Abstract
Immuno-inflammation has been shown to play a pivotal role in the pathogenesis of moyamoya disease (MMD). However, how did circulating Treg/Th17 cells involve in MMD patients remains unclear. 26 MMD, 21 atherothrombotic stroke, and 32 healthy controls were enrolled in this study. MMD patients have a significantly higher percentage of circulating Treg and Th17 cells as well as their dominantly secreting cytokines than other groups (P < 0.0001), whereas no difference was found in the ratio of Treg/Th17 between patients in MMD and atherothrombotic stroke group or control subjects (P = 0.244). However, the increased Treg in MMD patients which were enriched with FrIII Treg cells had deficient suppressive functions (P = 0.0017) compared to healthy volunteers. There was a positive correlation between Treg or TGF-β and MMD Suzuki’s stage. And the level of circulating Treg was as an independent factor associated with MMD stage. Besides, TGF-β was also correlated with the increased expression of VEGF in MMD patients. Our findings indicated an important involvement of circulating Treg in the pathogenic development of MMD and TGF-β in Treg induced VEGF.
Similar content being viewed by others
Introduction
Moyamoya disease (MMD) is a chronic steno-occlusive cerebrovascular disorder characterized by progressive stenosis of the terminal internal carotid artery (ICA) and/or its proximal branches, typically accompanied by an abnormally thin and fragile collateral vascular network at the base of the brain developed to compensate as the blood flow decreases in the affected area1. Accumulating studies showed that inflammation and autoimmune responses may be involved in the development of MMD2,3,4. Currently, imbalance of two unique CD4+T helper (Th) cell subsets, Treg and Th17 cells, has been implicated in the pathogenesis of a wide spectrum of autoimmune and inflammatory diseases5, 6. Moreover, different Treg subsets with distinct functions were identified recently6,7,8. For example, CD4+CD25+FoxP3lowCD45RA−Tregs cells also named as Fraction (Fr) III Treg potent effector-Th cells capabilities9. However, whether Treg/Th17 cells are involved in the pathogenic development of MMD remains to be explored.
Vascular endothelial growth factor (VEGF) plays an essential role in the formation and maintenance of moyamoya vessels in MMD patients10. Interestingly, Treg have been shown to promoting angiogenesis via secreting VEGFA in response to hypoxia11. Besides, Treg-produced transforming growth factor (TGF)-β1 could induce production of VEGF and stimulate subsequent angiogenesis12. Nonetheless, whether Treg/Th17 contribute to the production of VEGF and subsequent angiogenesis in development of MMD was unknown.
Therefore, we would like to investigate here whether imbalance of Treg/Th17 is associated with the course of MMD, and if so whether it contributes to abnormal angiogenesis in MMD through regulation of VEGF signaling. Our results will clarify the importance of Treg/Th17s in the pathogenesis of MMD, thus providing a potential therapeutic target for MMD patients.
Materials and Methods
Patients
This study was approved by the ethics committee of the affiliated Drum Tower Hospital, Nanjing University Medical School, and all experiments were performed in accordance with relevant guidelines and regulations. Twenty-six inpatients diagnosed with definitive MMD by DSA according to the diagnostic criteria13 were enrolled from the Department of Neurology and Neurosurgery of Drum Tower Hospital between 2013 and 2014. After a detailed explanation of the study procedures, all participants or their guardians signed an informed consent form before the study. Patients who met any of the following criteria were excluded: 1) diagnosed with Quasi-moyamoya disease; 2) active intracranial hemorrhage including intracerebral hemorrhage, intraventricular hemorrhage, and subarachnoid hemorrhage; 3) patients were not suitable for DSA or MRI; 4) patients with severe infection and other disease which could influence inflammation and autoimmune responses. For controls we recruited twenty-one atherothrombotic stroke patients diagnosed by guidelines for diagnosis and therapy on Chinese patients with acute ischemic stroke14 and thirty-two age-matched healthy volunteers in this research. To minimize the effects of stroke on inflammation and autoimmune responses, heparinized whole blood samples of MMD and atherothrombotic stroke patients were collected at 48 ± 16.3 days after stroke which is believed as the recovery phase following ischemic stroke.
