Abstract
The aim of this study was to investigate the impact of local treatment modalities on the survival of patients with International Federation of Gynecology and Obstetrics (FIGO) stage IB-IIB cervical cancer, including cancer-directed surgery (CDS) alone and CDS combined with radiotherapy (RT). A total of 8,357 patients with cervical cancer between 1988 and 2013 were included in the final study cohort, including 4,298 (51.4%) patients who underwent CDS alone and 4,059 (48.6%) patients who received combination therapy. Univariate and multivariate analyses showed that local treatment modalities were prognostic factors for cause-specific survival (CSS). Patients who received combination therapy had worse CSS (HR = 1.38; 95% CI = 1.20–1.59; P < 0.001). Subgroup analyses showed the prognostic effect of local treatment modalities was significantly influenced by FIGO stage. In the propensity-score matched (PSM) dataset, CDS was associated with better CSS (P < 0.001) for patients with IB-IIA cervical cancer; nevertheless, no differences were observed in CSS (P = 0.639) for patients with IIB cervical cancer. In conclusion, radical surgery was the preferred treatment for patients with IB-IIA cervical cancer, and there was no difference between radical surgery alone and combination therapy for patients with IIB cervical cancer.
Similar content being viewed by others
Introduction
Despite the significant advances in the screening and treatment of cervical dysplasia, cervical cancer is the sixth most prevalent female malignancy, and the incidence and mortality of cervical cancer is increasing yearly in China1, 2. According to the National Comprehensive Cancer Network (NCCN) guidelines, the current standard treatments for International Federation of Gynecology and Obstetrics (FIGO) stage IB-IIB cervical cancer are recommended according to disease stages3. For most patients presenting with IB-IIA disease, radical hysterectomy and pelvis with or without para-aortic lymphadenectomy is the current standard treatment, and no differences were observed between radiotherapy and surgery in terms of 5-year survival rates. Additionally, for patients with IIB cervical cancer, combination therapy is the standard treatment method4.
In practice, there is still controversy on choice of treatment method for early stage cervical cancer. Several studies suggested that radical surgery should be enough for local disease control even without adjuvant or neoadjuvant radiotherapy (RT)5,6,7. However, it has also been suggested the survival for combination therapy is superior to primary surgery alone8,9,10. Unfortunately, it is difficult to draw conclusions on local treatments in early stage cervical cancer from previous studies comprised of limited case reports11. In this regard, we used the data from the Surveillance Epidemiology and End Results (SEER) database to investigate the difference between combination therapy and primary surgery alone. Furthermore, we discovered significant differences in the baseline characteristic of previous studies. Thus, in this study, we performed propensity-score matched (PSM) analyses to adjust for biases from baseline characteristics of the two treatment groups.
Results
Baseline characteristics in the entire population
In the unmatched database, a total of 8,357 patients met our inclusion criteria and were included in our final analysis. The median follow-up time was 72 months (range: 0–311 months). Table 1 summarizes the characteristics of the study population. The median age of cervical cancer diagnosis was 43 years (range: 15–97 years) and 31.8% of patients were aged 50 years or more. A total of 4,298 (51.4%) patients underwent CDS and 4,059 (48.6%) patients received CDS + RT treatment. Significant differences between two treatment groups were recorded regarding patient characteristics. As shown in Table 1, it was investigated that significant differences were found among the age, race, marital status, histological subtypes, primary site, grade, FIGO stage, nodal status size and surgical methods. All of them had statistical difference (P < 0.05) except race (P = 0.072) and marital status (P = 0.138).
Analysis of prognostic factors
In the dataset, univariate analysis showed that age, race, histological subtypes, primary site, grade, FIGO stage, nodal status, tumor size, surgical methods and local treatment modalities were prognostic factors that affected CSS (P < 0.05; Table 2). Marital status was not associated with CSS (P > 0.05; Table 2). Multivariate analysis showed that race, histological subtypes, grade, FIGO stage, nodal status, tumor size, surgical methods and local treatment modalities were prognostic factors that affected CSS (P < 0.05; Table 3). Patients who received CDS + RT treatment had worse CSS (HR = 1.38; 95% CI = 1.20–1.59; P < 0.001).
