Abstract
A large number of studies have shown that programmed death-ligand 1 (PD-L1) is abnormally expressed in gliomas. However, the prognostic significance of PD-L1 expression in glioma patients remains unresolved. Accordingly, we conducted a meta-analysis to determine the prognostic role of high PD-L1 in patients with glioma. Electronic databases were searched to identify studies evaluating PD-L1 expression and overall survival (OS) in these patients. A total of 6 studies (published in 4 articles) that involved 1052 patients were included. Pooled results showed that high PD-L1 expression was associated with worse OS in glioma patients (HR = 1.30, 95% CI: 1.02–1.65, P = 0.032). Further subgroup analysis indicated that high PD-L1 expression in glioblastoma (GBM) was also associated with worse OS (HR = 1.40, 95% CI: 1.03–1.90, P = 0.030). Conversely, in index subgroup analysis, neither PD-L1 protein (HR = 1.43, 95% CI: 0.97–2.10, P = 0.068) nor gene (HR = 1.20, 95% CI: 0.83–1.74, P = 0.322) expression was significantly associated with OS. PD-L1 may represent a promising biomarker that predicts disease progression in patients with glioma or GBM. However, because of our limited sample size, further prospective or retrospective multi-centre, well-designed studies should be performed to verify this result.
Similar content being viewed by others
Introduction
Gliomas are the most common primary central nervous system (CNS) tumour, representing 40% of all brain tumours1. According to the World Health Organization (WHO) 2007 classification, gliomas are divided into grades I–IV, with each higher grade corresponding to an increased level of malignancy and poorer overall survival (OS). Glioblastoma (GBM, glioma grade IV) is the most malignant and aggressive form of primary brain tumour. Despite the use of a standard treatment regimen, including total surgical resection, radiotherapy, and adjuvant chemotherapy, GBM remains a major clinical challenge, with an overall 5-year survival rate of only 9.8%2. One significant challenge to treating GBM is the inevitable recurrence of these tumours. It is therefore very important to obtain an accurate prognosis while the tumour is in an early stage.
Programed death-ligand 1 (PD-L1) is a T cell costimulatory molecule implicated in tumour immune escape mechanisms. Binding of PD-L1 to its receptor (PD-1) induces apoptosis or exhaustion of activated immune cells3. Observed in human malignancies, aberrant expression of PD-L1 is associated with clinicopathological features in several types of cancer, including colorectal4, breast5, and lung cancers6. Blocking PD-L1 or PD-1 has been demonstrated to be among the most promising immunotherapeutic strategies for boosting the immune system’s ability to combat cancer7, 8. Although clinical anti-PD-L1/PD-1 therapies have been developed, data regarding the prognostic role of PD-L1 expression in glioma are limited, and findings to date are controversial. Several studies have found that high PD-L1 expression on glioma cells correlates with poor prognosis9, 10, though not all reports support this conclusion11, 12. Thus, it would be useful to determine whether PD-L1 expression is associated with the prognosis of glioma patients.
In this study, we conducted a meta-analysis to evaluate the prognostic role of PD-L1 in patients with glioma. To our knowledge, this is the first meta-analysis to quantitatively synthesize information from all previously published studies related to the potential prognostic value of PD-L1 in glioma patients.
Methods
Literature Search Strategy
All relevant articles were retrieved from searches of the PubMed, EMBASE, Ovid and Cochrane Library databases. These searches were performed using the following keywords and text words: (“PD-L1”, “Programmed cell death ligand 1”, “B7-H1”) and (“glioma” or “glioblastoma” or “central nervous cancer” or “CNS cancer”). The final search in this study was updated on October 15, 2016. References in eligible studies or textbooks were further manually reviewed to identify additional potentially eligible studies.
Inclusion and Exclusion Criteria
Published studies were selected for analysis using the following inclusion criteria: (1) the study patients were confirmed by the department of pathology using diagnostic criteria for glioma, and gliomas were classified based on current WHO guidelines; (2) the study explored the prognostic significance of PD-L1; (3) the article was published in English. The exclusion criteria included the following: (1) duplicate studies; (2) letters, comments, meeting abstracts and reviews; (3) laboratory studies or animal studies or studies related to other types of CNS cancer.
Data Extraction
The following data from each enrolled study were extracted: the first author’s name, year of publication, country of origin, tests used for indexing, technique used to assay PD-L1 levels, cut-off value used to determine PD-L1 positivity and survival analysis method. Hazard ratios (HRs) for PD-L1 expression and OS and the corresponding 95% confidence intervals (95% CIs) were extracted from tables or Kaplan-Meier curves for both PD-L1 low/negative (control group) and PD-L1 high/positive (experimental group) expressers. When both univariate and multivariate analyses of OS results were performed, HRs and 95% CIs were extracted preferentially from the multivariate analysis. When HRs were not reported, we used a previously published methodology13 in Engauge Digitizer version 4.1 to estimate the logarithm-transformed HR and determined variance based on Kaplan–Meier curves.