Flow cytometry
To investigate the changes of Treg and Th17 cells in MMD patients, flow cytometry was used to measure the percentage of Th17 and Treg cells. Briefly, peripheral blood mononuclear cells (PBMCs) were isolated from the fresh blood by Ficoll gradient centrifugation. For Th17 cells, the isolated PBMCs were pre-treated with phorbol 12-myristate-13-acetate (PMA, 25 ng/ml), ionomycin (50 µg/ml) and brefeldin-A(BFA, 10 µg/ml, Enzo Life Sciences, Farmingdale, USA) at 37 °C for 4 h, then were collected and surface-stained with antibodies (eBiosicence, Frankfurk, Germany) at room temperature (RT) for 15 min, followed by fixed and permeabilized with the transcription factor staining buffer set kit according to the manufacturer’s protocol (eBioscience), then intracellular-stained with IL-17 antibody (eBioscience) for 30 min. Treg and its subtypes were incubated with surface antibodies at RT for 15 min. After fixed and permeabilized, cells were stained with Foxp3 antibody (eBiosicence) at RT for 30 min. Isotype controls were used in parallel. CD4+CD25+Foxp3+ cells were considered as Treg cells while CD3+CD8−IL-17+ cells were defined as Th17 cells. Cells were measured using flow cytometry (BD bioscience, San Diego, CA, USA). Data were analyzed using Flowjo software (Tree Star, Ashland, OR).
Cytometric Bead Array (CBA) and enzyme-linked immunosorbent assay (ELISA) assay
Next, to evaluate the role of Treg/Th17-driven inflammation, serum cytokines from Treg/Th17, Th1/Th2, and other inflammatory and angiogenenic factors, including interleukin (IL)-2, IL-4, IL-6, IL-10, IL-17, IL-23, tumor necrosis factor (TNF)-α, interferon (INF)-γ, VEGF, intercellular adhesion molecule (ICAM)-1 and vascular cell adhesion molecule (VCAM) were measured by Cytometric Bead Array (CBA, human inflammation kit, BD Biosciences) according to the manufacturer’s instructions. TGF-β and high-mobility group protein (HMGB)-1 were measured by a commercially available ELISA (R&D Systems, Minneapolis, MN) according to the manufacturer’s instructions.
Cell purification and Treg suppressive assay
To determine whether the Treg from MMD have immunosuppressive capacity, the proliferation effect of T cells was measured by flow cytometry. Treg cells were isolated using human CD4+CD25+Treg Isolation Kit (MiltenyiBiotec, Inc., Auburn, CA) according to the manufacturer’s instructions. The CD4+CD25− fraction was defined as effector T (Teff) cells. The Treg suppressive assay was conducted as described before15. In brief, 5 * 104 carboxyfluorescein diacetate succinimidyl ester (CFSE)-labeled Teff cells (2.5 µM) per well were plated and cultured in a 24-well plate with Treg cells (Teff/Treg = 1:1) in the presence of CD3/CD28 antibodies (5 ng/ml), TGF-β (10 ng/ml) and IL-2 (100 IU/ml) for 96 h. The Teff cells were harvested and evaluated by flow cytometry. Cultured CD4+CD25− cells were taken as control group. The data were analyzed using Modfit software (Verity Software House 2.0, Top-sham, ME, USA).
Statistical Analysis
All samples and standards were assayed in triplicate. We used SPSS version 19.0 (SPSS Inc, New York, USA) to perform the statistical analyses. Shapiro-Wilk test was used to measure normality of data. Normal continuous variables were presented as mean ± S.D, while non-normal continuous variables were displayed as median and quartiles. Categorical variables were presented as percentages. For normal variables, Student’s t-test and one-way ANOVA were used to comparison between two groups and more than two groups, respectively. For non-normal variables, comparison between two groups and more than two groups was statistically evaluated by Mann-Whitney U-test and Kruskal-Wallis test, respectively. A multiple linear regression analysis was conducted for investigating the impact of Treg, Th17, TGF-β, IL-10 and IL-17 on the serum VEGF. Correlation of the inflammatory and angiogenic factors with the severity of MMD was evaluated by Spearman correlation coefficient (r). The predictive value of serum cytokines on the severity of MMD was tested by binary of logistic regression analysis. A P value < 0.05 was considered statistically significant.
