortex atrophy22, 31, 33. In our study, the plasma clusterin level was significantly higher in patients with AD than in controls, even after adjustment for multiple confounders. In addition, the association observed between the plasma clusterin level and CDR-SB score was compatible with previous findings22. However, we found no association between the MTA rating and the plasma clusterin level. Our statistical power calculation confirmed that this lack of association was not related to the sample size.
We found that the plasma clusterin level was associated significantly with the right-side PA score. In our previous study and in the current sample, right-side PA scores were associated with the NPI agitation/aggression symptoms score11.
However, the plasma clusterin level was not correlated with the NPI agitation/aggression or frontal symptoms subscale score. These findings suggest that the plasma clusterin level was correlated with the right-side PA score in patients with AD, but was not associated directly with the NPI agitation/aggression symptoms score. Elizabeta et al.34 recently found that the plasma/platelet clusterin ratio was associated positively with NPI measures of agitation, apathy, irritability, and motor aberrant behavior in subjects with AD showing BPSD. Further studies are needed to elucidate the potential role of the clusterin level in the development of behavioral symptoms in patients with AD.
Plasma biomarker and MCI
In patients with MCI, our results showed higher level of plasma Aß1-40 and clusterin than controls, which is in line with previous studies35, 36. However, our findings did not show association between plasma biomarkers and clinical symptoms or MR visual rating scores. A recent study showed plasma ratio of Aß1-42/Aß1-40 was stepwise decreased from age-matched controls via MCI to AD and shows a clear correlation with memory scores37. Another study showed plasma clusterin level was negatively correlated with cognitive scores of patients with MCI38. These discrepancies may relate to the heterogeneous of MCI group, the different diagnostic criteria of MCI, fewer subjects sample size in our group and different measurement tools. From recent review, it showed not all patients with MCI convert to AD reversion of MCI in about 30–50% within 2–5 years follow-up39.
Study limitations
This study has several limitations. First, we did not include all factors potentially confounding plasma Aß data. Previous studies have shown that factors such as age, race, ApoE status, education, and creatinine level may influence plasma Aß levels40. In addition, Aß in plasma does not originate exclusively from the brain; it is also the product of amyloid precursor protein metabolism in the skeletal muscle, pancreas, kidney, and liver. Platelets are another important source of Aß1-40 and Aß1-42 in plasma41. Thus, the plasma Aß level may only partially reflect Aß in the brain. The methods of plasma Aß and clusterin measurement must also be considered in interpreting our results. We did not measure cell-bound Aß or the platelet clusterin level. Cell-bound Aß may be more closely related than plasma Aß to their physiological counterpart, hippocampal damage30. Plasma and platelet clusterin ratios may better correlate with agitation symptoms in patients with AD34.
Second, the number of subjects included in the study was not large and age differed significantly between patients with AD and controls. Although the regression analysis was adjusted for age and had sufficient statistical power, we could not completely exclude the confounding effect of age on our results. A study conducted with a large number of age-matched controls might help to build strong evidence for the relationships between plasma biomarkers and clinical symptoms. In addition, as we did not include large number of patients with MCI, our findings are not necessarily applicable to the period before the onset of clinical dementia symptoms. This factor may limit the clinical impact of this study on the early diagnosis of AD.
Third, we did not extensively evaluate whole brain atrophy scores or other regional brain atrophy, such as that occurring in the frontal lobe or subcortical region. This factor may have contributed partially to the lack of a significant association between the plasma clusterin level and MTA score. Furthermore, we could not examine relationships between frontal lobe atrophy and clinical symptoms and plasma biomarkers. Future studies involving whole-brain rating or even voxel-based analysis may improve upon our findings.
Conclusion
Our results revealed that the plasma Aß1-42/Aß1-40 ratio is correlated with MTA. The mean MTA score was associated significantly with cognitive symptoms. The plasma clusterin level was associated with the severity of AD and right-side PA, which may be related to NPI agitation/aggression symptoms in patients with AD.
