Abstract
This study evaluated the impact of calcium and magnesium on the in vitro degradation and in vivo clearance of oxaliplatin. Intact oxaliplatin and Pt(DACH)Cl2 were measured in incubation solutions by HPLC-UV. A clinical study determined changes in plasma concentrations of calcium and magnesium in cancer patients and their impact on oxaliplatin clearance. Kinetic analyses modelled oxaliplatin degradation reactions in vitro and contributions to oxaliplatin clearance in vivo. Calcium and magnesium accelerated oxaliplatin degradation to Pt(DACH)Cl2 in chloride-containing solutions in vitro. Kinetic models based on calcium and magnesium binding to a monochloro-monooxalato ring-opened anionic oxaliplatin intermediate fitted the in vitro degradation time-course data. In cancer patients, calcium and magnesium plasma concentrations varied and were increased by giving calcium gluconate and magnesium sulfate infusions, but did not alter or correlate with oxaliplatin clearance. The intrinsic in vitro clearance of oxaliplatin attributed to chloride-, calcium- and magnesium-mediated degradation predicted contributions of <2.5% to the total in vivo clearance of oxaliplatin. In conclusion, calcium and magnesium accelerate the in vitro degradation of oxaliplatin by binding to a monochloro-monooxalato ring-opened anionic intermediate. Kinetic analysis of in vitro oxaliplatin stability data can be used for in vitro prediction of potential effects on oxaliplatin clearance in vivo.
Similar content being viewed by others
Introduction
Calcium and magnesium have been implicated in the mechanism and clinical prevention of oxaliplatin-induced neurotoxicity. Oxaliplatin (((1 R,2 R)-cyclohexane-1,2-diamine)(ethanedioato-O,O’)platinum(II)) is an important anticancer drug for the treatment of many cancers of the gastrointestinal tract1,2,3,4,5,6,7,8. It, in combination with a fluoropyrimidine, has become the standard chemotherapy for colorectal cancer in both adjuvant and palliative settings1, 4,5,6,7. However, its neurotoxicity is a major treatment-limiting adverse effect resulting in a dose reduction or early termination of the drug treatment and long term toxicity that may adversely affect patient’s quality of life for many months to years9. Clinically, most patients undergoing oxaliplatin therapy typically experience cold-induced peripheral paraesthesia, and some experience muscle cramps, throat or jaw tightness, and pharyngolaryngeal dysesthesia immediately after the oxaliplatin infusion9. Abnormal spontaneous high-frequency motor unit action potentials are detectable on electromyography, reflecting hyper-excitability of these peripheral nerves10,11,12. The mechanism of this acute neurotoxicity of oxaliplatin has been proposed to be related to the prolonged opening of calcium-dependent voltage-gated sodium channels resulting from chelation of calcium by oxalate13,14,15,16. The prolonged opening of these sodium channels may induce cellular stress, which in addition to the accumulation of platinum compounds in the dorsal root ganglial cells, may cause damage to cell body and axon17,18,19, and contribute to the development of chronic peripheral sensory neurotoxicity of oxaliplatin. It has also been suggested that oxaliplatin and/or its metabolites may increase calcium influx into the cytosol of peripheral neurons, which in turn may enhance the activation of sodium and potassium channels, calcium regulated transcription factors and intracellular signalling involving calcium-dependent protein kinases20, 21. On the basis of a retrospective clinical study suggesting neuroprotective effects of calcium gluconate and magnesium sulfate (CaGluc/MgSO4) infusions given concurrently with oxaliplatin therapy22 and supporting preclinical data23, these infusions became routinely used without further confirmatory prospective randomised trials or evaluation of any potential pharmacokinetic interactions with oxaliplatin. Since 2013, after two prospective randomised trials definitively showing a lack of neuroprotective effects of these infusions against both acute and chronic forms of oxaliplatin neurotoxicity24, 25, they are now commonly omitted from the routine clinical practice26.
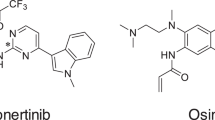
The potential impact of calcium and magnesium on the in vitro degradation and in vivo clearance of oxaliplatin was previously unknown. Once administered oxaliplatin has been proposed to undergo rapid non-enzymatic biotransformation reactions with water and nucleophiles such as chloride, methionine and glutathione27,28,29. It is not known to be subject to CYP-P450 mediated metabolism. The initial reaction in oxaliplatin biotransformation can involve displacement of the oxalate group by water and chloride, resulting in formation of reactive species such as monochloro-, dichloro-, and diaquo-DACH platinum, where DACH is the common abbreviation for cyclohexane-1,2-diamine29. Initial degradation of oxaliplatin in the presence of chloride in vitro was previously suggested to lead to formation of an intermediate species, monochloro-monooxalato ring-opened complex, [Pt(DACH)oxCl]− 30 (Fig. 1). This complex can convert back to oxaliplatin or transform into the final product, Pt(DACH)Cl2, resulting in overall slow degradation of oxaliplatin. The contributions made by these different ligand displacement reactions to the in vivo clearance of oxaliplatin are not well understood. To date, there have been few previous attempts to apply in vitro – in vivo extrapolation methods to predicting effects on the in vivo clearance of oxaliplatin. In drug discovery, techniques for predicting in vivo clearance of drugs using in vitro drug metabolism kinetic data has been used, particularly in vitro hepatocyte or microsomal metabolic stability kinetic data for predicting hepatic clearance of drugs in vivo 31, 32. For drugs, such as oxaliplatin, that are not metabolised by the liver, there is little literature available about the prediction of in vivo clearance using in vitro kinetic data.