Quality Assessment of Studies Included
Two reviewers (Song Xue and Ge Song) independently assessed the quality of the selected papers using a modified Newcastle-Ottawa Scale. The scale consisted of three items describing the subject selection criteria (0–4 points), comparability of subjects (0–2 points), and outcomes (0–3 points). The full score attainable was 9 points. In addition, articles with a total score of more than 5 points were considered to be of high quality14.
Statistical Analysis
HRs and 95% CIs were used to measure the effect size. An HR greater than 1 indicated a poor prognosis for patients with high/positive PD-L1 expression. The impact of PD-L1 on survival was considered to be statistically significant if the 95% CI for the HR did not overlap 1. Heterogeneity among studies was evaluated using Cochrane’s Q tests (Chi-squared tests) and the I2 metric. I2 > 50% or P < 0.10 in a Q test indicated large heterogeneity between studies, and we used random effects models to calculate the pooled HR and 95% CI. The fixed effects model was utilized for the remaining analyses. Subgroup analyses were applied to identify the sources of any observed heterogeneity. Such analyses were conducted for the GBM patients, index for PD-L1 protein and gene expression, cut-off value to indicate tumour PD-L1 positivity, and survival analysis method. All analyses were performed using Stata Version 12.0 (Stata Corporation) and Cochrane Review Manager version 5.3 (Cochrane Collaboration). All statistical tests were two sided, and P < 0.05 was taken to indicate statistical significance.
Results
Search Results
Using a previously established retrieval strategy, 139 potentially relevant articles were initially identified from the databases searched. Eighty-six manuscripts were then excluded from the analysis for the following reasons: 9 were duplicate, 22 were reviews or letters, 32 concerned a carcinoma not related to glioma or GBM, and 23 were not related to PD-L1. Thus, 53 articles remained for further full-text assessment. After careful reading of the full text, 49 of the reports were excluded because they did not provide a prognosis (n = 41) or were based on an animal model (n = 8). Ultimately, 4 articles were included in this meta-analysis (Fig. 1)9,10,11,12.
Characteristics of the Included Studies and Quality Assessment
Two of the selected articles each have enrolled two cohorts, and two articles each were selected to assess the prognostic value of expression of the PD-L1 protein and PD-L1 gene10, 11. There was no overlap between the cohorts enrolled in each article. Thus, 6 studies (from 4 articles) involving 1052 patients were available for this meta-analysis. All of the relevant features in the 6 eligible studies are listed in Table 1. The publication years of the eligible studies ranged from 2013 to 2016. Five of the studies evaluated GBM (WHO IV), and the remaining study evaluated glioma (WHO I–IV). Two of the studies evaluated PD-L1 at the gene level, and four evaluated it at the protein level. In one of the gene-level studies, the researchers applied Agilent microarray techniques to assess PD-L1 gene expression, whereas Illumina RNASeq was used in the other. For the protein-level studies, PD-L1 expression was detected using immunohistochemistry (IHC) in 3 and immunofluorescence histochemistry in the other. Three studies reported the observed staining pattern. PD-L1 expression was detected either on the cell surface or in the cytoplasm. The cut-off criterion used to evaluate positivity for PD-L1 protein expression was the percentage of cells stained (≥5%) in 3 studies and the simple presence of PD-L1 staining in 1 study. Among the included protein studies, the percentage of stained cells (≥5%) was therefore the most common cut-off value used to evaluate positive PD-L1 expression. Only two studies conducted multivariate analysis of OS, and remaining four conducted univariate analysis. The rates of patients with gliomas that were positive for PD-L1 expression ranged from 35.29% to 61. 70%.
The quality of the selected studies was assessed by using the Newcastle-Ottawa Scale and found to range from 6 to 8, indicating that the studies were of high quality (Table 2).
Correlation between OS and PD-L1 expression in glioma and GBM
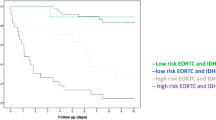
The combined HR for the six studies evaluating PD-L1 expression and it relationship with OS was 1.30 (95% CI: 1.02–1.65, P = 0.032), suggesting that high/positive PD-L1 expression is an indicator of a poor prognosis in glioma patients. Fig. 2 shows a forest plot of the association between PD-L1 and OS in glioma patients. As significant heterogeneity among the studies was observed (Cochran’s Q, P = 0.034, I2 = 58.4%), subgroup analysis of GBM patients was performed. A total of five studies were included in the GBM patient sub-group analysis (Table 3), which was performed using a random-effects model (P = 0.021, I2 = 65.5%). Our results revealed an HR for OS and positive PD-L1 expression of 1.40 (95% CI: 1.03–1.90, P = 0.030) (Fig. 3).