Methods
Subjects
Subjects with AD were recruited from the outpatient clinic of Taipei Veterans General Hospital between August 2012 and November 2014. The ages between 60 and 90 of both genders with adequate visual and auditory abilities to perform all aspects of the study assessments were included. The diagnosis of probable AD followed the clinical criteria described by the National Institute on Aging–Alzheimer’s Association42. Diagnoses were made during a multidisciplinary consensus meeting. All patients underwent a standardized assessment that included the acquisition of data on dementia history, neuropsychological assessment, laboratory tests, and MRI examination. Availability of a reliable caregiver who lives with the subjects or has at least 10 hours/week of contact with the subject was needed. The disease duration was defined as the period between the initial onset of symptoms, reported by caregivers, and the performance of this study. The exclusion criteria was subjects who had significant neurological disease other than AD that may affect cognition, such as Parkinson’s disease, multi-infarct dementia, Huntington’s disease, normal pressure hydrocephalus, brain tumor, progressive supranuclear palsy, seizure disorder, subdural hematoma, multiple sclerosis, or history of significant head trauma followed by persistent neurologic defaults or known structural brain abnormalities were excluded. Controls were recruited among spouses of patients with AD who were included in the study and cognitively healthy patients who presented to the Department of Neurology for the assessment of other disorders. Subjects with histories of major neurological, psychiatric, or severe cardiovascular diseases were excluded from the study. All methods were performed in accordance with the relevant guidelines and regulations. The Institutional Review Board of Taipei Veterans General Hospital approved this study. Written informed consent was obtained from participants and their next of kin or legally authorized representatives.
Measurement of ApoE gene, plasma Aß and clusterin levels
Genomic DNA was isolated from whole blood using the Gentra Puregene kit (Qiagen, Hilden, Germany), according to the manufacturer’s protocol. The presence of the ε2, ε3, and ε4 alleles of the ApoE gene was determined by assessing the sequences at two single-nucleotide polymorphisms (rs429358 and rs7412)10, 43. The ApoE4 gene carrier was defined as one of the alleles containing the ε4 gene.
Blood samples were collected in tubes containing sodium EDTA as an anticoagulant. Following centrifugation, plasma was aliquoted into polypropylene tubes and stored at −80 °C until analysis. Plasma clusterin levels were measured using a Human Clusterin Quantikine ELISA Kit (R&D Systems, Minneapolis, MN, USA) following the manufacturer’s instructions and standard procedures. The plasma Aß peptide assay was performed using the INNO-BIA plasma Aß forms assay (Innogenetics, Ghent, Belgium) based on the multiplex xMAP technique with a LABScan-100 system (Luminex BV, The Netherlands). Each sample was assessed in duplicate. All samples from each participant were measured together on the same plate to avoid interplate variation. The coefficients of variation of the two assays were less than 20%.
Neuropsychological assessment
Cognitive function was assessed using standardized tests that included several domains. In controls and patients with AD, the MMSE was used to assess global cognition2. To evaluate the severity of dementia, the CDR and CDR-SB scores were determined with caregivers’ input44. Only patients with AD underwent detailed cognition and NPI studies. To assess memory, we used the delayed recall of 12 items memory test45. To examine language function, we used the modified Boston Naming Test46. A categorical verbal fluency test was used to evaluate verbal ability and executive control. In this test, the subject named as many fruits as possible within 1 minute47. Forward digit span and digit reversal tests were used to assess attention and working memory domain48. Finally, the NPI questionnaire was administered to assess the frequency and severity of BPSD7, 49. The NPI agitation/aggression, mood and frontal symptoms subscales were used in this study8. The NPI agitation/aggression subscale includes agitation/aggression, disinhibition, irritability, and aberrant motor behavior items. The NPI mood subscale includes depression, anxiety, and irritability items. The NPI frontal symptoms subscale includes apathy, disinhibition, irritability, and euphoria items. Each subscale score was calculated by summing item scores (indicating severity) and then multiplying by duration. Trained raters administered all tests in a clinical setting.