With this background, we sought to evaluate the potential impact of calcium and magnesium on the in vitro degradation and the in vivo clearance of oxaliplatin. Drug stability studies and kinetic modelling were used to explore reactions of oxaliplatin and its degradation products with calcium and magnesium in vitro. A clinical study was undertaken to determine changes in plasma concentrations of calcium and magnesium in cancer patients given oxaliplatin with or without infusions of calcium gluconate and magnesium sulfate, and their impact on oxaliplatin clearance. These in vitro and clinical datasets provided an opportunity to develop and exemplify experimental approaches for prediction of effects on oxaliplatin clearance in vivo from oxaliplatin stability data generated in vitro.
Results
In vitro degradation of oxaliplatin
To evaluate the potential impact of calcium and magnesium on the in vitro degradation of oxaliplatin, oxaliplatin was incubated in water and solutions containing NaCl, CaCl2 and MgCl2 at 37 °C for 8 hours. Incubation samples were collected and analysed using a validated HPLC-UV method33 to determine oxaliplatin and Pt(DACH)Cl2 concentrations at pre-defined time points over the incubation period. Data were presented as plots of concentration versus time and the mass balance of the reaction (Fig. 2). Oxaliplatin was unstable in the presence of chloride and degraded to Pt(DACH)Cl2 via an intermediate species (Fig. 1), as previously shown by Jerremalm et al.30 who had identified the intermediate to be [Pt(DACH)oxCl]−. In contrast, oxaliplatin remained stable in water (Fig. 2). The rate of oxaliplatin degradation to Pt(DACH)Cl2 was accelerated in the presence of calcium and magnesium ions in association with higher transient formation of the intermediate species than was observed in NaCl.
Time-course and mass balance analysis of oxaliplatin degradation in (A) water, (B) 150 mM NaCl, (C) 75 mM CaCl2, and (D) 75 mM MgCl2 solutions under physiological conditions (pH 7.3; 37 °C). Oxaliplatin was unstable in chloride containing solutions in contrast to its stability in water. Oxaliplatin degradation was accelerated in the presence of calcium and magnesium. Red: Intact oxaliplatin. Yellow: intermediate. Green: Pt(DACH)Cl2. Data points represent the mean of independent replicate measured values. The lines represent kinetic models shown in the text whose rate constants are shown in Table 1.
Kinetic analysis of in vitro degradation
The kinetic model proposed by Jerremalm et al.29, 30 for the stepwise reaction of oxaliplatin with chloride, comprising of a reversible first step producing [Pt(DACH)oxCl]− followed by an irreversible second step producing Pt(DACH)Cl2 (Fig. 1), was fitted to the mean measured concentration values obtained at time points during the in vitro degradation studies. Rate constants (Table 1) were obtained by least-squares fitting to the analytical expressions shown below (Equations (1–5) for the reaction scheme in Fig. 1 to the three species simultaneously34. Standard errors for the rate constants were derived from a Jack-knife procedure35.
The parameters λ1 and λ2 are the observed biexponential decay constants, and are combinations of the rate constant for oxalate ring opening k1, the rate constant for ring closing k−1, and the rate constant for oxalate loss k2. The kinetic models fitted the experimental data for all conditions (Fig. 2). Addition of CaCl2 or MgCl2 increased the observed rate of degradation of oxaliplatin and caused increased amounts of the intermediate species to form. However, analysis of the data showed that the k1 rate constants for the oxalate ring opening step in the oxaliplatin degradation reaction were similar in 150 mM NaCl, 75 mM CaCl2 and 75 mM MgCl2, while the k−1 rate constants for the back reaction corresponding to oxalate chelate ring closing and reformation of oxaliplatin from the [Pt(DACH)oxCl]− intermediate were decreased in 75 mM CaCl2 and 75 mM MgCl2 as compared to 150 mM NaCl. Finally, the values for the k2 rate constant for the loss of the monodentate oxalate ligand from [Pt(DACH)oxCl]− leading to formation of Pt(DACH)Cl2 were increased in 75 mM CaCl2 and 75 mM MgCl2 as compared to 150 mM NaCl. Thus, the observed increase in degradation is not due to an increased rate of the initial oxalate ring opening, but rather is due to a combination of a decrease in the reverse rate of oxalate ring closure combined with an increase in the rate of loss of oxalate.
