Abstract
This study evaluated the performance of plusoptiX A12C in detecting amblyopia risk factors (ARFs) in Chinese children aged 3-to-4-year. PlusoptiX examination was successfully conducted among 1,766 subjects without cycloplegia to detect refractive error, asymmetry and media opacity. Cycloplegic retinoscopy (CR) was conducted on 357 children suspected of having vision abnormalities. Statistical differences between CR and the device were confirmed using the mean spherical value (+1.41 ± 0.87 D versus +1.14 ± 0.81 D), cylindrical value (−0.47 ± 0.64 versus −0.84 ± 0.78) and spherical equivalent (SE) value (+1.17 ± 0.84 D versus +0.72 ± 0.64 D) (all P < 0.0001). In the emmetropia group, the differences were statistically significant for the cylinder and SE (all P < 0.0001) but not the sphere (P = 0.33). In the hyperopia group, the differences were statistically significant for the sphere, cylinder and SE (all P < 0.0001). For refractive and strabismic ARFs detection, the sensitivity, specificity, positive predictive value, and negative predictive value were calculated, respectively.
Similar content being viewed by others
Introduction
Approximately 1% to 3% of preschool-aged children have amblyopia1, a neurological vision disorder attributed to abnormal binocular interaction or visual deprivation during early life. Amblyopia causes vision loss and impaired binocular function in both childhood and adult populations. Although conducting vision screening in school children more than 6 years old is easier, evidence suggests that younger children are more responsive to amblyopia treatment than children older than 72, 3. However, conducting successful visual acuity test in children by using a vision chart is challenging and highly dependent on the cooperation of the children and the experience of the screener.
Instrument-based screening is quick and requires minimal cooperation of the child; therefore, children younger than 4 years old can benefit from this method4. The plusoptiX photoscreener, a newly designed screening tool, can assess both eyes simultaneously and is approved by the US Food and Drug Administration. This device uses infrared images of the eye’s red reflex to estimate refractive error, media opacity, ocular alignment and other factors, such as ptosis, all of which increases the risk of a child from developing amblyopia.
Many studies have investigated the performance of the plusoptiX photoscreener for detecting amblyopia risk factors (ARFs)5. Given the update of the guidelines of the American Association for Pediatric Ophthalmology and Strabismus (AAPOS) for automated preschool vision screening in 2013, evaluating this device according to the new criteria is necessary6. However, the plusoptiX photoscreener has not been applied widely in China, and the only device reporting on the performance of this device in Chinese children utilized the AAPOS 2003 guidelines7. Meanwhile, the sixth generation of the devices, including S12 and A12, have not been evaluated fully.
In the present study, we evaluate the performance of the plusoptiX A12C in detecting ARFs in Chinese children aged 3 to 4 years on the basis of the 2013 AAPOS guidelines. This analysis is part of the ongoing prospective Yuhuatai Pediatric Eye Disease Study (YPEDS).
Results
Characteristics of study population
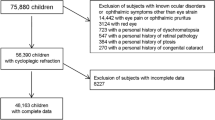
A total of 1,818 children aged 3 to 4 years (mean age ± SD: 40.85 ± 3.43 months) agreed to undergo comprehensive eye examinations. Among the subjects, the number of boys (969, 53.3%) is slightly greater than the girls (849, 46.7%). In the 1,818 children, 11 uncooperative children were not tested by the plusoptiX (testability: 99.39%). Among the remaining 1,807 children, the plusoptiX A12C failed to test 41 children (Table 1).
Comparison between the plusoptiX and cycloplegic retinoscopy
Cycloplegic retinoscopy (CR) was available in 357 (20.24%) of the 1,764 children. The plusoptiX and CR were then compared (Table 2). Statistical differences between CR and plusoptiX were confirmed in the mean spherical value (+1.41 ± 0.87 D versus +1.14 ± 0.81 D; average difference, 0.27 D; P < 0.0001), mean cylindrical value (−0.47 ± 0.64 versus −0.84 ± 0.78; average difference, 0.37 D; P < 0.0001) and mean SE value (+1.17 ± 0.84 D versus +0.72 ± 0.64 D; average difference, 0.46 D; P < 0.0001).