MRI and image analysis
Patients with AD underwent whole-brain MRI (3T DISCOVERY 750; GE) as part of the clinical assessment. First, trans-axial T2-weighted scans (TR/TE = 1130/80 ms, NEX = 2, voxel size = 0.55 × 0.55 × 10 mm3), 3D fluid-attenuated inversion recovery (FLAIR) images (TR/TE = 6000/126 ms, inversion time = 1861 ms, NEX = 1, voxel size = 0.56 × 0.56 × 1 mm3), and high-resolution sagittal T1-weighted images (TR/TE = 9.1/3.7 ms, NEX = 1, voxel size = 0.5 × 0.5 × 1.0 mm3) were acquired. The image analysis and rating procedure has been described in detail previously11. In short, image analysis included the visual rating of MTA and PA on T1-weighted images. The MTA in the hippocampus was rated using a 5-point scale50. PA in the posterior cingulate, parieto-occipital region, and precuneus was rated using a 4-point scale51. Mean MTA and PA scores were calculated for both hemispheres. WMH was evaluated using a scale of age-related white matter change (ARWMC) on axial T2-weighted and 3D-FLAIR images52. The 4-point ARWMC scale rates WMH in five brain regions per hemisphere.
Statistical analysis
All statistical analyses were performed using SPSS (version 21.0; IBM Corporation, Armonk, NY, USA). The skewness and kurtosis of continuous variables, such as age, years of education, BMI, clusterin level, and MMSE score, were within −1 to 1. As skewness values for the plasma Aß1-40 and Aß1-42 levels and the Aß1-42/Aß1-40 ratio exceeded 3, we log transformed these variables for further analysis53. Independent two-sample t-tests and X2 tests were conducted to compare age, sex, BMI, neuropsychological test scores, plasma Aß and clusterin levels, MTA and PA scores, and ARWMC scores between controls and patients with AD and MCI. Pearson correlation analysis was conducted to study the relationships between plasma biomarkers and age, sex, education, disease duration, BMI, MMSE score, CDR-SB score, and visual rating scores. To explore the associations between plasma biomarkers and MTA, PA, MMSE, cognitive domain, and NPI subscales scores (dependent variables), we used plasma Aß and clusterin levels as independent variables. Age, education, sex, and ApoE4 genetic data were entered as covariates. To assess the relationships between visual rating scores and cognitive functions and neuropsychiatric symptoms, we used regression analysis with MTA and PA scores serving as independent variables, and MMSE, cognitive domain, CDR-SB, and NPI subscale scores serving as dependent variables. Age, education, sex, and ApoE4 genetic data were entered as covariates. Statistical significance was defined as p < 0.05. Post-hoc calculation of the statistical power achieved under the condition α = 0.05 was calculated using the G*Power program (http://gpower.hhu.de/).
References
Kalbe, E. et al. DemTect: a new, sensitive cognitive screening test to support the diagnosis of mild cognitive impairment and early dementia. International journal of geriatric psychiatry 19, 136–143, doi:10.1002/gps.1042 (2004).
Folstein, M. F., Folstein, S. E. & McHugh, P. R. “Mini-mental state”. A practical method for grading the cognitive state of patients for the clinician. Journal of psychiatric research 12, 189–198 (1975).
Woost, T. B. et al. Neural correlates of the DemTect in Alzheimer’s disease and frontotemporal lobar degeneration - A combined MRI & FDG-PET study. NeuroImage. Clinical 2, 746–758, doi:10.1016/j.nicl.2013.05.008 (2013).
Smits, L. L. et al. Regional atrophy is associated with impairment in distinct cognitive domains in Alzheimer’s disease. Alzheimer’s & dementia: the journal of the Alzheimer’s Association 10, S299–305, doi:10.1016/j.jalz.2013.06.007 (2014).
Hart, D. J. et al. A retrospective study of the behavioural and psychological symptoms of mid and late phase Alzheimer’s disease. International journal of geriatric psychiatry 18, 1037–1042, doi:10.1002/gps.1013 (2003).
Fuh, J. L., Wang, S. J. & Cummings, J. L. Neuropsychiatric profiles in patients with Alzheimer’s disease and vascular dementia. Journal of neurology, neurosurgery, and psychiatry 76, 1337–1341, doi:10.1136/jnnp.2004.056408 (2005).
Cummings, J. L. The Neuropsychiatric Inventory: assessing psychopathology in dementia patients. Neurology 48, S10–16 (1997).