These findings suggested that calcium and magnesium did not interact significantly with oxaliplatin at the concentrations studied, but bound to the monodentate oxalate-containing complex [Pt(DACH)oxCl]−, and in doing so, decreased the rate of oxalate ring closure and increased the rate of loss of oxalate from the ring-opened intermediate. The kinetics of the reaction mechanism were therefore modelled further by including an additional metal bonded intermediate species as shown in the shaded area of Fig. 1. With the assumption that the rate constant for the reformation of oxaliplatin from the metal bonded intermediate (k−1,M) was zero, then the calculated values of the equilibrium constant (K) for the reversible conversion of [Pt(DACH)oxCl]− to the metal bonded intermediate were 20 M−1 for Ca2+ and 30 M−1 for Mg2+. If k−1,M was not zero then the equilibrium constants would be higher. These equilibrium constant values indicate that in 75 mM CaCl2 or MgCl2 60% or 70% respectively of the [Pt(DACH)oxCl]− is ion-paired with the metal. Using these equilibrium constant values, the values of the rate constant for the conversion of the metal bonded intermediate to Pt(DACH)Cl2 (k2,M) were calculated to be 3.3 hr−1 and 1.5 hr−1 for calcium and magnesium, respectively.
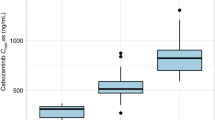
Plasma calcium and magnesium concentrations after CaGluc/MgSO4 infusions in patients
The in vitro findings described above suggested that calcium and magnesium may alter the in vivo clearance of oxaliplatin by accelerating its degradation via binding to [Pt(DACH)oxCl]−. Plasma calcium and magnesium concentrations vary between patients, on different occasions, and are altered in the presence of cancer, associated disease processes and treatments36, 37. Until recently, CaGluc/MgSO4 infusions had been routinely given concurrently with oxaliplatin for the purpose of limiting neurotoxicity26 but their effects on oxaliplatin clearance or plasma calcium and magnesium levels had not been well studied. In a randomised placebo-controlled crossover clinical study, we sought to understand how variation in plasma calcium and magnesium concentrations, and the administration of CaGluc/MgSO4 infusions, influenced oxaliplatin clearance in cancer patients receiving chemotherapy, by measuring plasma concentrations of calcium and magnesium before and after CaGluc/MgSO4 and placebo infusions given with oxaliplatin. We previously reported that oxaliplatin clearance was not altered by giving CaGluc/MgSO4 infusions24. The mean oxaliplatin clearance was 35.3 L/hr (SD 9.8) with CaGluc/MgSO4 infusions and 33.6 L/hr (7.7) with placebo infusions (p = 0.17). Here we report that plasma concentrations of calcium and magnesium were significantly higher after the first CaGluc/MgSO4 infusions than at baseline (calcium 1.04-fold increase, p < 0.001; magnesium 1.2-fold increase, p < 0.001) (Fig. 3). Plasma calcium concentration had returned to near baseline levels immediately prior to the second CaGluc/MgSO4 infusion two hours later but increased again after the second infusion (1.09-fold increase, p < 0.001). Plasma magnesium concentration, however, remained significantly higher (1.13-fold increase, p < 0.001) than baseline when the second infusion was due and were increased further following the second infusion (1.5-fold increase, p < 0.001). There were no significant changes in plasma calcium and magnesium levels after the placebo infusions.
Plasma calcium (A,B) and magnesium (C,D) concentrations in colorectal cancer patients measured before and after CaGluc/MgSO4 (red) or placebo (blue) infusions given with oxaliplatin chemotherapy. “Pre” and “post”refer to the timing of the plasma calcium and magnesium measurements before or after the CaGluc/MgSO4 infusions. The p values shown as p < 0.0001 are for a comparison of measurements determined with CaGluc/MgSO4 versus placebo infusions using repeated measures one way ANOVA, and those shown as *** (p < 0.001) or NS (not significant) are from Tukey’s multiple comparison test. Plasma calcium and magnesium concentrations were increased after CaGluc/MgSO4 infusions but not after placebo infusions. CaGluc/MgSO4: calcium gluconate/magnesium sulfate infusions.
Oxaliplatin clearance values measured on treatment cycles given with CaGluc/MgSO4 or placebo infusions were plotted against their corresponding maximal plasma calcium and magnesium levels for each study patient (Fig. 4). Maximum plasma concentrations of calcium and magnesium were within normal limits after placebo infusions. After CaGluc/MgSO4 infusions, however, maximum plasma levels exceeded the upper limit of normal in 4 (21%) and 19 (100%) patients for calcium and magnesium, respectively. According to Common Toxicity Criteria Adverse Effect version 4.0 grading, elevated plasma calcium were severity grade 1 in 3 patients (16%) and grade 2 in 1 patient (5%), while elevated plasma magnesium was severity grade 1 in 12 patients (63%) and grade 3 in 7 patients (37%). Pearson co-efficient correlation analysis showed that oxaliplatin clearance did not correlate with plasma calcium (p = 0.33) or magnesium (p = 0.60) concentrations.
Correlation plots of oxaliplatin clearance versus plasma calcium (A) and magnesium (B) concentrations in colorectal cancer patients. Patients (n = 19) received CaGluc/MgSO4 and placebo infusions on alternate cycles of oxaliplatin treatment in random order, during which oxaliplatin clearance and plasma calcium and magnesium levels were measured. Data points represent oxaliplatin clearance values and the maximal plasma calcium and magnesium concentrations achieved during the placebo (blue) and CaGluc/MgSO4 infusion cycle (red) for each patient. Oxaliplatin clearance did not correlate with plasma calcium or magnesium concentrations (correlation coefficient = −0.38; r2 = 0.14; and p = 0.11). Vertical lines show Common Toxicity Criteria Adverse Event (CTCAE) severity gradings for hypercalcaemia and hypermagnesaemia. ULN: upper limit of normal.
