Abstract
Reduced amplitude of mismatch negativity (MMN) is one of the more promising biological markers of schizophrenia. This finding holds true in both early and chronic phases of the disorder, and is compatible with the glutamatergic dysfunction hypothesis. To further establish MMN as a biomarker of aberrant glutamatergic neurotransmission, an exploration for an association with blood levels of glutamatergic amino acids is an important next step. Despite a large body of work investigating MMN in schizophrenia, no previous studies have undertaken this endeavor. Nineteen patients with first-episode psychosis (FEP), 21 ultra-high risk individuals (UHR), and 16 healthy controls (HC) participated in the study. The MMNs in response to duration change (dMMN) and frequency change (fMMN) were measured. The fasting plasma levels of glutamate, glutamine, glycine, D-serine, and L-serine were measured. dMMN amplitudes were significantly reduced in FEP and UHR, compared to HC. The plasma levels of glutamate of FEP were significantly higher than those of HC. Higher plasma levels of glutamate were associated with smaller dMMN amplitudes in the FEP and HC groups. These findings are compatible with the hypothesis that MMN is a useful biological marker of aberrant glutamatergic neurotransmission in the early stages of schizophrenia.
Similar content being viewed by others
Introduction
Reduced amplitude of auditory mismatch negativity (MMN) is one of the more promising biological markers in schizophrenia1,2,3,4,5. MMN is an event-related potential (ERP) elicited when infrequent stimuli, deviant in physical features (e.g., duration, frequency [pitch]), occur in a sequence of repetitive auditory stimuli. MMN is thought to reflect auditory sensory memory or preattentive processing. N-methyl-D-aspartate (NMDA) receptor antagonists attenuate MMN amplitude in humans6 and in non-human primates7, 8; therefore, MMN is considered to be a biological indicator of glutamatergic neurotransmission. The reduced amplitude of MMN is conceptually compatible with the glutamatergic dysfunction hypothesis of schizophrenia9,10,11,12,13.
A number of studies have shown MMN amplitude attenuation, not only in chronic schizophrenia patients, but also in subjects in the early stages of psychosis3, 14,15,16,17,18,19,20. These findings suggest that MMN in response to duration deviant stimuli (dMMN) and MMN in response to frequency deviant stimuli (fMMN) may reflect different aspects of the pathophysiology in the early stages of psychosis3. Many studies have reported dMMN amplitude reduction in the early stages of psychosis. In individuals with ultra-high risk (UHR), dMMN amplitude reduction predicts the onset of psychosis21. On the other hand, few studies have reported fMMN amplitude reduction in the early stages of psychosis. In patients with first-episode schizophrenia, fMMN shows progressive reduction after the onset of psychosis22. While these findings indicate MMN amplitude reduction in early stages of psychosis as a group, MMN amplitude reduction is only present in a subset of individuals with early stages of psychosis in these studies. Because MMN is thought to reflect NMDA receptor function, the MMN amplitude attenuation in the subset may be due to the pathophysiology of NMDA receptor hypofunction. Therefore, MMN may serve as a biomarker to identify the subset that has psychosis based on NMDA receptor hypofunction.
To further establish MMN as a useful biological markers of aberrant glutamatergic neurotransmission, especially in the early stages of psychosis, the next step should be to investigate the relationship between MMN amplitude and blood level of molecules that influence NMDA receptor function, such as glutamate and D-serine. Peripheral glutamatergic amino acids have been investigated in patients with schizophrenia23, 24 and a meta-analysis showed that peripheral glutamate levels in schizophrenia patients were significantly higher than those in controls24. This is consistent with a prevalent model of hyperglutamatergic state in schizophrenia. This model is the so-called disinhibition mechanisms whereby NMDA antagonists block the NMDA-medicated drive on GABA interneurons that normally inhibit pyramidal cells. This leads to enhanced activity of pyramidal cells, which then results in increased glutamate release in adjacent cortical or afferent regions25.
However, to the authors’ knowledge, no studies have reported associations between MMN amplitude and peripheral glutamatergic amino acids in early stages of psychosis.
In this study, we measured MMN and the plasma levels of glutamatergic amino acids in subjects in the early stages of psychosis (UHR and first-episode psychosis [FEP]). We hypothesized the reduction of MMN amplitude, increased plasma level of glutamate, and an association between MMN amplitude and the plasma levels of glutamate in early stages of psychosis.
Results
Demographic and clinical variables
There were no significant differences in sex ratio, mean age, education, and premorbid IQ across the three groups. PANSS negative, general, or total were not significantly different between FEP and UHR. PANSS positive, GAF and antipsychotics dose were significantly different between FEP and UHR (Table 1).
MMN
The numbers of epochs for deviants in dMMN were 174 (±20) in HC, 156 (±31) in UHR, and 164 (±28) in FEP. One-way ANOVA revealed no significant difference among the three groups (F2,53 = 1.87, p = 0.17). The numbers of epochs for standards in dMMN were 1607 (±102) in HC, 1505 (±250) in UHR and 1496 (±257) in FEP. One-way ANOVA revealed no significant difference among the three groups (F2,53 = 1.34, p = 0.27).