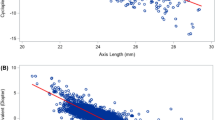
Figure 1 shows the agreement between the measurements. The 95% limit of agreement (LOA) (CRSphere − Psphere) of the mean spherical value ranged from −1.59 D to +2.13 D in 277 cases with ±1.00 D (77.59%); the 95% LOA (CRcylinder − Pcylinder) of the cylindrical value ranged from −0.73 D to +1.47 D in 331 cases with ±1.00 D (92.72%); the 95% LOA (CRSE − PSE) of the SE value ranged from −1.24 D to +2.16 D in 270 cases with ±1.00 D (75.63%).
According to the SE results, the 357 children were classified into 3 subgroups. In the myopia group of 3 children, the differences were not statistically significant for the sphere (−0.42 ± 1.13 D versus −0.33 ± 1.61 D; average difference, 0.08 D; P = 0.84), cylinder (−1.50 ± 1.80 D versus −1.67 ± 1.15 D; average difference, 0.17 D; P = 0.74) and SE (−1.17 ± 0.29 D versus −1.17 ± 1.04 D; average difference, 0.00 D; P = 1.00). In the emmetropia group of 298 children, the differences were statistically significant for the cylinder (−0.47 ± 0.64 D versus −0.86 ± 0.80 D; average difference, 0.39 D; P < 0.0001) and SE (0.94 ± 0.54 D versus −0.70 ± 0.59 D; average difference, 0.24 D; P < 0.0001) but not the sphere (1.17 ± 0.59 D versus 1.13 ± 0.78 D; average difference, 0.05 D; P = 0.33). In the hyperopia group of 56 children, the differences were statistically significant for the sphere (2.77 ± 0.80 D versus 1.29 ± 0.82 D; average difference, 1.48 D; P < 0.0001), cylinder (−0.44 ± 0.55 D versus −0.72 ± 0.62 D; average difference, 0.28 D; P < 0.05) and SE (2.55 ± 0.69 D versus 0.93 ± 0.69 D; average difference, 1.62 D; P < 0.0001).
Detection of refractive ARFs
Among the 1,766 tested children, 359 whose refractive measurement values were available or out of range of the device’s setting were included in the analysis of the accuracy of detecting refractive ARFs.
Only 14 children were confirmed to have refractive ARFs according to the criteria of AAPOS (3.90%), including those without myopia, 2 with hyperopia, 10 with astigmatism and 3 with anisometropia. One child was simultaneously diagnosed with hyperopia and anisometropia. The sensitivity and specificity values are displayed in Table 3. The sensitivity ranged from 92.86% to 100%, specificity ranged from 49.57% to 94.49%, positive predictive value (PPV) ranged from 7.45% to 40.63% and negative predictive value (NPV) ranged from 99.69% to 100%, according to the different referral criteria recommended by the manufacturer (Table 3)6, 8. The analysis of the adjusted optimal cutoff for detecting refractive ARFs was not conducted because of the small sample size of children with refractive ARFs.
Detection of strabismic ARFs
In addition to the 1,766 successfully tested children, 13 children had refractions that were not measured but had asymmetry measurements that were included in the analysis for the detection of strabismic ARFs. In the 1,779 children, 48 children were diagnosed with strabismus, including 44 with intermittent exotropia, 1 with constant exotropia and 3 with esotropia. However, only 1 child with accommodative esotropia was referred by the device on the basis of the ≥10° criteria for asymmetry (sensitivity 25.00%, specificity 99.83%, PPV 25.00%, NPV 99.83%). Three other children with intermittent exotropia met the ≥5° criteria of asymmetry recommended by the manufacturer (sensitivity 100.00%, specificity 96.11%, PPV 5.48%, NPV 100.00%) (Table 4).