In vitro Prediction of calcium-, magnesium- and chloride- mediated clearance of oxaliplatin
To estimate potential contributions of calcium-, magnesium- and chloride-mediated degradation to the in vivo clearance of oxaliplatin in patients, an in vitro – in vivo extrapolation method was developed. First, the in vitro intrinsic clearances of oxaliplatin attributable to calcium-, magnesium- and chloride-mediated degradation were calculated. Non-compartmental analysis was used to calculate the AUC0−infinity for oxaliplatin concentration versus time for each experimental condition. Then the total in vitro clearance of oxaliplatin for each condition was obtained by dividing the amount of oxaliplatin added to the solution per unit volume by the AUC0−infinity. Oxaliplatin clearance attributable to calcium- or magnesium- mediated degradation was then calculated by subtracting the clearance attributable to chloride from the total in vitro clearance value for the relevant experimental condition. Calculated values for oxaliplatin clearance attributable to chloride, calcium and magnesium were then plotted against the concentrations of the relevant ion in the incubation solution and analysed by linear regression. The in vitro intrinsic clearance attributable to chloride, calcium and magnesium was taken from the slope of the linear regression fit to its data as shown in Table 2 and Supplementary Figure. These data were then scaled to the in vivo setting by calculating the total extracellular fluid (ECF) content of calcium, magnesium and chloride from estimates of ECF volume and measured plasma concentrations of these ions in patients from our clinical study. In vivo clearance predictions were then made by multiplying the in vitro intrinsic clearance value by the calculated ECF content value of each ion.
The in vitro intrinsic clearance of oxaliplatin attributable to calcium-, magnesium- and chloride-mediated degradation was calculated to be 0.0039, 0.0023 and 0.00037 L/hr/mmol, respectively (Table 3). The predicted in vivo oxaliplatin clearances attributable to calcium, magnesium and chloride were 0.15 L/hr, 0.03 L/hr and 0.68 L/hr, respectively, before CaGluc/MgSO4 infusions. After the CaGluc/MgSO4 infusion, these predicted in vivo oxaliplatin clearance values increased slightly to 0.16 L/hr for calcium and 0.05 L/hr for magnesium but remained unchanged for chloride. The combined oxaliplatin clearance attributable to the sum of calcium-, magnesium- and chloride-mediated degradation was predicted to be 0.86 and 0.89 L/hr before and after CaGluc/MgSO4 infusions, respectively. Considering the total in vivo clearance of oxaliplatin measured in our clinical study (35.3 L/hr), calcium-, magnesium- and chloride-mediated degradation was predicted to account for less than 2.5% of the total clearance of oxaliplatin in vivo.
Discussion
This study showed that calcium and magnesium accelerate oxaliplatin degradation by binding to the monochloro-monooxalato ring-opened anionic oxaliplatin intermediate, [Pt(DACH)oxCl]−, that forms in chloride-containing physiological solutions in vitro. To our knowledge, calcium and magnesium have not been previously reported to alter oxaliplatin degradation or bind to its degradation intermediates. We showed that the in vitro degradation of oxaliplatin to Pt(DACH)Cl2 was faster in the presence of calcium and magnesium by directly quantifying both intact oxaliplatin and Pt(DACH)Cl2 using HPLC-UV. Mass balance analysis revealed a deficit after accounting for these two compounds consistent with the transient formation of an intermediate species. Further evidence came from kinetic analyses and rate constants calculated for the reaction scheme in Fig. 1 suggesting that calcium and magnesium interacted with the oxalate ring-opened anionic oxaliplatin intermediate, [Pt(DACH)oxCl]−, resulting in a decreased rate of oxalate ring closure, and an increased loss of monodentate oxalate leading to formation of Pt(DACH)Cl2. Oxaliplatin was unstable in the presence of chloride as previous reported by Jerremalm et al.30 but our findings also provide a mechanism of how calcium and magnesium influence this process of oxaliplatin degradation. This new information may have important implications for understanding how oxaliplatin behaves under in vivo conditions when other reactants or cations are present.
This current study provides a new experimental approach for predicting effects on the in vivo clearance of oxaliplatin from in vitro studies of oxaliplatin degradation. It is, to our best knowledge, the first time that in vitro – in vivo extrapolation methods have been applied to predicting effects on oxaliplatin clearance. The concept was based on methods which are already established for in vitro - in vivo prediction of drug clearance mediated by hepatic microsomal metabolism by CYP-P450 and other enzymes, and which are commonly used in pre-clinical studies of the metabolic stability of new chemical entities32. However, oxaliplatin is not subject to hepatic metabolism, but degrades via leaving group displacement reactions, although little is known about their contributions to the in vivo clearance of oxaliplatin. To estimate effects on the in vivo clearance of oxaliplatin, we first obtained experimentally determined values for the in vitro intrinsic clearance of oxaliplatin attributable to calcium-, magnesium- and chloride-mediated oxaliplatin degradation, calculated from kinetic analyses of in vitro oxaliplatin stability data. Then, scaling factors were used to estimate the contributions of these processes to the in vivo clearance of oxaliplatin. This experimental approach has potential for providing new insights into mechanisms of oxaliplatin clearance. Previously, for example, it was suggested that oxaliplatin may initially react with water or chloride during its in vivo biotransformation28, 29. However, we found oxaliplatin to be stable in water in vitro, and that chloride-mediated oxaliplatin degradation was predicted to contribute only 1.9% to the total in vivo clearance of oxaliplatin. This stability of oxaliplatin in pure water or in chloride may be due to slow oxalate ring opening and/or fast oxalate ring closing. These findings suggest that oxaliplatin degradation mediated only by water or chloride may contribute less than previously thought to the total clearance of oxaliplatin in vivo, as suggested by a low formation of Pt(DACH)Cl2 from oxaliplatin under in vivo conditions24, 38.