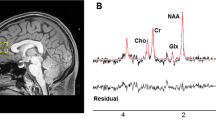
Figure 1 (left) represents the average waveform of dMMN at the electrode FCz. The data of dMMN amplitude of FEP, UHR, HC are all normally distributed according to Shapiro-Wilk test (p = 0.96, p = 0.09, p = 0.52, respectively). One-way ANOVA revealed significant group differences in dMMN amplitude (F2,53 = 6.41, p = 0.003, η 2 = 0.19). Post hoc tests with the Bonferroni correction showed significant differences in dMMN amplitude between FEP and HC (p = 0.004, Cohen’s d = 1.24), and between UHR and HC (p = 0.02, Cohen’s d = 0.88). There was no significant difference in dMMN amplitude between FEP and UHR (p = 1.00, Cohen’s d = 0.21).
The numbers of epochs for deviants in fMMN were 180 (±11) in HC, 156 (±27) in UHR and 167 (±33) in FEP. One-way ANOVA revealed significant difference among the three groups (F2,53 = 3.93, p = 0.026). Post hoc tests with the Bonferroni correction showed significant differences between UHR and HC (p = 0.021), but no significant differences between FEP and HC (p = 0.37) and between FEP and UHR (p = 0.64). There was no significant correlation between the number of epochs and fMMN amplitude in FEP (rs = 0.26, p = 0.28), UHR (rs = −0.03, p = 0.90) or HC (rs = −0.49, p = 0.06). The numbers of epochs for standards in fMMN are 1595 (±118) in HC, 1522 (±207) in UHR and 1526 (±249) in FEP. One-way ANOVA revealed no significant difference among the three groups (F2,53 = 0.70, p = 0.50).
Figure 1 (right) represents the average waveform of fMMN at the electrode FCz. Among the data of fMMN amplitude of FEP, UHR, HC, those of UHR are not normally distributed according to Shapiro-Wilk test (p = 0.47, p = 0.00, p = 1.00, respectively). Kruskal-Wallis test showed significant difference in fMMN amplitude among the three groups. Howerver, Post hoc Mann-Whitney test with significance level p < 0.05/3 = 0.017 did not show any significant difference between HC and UHR (p = 0.025, r = 0.37), or between UHR and FEP (p = 0.728, r = 0.06), or between HC and FEP (p = 0.034, r = 0.36).
The plasma levels of glutamatergic amino acids
The plasma level of glutamate did not follow a normal distribution in FEP (p = 0.28), UHR (p = 0.03), and HC (p = 0.001) according to Shapiro-Wilk test. Kruskal-Wallis test showed significant difference in the plasma level of glutamate among the three groups (χ2 = 10.69, p = 0.005). Mann-Whitney tests with significance level p < 0.05/3 = 0.017 showed significant difference between HC and FEP (p = 0.001, r = 0.54) (Fig. 2). There was no significant difference between HC and UHR (p = 0.16, r = 0.24), or between UHR and FEP (p = 0.04, r = 0.32). The plasma levels of glutamine was normally distributed in FEP (p = 0.14), UHR (p = 0.36), and HC (p = 0.19) according to Shapiro-Wilk test. One-way ANOVA showed no significant difference in the plasma levels of glutamine among the three groups (F2,53 = 0.64, p = 0.53, η 2 = 0.02). The plasma levels of glycine were normally distributed in FEP (p = 0.52), UHR (p = 0.054), and HC (p = 0.18) according to Shapiro-Wilk test. One-way ANOVA showed no significant difference in the plasma levels of glycine among the three groups (F2,53 = 1.91, p = 0.16, η 2 = 0.07). The plasma levels of D-serine was normally distributed in FEP (p = 0.56), UHR (p = 0.34), and HC (p = 0.70) according to Shapiro-Wilk test. One-way ANOVA showed no significant difference in the plasma levels of D-serine among the three groups (F2,53 = 1.45, p = 0.24, η 2 = 0.05). The plasma levels of L-serine was normally distributed in FEP (p = 0.13), UHR (p = 0.10), and HC (p = 0.81) according to Shapiro-Wilk test. One-way ANOVA showed no significant difference in the plasma levels of L-serine among the three groups (F2,53 = 1.09, p = 0.34, η 2 = 0.04).
The correlations between MMN amplitude and plasma levels of glutamatergic amino acids
The smaller amplitudes of dMMN were significantly associated with higher plasma levels of glutamate in FEP (rs = 0.56, p = 0.01) and HC (rs = 0.55, p = 0.03) (Fig. 3). UHR showed no significant correlations between them (rs = 0.15, p = 0.52) (Fig. 3). We found no significant correlations between MMN amplitudes and the plasma levels of the other glutamatergic amino acids under investigation.
Although 18 patients with FEP and 9 individuals with UHR took antipsychotics, the antipsychotics dose was not significantly correlated with dMMN amplitude (FEP; rs = 0.21, p = 0.39, UHR; rs = 0.38, p = 0.09) or the plasma level of glutamate (FEP; rs = 0.20, p = 0.41, UHR; rs = −0.10, p = 0.67). In contrast, a higher antipsychotics dose was correlated with smaller fMMN amplitude in FEP (rs = 0.51, p = 0.03).
The correlations of clinical symptoms with MMN amplitude and plasma levels of glutamatergic amino acids
Neither MMN amplitude nor glutamate levels was significantly correlated with PANSS positive, negative, general or total in FEP or UHR (−0.27 < rs < 0.36, p > 0.13).