Children testing failing
Table 5 provides the detailed diagnosis of the 41 children who failed the test and 11 untested children. Among these children, 20 have vision abnormalities, including 12 with amblyopia, 2 with myopia, 7 with hyperopia, 7 with astigmatism, 6 with anisometropia, 4 with strabismus and 2 with congenital persistent pupillary membrane. The other 28 children were identified to have normal vision.
Discussion
The present study evaluated the performance of the plusoptiX A12C in detecting ARFs in preschool Chinese children. As the sixth generation product, the plusoptiX A12C is a portable instrument with rechargeable batteries and requires half the time of the VA-based vision screening. Thus, the plusoptiX A12C can be applied not only in clinical settings but also in community settings9. This device uses a smiling face with flashing lights as the fixation target and has a warble sound to catch the attention of young children. The average number of screenings to obtain a reliable result was less than three in 3-year-old children10. In this study, almost all children were testable (testability: 99.39%); this finding was consistent with previous reports11, 12.
The plusoptiX has been reported by the majority of studies to underestimate children’s refractive error and to have higher accuracy in myopic children than hyperopic children13,14,15. In the present study, the plusoptiX A12C led to a considerable shift towards myopic values (0.45 D), particularly in the hyperopia group (1.62 D), because of normal accommodation. The obvious disparity should be counteracted by appropriate cut-off value. During further analysis, the spherical values agreed well with the emmetropia group (P = 0.33) compared with the hyperopia group (P < 0.0001). Regarding the cylindrical results, several researchers agreed with the consistency of the cylindrical power between the device and CR13, 15, whereas others did not16, 17. In the present study, the plusoptiX overestimated the the cylindrical power in all groups, thus resulting in the partial or total underestimation of SE (all P < 0.0001). The consistency of the results in the myopia group was not analysed because of the small sample size of three children in these primarily children.
Given the high prevalence of ARFs at 15% to 20%18, 19, the majority of children with ARFs do not develop amblyopia, as confirmed by a longitudinal follow-up study20. Children with deep amblyopia are less likely to improve by spectacle treatment alone, thus these children must be identified at a younger age21. Results suggest that preschool vision screening devices should aim to detect only the greatest magnitude of anisometropia at younger ages by focusing on high specificity and low sensitivity. Reevaluating the majority of studies on the plusoptiX according to the new guidelines updated in 2013 is necessary to reduce the referral rate for young children by raising the threshold referral values.
Previous studies have reported that the plusoptiX has low sensitivity for detecting strabismus, particularly in strabismus with small angle12, 22. In the present study, the majority of the strabismic children have controllable intermittent exotropia (44/48, 91.67%). In the other 4 children, only 1 child was referred by the device under the criteria as asymmetry ≥10° (sensitivity: 25.00%).
The plusoptiX has been demonstrated to be a useful screening tool compared with other devices, including the Suresight, SPOT, Retinomax and MTI23,24,25,26. Several studies have investigated the accuracy of the plusoptiX in detecting ARFs in the pediatric population by modifying the referral criteria to improve the clinical utility of the device5, 27, 28. The results of these studies suggested that the referral criteria should be chosen according to local conditions and interval of vision screening5, 29. A criteria with higher sensitivity may be more suitable for children with poor access to vision care and vice versa. The sensitivity and specificity of detecting refractive ARFs according to the five criteria recommended by the manufacturer are displayed in Table 3, which shows that the sensitivity ranged from 92.86% to 100%, while the specificity of the criteria of the manufacturer (sensitivity) (49.57%) and Matta/Silbert (57.68%) were lower with the lowest threshold and the criteria of AAPOS 2013 and ABCD 2012 had the highest specificity (AAPOS 2013: 94.49%; ABCD 2012: 90.72%) and PPV (AAPOS 2013: 40.63%; ABCD 2012: 30.43%). In this population-based study, only 14 successfully tested children were confirmed to have refractive ARFs thus increasing the error in analyzing the sensitivity and specificity of the refractive ARFs. By using the AAPOS guidelines updated in 2013, a study on 3-year-old children reported a similar lower PPV of 51% than other studies in representative preschool populations10. Such observations can be explained by the more stringent criteria and earlier age range of these two studies.