In cancer patients receiving oxaliplatin chemotherapy, we found that plasma calcium and magnesium concentrations were increased significantly after the infusions of calcium gluconate and magnesium sulfate given immediately before and after oxaliplatin chemotherapy. These infusions were, until recently, routinely used in the clinic for the purpose of reducing neurotoxicity. Statistically significant increases in plasma calcium and magnesium occurred following each of the two CaGluc/MgSO4 infusions. Post-infusion elevations in plasma calcium were CTCAE severity grade 1 in three patients and grade 2 in one patient, while elevations in plasma magnesium were CTCAE grade 1 in twelve patients and grade 3 in seven patients. There has not been a previous study, which we are aware of, showing these effects on plasma calcium and magnesium levels in patients immediately or soon after these infusions prior to this current study. In our study, plasma calcium and magnesium levels were measured only at baseline, 20 minutes after the first CaGluc/MgSO4 infusions and immediately after the second CaGluc/MgSO4 infusion. We did not fully evaluate the time-course, duration, extent or clinical safety concerns related to these treatment-associated elevations in plasma calcium and magnesium levels. Previously, Gamelin et al.39 reported no difference in plasma calcium and magnesium levels after the end of oxaliplatin infusion given without CaGluc/MgSO4 infusions. Their reported values were very similar to those found in the current study at baseline or after placebo infusions. This clinical study also provided an opportunity to explore potential relationships between plasma calcium and magnesium levels and the clearance of oxaliplatin. Plasma calcium and magnesium varied widely between different patients and treatment cycles but did not correlate with oxaliplatin clearance. This finding was in keeping with the in vitro prediction that calcium- and magnesium-mediated degradation contributed a relative small amount (<2.5%) to the total in vivo clearance of oxaliplatin.
The method we describe for the in vitro prediction of effects on the in vivo clearance of oxaliplatin could assist with translating new treatments to clinical evaluation for preventing oxaliplatin neurotoxicity. Many new candidate treatments for preventing neurotoxicity of oxaliplatin are being identified by preclinical studies, for example, L-type calcium channel blockers20 and calcium/calmodulin-dependent kinase inhibitors21. Our method could identify the potential for deleterious pharmacokinetic interactions with oxaliplatin prior to clinical studies. In this way, this in vitro assessment will complement trial design and endpoints we recently proposed for the early clinical evaluation of investigational treatments for preventing oxaliplatin neurotoxicity40.
In conclusion, calcium and magnesium accelerate the in vitro degradation of oxaliplatin by binding to a monochloro-monooxalato ring-opened anionic intermediate. Kinetic analyses of in vitro oxaliplatin stability data predicted the contributions of calcium-, magnesium- and chloride-mediated degradation to the total in vivo clearance of oxaliplatin in patients. In vitro-in vivo extrapolation methods can be used in future studies for the in vitro prediction of potential effects on oxaliplatin clearance in vivo.
Materials and Methods
In vitro incubation studies
Oxaliplatin and Pt(DACH)Cl2 were obtained from Sigma-Aldrich (St Louis, MO, USA). Hydroxyethylpiperazine-N’-2-ethane sulfonic acid (‘HEPES’) was obtained from Gibco-BRL Life Technologies (Grand Island, NY, USA). Powder sodium chloride (NaCl) and magnesium chloride (MgCl2) anhydrous were obtained from Sigma Aldrich (St Louis, MO, USA). Calcium chloride (CaCl2) was obtained from Riedel-de Haen AG (Germany). Methanol of chromatographic grade, triflic acid (98% reagent grade) was obtained from Sigma Aldrich (St Louis, MO, USA). All solutions and mobile phase were prepared using Milli-Q grade water (Millipore, Bedford, USA).