Sub-group analysis
To obtain further insight, we performed subgroup analysis of the testing index, analytical method, and cut-off value to evaluate the prognostic significance of PD-L1 expression in glioma patients. The subgroup analysis of the testing index revealed a merged HR for PD-L1 protein expression of 1.43 (95% CI: 0.97–2.10, P = 0.068), whereas that for PD-L1 gene expression was 1.20 (95% CI: 0.83–1.74, P = 0.322). There was no statistically significant difference between these two groups (P for subgroup difference = 0.530) (Fig. 4). Three of the eligible studies were enrolled in our subgroup analysis of cut-off values (≥5%). High/Positive PD-L1 expression was associated with worse OS (HR = 1.24, 95% CI: 0.99–1.54), but these results were not significant (P = 0.061) (Fig. 5), and the studies showed moderate heterogeneity (P = 0.222, I2 = 33.5%). The results of our subgroup analysis of the analytical method were the same as those of the testing index subgroup analysis (See Supplementary Figure S1). A summary of the hazard ratios obtained in the subgroup analyses is shown in Table 3.
Sensitivity Analysis
The selected studies were sequentially removed to determine whether any single study influenced the pooled results. As shown in Fig. 6, the stable pooled HRs were not significantly affected by any individual study.
Discussion
Both glioma cell lines and glioma cells in tissue samples have been found to aberrantly express PD-L115,16,17. Expression of PD-L1 may affect tumour cell oncogenic signalling pathways that have been collectively termed an “innate immune resistance” mechanism. Parsa et al. found that glioma cells lines (SF126, SF210, U87, U251, and U373) with genetic deletions or mutations in phosphatase and tensin homologue (PTEN) had higher PD-L1 protein levels than cells wild-type for PTEN18. In addition, PD-L1 expression levels in cells in the tumour microenvironment exposed to cytokines were markedly higher, which has been termed an “adaptive immune resistance” mechanism. One example of adaptive immune resistance is an increase in the level of PD-L1 expression in glioma cell lines after the addition of IFN-γ16.
Increased PD-L1 levels have been associated with a poor prognosis in several cancers, such as nasopharyngeal carcinoma19, gastric carcinoma20, and lung cancer21. In contrast, there are no consistent results for the prognostic value of PD-L1 in glioma. In a study of 229 glioma patients (grades I–IV), Zeng et al. found no significant associations between PD-L1 and prognosis by univariate analysis. When the median survival time (12 months) was used as a cut-off value, they found that positive PD-L1 expression had a significant impact on poor OS in patients who survived or were followed up for 12 months12. Liu et al. first sought to determine the prognostic value of PD-L1 in tumour masses (TMs) collected from patients with GBM. A higher level of PD-L1 expression (>10 PD-L1+ cells) in a TM was significantly correlated with a poor prognosis, whereas no or low levels of PD-L1 (1–9 PD-L1+ cells) were not9. An increasing number of researchers have performed studies aimed at investigating the prognostic value of PD-L1 in GBM, but the results thus far have been inconsistent. For example, using IHC to analyse 135 GBM specimens, Berghoff et al. found no significant associations between a membranous staining pattern for PD-L1 expression and OS11. The same approach was taken by Nduom et al., who investigated the prognostic role of PD-L1 expression in 94 patients with GBM and found that high/positive PD-L1 expression was associated with significantly shorter survival (P = 0.0086). Additionally, by applying a multivariate Cox proportional hazards regression model, they found low/negative PD-L1 expression to be a protective factor for OS (HR = 0.554; P = 0.018)10. Moreover, both of these groups analysed the GBM dataset at The Cancer Genome Atlas (TCGA) and reached contradictory conclusions regarding the prognostic value of PD-L1 gene expression. Berghoff et al. used a level 2 Agilent microarray to analyse a cohort of 446 patients, and the results showed no prognostic value of PD-L1 gene expression11. In contrast, Nduom et al. utilized level 3 Illumina RNASeq and found a significant correlation between high levels of PD-L1 gene expression and unfavourable prognoses. Multivariate analysis demonstrated that PD-L1 independently and negatively impacted survival (HR = 1.52; 95% CI = 1.03–2.25; P = 0.0343)10. Therefore, meta-analysis of the data available regarding the prognostic significance of PD-L1 would be useful and is urgently needed.