Approximately half of the 52 children (2.86%) who were not tested successfully were diagnosed with ARFs, thus indicating that such children with high risk for amblyopia should be referred. The small height of palpebral fissure and the occlusion of eyelashes may explain the failure of assessment in the other half of the children.
The advantages of this study include its population-based design (for strabismic ARFs), one of the largest sample size of preschool children, a specific age norm, the newest device and the adopted guidelines of AAPOS updated in 2013. Additional information was provided regarding the strabismic ARFs and children who were not tested. However, this study has several limitations. Although guaranteed by comprehensive eye examinations including refractive status by table-mounted autorefractor and CR, cycloplegia examination was not performed in all included children, thus causing deviation in the analysis, resulting that the detection of refractive ARFs was actually in clinic settings. Only strabismic ARFs was detecting in screening settings. Furthermore, due to the low incidence of refractive error and strabismus in a healthy population, the number of children identified with ARFs was too small to evaluate the accuracy of this device and adjust the optimal cut-off for detecting both refractive and strabismic ARFs. Moreover, the subgroups by refractive state suffers from very unequal sample sizes limited by the specific age norm.
In conclusion, this investigation has shown the statistically significant difference in SE values between the plusoptiX A12C and CR in Chinese children aged 3 to 4 years. We found that the device was accurate in evaluating the spherical value of children with emmetropia. Children who failed the test or were untested should be considered to be at high risk for amblyopia. By using the appropriate criteria, the plusoptiX A12C can be a useful device for detecting refractive ARFs but not strabismic ARFs in preschool children aged 3 to 4 years.
Methods
Study design and population
The YPEDS is a population-based vision screening study that aims to establish a systematic database on refraction, visual acuity, ocular biometric parameters, ocular position and other ophthalmic measures. This study also aims to explore the rule for vision development and estimate the occurrence of common pediatric ocular disorders in preschool children aged 3 to 6 years in the Yuhuatai District, Nanjing, China. The YPEDS used inclusion and exclusion criteria similar to those employed in the MEPEDS30. After confirmation from parents or legal guardians that the participants are all residents of Yuhuatai District, all children born between September 2011 and August 2012 and those about to enter kindergarten in Yuhuatai District were invited to participate in the study and to undergo comprehensive health examination and vision examination. All children were 3-to-4-year during the examinations.
This study was approved by the Ethics Committee of Nanjing Medical University and was conducted in accordance to the tenets of the Declaration of Helsinki. Written informed consent was obtained from the parents or legal representatives of all participating children.
Examination
Comprehensive eye examinations were performed by a team of two optometrists and two ophthalmologists who were trained and certified using standardized study protocols as previously described in the MEPEDS30. Basic participant information including name, gender, nation, birth day and examination date, was recorded during the clinical visit. The examinations included anthropometric parameters, distance visual acuity (using HOTV VA chart at a distance of 3 m), anterior segment examination, autorefraction, plusoptix A12C photorefraction (PlusoptiX GmbH, Nuremberg, Germany), cover test at distant and near fixation, ocular motility, fundus examination and ocular biometric parameters.
The plusoptiX A12C was placed at a distance of 1 meter in front of the children under dim ambient light. Examination with the device was conducted simultaneously on both eyes by a trained optometrist in accordance with the manufacturer’s instructions. The refraction setting ranged from −7.00 D to +5.00 D for spherical and cylindrical values, respectively, with increments of 0.25 D. The asymmetry ranged from 0° to 25° with increments of 0.1°. When the SE was out of the range, the measurement value only displayed ‘Hyperopia’ or ‘Myopia’. Until it succeeded, the test were conducted for five times at least.