Results
Clinical features of patients
Between Jan 2013 and Dec 2014, a total of 26 consecutive patients with MMD (10 females and 16 males), 21 patients with atherothrombotic stroke (8 females and 13 males) and 32 age-matched healthy volunteers (19 females and 13 males) as controls were enrolled into our cohort. General clinical features of control group, MMD and atherothrombotic stroke patients are summarized in Table 1. The common initial presentations in MMD patients was ischemic stroke in our study (46.15%) followed by cerebral hemorrhage (26.92%), subarachnoid hemorrhage (23.08%) and TIA (3.85%, Table 2). The majority of patients were presented at Suzuki Angiographic stage 4 and 5 (53.84% and 23.08%, respectively) and 92.3% of patients had bilateral lesions. Besides, there was no significant difference in leukocyte count and C-reactive protein (CRP)-levels among MMD, atherothrombotic stroke and controls (data not shown).
Increased peripheral Treg and Th17 in MMD patients
Compared to control, the serum protein level of several inflammatory molecules including HMGB-1, ICAM-1 and VCAM in MMD patients was strikingly increased by 92.32% [57.000 (34.000, 154.000) vs. 27.000 (13.500, 61.000), P < 0.05], 31.66% [38.070 (31.750, 42.760) vs. 28.080 (21.280, 34.905), P < 0.01] and 51.5% [158.135 (130.560, 211.360) vs. 103.975 (85.435, 135.810), P < 0.001], respectively. (Supplementary Fig. 1) These findings indicate that peripheral inflammatory responses were induced in MMD patients.
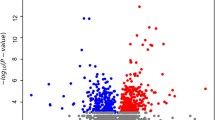
To clarify whether imbalance of peripheral Treg/Th17 is involved in the pathophysiology of MMD, the percentage of Treg and Th17 cells from circulating CD4+ T cells and their dominantly secreting inflammatory cytokines were measured in MMD patients and control. Results showed that Treg and Th17 were significantly increased in MMD patients [4.615 (3.530, 7.240) and 2.440 (1.740, 3.990)] compared to atherothrombotic stroke [2.370 (1.550, 2.680), P < 0.0001 and 1.490 (1.090, 1.690), P < 0.0001)] or healthy control group [2.525 (2.040, 3.350), P < 0.0001 and 1.215 (0.825, 1.695), P < 0.0001] (Fig. 1A,B). However, there was no difference in the ratio of Treg/Th17 among the three groups (P = 0.244, Fig. 1C).
The percentage of peripheral Treg and Th17 cells in MMD patients, atherothrombotic stroke patients and controls. Both the levels of Treg and Th17 were significantly increased in MMD patients compared to other groups. (A,B) Representative FACS plots for Treg and Th17 cells in peripheral blood. (C) The ratio of Treg/Th17 among the three groups. (D) Each bar represents the median and quartiles of three independent experiments. *P < 0.05, **P < 0.01 and ***P < 0.001.
In consistent, serum expression of Treg-related TGF-β and IL-10 was enhanced by 121.67% [34.262 (28.016, 45.254) vs. 16.973 (12.117, 19.643), P < 0.001] and 8.83% [12.855 (12.210, 13.620) vs. 12.000 (11.155, 12.860), P = 0.0029] in MMD patients compared with control. Similarly, Th17-related IL-17, TNF-α, IL-6 and IL-23 were significantly higher than control by 57.94% [130.655 (99.710, 150.030) vs. 78.565 (74.070, 85.455), P < 0.001], 7.33% [16.680 (15.870, 17.620) vs. 15.970 (14.500, 16.835), P < 0.05], 92.52% [8.420 (7.130, 11.770) vs. 5.285 (2.855, 7.265), P < 0.001] and 39.47% [10.925 (8.200, 15.800) vs. 8.185 (6.950, 9.575), P < 0.01] in MMD patients, respectively (Supplement Fig. 1). Nevertheless, the level of Th1/Th2-related cytokines, such as IL-2, IL-4, and INF-γ was not significantly different between the two groups [IL-2: 6.860 (5.930, 8.280) vs. 6.660 (5.630, 8.180), P = 0.9271; IL-4: 11.210 (9.720, 12.370) vs. 10.560 (9.180, 12.430), P = 0.8562; INF-γ: 14.030 (13.580, 15.000) vs. 13.840 (13.160, 14.675), P = 0.5483].