The present meta-analysis is the first to estimate the correlation between PD-L1 overexpression and survival in patients with glioma. In this meta-analysis, we combined the statistics reported in 4 articles (6 studies) including 1052 patients with glioma, and the data indicated that PD-L1 expression plays a significant role in predicting OS in these patients. We found that the combined HR (1.40) for the GBM data alone was larger than that for all 6 eligible studies of glioma (1.30), suggesting that PD-L1 expression could serve as an important prognostic factor for malignant glioma. However, this result should be considered cautiously because heterogeneity was not eliminated in our GBM subgroup analysis of OS.
Based on subgroup analysis of the testing index, positive PD-L1 expression, at both the protein and gene levels, was associated with poor OS, but this relationship was not significant (P = 0.068 and P = 0.322, respectively). In addition, a strong tendency toward statistical significance was observed between positive PD-L1 expression and a worse prognosis in the cut-off subgroup analysis (HR = 1.24, 95% CI 0.99–1.54, P = 0.061), suggesting that a cut-off value of 5% can be used to estimate OS. Nevertheless, several concerns should be addressed regarding these results. We could not eliminate heterogeneity in the testing index subgroup analysis of OS. There is a lack of validated assays for quantifying the level of PD-L1 expression, and no standardized cut-off criteria are currently applied when determining whether PD-L1 expression is positive. These factors may underlie the heterogeneity observed among the included studies22. In addition, the results of the subgroup analysis of cut-off values should be interpreted with caution because a relatively small number of studies (3 studies) used 5% as the cut-off value. Hence, additional analyses are needed to develop better sensitivity, and specific assays are needed to detect PD-L1 expression23.
Several important limitations should be considered when interpreting our analysis. First, we only included articles published in English. Additionally, we did not analyse publication bias because the number of included studies was relatively small (<10); this likely introduced bias. Moreover, we could not extract HRs with 95% CIs from some of the studies; thus, we evaluated HRs using Kaplan-Meier curves. Finally, we were unable to evaluate the prognostic significance of PD-L1 by stratifying patients according to their clinical features because most of the primary studies did not provide sufficient information to analyse correlations between PD-L1 expression and clinical features, such as age, sex, Karnofsky Performance Status, and O-6-methylguanine-DNA methyltransferase status. Based on these observations, we believe that additional studies are needed and that our conclusions should be interpreted with caution.
In conclusion, despite the limitations described above, our meta-analysis is the first report to focus on the prognostic significance of PD-L1 expression in glioma patients. Our study demonstrated high/positive PD-L1 expression to be associated with poor OS in patients with glioma, and this effect remained significant when the analysis was restricted to GBM patients. Furthermore, our sensitivity analysis did not indicate that alterations in the results (HR) were caused by any individual study, which strengthens the value of our findings. PD-L1 is therefore likely to be particularly useful as a prognostic marker, and it should be included in future validation studies.
References
Turner, J. D. et al. The many roles of microRNAs in brain tumor biology. Neurosurg Focus. 28, E3, doi:10.3171/2009.10.FOCUS09207 (2010).
Tran, B. & Rosenthal, M. A. Survival comparison between glioblastoma multiforme and other incurable cancers. J Clin Neurosci. 17, 417–421 (2010).
Afreen, S. & Dermime, S. The immunoinhibitory B7-H1 molecule as a potential target in cancer: killing many birds with one stone. Hematol Oncol Stem Cell Ther. 7, 1–17 (2014).
Zhao, L. W. et al. B7-H1 and B7-H4 expression in colorectal carcinoma: Correlation with tumor FOXP3+ regulatory T-cell infiltration. Acta Histochem. 116, 1163–1168 (2014).
Muenst, S., Schaerli, A. R., Gao, F. & Däster, S. Expression of programmed death ligand 1 (PD-L1) is associated with poor prognosis in human breast cancer. Breast Cancer Res Treat. 146, 15–24 (2014).
Boland, J. M. et al. Tumor B7-H1 and B7-H3 expression in squamous cell carcinoma of the lung. Clin Lung Cancer 14, 157–163 (2013).
Topalian, S. L., Drake, C. G. & Pardoll, D. M. Targeting the PD-1/B7-H1(PD-L1) pathway to activate anti-tumor immunity. Curr Opin Immunol. 24, 207–212 (2012).
Lu, J., Leegabel, L., Nadeau, M. C., Ferencz, T. M. & Soefje, S. A. Clinical evaluation of compounds targeting PD-1/PD-L1 pathway for cancer immunotherapy. J Oncol Pharm Pract. 21, 451–467 (2015).