Discussion
The current study found significantly reduced dMMN amplitude and relatively preserved fMMN amplitudes in FEP and UHR. We also observed increased plasma levels of glutamate in FEP. Importantly, smaller dMMN amplitudes were associated with higher plasma levels of glutamate in FEP. These findings are compatible with the glutamatergic dysfunction hypothesis of schizophrenia, and confirm that dMMN is a useful biomarker of aberrant glutamatergic neurotransmission in the early stages of schizophrenia.
FEP and UHR showed significantly smaller dMMN amplitude and relatively intact fMMN amplitude compared to HC. These results are in line with previous studies16, 26, 27. Previous studies have shown that dMMN amplitude predicts the onset of psychosis in individuals with ultra-high risk21, and that fMMN amplitude may be associated with chronicity1.
The plasma level of glutamate of FEP was significantly higher than that of HC. The result is compatible with previous reports, which showed increased serum levels of glutamate in chronic schizophrenia patients28, 29. A couple of reports have attempted and failed to replicate these findings30, 31; however, a recent meta-analysis confirmed that the peripheral glutamate level of schizophrenia subjects was significantly higher than that of HC24. While these are findings pertain to chronic schizophrenia, we found increased glutamate levels in FEP. Since the present study used peripheral blood samples, it is uncertain whether the concentration of glutamate in the brain was also elevated. However, previous studies reported the peripheral glutamate levels were significantly correlated with cerebrospinal fluid (CSF) levels of glutamate32, 33. Furthermore, a recent meta-analysis reported that in schizophrenia, there were significant elevations in glutamate in the basal ganglia and no region showed a reduction in glutamate metabolites34. Therefore, the higher plasma glutamate concentration established in the present study might, at least in part, reflect an elevated glutamate level in the brain of FEP subjects.
Plasma levels of glutamine, glycine, D-serine, and L-serine showed no significant differences between FEP, UHR, and HC. Previous studies of peripheral levels of these glutamatergic amino acids in schizophrenia have yielded mixed findings: glutamine: significantly lower than HC35, comparable with HC31; glycine: higher36, lower37, comparable38; D-serine: higher36, lower31, 38, 39; L-serine: higher40, comparable39. Additionally, Hashimoto et al.41 reported that CSF glutamine levels were not different between schizophrenia subjects and HC. A recent meta-analysis showed the peripheral and CSF levels of glycine, D-serine, and L-serine were not significantly different between schizophrenia subjects and HC23, which corroborates our findings.
The most important finding of this study is that lower dMMN amplitudes were associated with higher plasma glutamate levels in FEP, although this inverse correlation did not appear to be specific to FEP; it was also observed in HC. There was no such association in UHR. To the authors’ knowledge, this is the first study that has reported the correlation between MMN amplitude and peripheral glutamate level in psychotic disorders. Although the molecular mechanism underlying the increased plasma level of glutamate in schizophrenia patients remains elusive, administration of NMDA receptor antagonists increased the concentration of glutamate in the prefrontal cortex in animals42, 43. Furthermore, administration of NMDA receptor antagonists attenuates MMN amplitude6, 7, 44. Therefore, hypofunction of NMDA receptors might cause increased plasma levels of glutamate and reduced MMN amplitude in FEP. The plasma level of glycine, D-serine and L-serine neither decrease nor correlate with MMN amplitude in FEP or UHR. These results suggest that NMDA hypofunction in schizophrenia may not due to the decrease of NMDA receptor co-agonists. The plasma level of glutamine also showed no significant correlation with MMN amplitude in FEP or UHR. Because glutamine has no agonistic activity at NMDA receptors, the plasma level of glutamine may not reflect NMDA receptor function.
Although dMMN amplitude was lower and the plasma level of glutamate was higher in FEP compared to HC, not all patients with FEP had reduced amplitude of dMMN and increased level of glutamate (Fig. 3). These results suggest that not all patients with FEP but a subset of FEP may have hypofunction of NMDA receptors. Therefore, dMMN and the plasma level of glutamate may serve as biomarkers to differentiate individuals with hypofunction of NMDA receptors from individuals without hypofunction of NMDA receptors in patients with FEP. According to a recent meta-analysis, glutamate positive modulators may not be effective in reversing overall cognitive impairments in patients with schizophrenia45. However, glutamate positive modulators may be effective only in a subset of the patients who has NMDA receptor hypofunction. The plasma level of glutamate and dMMN may be useful for identifying this subset. Future clinical trials using dMMN and the plasma level of glutamate as biomarkers will be useful for developing new treatments that modulate NMDA receptor function. These stratified clinical trials based on biomarkers will lead to precision medicine for early stages of psychosis that is the objective of the Research Domain Criteria (RDoC)46.
We investigated association between MMN and glutamatergic amino acids in psychosis based on glutamatergic hypothesis of schizophrenia. However, previous studies reported the reduced amplitude of MMN in other mental disorders such as bipolar disorder47. In addition, bipolar disorder also shows aberrant glutamate transmission48. Therefore, the association between reduced amplitude of MMN and increased plasma level of glutamate may not be specific to psychosis. However, future studies with a sample including various mental disorders will be needed to investigate the specificity of the association between reduced amplitude of MMN and increased plasma level of glutamate.