Decreased suppressive function of peripheral Treg in MMD patients
Since no difference was found in the ratio of Treg/Th17, we further investigated whether suppressive function of Treg in MMD patients was altered. Interestingly, we found that the Treg from MMD patients had a lower suppressive function compared to those from control using proliferative assay (91.81 ± 0.6439 vs 85.84 ± 0.9120, P = 0.0017, Fig. 2A).
The proliferation of CD4+CD25− T cells co-cultured with Treg (A). The suppressive function of Treg isolated from MMD patients was lower than controls. The changes of Treg subtypes in MMD patients and healthy controls. Both the percentage of FrIII Treg cells among CD4+CD25+ T cells (B) and total Treg cells (C) were significantly elevated in MMD patients. FACS plots for subtypes of Treg cells in MMD patients and healthy controls (D). Each bar represents the mean ± SD of three independent experiments. *P < 0.05 and **P < 0.01 vs. normal Treg cells group, ## P < 0.01 vs. control group.
Different Treg subsets have been shown to potent distinct functions. We therefore further measured changes in the percentage of three major Treg subtypes. The results showed that the percentage of FrIII Treg cells among CD4+CD25+ T cells and CD4+CD25+FoxP3+Tregs were significantly elevated in MMD patients compared to control (10.88 ± 0.8052 vs 7.324 ± 0.4782 among CD4+, P = 0.0018; 59.86 ± 2.095 vs 50.74 ± 2.238 among Treg, P = 0.0184, Fig. 2B,C). However, the proportion of FrI Treg among total Treg was markedly decreased in MMD patients (19.17 ± 0.8452 vs 28.37 ± 2.456 among Treg, P = 0.0126). Meanwhile, no significant difference was found in the proportion of FrII Treg cells between the two groups (3.876 ± 0.5328 vs 3.269 ± 0.2573 among CD4+, P = 0.2733; 20.97 ± 1.755 vs 22.52 ± 0.9697 among Treg, P = 0.4172). FrIII Treg cells are lack of suppressive functions. These findings suggested that Treg which induced inflammation and lacked suppressive capacity of T cells resulted from increasing FrIII Treg in MMD patients.
Increased serum expression of VEGF in MMD patients
Moreover, the serum protein expression of angiogenic factor, VEGF was significantly increased by five folds [29.060 (13.910, 63.150) vs. 7.360 (5.325, 10.035), P < 0.0001] in MMD patients compared to control, which was consistent with previous findings16. Intriguingly, results of the multiple linear regression analysis showed that TGF-β had a correlation with VEGF (P < 0.01, Table 3).
Treg and TGF-β is associated with the pathophysiology of MMD
Finally, we investigated the correlation of the inflammatory and angiogenic factors with the severity of MMD. 26 MMD patients were divided into 3 grades based on the Suzuki’s angiographic stage of MMD: grade 1 (Suzuki’s stage 1 and 2, n = 2), grade 2 (Suzuki’s stage 3 and 4, n = 15) and grade 3 (Suzuki’s stage 5 and 6, n = 9). The results suggested that the Suzuki’s angiographic stage is positively correlated with the level of Treg, TGF-β and the ratio of Treg/Th17, but not Th17 and IL-17 (Table 4). To investigate the predictive role of serum Treg and TGF-β for the severity of MMD, binary logistic regression analysis was used. And the results showed that the higher level of Treg could be considered as an predictive factor of (OR 3.842, 95% CI 1.093-13.505) grade 3, compared to grade 2, of MMD after adjusting TGF-β (Table 5). However, these factors had no relationship with onset symptoms and gender.
Discussion
Here, for the first time, we reported: 1) Circulating Treg and Th17 cells were higher in MMD patients than that in atherothrombotic stroke and healthy controls. 2) The dominantly expressed FrIII Treg subset in MMD patients may be responsible for the deficient suppressive function of Treg. 3) TGF-β had a positive relationship with VEGF. 4) Treg is an independent factor associated with MMD Suzuki’s angiographic stage.