Liu, Y. et al. PD-L1 expression by neurons nearby tumors indicates better prognosis in glioblastoma patients. J Neurosci. 33, 14231–14245 (2013).
Nduom, E. K. et al. PD-L1 expression and prognostic impact in glioblastoma. Neuro Oncol. 18, 195–205 (2015).
Berghoff, A. S. et al. Programmed death ligand 1 expression and tumor-infiltrating lymphocytes in glioblastoma. Neuro Oncol. 17, 1064 (2014).
Zeng, J. et al. Expression of programmed cell death-ligand 1 and its correlation with clinical outcomes in gliomas. Oncotarget 7, 8944–8955 (2016).
Tierney, J. F., Stewart, L. A., Ghersi, D., Burdett, S. & Sydes, M. R. Practical methods for incorporating summary time-to-event data into meta-analysis. Trials. 8, 16 (2007).
Wells, G. A., Shea, B. & O’connell, D. The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomized studies in meta-analyses. In: Third Symposium on Systematic Reviews: Beyond the Basics Oxford (July 3–5, 2000).
Wintterle, S. et al. Expression of the B7-related molecule B7-H1 by glioma cells: a potential mechanism of immune paralysis. Cancer Res. 63, 7462–7467 (2003).
Wilmotte, R. et al. B7-homolog 1 expression by human glioma: a new mechanism of immune evasion. Neuroreport. 16, 1081–1085 (2005).
Yao, Y. et al. B7-H1 is correlated with malignancy-grade gliomas but is not expressed exclusively on tumor stem-like cells. Neuro Oncol. 11, 757–766, doi:10.1215/15228517-2009-014 (2009).
Parsa, A. T. et al. Loss of tumor suppressor PTEN function increases B7-H1 expression and immunoresistance in glioma. Nat. Med. 13, 84–88 (2007).
Hsu, M. C. et al. Increase of programmed death-1-expressing intratumoral CD8 T cells predicts a poor prognosis for nasopharyngeal carcinoma. Mod Pathol. 23, 1393–1403 (2010).
Wu, C. et al. Immunohistochemical localization of programmed death-1 ligand-1 (PD-L1) in gastric carcinoma and its clinical significance. Acta Histochem. 108, 19–24 (2006).
Mu, C. Y., Huang, J. A., Chen, Y., Chen, C. & Zhang, X. G. High expression of PD-L1 in lung cancer may contribute to poor prognosis and tumor cells immune escape through suppressing tumor infiltrating dendritic cells maturation. Med Oncol. 28, 682–688 (2011).
Preusser, M., Lim, M., Hafler, D. A. & Sampson, J. H. Prospects of immune checkpoint modulators in the treatment of glioblastoma. Nat Rev Neurol. 11, 504–514 (2015).
Shin, D. S. & Ribas, A. The evolution of checkpoint blockade as a cancer therapy: what’s here, what’s next? Curr Opin Immunol. 33C, 23–35 (2015).
Acknowledgements
We thank the following organizations for offering financial support for this research study: the National Natural Science Foundation of China (Grant No. 81472812) and Innovation Project of Shandong Academy of Medical Science.
Author information
Authors and Affiliations
Contributions
S.X. designed the study. G.S. collected and analysed data. S.X. and G.S. wrote the main manuscript. J.Y. revised the manuscript. All authors reviewed the manuscript and approved the final vision to be submitted.
Corresponding author
Ethics declarations
Competing Interests
The authors declare that they have no competing interests.
Additional information
Publisher's note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Xue, S., Song, G. & Yu, J. The prognostic significance of PD-L1 expression in patients with glioma: A meta-analysis. Sci Rep 7, 4231 (2017). https://doi.org/10.1038/s41598-017-04023-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-017-04023-x
This article is cited by
-
Advanced immunotherapies for glioblastoma: tumor neoantigen vaccines in combination with immunomodulators
Acta Neuropathologica Communications (2023)
-
Difference in immunohistochemical findings among anti-PD-L1 antibodies and their relationships with CD4+ and CD8+ T cells in Japanese melanoma patients
International Journal of Clinical Oncology (2022)
-
Frequency of mismatch repair protein deficiency and PD-L1 in high-grade gliomas in adolescents and young adults (AYA)
Brain Tumor Pathology (2021)
-
The role of vascular endothelial growth factor in the hypoxic and immunosuppressive tumor microenvironment: perspectives for therapeutic implications
Medical Oncology (2020)
-
Elevated PD-L1 expression predicts poor survival outcomes in patients with cervical cancer
Cancer Cell International (2019)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.