Trzepacz, P. T. et al. Subscale validation of the neuropsychiatric inventory questionnaire: comparison of Alzheimer’s disease neuroimaging initiative and national Alzheimer’s coordinating center cohorts. The American journal of geriatric psychiatry: official journal of the American Association for Geriatric Psychiatry 21, 607–622, doi:10.1016/j.jagp.2012.10.027 (2013).
Robert, P. H. et al. Grouping for behavioral and psychological symptoms in dementia: clinical and biological aspects. Consensus paper of the European Alzheimer disease consortium. European psychiatry: the journal of the Association of European Psychiatrists 20, 490–496, doi:10.1016/j.eurpsy.2004.09.031 (2005).
Chen, C. S. et al. Apolipoprotein E polymorphism and behavioral and psychological symptoms of dementia in patients with Alzheimer disease. Alzheimer disease and associated disorders 26, 135–139, doi:10.1097/WAD.0b013e31821f5787 (2012).
Hsu, J. L. et al. Posterior Atrophy and Medial Temporal Atrophy Scores Are Associated with Different Symptoms in Patients with Alzheimer’s Disease and Mild Cognitive Impairment. PloS one 10, e0137121, doi:10.1371/journal.pone.0137121 (2015).
Bruen, P. D., McGeown, W. J., Shanks, M. F. & Venneri, A. Neuroanatomical correlates of neuropsychiatric symptoms in Alzheimer’s disease. Brain: a journal of neurology 131, 2455–2463, doi:10.1093/brain/awn151 (2008).
Logue, M. W. et al. Magnetic resonance imaging-measured atrophy and its relationship to cognitive functioning in vascular dementia and Alzheimer’s disease patients. Alzheimer’s & dementia: the journal of the Alzheimer’s Association 7, 493–500, doi:10.1016/j.jalz.2011.01.004 (2011).
Rafii, M. S. et al. Neuropsychiatric symptoms and regional neocortical atrophy in mild cognitive impairment and Alzheimer’s disease. American journal of Alzheimer’s disease and other dementias 29, 159–165, doi:10.1177/1533317513507373 (2014).
Kandiah, N., Chander, R., Zhang, A. & Yee, C. C. Cerebral white matter disease is independently associated with BPSD in Alzheimer’s disease. Journal of the neurological sciences 337, 162–166, doi:10.1016/j.jns.2013.11.042 (2014).
Blennow, K., Zetterberg, H. & Fagan, A. M. Fluid biomarkers in Alzheimer disease. Cold Spring Harbor perspectives in medicine 2, a006221, doi:10.1101/cshperspect.a006221 (2012).
Janelidze, S. et al. Plasma beta-amyloid in Alzheimer’s disease and vascular disease. Scientific reports 6, 26801, doi:10.1038/srep26801 (2016).
Mayeux, R. & Schupf, N. Blood-based biomarkers for Alzheimer’s disease: plasma Abeta40 and Abeta42, and genetic variants. Neurobiology of aging 32(Suppl 1), S10–19, doi:10.1016/j.neurobiolaging.2011.09.004 (2011).
Galozzi, S., Marcus, K. & Barkovits, K. Amyloid-beta as a biomarker for Alzheimer’s disease: quantification methods in body fluids. Expert Rev Proteomics 12, 343–354, doi:10.1586/14789450.2015.1065183 (2015).
Kaffashian, S. et al. Association of plasma beta-amyloid with MRI markers of structural brain aging the 3-City Dijon study. Neurobiology of aging 36, 2663–2670, doi:10.1016/j.neurobiolaging.2015.03.016 (2015).
Huang, C. W. et al. Potential blood biomarker for disease severity in the Taiwanese population with Alzheimer’s disease. American journal of Alzheimer’s disease and other dementias 28, 75–83, doi:10.1177/1533317512467674 (2013).
Gupta, V. B. et al. Plasma apolipoprotein J as a potential biomarker for Alzheimer’s disease: Australian Imaging, Biomarkers and Lifestyle study of aging. Alzheimer’s & dementia 3, 18–26, doi:10.1016/j.dadm.2015.12.001 (2016).
Mayeux, R. et al. Plasma A[beta]40 and A[beta]42 and Alzheimer’s disease: relation to age, mortality, and risk. Neurology 61, 1185–1190 (2003).