To study the stability of oxaliplatin in the presence of chloride, calcium and magnesium under physiological conditions, oxaliplatin (100 μM prepared in Milli-Q water) was incubated in water alone, NaCl (15, 50, and 150 mM), CaCl2 (1.8, 37.5 and 75 mM), and MgCl2 (1.8, 37.5 and 75 mM) in HEPES buffer at pH 7.3 and 37 °C. A temperature regulated water-bath (Julabo TW12, John Morris Scientific Ltd., Auckland) was used to maintain temperature during incubation. Samples for analysis were taken at 0, 5, 10, 20, 30, and 60 minutes then hourly thereafter until 8 hours. To detect oxaliplatin and its degradation product, Pt(DACH)Cl2, these incubation samples were analysed using a Hewlett Packard HP1200 HPLC online system. This included a binary pump, a degasser and an autosampler (Wilmington, DE, USA), a Waters µBondapak C18 3.9 × 300 mm column (Waters, Massachusetts, USA) with a guard column (Phenomenex, Torrance, LA, USA). The UV detector used was Millipore Waters Lambda-max model 480 LC Spectrophometer (Millipore, Land Cove, Australia). The HPLC separations were performed at room temperature using a mobile phase containing 3% methanol in Milli-Q water (adjusted to pH 2.5 with triflic acid). The flow rate was 0.5 mL/min. The UV wavelength monitored was 210 nm with a reference of 550 nm. The injection volume of all samples was 50 µL. Data acquisition and processing were performed using HP4500 ChemStation and HP1200 Agilent ChemStation offline software B.04.01 (Agilent Technologies, Avodale, USA). The samples were analysed immediately after they were taken from the incubation solutions whenever possible, otherwise they were snap frozen using liquid nitrogen and thawed within a minute before being injected onto the HPLC for analysis to avoid continuation of degradation of oxaliplatin at higher temperatures. All samples from each incubation study were analysed on the same day using the same mobile phase. Concentrations of oxaliplatin and Pt(DACH)Cl2 were determined by using their respective calibration curves to convert the areas under the chromatographic peaks to concentration values. The concentrations of the intermediate species were estimated from a mass balance after accounting for oxaliplatin and Pt(DACH)Cl2. The kinetics of degradation reactions were modelled as described below.
Clinical study
In our previously reported clinical study24, a randomised double-blind placebo-controlled design was used to evaluate the effects of calcium gluconate (1 g) and magnesium sulfate (1 g) (CaGluc/MgSO4) infusions on the pharmacokinetics and acute neurotoxicity of oxaliplatin. Each patient undergoing oxaliplatin chemotherapy was given either CaGluc/MgSO4 or placebo infusions immediately before and after oxaliplatin infusion on cycle 1 then the opposite study infusion on cycle 2. This study was approved by the Northern Y Regional Ethics Committee (approval number NTY/11/01/005) and was conducted in accordance with its guidelines and regulations. Informed consent was obtained from all study participants. The plasma pharmacokinetic samples were collected at 13 predefined times including at baseline, during and 3 hours post oxaliplatin infusion. The samples used for this current study were taken at baseline, 20 minutes post first CaGluc/MgSO4 or placebo infusion, immediately prior and post second CaGluc/MgSO4 or placebo infusions. The plasma was immediately prepared by centrifugation at 4 °C and 5000 G for 5 minutes, then snap-frozen using liquid nitrogen. The samples were stored at −80 °C until analysis. Plasma calcium (albumin adjusted) and magnesium concentrations were measured using Cobas 8000 modular analyser (Roche Diagnostics Ltd., Switzerland) at LabPlus, Auckland City Hospital (Auckland, New Zealand). Data were presented as measured values and the levels of calcium and magnesium were graded using Common Toxicity Criteria Adverse Effect (CTCAE) version 4. Plasma calcium and magnesium concentrations were compared between baseline and post CaGluc/MgSO4 or placebo infusions by repeated measures one-way ANOVA analysis. Correlation between calcium and magnesium concentrations and observed oxaliplatin clearance for each patient obtained from our previous study24 was assessed by Pearson correlation analysis. All statistical analyses were performed using PRISM 6, GraphPad, San Diego, USA.
Kinetic modelling
Kinetic analysis of oxaliplatin reactivity in the presence of calcium and magnesium was done using the mean concentration values for oxaliplatin and Pt(DACH)Cl2 at each sampling time. Rate constants were obtained by least-square fitting the analytical expressions for the reaction scheme to the three species simultaneously (Fig. 1 – unshaded area), using the Solver function in Microsoft Excel with the three rate constants k1, k−1, and k2 as adjustable parameters. Estimates of the standard errors for these parameters were then obtained using a Jack-knife procedure.
To determine in vitro intrinsic clearance of oxaliplatin attributable to chloride-, calcium- and magnesium-mediated degradation, the following steps were undertaken: (1) AUC0−infinity for oxaliplatin concentration versus time for each in vitro incubation experimental condition was calculated using non-compartmental analysis; (2) total in vitro clearance of oxaliplatin for each condition was calculated by dividing the amount of oxaliplatin in the incubation solution per unit volume by the corresponding AUC0−infinity; (3) oxaliplatin clearance attributable to calcium- and magnesium-mediated degradation was calculated by subtracting the clearance attributable to chloride from the total in vitro clearance value for each condition; (4) calculated values for oxaliplatin clearance attributable to these ions were then plotted against the concentrations of the corresponding ions in the incubation solution and analysed by linear regression; and (5) finally, the in vitro intrinsic clearance attributable to chloride, calcium and magnesium was taken from the slope of the linear regression fit to its data (Table 2 and Supplementary Figure).