We have several limitations in this study. First, although the antipsychotics dose was not significantly correlated with dMMN amplitude, nor with the plasma level of glutamate, correlational analyses may be insufficient to clarify potential medication effects. Further studies with drug-naïve participants would be necessary to investigate whether the association between dMMN and plasma level of glutamate reflect NMDA pathology of schizophrenia or potential medication effects. Second, since the present study is a cross-sectional one, the association between dMMN amplitude and plasma level of glutamate is correlative. A longitudinal study, currently underway in our laboratory, will clarify the association during the early stages of schizophrenia. Third, a sample size was small in this study. Further studies with a large sample size will be needed to confirm the correlation between MMN and the plasma level of glutamate.
In conclusion, we found reduced dMMN amplitude and increased plasma level of glutamate in FEP, and a significant association between the two indices. These findings suggest that dMMN and plasma glutamate levels may be useful biological markers for altered glutamatergic neurotransmission in the early stages of schizophrenia. If replicable in larger-scale studies, they may represent promising candidates for biomarkers to be utilized in real-world clinical settings, which has, thus far, been a great challenge in psychiatry.
Methods
Participants
Nineteen patients with FEP, 21 individuals with UHR and 16 healthy controls (HC) participated in this study (Table 1). MMNs from a subset of these participants were previously published16. Thirteen FEP, 7 UHR and 10 HC were included in the previous study who agreed to blood drawing and the examination of the plasma level of amino acids, and the rest were newly recruited for the present study. All participants with FEP or UHR were recruited from The University of Tokyo Hospital. All individuals with UHR, and most patients with FEP, were help-seeking individuals registered at the University of Tokyo Hospital outpatient unit specialized for early intervention. HC were recruited through advertisements placed at several universities near The University of Tokyo. This study was conducted as a part of our large-scale, multimodal, neuroimaging and psychophysiological studies in the early stages of psychosis (Integrative Neuroimaging Studies for Schizophrenia Targeting Early Intervention and Prevention; IN-STEP). Koike et al.49 reported the detail of the recruitment protocol. All subjects gave written informed consent to the Research Ethics Committee of the Faculty of Medicine, The University of Tokyo (approval Nos 629-8, 2094-7, 2226-4) following a complete explanation of this study, and in accordance with the Declaration of Helsinki. Inclusion and exclusion criteria for each group are shown in Table 2. We used the Structured Interview for Prodromal Symptoms (SIPS) as the UHR criteria, which consists of 3 criteria: attenuated psychotic symptoms (APS), brief intermittent psychotic symptoms (BIPS), or genetic risk and deterioration (GRD)50, 51. APS correspond to individuals who exhibited onset or worsened subthreshold psychotic symptoms within 12 months but not psychotic severity. BIPS correspond to individuals who had psychotic symptoms within 3 months but with a limited duration and frequency such that they were not at all or only slightly influenced by their symptoms and did not meet the psychotic episode criteria according to the DSM-IV criteria52. GRD corresponds to individuals whose functioning had deteriorated in the previous 12 months as defined by a 30% or more decrease in the GAF score52 as well as those who also had one or more first-degree relatives diagnosed with psychosis and/or schizotypal personality disorder according to the DSM-IV criteria.
Audiometer testing was used to ensure that all participants had normal hearing in both ears and could detect 30-dB sound pressure level tone at 1000 Hz and 40-dB at 4000 Hz. Eighteen FEP and 9 UHR subjects were prescribed second-generation antipsychotic medications at the time of testing. No other antipsychotic was prescribed. All patients with FEP were diagnosed by experienced psychiatrists according to the DSM-IV criteria. Out of 19 FEP patients, 17 patients had first-episode schizophrenia, and 2 patients had schizophreniform disorder. Estimated premorbid intelligence quotient (IQ) was assessed with the Japanese version of the National Adult Reading Test53, 54 FEP and UHR participants were assessed with regards to their functioning and symptoms, using the Global Assessment of Functioning (GAF)52 and the Positive and Negative Syndrome Scale (PANSS)55. These clinical ratings were measured by experienced psychiatrists (T.N., M.T., and D.K.). To control the quality of data assessment, we used video interviews to ensure the scoring of the clinical ratings and calculated the inter-rater reliability of the clinical ratings (Cronbach alpha = 0.86)49.
Measurement of the plasma levels of amino acids
We measured plasma levels of the peripheral glutamatergic amino acids glutamate, glutamine, glycine, D-serine, and L-serine. Measurement of the plasma levels of glutamate, glutamine, and glycine was carried out using a column-switching high performance liquid chromatography (HPLC) system (Shimadzu Corporation, Kyoto, Japan) with fluorescence detection, as has been previously reported41. Measurement of D-serine and L-serine was carried out using a HPLC system, as has been previously reported39, 56. In order to minimize the effect of amino acids originating from food sources, we obtained fastening (>3 h without any meals and/or nutritious drinks) blood samples, as has been previously reported57.
Stimuli and Procedure
For duration MMN (dMMN), a two-tone auditory oddball paradigm with 2000 stimuli was used. Ninety percent of the stimuli were standard tones (1000 Hz, 50 ms) and 10% of the stimuli were deviant tones (1000 Hz, 100 ms). For frequency MMN (fMMN), another two-tone auditory oddball paradigm with 2000 stimuli was used. Ninety percent of the stimuli were standard tones (1000 Hz, 50 ms) and 10% of the stimuli were deviant tones (1200 Hz, 50 ms). All the stimuli were of 80 dB sound pressure level and 1 ms rise/fall time. Stimulus onset asynchrony was 500 ms. These oddball paradigms were counter-balanced. Tones were presented binaurally through earphones while participants watched a silent cartoon.