Impact of local treatment modalities on survival
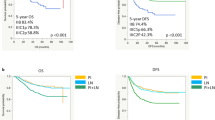
Kaplan-Meier analysis showed the impact of local treatment modalities on CSS for early stage cervical cancer patients (Fig. 1). Patients who received CDS alone had better CSS (P < 0.001; Fig. 1A) compared to patients who had CDS + RT. According to the NCCN guidelines, the preferred treatments for IB-IIB cervical cancer depend on disease stages. Thus, the prognostic effects of the different local treatment modalities according to FIGO stage were evaluated. For patients with IB and IIA cervical cancer, CDS was associated with better CSS (P < 0.001; Fig. 1B and C, respectively); nevertheless, for patients with IIB cervical cancer, no differences were observed in CSS according to different local treatment modalities (P = 0.259; Fig. 1D). According to this, we divided the data into two groups: one contains FIGO stage IB-IIA patients, the other FIGO stage IIB patients. Because there were both significant differences in the baseline characteristic of two groups, we performed two PSM analyses at a 1:1 ratio and a 5:1 ratio to erase significant difference of each variable, respectively (Table 3 and Table 4, respectively).
The 1:1 matching for CDS + RT versus CDS resulted in 1,499 matched pairs and a sample size of 2,998 patients (Table 3). The 5:1 matching for CDS + RT versus CDS resulted in 950 matched pairs and a sample size of 1,140 patients (Table 4). In the unmatched dataset, CDS was associated with better CSS in IB-IIA group (P < 0.001); nevertheless, no differences were observed in CSS according to different local treatment modalities in IIB group (P = 0.259). In the matched dataset, we obtained similar results: in IB-IIA group, CDS was still associated with better CSS (P < 0.001; Fig. 2A) and multivariate analysis demonstrated patients who received CDS + RT treatment had worse CSS (HR = 1.50; 95% CI = 1.18–1.90; P = 0.001); in IIB group, there was no difference between two treatment groups in CSS (P = 0.639; Fig. 2B).
Discussion
In this study, we found that prognostic effects of the different local treatment modalities were greatly influenced by FIGO stage. On this basis, we further performed PSM analyses to adjust for biases from different baseline characteristics of two treatment groups. We demonstrated that CDS was associated with better CSS for patients IB-IIA cervical cancer. A retrospective study by Soisson et al. explained the reason why CDS outperformed CDS + RT. They reported that surgery alone had a better disease-free survival than combination therapy for patients with IB-IIA cervical cancer, but patients receiving adjuvant radiotherapy had several risk factors for recurrence, including lymphatic metastases, tumor involvement of the surgical margin, and large cervical lesions. Radiotherapy appears to reduce the incidence of pelvic recurrences but has no effect on distant failure of patients with high risks7.
Besides, no difference was observed comparing CDS and CDS + RT for patients with IIB cervical cancer in our study. Several retrospective studies suggested that radiotherapy combined with radical surgery could prolong the survival time for patients with IIB cervical cancer8, 9. However, the previous studies may have a few shortcomings. First, these studies are composed of limited cases. Second, because multivariate analysis in our study showed that race, histological subtypes, grade, nodal status and tumor size were all affected prognosis of cervical cancer patients, it is important to adjust for differences between baseline characteristics; nevertheless previous studies have significant differences between baseline characteristics. There was also prospective study that indicated similar results11. Unfortunately, the significant differences between baseline characteristics were still observed in prospective studies. By contrast, our study has overcome these shortcomings. First, this study has a large sample size which included a total of 8,357 patients who met our inclusion criteria. In the matched dataset, there were still 2,998 and 1,140 patients in FIGO stage IB-IIA and IIB group respectively. Second, our current study is the first to adjust for imbalance in the baseline characteristics between two treatment groups using PSM analysis. Thus, our study is statistically significant and innovative.
Zhou et al.6, using the SEER database, looked at the prognostic role of local treatment modalities in early stage small-cell carcinoma of the cervix (SCCC). They found that CDS was associated with better CSS in FIGO stage I SCCC; in FIGO stage II SCCC, no differences were observed in CSS. In our study, we adopted a more refined staging method to group patients into FIGO stage IB, IIA and IIB. We found that CDS was associated with better CSS in FIGO IB and IIA, and no differences were observed in FIGO IIB by subgroup analysis. Accordingly, we performed two PSM analyses regarding to IB-IIA and IIB respectively, which further confirmed our results. Furthermore, we investigate all subtypes of cervical cancer rather than simple subtype. Therefore, our study has larger application range and more reliability.
Although our study tried to overcome shortcomings of previous studies, it still had several potential limitations. First, SEER database lacks some important information regarding patient status, such as infection of human papilloma virus (HPV), comorbidities and economic conditions, that is apparently associated with prognosis12, 13. Second, due to the limitations of SEER database, the information of chemotherapy regimens and dose is unknown, that limits our ability to assess the clinical outcome of local treatment modalities. Third, although our study has measure the effects of different surgery methods divided by resection scope, beyond that, how many patients had lymphadenecthomy and the number of lymphonodes removed both have effects on surgical outcomes. Nevertheless, the above information was not collected into SEER database. Fourth, the same condition for radiotherapy. The technique used and radiotherapy doses cannot be assessed. Fifth, adjuvant radiotherapy is recommended when postoperative pathological examinations reveal risk factors for recurrence, including lymph node metastasis, parametrial invasion, deep stromal invasion, lymph vascular space involvement, and bulky tumor (tumor size >4 cm)14. Unfortunately, the information about these risks is incomplete.