Mehta, P. D. et al. Plasma and cerebrospinal fluid levels of amyloid beta proteins 1–40 and 1–42 in Alzheimer disease. Archives of neurology 57, 100–105 (2000).
Lui, J. K. et al. Plasma amyloid-beta as a biomarker in Alzheimer’s disease: the AIBL study of aging. Journal of Alzheimer’s disease: JAD 20, 1233–1242, doi:10.3233/JAD-2010-090249 (2010).
Henriksen, K. et al. The future of blood-based biomarkers for Alzheimer’s disease. Alzheimer’s & dementia: the journal of the Alzheimer’s Association 10, 115–131, doi:10.1016/j.jalz.2013.01.013 (2014).
Kawarabayashi, T. & Shoji, M. Plasma biomarkers of Alzheimer’s disease. Curr Opin Psychiatry 21, 260–267, doi:10.1097/YCO.0b013e3282fc989f (2008).
Kleinschmidt, M. et al. Characterizing Aging, Mild Cognitive Impairment, and Dementia with Blood-Based Biomarkers and Neuropsychology. Journal of Alzheimer’s disease: JAD 50, 111–126, doi:10.3233/JAD-143189 (2015).
Fukumoto, H. et al. Age but not diagnosis is the main predictor of plasma amyloid beta-protein levels. Archives of neurology 60, 958–964, doi:10.1001/archneur.60.7.958 (2003).
Sotolongo-Grau, O. et al. Association between cell-bound blood amyloid-beta(1–40) levels and hippocampus volume. Alzheimer’s research & therapy 6, 56, doi:10.1186/s13195-014-0056-3 (2014).
Schrijvers, E. M., Koudstaal, P. J., Hofman, A. & Breteler, M. M. Plasma clusterin and the risk of Alzheimer disease. Jama 305, 1322–1326, doi:10.1001/jama.2011.381 (2011).
Dukic, L. et al. The role of human kallikrein 6, clusterin and adiponectin as potential blood biomarkers of dementia. Clinical biochemistry 49, 213–218, doi:10.1016/j.clinbiochem.2015.10.014 (2016).
Thambisetty, M. et al. Association of plasma clusterin concentration with severity, pathology, and progression in Alzheimer disease. Arch Gen Psychiatry 67, 739–748, doi:10.1001/archgenpsychiatry.2010.78 (2010).
Mukaetova-Ladinska, E. B. et al. Plasma and platelet clusterin ratio is altered in Alzheimer’s disease patients with distinct neuropsychiatric symptoms: findings from a pilot study. International journal of geriatric psychiatry 30, 368–375, doi:10.1002/gps.4145 (2015).
Song, F., Poljak, A., Smythe, G. A. & Sachdev, P. Plasma biomarkers for mild cognitive impairment and Alzheimer’s disease. Brain Res Rev 61, 69–80, doi:10.1016/j.brainresrev.2009.05.003 (2009).
Cammarata, S. et al. Amyloid-beta42 plasma levels are elevated in amnestic mild cognitive impairment. Journal of Alzheimer’s disease: JAD 18, 267–271, doi:10.3233/JAD-2009-1144 (2009).
Kleinschmidt, M. et al. Characterizing Aging, Mild Cognitive Impairment, and Dementia with Blood-Based Biomarkers and Neuropsychology. Journal of Alzheimer’s disease: JAD 50, 111–126, doi:10.3233/JAD-143189 (2016).
Meng, Y. et al. A correlativity study of plasma APL1beta28 and clusterin levels with MMSE/MoCA/CASI in aMCI patients. Scientific reports 5, 15546, doi:10.1038/srep15546 (2015).
Pandya, S. Y., Clem, M. A., Silva, L. M. & Woon, F. L. Does mild cognitive impairment always lead to dementia? A review. Journal of the neurological sciences 369, 57–62, doi:10.1016/j.jns.2016.07.055 (2016).
Metti, A. L. et al. The demographic and medical correlates of plasma abeta40 and abeta42. Alzheimer disease and associated disorders 27, 244–249, doi:10.1097/WAD.0b013e318260a8cb (2013).