Electroencephalography recording and analyses
Electroencephalography (EEG) data were acquired with a 64-channel Geodesic EEG System (Electrical Geodesics Inc., Eugene, OR). Electrodes were referenced to the vertex, and impedances were kept below 50 kΩ. The sampling rate was 500 Hz. The analog filter bandpass was set at 0.1–100 Hz. EEGLAB58 was used for EEG processing and data analysis. The continuous EEG data were re-referenced to an average reference, digitally filtered at 0.1–20 Hz, and segmented from −100 to 500 ms relative to the stimulus onset. The mean of the pre-stimulus baseline was subtracted for baseline correction. Independent component analysis was used for eye blink correction. Epochs exceeding ±100 μV at any electrode were rejected. After averaging across trials, the ERP waveform in response to standard stimuli was subtracted from the ERP waveform in response to deviant stimuli.
For MMN analysis, a front-central electrode (FCz) was selected (the largest amplitude was obtained with this FCz). The dMMN amplitude was measured as the mean voltage from 135 to 205 ms post stimuli, in accordance with previous studies16, 59, 60. The fMMN amplitude was measured as the mean voltage from 100 to 200 ms, in accordance with previous studies16, 61, 62.
Statistical Analyses
We performed Shapiro-Wilk tests to examine whether each variable follows a normal distribution. When the variable followed a normal distribution, we employed independent t-test for comparison between 2 groups and one-way analysis of variance (ANOVA) for comparison among 3 groups. When the variable did not follow a normal distribution, we employed Mann-Whitney test for comparison between 2 groups and Kruskal-Wallis test for comparison among 3 groups. We employed a χ2 test for sex ratio.
When we found significant difference in one-way ANOVA, Post hoc tests with the Bonferroni correction were performed to examine group difference. When we found significant difference in Kruskal-Wallis test, Mann-Whitney tests with the Bonferroni correction were performed to examine group differences.
We reported effect sizes using Cohen’s d for variables with normal distribution, r for variables with non-normal distribution, and η2 for ANOVA.
To assess the association of MMN amplitude with the plasma levels of glutamatergic amino acids, Spearman correlation coefficients were calculated. The significance level was set at p < 0.05.
References
Umbricht, D. & Krljes, S. Mismatch negativity in schizophrenia: a meta-analysis. Schizophr. Res. 76, 1–23, doi:10.1016/j.schres.2004.12.002 (2005).
Naatanen, R. & Kahkonen, S. Central auditory dysfunction in schizophrenia as revealed by the mismatch negativity (MMN) and its magnetic equivalent MMNm: a review. Int. J. Neuropsychopharmacol. 12, 125–135, doi:10.1017/S1461145708009322 (2009).
Nagai, T. et al. Mismatch negativity as a “translatable” brain marker toward early intervention for psychosis: a review. Front. Psychiatry. 4, 115, doi:10.3389/fpsyt.2013.00115 (2013).
Light, G. A. & Swerdlow, N. R. Future clinical uses of neurophysiological biomarkers to predict and monitor treatment response for schizophrenia. Ann. N. Y. Acad. Sci. 1344, 105–119, doi:10.1111/nyas.2015.1344.issue-1 (2015).
Javitt, D. C. & Sweet, R. A. Auditory dysfunction in schizophrenia: integrating clinical and basic features. Nat. Rev. Neurosci. 16, 535–550, doi:10.1038/nrn4002 (2015).
Umbricht, D. et al. Ketamine-induced deficits in auditory and visual context-dependent processing in healthy volunteers: implications for models of cognitive deficits in schizophrenia. Arch. Gen. Psychiatry. 57, 1139–1147, doi:10.1001/archpsyc.57.12.1139 (2000).
Javitt, D. C., Steinschneider, M., Schroeder, C. E. & Arezzo, J. C. Role of cortical N-methyl-D-aspartate receptors in auditory sensory memory and mismatch negativity generation: implications for schizophrenia. Proc. Natl. Acad. Sci. USA 93, 11962–11967, doi:10.1073/pnas.93.21.11962 (1996).
Gil-da-Costa, R., Stoner, G. R., Fung, R. & Albright, T. D. Nonhuman primate model of schizophrenia using a noninvasive EEG method. Proc. Natl. Acad. Sci. USA 110, 15425–15430, doi:10.1073/pnas.1312264110 (2013).
Konradi, C. & Heckers, S. Molecular aspects of glutamate dysregulation: implications for schizophrenia and its treatment. Pharmacol. Ther. 97, 153–179, doi:10.1016/S0163-7258(02)00328-5 (2003).
Coyle, J. T. Glutamate and schizophrenia: beyond the dopamine hypothesis. Cell. Mol. Neurobiol. 26, 365–384, doi:10.1007/s10571-006-9062-8 (2006).
Kantrowitz, J. T. & Javitt, D. C. N-methyl-d-aspartate (NMDA) receptor dysfunction or dysregulation: the final common pathway on the road to schizophrenia? Brain. Res. Bull. 83, 108–121, doi:10.1016/j.brainresbull.2010.04.006 (2010).