In conclusion, combination therapy has been investigated in several settings for decades15,16,17, but our study demonstrated that compared with radical surgery alone, radical surgery combined with radiotherapy did not improve survival in early stage cervical cancer patients. Given the excessive financial burden and side effects from radiotherapy7, 18, 19, radical surgery alone is preferred treatment for early stage cervical cancer patients. Further prospective studies designed adequately with larger sample size are needed to confirm the results of this study, as well as to define optimal local management in early stage cervical cancer.
Methods
Patient selection in the SEER database
Patient data were obtained from the latest version of the SEER database as released in July 2016 (covering 18 registries, 1973–2013), by using SEER* Stat version 8.3.2. We have got the permission to access them on purpose of research only (Reference number: 12641-Nov2014). The data released by the SEER database do not require informed patient consent, and our study was approved by the Ethical Committee and Institutional Review Board of Soochow University. The methods were performed in accordance with the guidelines outlined in the Declaration of Helsinki.
We extracted cases of patients with a primary diagnosis of FIGO stage IB-IIB uterine cervical cancer (International Classification of Disease for Oncology, Third Edition) between 1988 and 2013. We excluded patients with more than one primary tumor, metastatic disease. Patients with unconfirmed or unknown tumor information were also excluded. The following covariates were collected from the database: age, race, marital status, histological subtypes, primary site, grade, FIGO stage, nodal status, size and surgical method. Relevant treatment-related data included cancer-directed surgery combined with radiotherapy (CDS + RT) and cancer-directed surgery (CDS) alone. In order to evaluate the overall effect of RT, we merge patients receiving either adjuvant or neoadjuvant RT into one group. Duration of follow-up, and cause of death described as due to cancer (CSS) were also included.
Statistical analysis
The chi-squared test (or Fisher’s exact test, if appropriate) was used to analyze the differences between patients grouped by categorical variables. Clinical outcomes were compared between patients treated with CDS alone (referred to as CDS group) and CDS combined with RT (referred to as CDS + RT group). Survival curves were generated using Kaplan-Meier methods, and compared by log-rank test. Univariate and multivariate Cox regression analyses were used to analyze the independent risk factors for CSS. Only variables with statistical significance (P < 0.05) in univariate analysis were incorporated into multivariate analysis. Hazard ratios (HR) were calculated based on multivariable Cox proportional hazards models to estimate predictors of CSS. All CIs were stated at the 95% confidence level. Statistical significance was set at P < 0.05.
To adjust for differences between CDS + RT group and CDS group for FIGO stage IB-IIA and IIB patients, we performed two PSM analyses at a 1:1 ratio and a 5:1 ratio respectively. The PSM model was based upon age, race, marital status, histological subtypes, primary site, grade, nodal status, size and surgical method. The difference of each variable was considered significant if two-sided p-values less than 0.05. Statistical analyses were performed using SPSS statistical software package, version 22.0(SPSS Inc., Chicago, IL).
References
Chen, W. et al. Cancer statistics in China, 2015. CA: a cancer journal for clinicians 66, 115–132, doi:10.3322/caac.21338 (2016).
Quinn, M. A. et al. Carcinoma of the cervix uteri. FIGO 26th Annual Report on the Results of Treatment in Gynecological Cancer. International journal of gynaecology and obstetrics: the official organ of the International Federation of Gynaecology and Obstetrics 95(Suppl 1), S43–103, doi:10.1016/S0020-7292(06)60030-1 (2006).
Koh, W. J. et al. Cervical Cancer, Version 2.2015. Journal of the National Comprehensive Cancer Network: JNCCN 13, 395–404; quiz 404 (2015).
Colombo, N. et al. Cervical cancer: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Annals of oncology: official journal of the European Society for Medical Oncology/ESMO 23(Suppl 7), vii27–32, doi:10.1093/annonc/mds268 (2012).
Asano, H., Todo, Y. & Watari, H. Adjuvant chemotherapy for early-stage cervical cancer. Chinese journal of cancer research = Chung-kuo yen cheng yen chiu 28, 228–234, doi:10.21147/j.issn.1000-9604.2016.02.12 (2016).
Zhou, J. et al. The local treatment modalities in FIGO stage I-II small-cell carcinoma of the cervix are determined by disease stage and lymph node status. Cancer medicine 5, 1108–1115, doi:10.1002/cam4.687 (2016).