To extrapolate in vitro kinetic data from the incubation studies to in vivo oxaliplatin clearance attributable to plasma chloride, calcium and magnesium, a scaling factor was applied to the calculated intrinsic clearance for each of chloride, calcium and magnesium ions. The approach to scaling used in our study was a modified version of those used in the microsomal in vitro-in vivo extrapolation methods32. We used the estimated extracellular fluid (ECF) contents of chloride, calcium and magnesium in each patient. First, total body water was estimated as 60% of body weight in men and 50% in women, and the ECF volume was estimated as 40% of total body water. The ECF content of chloride, calcium and magnesium was then calculated by multiplying the measured plasma concentrations of these ions by the estimated ECF volume in each patient. Finally, in vivo clearance of oxaliplatin mediated by each of chloride, calcium and magnesium was calculated using the following formula: in vivo CL = in vitro CLint x ECF content, where units for CL = L/h; CLint = L/h/mmol; and ECF content = mmol).
References
Andre, T. et al. Improved overall survival with oxaliplatin, fluorouracil, and leucovorin as adjuvant treatment in stage II or III colon cancer in the MOSAIC trial. J Clin Oncol 27, 3109–16 (2009).
Conroy, T. et al. FOLFIRINOX versus gemcitabine for metastatic pancreatic cancer. N Engl J Med 364, 1817–25 (2011).
Cunningham, D. et al. Capecitabine and oxaliplatin for advanced esophagogastric cancer. N Engl J Med 358, 36–46 (2008).
de Gramont, A. et al. Leucovorin and fluorouracil with or without oxaliplatin as first-line treatment in advanced colorectal cancer. J Clin Oncol 18, 2938–47 (2000).
Haller, D. G. et al. Capecitabine plus oxaliplatin compared with fluorouracil and folinic acid as adjuvant therapy for stage III colon cancer. J Clin Oncol 29, 1465–71 (2011).
Kuebler, J. P. et al. Oxaliplatin combined with weekly bolus fluorouracil and leucovorin as surgical adjuvant chemotherapy for stage II and III colon cancer: results from NSABP C-07. J Clin Oncol 25, 2198–204 (2007).
Rothenberg, M. L. et al. Superiority of oxaliplatin and fluorouracil-leucovorin compared with either therapy alone in patients with progressive colorectal cancer after irinotecan and fluorouracil-leucovorin: interim results of a phase III trial. J Clin Oncol 21, 2059–69 (2003).
Yothers, G. et al. Oxaliplatin as adjuvant therapy for colon cancer: updated results of NSABP C-07 trial, including survival and subset analyses. J Clin Oncol 29, 3768–74 (2011).
Grothey, A. Oxaliplatin-safety profile: neurotoxicity. Semin Oncol 30, 5–13 (2003).
Hill, A. et al. Detecting acute neurotoxicity during platinum chemotherapy by neurophysiological assessment of motor nerve hyperexcitability. BMC Cancer 10, 451 (2010).
Lehky, T. J., Leonard, G. D., Wilson, R. H., Grem, J. L. & Floeter, M. K. Oxaliplatin-induced neurotoxicity: acute hyperexcitability and chronic neuropathy. Muscle Nerve 29, 387–92 (2004).
Wilson, R. H. et al. Acute oxaliplatin-induced peripheral nerve hyperexcitability. J Clin Oncol 20, 1767–74 (2002).
Adelsberger, H. et al. The chemotherapeutic oxaliplatin alters voltage-gated Na(+) channel kinetics on rat sensory neurons. Eur J Pharmacol 406, 25–32 (2000).
Grolleau, F. et al. A possible explanation for a neurotoxic effect of the anticancer agent oxaliplatin on neuronal voltage-gated sodium channels. J Neurophysiol 85, 2293–7 (2001).
Park, S. B. et al. Acute abnormalities of sensory nerve function associated with oxaliplatin-induced neurotoxicity. J Clin Oncol 27, 1243–9 (2009).
Webster, R. G., Brain, K. L., Wilson, R. H., Grem, J. L. & Vincent, A. Oxaliplatin induces hyperexcitability at motor and autonomic neuromuscular junctions through effects on voltage-gated sodium channels. Br J Pharmacol 146, 1027–39 (2005).
Jamieson, S. M. F., Liu, J., Connor, B. & McKeage, M. J. Oxaliplatin causes selective atrophy of a subpopulation of dorsal root ganglion neurons without inducing cell loss. Cancer Chemotherapy and Pharmacology 56, 391–399 (2005).
Screnci, D. et al. Relationships between hydrophobicity, reactivity, accumulation and peripheral nerve toxicity of a series of platinum drugs. British Journal of Cancer 82, 966–972 (2000).
Yan, F., Liu, J. J., Ip, V., Jamieson, S. M. & McKeage, M. J. Role of platinum DNA damage-induced transcriptional inhibition in chemotherapy-induced neuronal atrophy and peripheral neurotoxicity. J Neurochem 135, 1099–112 (2015).
Kawashiri, T. et al. L type Ca(2)+ channel blockers prevent oxaliplatin-induced cold hyperalgesia and TRPM8 overexpression in rats. Mol Pain 8, 7 (2012).
Shirahama, M. et al. Inhibition of Ca2+/calmodulin-dependent protein kinase II reverses oxaliplatin-induced mechanical allodynia in rats. Mol Pain 8, 26 (2012).
Gamelin, L. et al. Prevention of oxaliplatin-related neurotoxicity by calcium and magnesium infusions: a retrospective study of 161 patients receiving oxaliplatin combined with 5-Fluorouracil and leucovorin for advanced colorectal cancer. Clin Cancer Res 10, 4055–61 (2004).