Javitt, D. C., Zukin, S. R., Heresco-Levy, U. & Umbricht, D. Has an angel shown the way?Etiological and therapeutic implications of the PCP/NMDA model of schizophrenia. Schizophr. Bull. 38, 958–966, doi:10.1093/schbul/sbs069 (2012).
Hashimoto, K. Targeting of NMDA receptors in new treatments for schizophrenia. Expert Opin. Ther. Targets. 18, 1049–1063, doi:10.1517/14728222.2014.934225 (2014).
Erickson, M. A., Ruffle, A. & Gold, J. M. A meta-analysis of mismatch negativity in schizophrenia: from clinical risk to disease specificity and progression. Biol Psychiatry. 79, 980–987, doi:10.1016/j.biopsych.2015.08.025 (2016).
Haigh, S. M., Coffman, B. A. & Salisbury, D. F. Mismatch negativity in first-episode schizophrenia: a meta-analysis. Clin EEG Neurosci. 48, 3–10, doi:10.1177/1550059416645980 (2017).
Nagai, T. et al. Auditory mismatch negativity and P3a in response to duration and frequency changes in the early stages of psychosis. Schizophr. Res. 150, 547–554, doi:10.1016/j.schres.2013.08.005 (2013).
Miyanishi, T., Sumiyoshi, T., Higuchi, Y., Seo, T. & Suzuki, M. LORETA current source density for duration mismatch negativity and neuropsychological assessment in early schizophrenia. PLoS. One. 8, e61152, doi:10.1371/journal.pone.0061152 (2013).
Perez, V. B. et al. Automatic auditory processing deficits in schizophrenia and clinical high-risk patients: forecasting psychosis risk with mismatch negativity. Biol. Psychiatry. 75, 459–469, doi:10.1016/j.biopsych.2013.07.038 (2014).
Rudolph, E. D. et al. Finding the missing-stimulus mismatch negativity (MMN) in early psychosis: Altered MMN to violations of an auditory gestalt. Schizophr. Res. 166, 158–163, doi:10.1016/j.schres.2015.05.028 (2015).
Hay, R. A. et al. Equivalent mismatch negativity deficits across deviant types in early illness schizophrenia-spectrum patients. Biol. Psychol. 105, 130–137, doi:10.1016/j.biopsycho.2015.01.004 (2015).
Bodatsch, M., Brockhaus-Dumke, A., Klosterkötter, J. & Ruhrmann, S. Forecasting psychosis by event-related potentials –systemic review and specific meta-analysis. Biol. Psychiatry. 77, 951–958, doi:10.1016/j.biopsych.2014.09.025 (2015).
Salisbury, D. F., Kuroki, N., Kasai, K., Shenton, M. E. & McCarley, R. W. Progressive and interrelated functional and structural evidence of post-onset brain reduction in schizophrenia. Arch. Gen. Psychiatry. 64, 521–529, doi:10.1001/archpsyc.64.5.521 (2007).
Brouwer, A., Luykx, J. J., van Boxmeer, L., Bakker, S. C. & Kahn, R. S. NMDA-receptor coagonists in serum, plasma, and cerebrospinal fluid of schizophrenia patients: a meta-analysis of case-control studies. Neurosci. Biobehav. Rev. 37, 1587–1596, doi:10.1016/j.neubiorev.2013.06.007 (2013).
Song, J., Viggiano, A., Monda, M. & De Luca, V. Peripheral glutamate levels in schizophrenia: evidence from a meta-analysis. Neuropsychobiology. 70, 133–141, doi:10.1159/000364828 (2014).
Moghaddam, B. & Krystal, J. H. Capturing the angel in “angel dust”: twenty years of translational neuroscience studies of NMDA receptor antagonists in animals and humans. Schizophr. Bull. 38, 942–949, doi:10.1093/schbul/sbs075 (2012).
Todd, J. et al. Deviant matters: duration, frequency, and intensity deviants reveal different patterns of mismatch negativity reduction in early and late schizophrenia. Biol. Psychiatry. 63, 58–64, doi:10.1016/j.biopsych.2007.02.016 (2008).
Bodatsch, M. et al. Prediction of psychosis by mismatch negativity. Biol. Psychiatry. 69, 959–966, doi:10.1016/j.biopsych.2010.09.057 (2011).
Macciardi, F. et al. Amino acid patterns in schizophrenia: some new findings. Psychiatry. Res. 32, 63–70, doi:10.1016/0165-1781(90)90136-S (1990).
Tortorella, A. et al. Plasma concentrations of amino acids in chronic schizophrenics treated with clozapine. Neuropsychobiology. 44, 167–171, 54937 (2001).
Altamura, C. A. et al. Plasma and platelet excitatory amino acids in psychiatric disorders. Am. J. Psychiatry. 150, 1731–1733, doi:10.1176/ajp.150.11.1731 (1993).
Yamamori, H. et al. Changes in plasma D-serine, L-serine, and glycine levels in treatment-resistant schizophrenia before and after clozapine treatment. Neurosci. Lett. 582, 93–98, doi:10.1016/j.neulet.2014.08.052 (2014).
McGale, E. H., Pye, I. F., Stonier, C., Hutchinso, E. C. & Aber, G. M. Studies of the inter-relationship between cerebrospinal fluid and plasma amino acid concentrations in normal individuals. J. Neurochem. 29, 291–297, doi:10.1111/jnc.1977.29.issue-2 (1977).