Soisson, A. P. et al. Adjuvant radiotherapy following radical hysterectomy for patients with stage IB and IIA cervical cancer. Gynecologic oncology 37, 390–395 (1990).
Eifel, P. J. et al. Pelvic irradiation with concurrent chemotherapy versus pelvic and para-aortic irradiation for high-risk cervical cancer: an update of radiation therapy oncology group trial (RTOG) 90-01. Journal of clinical oncology: official journal of the American Society of Clinical Oncology 22, 872–880, doi:10.1200/JCO.2004.07.197 (2004).
Peters, W. A. 3rd. et al. Concurrent chemotherapy and pelvic radiation therapy compared with pelvic radiation therapy alone as adjuvant therapy after radical surgery in high-risk early-stage cancer of the cervix. Journal of clinical oncology: official journal of the American Society of Clinical Oncology 18, 1606–1613 (2000).
Rotman, M. et al. A phase III randomized trial of postoperative pelvic irradiation in Stage IB cervical carcinoma with poor prognostic features: follow-up of a gynecologic oncology group study. International journal of radiation oncology, biology, physics 65, 169–176, doi:10.1016/j.ijrobp.2005.10.019 (2006).
Li, X. et al. [Comparison of the clinical efficacy of different treatments based on radical surgery in stage b2 and a2 cervical cancer: a prospective randomized control study]. Zhonghua fu chan ke za zhi 51, 524–529, doi:10.3760/cma.j.issn.0529-567X.2016.07.008 (2016).
Kasamatsu, T. et al. Surgical treatment for neuroendocrine carcinoma of the uterine cervix. International journal of gynaecology and obstetrics: the official organ of the International Federation of Gynaecology and Obstetrics 99, 225–228, doi:10.1016/j.ijgo.2007.06.051 (2007).
Lee, D. Y. et al. Prognostic factors in neuroendocrine cervical carcinoma. Obstetrics & gynecology science 59, 116–122, doi:10.5468/ogs.2016.59.2.116 (2016).
Nagase, S. et al. Evidence-based guidelines for treatment of cervical cancer in Japan: Japan Society of Gynecologic Oncology (JSGO) 2007 edition. International journal of clinical oncology 15, 117–124, doi:10.1007/s10147-010-0061-x (2010).
Curtin, J. P. et al. Adjuvant chemotherapy versus chemotherapy plus pelvic irradiation for high-risk cervical cancer patients after radical hysterectomy and pelvic lymphadenectomy (RH-PLND): a randomized phase III trial. Gynecologic oncology 61, 3–10 (1996).
Angioli, R. et al. Neoadjuvant chemotherapy plus radical surgery followed by chemotherapy in locally advanced cervical cancer. Gynecologic oncology 127, 290–296, doi:10.1016/j.ygyno.2012.07.104 (2012).
Hosaka, M. et al. Treatment of cervical cancer with adjuvant chemotherapy versus adjuvant radiotherapy after radical hysterectomy and systematic lymphadenectomy. The journal of obstetrics and gynaecology research 34, 552–556, doi:10.1111/j.1447-0756.2008.00739.x (2008).
Takeshima, N. et al. Treatment results of adjuvant chemotherapy after radical hysterectomy for intermediate- and high-risk stage IB-IIA cervical cancer. Gynecologic oncology 103, 618–622, doi:10.1016/j.ygyno.2006.04.019 (2006).
Barter, J. F., Soong, S. J., Shingleton, H. M., Hatch, K. D. & Orr, J. W. Jr. Complications of combined radical hysterectomy-postoperative radiation therapy in women with early stage cervical cancer. Gynecologic oncology 32, 292–296 (1989).
Acknowledgements
This work was supported by grants from the National Natural Science Foundation of China (No. 81301960, 31428005, 31570877 and 31570908), the Key R&D Project of Science and Technology Department of Jiangsu Province (BE2015633 and BE2015634), General Program of Jiangsu Province Department of Health (H201350), and the Project of Jiangsu Key Laboratory of Medical Science and Laboratory Medicine (JSKLM-2014-003).
Author information
Authors and Affiliations
Contributions
H.-L.P., X.S. and Y.H. conceived and designed the study. X.S. performed the analysis, prepared the figures and tables and wrote the main manuscript. All of the authors reviewed the manuscript.
Corresponding authors
Ethics declarations
Competing Interests
The authors declare that they have no competing interests.
Additional information
Publisher's note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Song, X., Han, Y., Shao, Y. et al. Assessment of local treatment modalities for FIGO stage IB-IIB cervical cancer: A propensity-score matched analysis based on SEER database. Sci Rep 7, 3175 (2017). https://doi.org/10.1038/s41598-017-03580-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-017-03580-5
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.