In the present study, the ratio of Treg/Th17 was not significantly different between MMD patients and control subjects. However, Treg from MMD patients showed deficient suppressive functions. We believed that function imbalance in Treg/Th17 may contribute to the pathophysiology of MMD, since imbalance of Treg/Th17 is involved in several human autoimmune diseases and Treg depletion can evoke autoimmunity17,18,19,20. Suppressive function of Treg cells have been found to be defective in several other autoimmune diseases such as psoriasis21, type 1 diabetes mellitus (DM)22 and multiple sclerosis (MS)23. Subsequently, we found that increased Tregs were enriched with FrIII Tregs. Accumulating evidence have recently shown that Treg possess high plasticity and can acquire functions of effector-like Th cells, lose their suppressive function but secrete pro-inflammatory cytokines, including IL-1724, 25. Three distinct Treg subpopulations with different functions in human FoxP3+Tregs have been identified. CD4+ CD25+ FoxP3low CD45RA+Tregs (FrI, stable resting Treg), CD4+ CD25+ FoxP3high CD45RA−Tregs (FrII, activated Treg) and CD4+CD25+FoxP3lowCD45RA−Tregs cells (FrIII, unstable Treg). The FrI and FrII Treg are suppressive9, while FrIII Treg are lack of suppressive functions but possess some features of these “ex-Treg” and may be in the process of transforming into Th17 cells. Therefore, in the present study, the increased FrIII Tregs may be responsible for the decreased suppressive functions of Tregs in MMD patients.
C-reactive protein (CRP) is often used as a clinical marker of acute systemic inflammation. In this research, all blood samples of patients were collected at stable phase after stroke and the plasma concentration of CRP shows no significant difference among MMD, atherothrombotic stroke and control group (data not shown). We further found that both of the Treg/Th17 cells dominantly expressed cytokines including IL-10, TGF-β, IL-17, IL-6 and IL-23 were higher in MMD patients than controls. Moreover, IL-2, IL-4 and INF-γ, which are mainly from Th1/Th2, had no significant differences. They could mediate immune and inflammatory responses in several autoimmune diseases, including rheumatoid arthritis (RA), systemic lupus erythematosus (SLE), type 1 DM, MS, allergy, parasitosis, asthma, et al.26, 27. It suggests that the immune response of MMD is not completely consistent with SLE, RA, and so on. Treg/Th17-mediated autoimmune responses and inflammation may contribute to the pathogenesis of MMD.
In addition, HMGB-1, a late-acting pro-inflammatory cytokine, plays an important role and shows aberrant high level in chronic inflammatory diseases such as RA and SLE28. In this study, MMD patients had a higher serum level of HMGB-1 than controls, which is consistent with patients with chronic inflammatory diseases.
Consistent with previous findings, we also found that the serum level of VEGF in MMD patients was dramatically higher than controls16, 29. The increased level of VEGF in MMD may be subjected to upregulated levels of Treg cells and Th17 cells. Treg have been shown to secrete VEGFA in response to hypoxia, which plays a critical role in forming a VEGFA-rich microenvironment and promoting angiogenesis11, while IL-17 has been implicated in upregulating VEGF and promoting VEGFR expression30, 31. Therefore, Treg/Th17 cells may promote angiogenesis of MMD by upregulating the expression of VEGF. In addition, Treg-produced TGF-β1 can also induce production of VEGF and stimulate subsequent angiogenesis12. In our study, the increased TGF-β was associated with the VEGF, which indicated that TGF-β may promote the vascular endothelial cell proliferation leading to abnormal vessels hyperplasia in MMD.
However, there are several limitations in this study. First, this is a preliminary study. The sample size is small. Secondly, TGF-β is not specifically expressed by Treg cells. In our future study, we need enroll more patients. To clarify the relationship of TGF-β and VEGF or MMD stage, level of TGF-β expressed by Treg shouled be measured.
Summary
In conclusion, our research sheds new light on the involvement of Treg/Th17 cells in the pathogenesis of MMD, thereby providing a potential therapeutic target for treatment of MMD patients. A larger number of patients and control subjects should be recruited in the future studies to validate findings in this study.
References
Suzuki, J. & Takaku, A. Cerebrovascular “moyamoya” disease. Disease showing abnormal net-like vessels in base of brain. Archives of neurology 20, 288–299, doi:10.1001/archneur.1969.00480090076012 (1969).
Masuda, J., Ogata, J. & Yutani, C. Smooth muscle cell proliferation and localization of macrophages and T cells in the occlusive intracranial major arteries in moyamoya disease. Stroke 24, 1960–1967, doi:10.1161/01.STR.24.12.1960 (1993).