Alfredsson, G., Wiesel, F. A. & Lindberg, M. Glutamate and glutamine in cerebrospinal fluid and serum from healthy volunteers–analytical aspects. J. Chromatogr. 424, 378–384, doi:10.1016/S0378-4347(00)81116-0 (1988).
Merritt, K., Egerton, A., Kempton, M. J., Taylor, M. J. & McGuire, P. K. Nature of glutamate alterations in schizophrenia: a meta-analysis of proton magnetic resonance spectroscopy studies. JAMA. Psychiatry. 73, 665–674, doi:10.1001/jamapsychiatry.2016.0442 (2016).
He, Y. et al. Schizophrenia shows a unique metabolomics signature in plasma. Transl. Psychiatry. 2, e149, doi:10.1038/tp.2012.76 (2012).
Ohnuma, T. et al. Changes in plasma glycine, L-serine, and D-serine levels in patients with schizophrenia as their clinical symptoms improve: results from the Juntendo University Schizophrenia Projects (JUSP). Prog. Neuropsychopharmacol. Biol. Psychiatry. 32, 1905–1912, doi:10.1016/j.pnpbp.2008.07.022 (2008).
Hons, J. et al. Glycine serum level in schizophrenia: relation to negative symptoms. Psychiatry. Res. 176, 103–108, doi:10.1016/j.psychres.2009.11.008 (2010).
Tomiya, M. et al. Alterations in serum amino acid concentrations in male and female schizophrenic patients. Clin. Chim. Acta. 380, 186–190, doi:10.1016/j.cca.2007.02.011 (2007).
Yamada, K. et al. Identification of multiple serine racemase (SRR) mRNA isoforms and genetic analyses of SRR and DAO in schizophrenia and D-serine levels. Biol. Psychiatry. 57, 1493–1503, doi:10.1016/j.biopsych.2005.03.018 (2005).
Hashimoto, K. et al. Decreased serum levels of D-serine in patients with schizophrenia: evidence in support of the N-methyl-D-aspartate receptor hypofunction hypothesis of schizophrenia. Arch. Gen. Psychiatry. 60, 572–576, doi:10.1001/archpsyc.60.6.572 (2003).
Hashimoto, K. et al. Elevated glutamine/glutamate ratio in cerebrospinal fluid of first episode and drug naive schizophrenic patients. BMC. Psychiatry. 5, 6, doi:10.1186/1471-244X-5-6 (2005).
Moghaddam, B., Adams, B., Verma, A. & Daly, D. Activation of glutamatergic neurotransmission by ketamine: a novel step in the pathway from NMDA receptor blockade to dopaminergic and cognitive disruptions associated with the prefrontal cortex. J. Neurosci. 17, 2921–2927 (1997).
Lorrain, D. S., Baccei, C. S., Bristow, L. J., Anderson, J. J. & Varney, M. A. Effects of ketamine and N-methyl-D-aspartate on glutamate and dopamine release in the rat prefrontal cortex: modulation by a group II selective metabotropic glutamate receptor agonist LY379268. Neuroscience. 117, 697–706, doi:10.1016/S0306-4522(02)00652-8 (2003).
Schmidt, A. et al. Mismatch negativity encoding of prediction errors predicts S-ketamine-induced cognitive impairments. Neuropsychopharmacology. 37, 865–875, doi:10.1038/npp.2011.261 (2012).
Iwata, Y. et al. Effects of glutamate positive modulators on cognitive deficits in schizophrenia: a systematic review and meta-analysis of double-blind randomized controlled trials. Mol. Psychiatry. 20, 1151–1160, doi:10.1038/mp.2015.68 (2015).
Insel, T. R. & Cuthbert, B. N. Medicine. Brain disorders? Precisely. Science. 348, 499–500, doi:10.1126/science.aab2358 (2015).
Erickson, M. A., Ruffle, A. & Gold, J. M. A meta-analysis of mismatch negativity in schizophrenia: from clinical risk to disease specificity and progression. Biol. Psychiatry. 79, 980–987, doi:10.1016/j.biopsych.2015.08.025 (2015).
Chitty, K. M., Lagopoulos, J., Lee, R. S., Hickie, I. B. & Hermens, D. F. A systematic review and meta-analysis of proton magnetic resonance spectroscopy and mismatch negativity in bipolar disorder. Eur. Neuropsychopharmacol. 23, 1348–1368, doi:10.1016/j.euroneuro.2013.07.007 (2013).
Koike, S. et al. A multimodal approach to investigate biomarkers for psychosis in a clinical setting: the integrative neuroimaging studies in schizophrenia targeting for early intervention and prevention (IN-STEP) project. Schizophr. Res. 143, 116–124, doi:10.1016/j.schres.2012.11.012 (2013).
Miller, T. J. et al. Symptom assessment in schizophrenic prodromal states. Psychiatr. Q. 70, 273–287, doi:10.1023/A:1022034115078 (1999).
Kobayashi, H., Nozaki, S. & Mizuno, M. Reliability of the Structured Interview for Prodromal Syndromes Japanese version (SIPS-J). Jpn. Bull. Soc. Psychiatry. 15, 168–174 (2007).
American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, 4th ed. (American Psychiatric Press, 1994).