Roher, A. E. et al. Amyloid beta peptides in human plasma and tissues and their significance for Alzheimer’s disease. Alzheimer’s & dementia: the journal of the Alzheimer’s Association 5, 18–29, doi:10.1016/j.jalz.2008.10.004 (2009).
McKhann, G. M. et al. The diagnosis of dementia due to Alzheimer’s disease: recommendations from the National Institute on Aging-Alzheimer’s Association workgroups on diagnostic guidelines for Alzheimer’s disease. Alzheimer’s & dementia: the journal of the Alzheimer’s Association 7, 263–269, doi:10.1016/j.jalz.2011.03.005 (2011).
Liao, Y. C. et al. ABCA7 gene and the risk of Alzheimer’s disease in Han Chinese in Taiwan. Neurobiology of aging 35, 2423 e2427–2423 e2413, doi:10.1016/j.neurobiolaging.2014.05.009 (2014).
Hughes, C. P., Berg, L., Danziger, W. L., Coben, L. A. & Martin, R. L. A new clinical scale for the staging of dementia. The British journal of psychiatry: the journal of mental science 140, 566–572 (1982).
Vanderploeg, R. D. et al. Elderly norms for the Hopkins Verbal Learning Test-Revised. The Clinical neuropsychologist 14, 318–324, doi:10.1076/1385-4046(200008)14:3;1-P;FT318 (2000).
Mack, W. J., Freed, D. M., Williams, B. W. & Henderson, V. W. Boston Naming Test: shortened versions for use in Alzheimer’s disease. Journal of gerontology 47, P154–158 (1992).
Barr, A. & Brandt, J. Word-list generation deficits in dementia. Journal of clinical and experimental neuropsychology 18, 810–822, doi:10.1080/01688639608408304 (1996).
Wechsler, D. Wechsler Adult Intelligence Scale-Third Edition. (The Pshchological Corporation, 1997).
Fuh, J. L., Liu, C. K., Mega, M. S., Wang, S. J. & Cummings, J. L. Behavioral disorders and caregivers’ reaction in Taiwanese patients with Alzheimer’s disease. International psychogeriatrics/IPA 13, 121–128 (2001).
Scheltens, P. et al. Atrophy of medial temporal lobes on MRI in “probable” Alzheimer’s disease and normal ageing: diagnostic value and neuropsychological correlates. Journal of neurology, neurosurgery, and psychiatry 55, 967–972 (1992).
Koedam, E. L. et al. Visual assessment of posterior atrophy development of a MRI rating scale. European radiology 21, 2618–2625, doi:10.1007/s00330-011-2205-4 (2011).
Wahlund, L. O. et al. A new rating scale for age-related white matter changes applicable to MRI and CT. Stroke; a journal of cerebral circulation 32, 1318–1322 (2001).
Munro, B. H. Statistical Methods for Health Care Research. 4th edn, 42–46 (Lippincott, 2001).
Acknowledgements
The study was supported by grants from Academia Sinica of Taiwan (Taiwan Biobank: Biosignature study of Alzheimer disease); the Ministry of Science and Technology of Taiwan (104-2314-B-075 -005 -MY2, 104-2745-B-075 -001 -, 106-2321-B-075-001-); Taipei Veterans General Hospital (V105C-110, V105E9-001-MY2-1), the Ministry of Science and Technology support for the Centre for Dynamical Biomarkers and Translational Medicine, National Central University, Taiwan (MOST 103-2911-I-008-001); the Brain Research Center, National Yang-Ming University; and the Ministry of Education Aim for the Top University Plan.
Author information
Authors and Affiliations
Contributions
J.L.H. was the physician for the ideal generation, study conception and design, and drafted manuscript. W.J.L., Y.C.L., J.F.L. and J.L.F. contributed to recruit cases, study preparation, the interpretation of the results, and manuscript preparation. S.J.W. and J.L.F. involved in grants application and revised the manuscript. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Competing Interests
The authors declare that they have no competing interests.
Additional information
Publisher's note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Hsu, JL., Lee, WJ., Liao, YC. et al. Plasma biomarkers are associated with agitation and regional brain atrophy in Alzheimer’s disease. Sci Rep 7, 5035 (2017). https://doi.org/10.1038/s41598-017-05390-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-017-05390-1
This article is cited by
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.