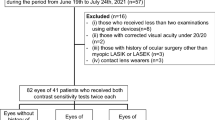
The refraction status and the BCVA of children who volunteered or with abnormal results in the examinations of the PlusoptiX, the table-mounted autorefraction (R-F10, Cannon, Tokyo, Japan), ocular alignment, ocular movement, pupil distance, distance VA and ocular biometric parameters (IOLMaster, Carl Zeiss Meditec, Jena, Germany) were advised to undergo further evaluation with topical 1.0% cyclopentolate (Cyclogyl, Alcon, Belgium). Two drops were instilled 5 minutes apart, with the third drop administered after 20 minutes. After an additional 15 minutes, cycloplegia was evaluated and considered complete in the absence of light reflex. If light reflex was detected, another drop of cyclopentolate was administered; the light reflex was tested after 15 minutes, and refractive errors were measured by CR.
Definition
According to the AAPOS guidelines updated in 2013, automated preschool vision screening for ARF should detect refractive ARFs, including astigmatism >2.0 D, hyperopia >4.0 D, anisometropia >2.0 D and myopia <−3.0 D, and nonrefractive ARFs, including media opacities (>1 mm) and manifest strabismus (>8 PD in primary position) in children aged 31 to 48 months6. Intermittent exotropia and well-controlled deviations were not considered as strabismic ARFs.
Data analysis
Statistical analyses were performed using the Statistic Product for Service Solution (SPSS) for Windows V.7.0 software (V.22.0, IBM, China). All probabilities quoted are two-sided and were considered statistically significant at less than 0.05. All confidence intervals (CIs) are 95%. Data from the right eyes were analysed to avoid enantiomorphism bias except for the anisometropia calculation31.
Data were calculated using the following equations: SE = sphere + (cylinder/2); spherical anisometropia = |sphere (left) − sphere (right)|; and cylindrical anisometropia = |cylinder (left) − cylinder (right)|. The myopia group was defined as SE myopia when ≤−1.00 D, and the hyperopia group was defined as SE hyperopia at ≥+2.00 D.
Descriptive data were presented as mean, standard deviation and frequency. Paired t-test analysis was performed to assess the difference and quantitative relationship of the results. The Bland-Altman plot was used to document the agreement of the measurements. The sensitivities, specificities, PPVs and NPVs were calculated based on 5 sets of criteria recommended by the manufacturer. The receiver operating characteristic curve was employed to select the best cut-off points related to appropriate sensitivity and specificity.
References
Solebo, A. L., Cumberland, P. M. & Rahi, J. S. Whole-population vision screening in children aged 4-5 years to detect amblyopia. Lancet Lond. Engl 385, 2308–2319 (2015).
Holmes, J. M. et al. Effect of age on response to amblyopia treatment in children. Arch. Ophthalmol. Chic. Ill 1960 129, 1451–1457 (2011).
US Preventive Services Task Force. Vision screening for children 1 to 5 years of age: US Preventive Services Task Force Recommendation statement. Pediatrics 127, 340–346 (2011).
Miller, J. M. et al. Instrument-based pediatric vision screening policy statement. Pediatrics 130, 983–986 (2012).
Singman, E., Matta, N., Tian, J. & Silbert, D. A comparison of referral criteria used by the plusoptiX photoscreener. Strabismus 21, 190–194 (2013).
Donahue, S. P. et al. Guidelines for automated preschool vision screening: a 10-year, evidence-based update. J. AAPOS Off. Publ. Am. Assoc. Pediatr. Ophthalmol. Strabismus Am. Assoc. Pediatr. Ophthalmol. Strabismus 17, 4–8 (2013).
Yan, X.-R. et al. Performance of the Plusoptix A09 photoscreener in detecting amblyopia risk factors in Chinese children attending an eye clinic. PloS One 10, e0126052 (2015).
PlusOptix S12 Hand-Held Binocular Auto Refractometer Instruction Manual, Version 6.0.1.0. Nurem-Berg Ger. PlusOptix (2013).
Vision in Preschoolers Study Group. Preschool vision screening tests administered by nurse screeners compared with lay screeners in the vision in preschoolers study. Invest. Ophthalmol. Vis. Sci. 46, 2639–2648 (2005).