Young, A. M., Karri, S. K., Ogilvy, C. S. & Zhao, N. Is there a role for treating inflammation in moyamoya disease?: a review of histopathology, genetics, and signaling cascades. Front neurol 4, 105, doi:10.3389/fneur.2013.00105 (2013).
Kronenburg, A., Braun, K. P., van der Zwan, A. & Klijn, C. J. Recent advances in moyamoya disease: pathophysiology and treatment. Curr Neurol Neurosci Rep 14, 423, doi:10.1007/s11910-013-0423-7 (2014).
Curtis, M. M. & Way, S. S. Interleukin-17 in host defence against bacterial, mycobacterial and fungal pathogens. Immunology 126, 177–185, doi:10.1111/j.1365-2567.2008.03017.x (2009).
Kumar, P. & Subramaniyam, G. Molecular underpinnings of Th17 immune-regulation and their implications in autoimmune diabetes. Cytokine 71, 366–376, doi:10.1016/j.cyto.2014.10.010 (2015).
Whibley, N. & Gaffen, S. L. Brothers in arms: Th17 and Treg responses in Candida albicans immunity. PLoS Pathog 10, e1004456, doi:10.1371/journal.ppat.1004456 (2014).
Pandiyan, P. & Zhu, J. Origin and functions of pro-inflammatory cytokine producing Foxp3+ regulatory T cells. Cytokine 76, 13–24, doi:10.1016/j.cyto.2015.07.005 (2015).
Miyara, M. et al. Functional delineation and differentiation dynamics of human CD4+ T cells expressing the FoxP3 transcription factor. Immunity 30, 899–911, doi:10.1016/j.immuni.2009.03.019 (2009).
Shibuya, M. Vascular endothelial growth factor-dependent and-independent regulation of angiogenesis. BMB reports 41, 278–286, doi:10.5483/BMBRep.2008.41.4.278 (2008).
Facciabene, A. et al. Tumour hypoxia promotes tolerance and angiogenesis via CCL28 and T(reg) cells. Nature 475, 226–230, doi:10.1038/nature10169 (2011).
Gupta, S., Joshi, K., Wig, J. D. & Arora, S. K. Intratumoral FOXP3 expression in infiltrating breast carcinoma: Its association with clinicopathologic parameters and angiogenesis. Acta Oncol 46, 792–797, doi:10.1080/02841860701233443 (2007).
Fujimura, M. & Tominaga, T. Diagnosis of moyamoya disease: international standard and regional differences. Neurol Med Chir 55, 189–193, doi:10.2176/nmc.ra.2014-0307 (2015).
Jauch, E. C. et al. Guidelines for the early management of patients with acute ischemic stroke: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke 44, 870–947, doi:10.1161/STR.0b013e318284056a (2013).
Venken, K. et al. A CFSE based assay for measuring CD4+ CD25+ regulatory T cell mediated suppression of auto-antigen specific and polyclonal T cell responses. J Immunol Methods 322, 1–11, doi:10.1016/j.jim.2007.01.025 (2007).
Sakamoto, S. et al. Expression of vascular endothelial growth factor in dura mater of patients with moyamoya disease. Neurosurg Rev 31, 77–81, doi:10.1007/s10143-007-0102-8 (2008).
Wing, K. & Sakaguchi, S. Regulatory T cells exert checks and balances on self tolerance and autoimmunity. Nat Iimmunol 11, 7–13, doi:10.1038/ni.1818 (2010).
Sakaguchi, S., Yamaguchi, T., Nomura, T. & Ono, M. Regulatory T cells and immune tolerance. Cell 133, 775–787, doi:10.1016/j.cell.2008.05.009 (2008).
Cao, D. et al. Isolation and functional characterization of regulatory CD25 bright CD4+ T cells from the target organ of patients with rheumatoid arthritis. Eur J Immunol 33, 215–223, doi:10.1002/immu.200390024 (2003).
de Kleer, I. M. et al. CD4+ CD25bright regulatory T cells actively regulate inflammation in the joints of patients with the remitting form of juvenile idiopathic arthritis. J Immunol 172, 6435–6443, doi:10.4049/jimmunol.172.10.6435 (2004).
Sugiyama, H. et al. Dysfunctional blood and target tissue CD4+ CD25 high regulatory T cells in psoriasis: mechanism underlying unrestrained pathogenic effector T cell proliferation. J Immunol 174, 164–173, doi:10.4049/jimmunol.174.1.164 (2005).