Sakurai, M. et al. Oxaliplatin-induced neuropathy in the rat: involvement of oxalate in cold hyperalgesia but not mechanical allodynia. Pain 147, 165–74 (2009).
Han, C. H., Khwaounjoo, P., Kilfoyle, D. H., Hill, A. & McKeage, M. J. Phase I drug-interaction study of effects of calcium and magnesium infusions on oxaliplatin pharmacokinetics and acute neurotoxicity in colorectal cancer patients. BMC Cancer 13 (2013).
Loprinzi, C. L. et al. Phase III Randomized, Placebo-Controlled, Double-Blind Study of Intravenous Calcium and Magnesium to Prevent Oxaliplatin-Induced Sensory Neurotoxicity (N08CB/Alliance). J Clin Oncol 32, 997–1005 (2014).
Pachman, D. R. et al. Calcium and Magnesium Use for Oxaliplatin-Induced Neuropathy: A Case Study to Assess How Quickly Evidence Translates Into Practice. J Natl Compr Canc Netw 13, 1097–101 (2015).
Allain, P. et al. Early biotransformations of oxaliplatin after its intravenous administration to cancer patients. Drug Metabolism and Disposition 28, 1379–1384 (2000).
Graham, M. A. et al. Clinical pharmacokinetics of oxaliplatin: A critical review. Clinical Cancer Research 6, 1205–1218 (2000).
Jerremalm, E., Wallin, I. & Ehrsson, H. New Insights Into the Biotransformation and Pharmacokinetics of Oxaliplatin. Journal of Pharmaceutical Sciences 98, 3879–3885 (2009).
Jerremalm, E., Hedeland, M., Wallin, I., Bondesson, U. & Ehrsson, H. Oxaliplatin degradation in the presence of chloride: Identification and cytotoxicity of the monochloro monooxalato complex. Pharmaceutical Research 21, 891–894 (2004).
Houston, J. B. & Carlile, D. J. Incorporation of in vitro drug metabolism data into physiologically-based pharmacokinetic models. Toxicology in Vitro 11, 473–478 (1997).
Obach, R. S. Predicting Clearance in Humans from In Vitro Data. Current Topics in Medicinal Chemistry 11, 334–339 (2011).
Ip, V. et al. Platinum-specific detection and quantification of oxaliplatin and Pt(R, R-diaminocyclohexane)Cl(2) in the blood plasma of colorectal cancer patients. Journal of Analytical Atomic Spectrometry 23, 881–884 (2008).
Moore, J. W. & Pearson, R. G. Kinetics and Mechanism. John Wiley and Sons, New York. (1981).
Efron, B. Nonparametric estmates of standard error: The jackknife, the bootstrap and other methods. Biometrika 68, 589–599 (1981).
Stewart, A. F. Clinical practice. Hypercalcemia associated with cancer. N Engl J Med 352, 373–9 (2005).
Swaminathan, R. Magnesium metabolism and its disorders. Clin Biochem Rev 24, 47–66 (2003).
Shord, S. S. et al. Oxaliplatin biotransformation and pharmacokinetics: a pilot study to determine the possible relationship to neurotoxicity. Anticancer Res 22, 2301–9 (2002).
Gamelin, L. et al. Predictive factors of oxaliplatin neurotoxicity: the involvement of the oxalate outcome pathway. Clin Cancer Res 13, 6359–68 (2007).
Han, C. H., Kilfoyle, D. H., Hill, A. G., Jameson, M. B. & McKeage, M. J. Preventing oxaliplatin-induced neurotoxicity: rationale and design of phase Ib randomized, double-blind, placebo-controlled, cross-over trials for early clinical evaluation of investigational therapeutics. Expert Opin Drug Metab Toxicol 12, 1479–1490 (2016).
Acknowledgements
We thank the Auckland Medical Research Foundation for research grant support (110014) and Health Research Council of New Zealand for a Clinical Research Training Fellowship for Catherine Han (12–788) and project grant support (12–254). We also thank James McKeage for his invaluable assistance in kinetic analysis of the incubation study data.
Author information
Authors and Affiliations
Contributions
M.J.M., C.H.H. and A.G.H. conceived and designed the clinical study and incubation experiments. C.H.H., P.K. and A.G.H. conducted the incubation experiments. C.H.H. carried out the clinical study and obtained clinical samples. C.H.H. and P.K. analysed the clinical and incubation samples. M.J.M., C.H.H. and P.K. analysed the incubation study data. G.M.M. performed the kinetic modelling and analysis. C.H.H. and M.J.M. analysed the clinical data and developed the extrapolation method. C.H.H. and M.J.M. prepared the manuscript with contributions from all co-authors.
Corresponding author
Ethics declarations
Competing Interests
The authors declare that they have no competing interests.
Additional information
Publisher's note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Han, C.H., Khwaounjoo, P., Hill, A.G. et al. Predicting effects on oxaliplatin clearance: in vitro, kinetic and clinical studies of calcium- and magnesium-mediated oxaliplatin degradation. Sci Rep 7, 4073 (2017). https://doi.org/10.1038/s41598-017-04383-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-017-04383-4
This article is cited by
-
Management of extravasation of oxaliplatin by mimicking its biotransformation
Clinical and Translational Oncology (2018)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.