Matsuoka, K., Uno, M., Kasai, K., Koyama, K. & Kim, Y. Estimation of premorbid IQ in individuals with Alzheimer’s disease using Japanese ideographic script (Kanji) compound words: Japanese version of National Adult Reading Test. Psychiatry. Clin. Neurosci. 60, 332–339, doi:10.1111/pcn.2006.60.issue-3 (2006).
Uetsuki, M. et al. Estimation of premorbid IQ by JART in schizophrenia. Seishin. Igaku. 48, 15–22 (2006).
Kay, S. R., Fiszbein, A. & Opler, L. A. The positive and negative syndrome scale (PANSS) for schizophrenia. Schizophr. Bull. 13, 261–276, doi:10.1093/schbul/13.2.261 (1987).
Fukushima, T., Kawai, J., Imai, K. & Toyo’oka, T. Simultaneous determination of D- and L-serine in rat brain microdialysis sample using a column-switching HPLC with fluorimetric detection. Biomed. Chromatogr. 18, 813–819, doi:10.1002/bmc.394 (2004).
Koike, S. et al. A snapshot of plasma metabolites in first-episode schizophrenia: a capillary electrophoresis time-of-flight mass spectrometry study. Transl. Psychiatry. 4, e379, doi:10.1038/tp.2014.19 (2014).
Delorme, A. & Makeig, S. EEGLAB: an open source toolbox for analysis of single-trial EEG dynamics including independent component analysis. J. Neurosci. Methods. 134, 9–21, doi:10.1016/j.jneumeth.2003.10.009 (2004).
Michie, P. T., Innes-Brown, H., Todd, J. & Jablensky, A. V. Duration mismatch negativity in biological relatives of patients with schizophrenia spectrum disorders. Biol. Psychiatry. 52, 749–758, doi:10.1016/S0006-3223(02)01379-3 (2002).
Light, G. A. & Braff, D. L. Mismatch negativity deficits are associated with poor functioning in schizophrenia patients. Arch. Gen. Psychiatry. 62, 127–136, doi:10.1001/archpsyc.62.2.127 (2005).
Hirayasu, Y. et al. Auditory mismatch negativity in schizophrenia: topographic evaluation with a high-density recording montage. Am. J. Psychiatry. 155, 1281–1284, doi:10.1176/ajp.155.9.1281 (1998).
Salisbury, D. F., Shenton, M. E., Griggs, C. B., Bonner-Jackson, A. & McCarley, R. W. Mismatch negativity in chronic schizophrenia and first-episode schizophrenia. Arch. Gen. Psychiatry. 59, 686–694, doi:10.1001/archpsyc.59.8.686 (2002).
Acknowledgements
This research is supported by the Brain Mapping by Integrated Neurotechnologies for Disease Studies (Brain/MINDS) from Japan Agency for Medical Research and Development (AMED) (K.Ka). This work was also in part supported by Grant-in-Aid for scientific Research on Innovative Areas (23118001 & 23118004; Adolescent Mind & Self-Regulation) from the Ministry of Education, Culture, Sports, Science and Technology of Japan (K.Ka); JSPS KAKENHI Grant numbers JP16H06395, 16H06399, 16K21720 (K.Ka), 25860990, 15K19713 (K.Ki). We thank the members of the Integrative Neuroimaging Studies for Schizophrenia Targeting Early Intervention and Prevention (IN-STEP) research team at The University of Tokyo Hospital for their advice and assistance. We gratefully acknowledge all the participants of this study. We thank Ms. Yuko Fujita for her technical assistance with the measurement of amino acid levels.
Author information
Authors and Affiliations
Contributions
K.Ka. had full access to all the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis. Study concept and design: T.A. and K.Ka. Acquisition, analysis, or interpretation of data: T.N., K.Ki., M.T., D.K., S.K. M.S., T.A. and K.H. Drafting of the manuscript: T.N., K.Ki. and K.Ka. Statistical analysis: T.N., K.Ki and K.Kai. Obtained funding: K.Ki., K.Ka.
Corresponding author
Ethics declarations
Competing Interests
T.A. is affiliated with the Department of Youth Mental Health, which is an endowment department supported by an unrestricted grant from Otsuka Pharmaceutical Co., Ltd. The other authors reported no biomedical financial interests or potential conflicts of interest related to the study.
Additional information
Publisher's note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Nagai, T., Kirihara, K., Tada, M. et al. Reduced Mismatch Negativity is Associated with Increased Plasma Level of Glutamate in First-episode Psychosis. Sci Rep 7, 2258 (2017). https://doi.org/10.1038/s41598-017-02267-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-017-02267-1
This article is cited by
-
Longitudinal trajectories of anterior cingulate glutamate and subclinical psychotic experiences in early adolescence: the impact of bullying victimization
Molecular Psychiatry (2024)
-
Mouse mutants in schizophrenia risk genes GRIN2A and AKAP11 show EEG abnormalities in common with schizophrenia patients
Translational Psychiatry (2023)
-
Atypical prediction error learning is associated with prodromal symptoms in individuals at clinical high risk for psychosis
Schizophrenia (2022)
-
Recent advancements in biomarker research in schizophrenia: mapping the road from bench to bedside
Metabolic Brain Disease (2022)
-
mGluR5 binding changes during a mismatch negativity task in a multimodal protocol with [11C]ABP688 PET/MR-EEG
Translational Psychiatry (2022)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.