Lindley, S. et al. Defective suppressor function in CD4+CD25+ T-cells from patients with type 1 diabetes. Diabetes 54, 92–99, doi:10.2337/diabetes.54.1.92 (2005).
Viglietta, V., Baecher-Allan, C., Weiner, H. L. & Hafler, D. A. Loss of functional suppression by CD4+ CD25+ regulatory T cells in patients with multiple sclerosis. J Exp Med 199, 971–979, doi:10.1084/jem.20031579 (2004).
Zhou, X., Bailey-Bucktrout, S., Jeker, L. T. & Bluestone, J. A. Plasticity of CD4+ FoxP3+ T cells. Curr Opin Immunol 21, 281–285, doi:10.1016/j.coi.2009.05.007 (2009).
Yang, X. O. et al. Molecular antagonism and plasticity of regulatory and inflammatory T cell programs. Immunity 29, 44–56, doi:10.1016/j.immuni.2008.05.007 (2008).
Kidd, P. Th1/Th2 Balance: The Hypothesis, its Limitations, and Implications for Health and Disease. Altern Med Rev 8, 223–246 (2003).
Huang, Y. P., Perrin, L. H., Miescher, P. A. & Zubler, R. H. Correlation of T and B cell activities in vitro and serum IL-2 levels in systemic lupus erythematosus. J Immunol 141, 827–833 (1988).
Pisetsky, D. S., Erlandsson-Harris, H. & Andersson, U. High-mobility group box protein 1 (HMGB1): an alarmin mediating the pathogenesis of rheumatic disease. Arthritis Res Ther 10, 209, doi:10.1186/ar2440 (2008).
Rafat, N., Beck, G., Pena-Tapia, P. G., Schmiedek, P. & Vajkoczy, P. Increased levels of circulating endothelial progenitor cells in patients with Moyamoya disease. Stroke 40, 432–438, doi:10.1161/STROKEAHA.108.529420 (2009).
Yang, B. et al. The role of interleukin 17 in tumour proliferation, angiogenesis, and metastasis. Mediators Inflamm 2014, 623759–12, doi:10.1155/2014/623759 (2014).
Tartour, E. et al. Angiogenesis and immunity: a bidirectional link potentially relevant for the monitoring of antiangiogenic therapy and the development of novel therapeutic combination with immunotherapy. Cancer Metastasis Rev 30, 83–95, doi:10.1007/s10555-011-9281-4 (2011).
Acknowledgements
We thank Brad Peterson for editing the English. This research was supported by the National Natural Science Foundation of China (81230026, 81630028, 81171085, 81601016), the Science and Technology Department of Jiangsu Province (BE2016610), the Natural Science Foundation of Jiangsu Province of China (BK20141121, BK20160119) and the Health Institute of Wuxi (Q201625).
Author information
Authors and Affiliations
Contributions
Y.X. designed the experiments and edited the manuscript. L.W., X.C. performed experiments. Y.Y., X.X., Y.G. collected blood samples and clinic diagnosis. L.H., L.W., H.Z. wrote the manuscript. S.Q., Y.Y., X.W., X.C., W.Z., Y.C. and J.L. revised this paper. All authors contributed to the data analysis and the manuscript preparation.
Corresponding authors
Ethics declarations
Competing Interests
The authors declare that they have no competing interests.
Additional information
Publisher's note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Weng, L., Cao, X., Han, L. et al. Association of increased Treg and Th17 with pathogenesis of moyamoya disease. Sci Rep 7, 3071 (2017). https://doi.org/10.1038/s41598-017-03278-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-017-03278-8
This article is cited by
-
Identification of diagnostic markers for moyamoya disease by combining bulk RNA-sequencing analysis and machine learning
Scientific Reports (2024)
-
Chemical and perfusion markers as predictors of moyamoya disease progression and complication types
Scientific Reports (2024)
-
Factors Influencing Collateral Circulation Formation After Indirect Revascularization for Moyamoya Disease: a Narrative Review
Translational Stroke Research (2023)
-
GM-CSF Promotes the Development of Dysfunctional Vascular Networks in Moyamoya Disease
Neuroscience Bulletin (2023)
-
Aging-associated inflammation and fibrosis in arachnoid membrane
BMC Neurology (2021)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.