Lowry, E. A., Wang, W. & Nyong’o, O. Objective vision screening in 3-year-old children at a multispecialty practice. J. AAPOS Off. Publ. Am. Assoc. Pediatr. Ophthalmol. Strabismus Am. Assoc. Pediatr. Ophthalmol. Strabismus 19, 16–20 (2015).
Dahlmann-Noor, A. H. et al. Vision screening in children by Plusoptix Vision Screener compared with gold-standard orthoptic assessment. Br. J. Ophthalmol. 93, 342–345 (2009).
Bloomberg, J. D. & Suh, D. W. The accuracy of the plusoptiX A08 photoscreener in detecting risk factors for amblyopia in central Iowa. J. AAPOS Off. Publ. Am. Assoc. Pediatr. Ophthalmol. Strabismus Am. Assoc. Pediatr. Ophthalmol. Strabismus 17, 301–304 (2013).
Rajavi, Z. et al. Accuracy and Repeatability of Refractive Error Measurements by Photorefractometry. J. Ophthalmic Vis. Res. 10, 221–228 (2015).
Payerols, A., Eliaou, C., Trezeguet, V., Villain, M. & Daien, V. Accuracy of PlusOptix A09 distance refraction in pediatric myopia and hyperopia. BMC Ophthalmol. 16, 72 (2016).
Rajavi, Z., Parsafar, H., Ramezani, A. & Yaseri, M. Is noncycloplegic photorefraction applicable for screening refractive amblyopia risk factors? J. Ophthalmic Vis. Res. 7, 3–9 (2012).
Ayse, Y. K., Onder, U. & Suheyla, K. Accuracy of Plusoptix S04 in children and teens. Can. J. Ophthalmol. J. Can. Ophtalmol. 46, 153–157 (2011).
Ozdemir, O., Özen Tunay, Z., Petriçli, I. S., Ergintürk Acar, D. & Erol, M. K. Comparison of non-cycloplegic photorefraction, cycloplegic photorefraction and cycloplegic retinoscopy in children. Int. J. Ophthalmol 8, 128–131 (2015).
Borchert, M. et al. Anisometropia in Hispanic and african american infants and young children the multi-ethnic pediatric eye disease study. Ophthalmology 117, 148–153.e1 (2010).
Dirani, M. et al. Prevalence of refractive error in Singaporean Chinese children: the strabismus, amblyopia, and refractive error in young Singaporean Children (STARS) study. Invest. Ophthalmol. Vis. Sci. 51, 1348–1355 (2010).
Colburn, J. D. et al. Longitudinal follow-up of hypermetropic children identified during preschool vision screening. J. AAPOS Off. Publ. Am. Assoc. Pediatr. Ophthalmol. Strabismus Am. Assoc. Pediatr. Ophthalmol. Strabismus 14, 211–215 (2010).
Cotter, S. A. et al. Treatment of anisometropic amblyopia in children with refractive correction. Ophthalmology 113, 895–903 (2006).
Saber Moghadam, A., Alizadeh, R. & Zarei-Ghanavati, M. Plusoptix S08 sensitivity in detecting strabismus as amblyogenic risk factor. Strabismus 21, 230–234 (2013).
Peterseim, M. M. W. et al. Photoscreeners in the pediatric eye office: compared testability and refractions on high-risk children. Am. J. Ophthalmol. 158, 932–938 (2014).
Silbert, D., Matta, N., Tian, J. & Singman, E. Comparing the SureSight autorefractor and the plusoptiX photoscreener for pediatric vision screening. Strabismus 22, 64–67 (2014).
Yilmaz, I. et al. Comparison of the Plusoptix A09 and Retinomax K-Plus 3 with retinoscopy in children. J. Pediatr. Ophthalmol. Strabismus 52, 37–42 (2015).
Matta, N. S., Arnold, R. W., Singman, E. L. & Silbert, D. I. Comparison between the plusoptiX and MTI Photoscreeners. Arch. Ophthalmol. Chic. Ill 1960 127, 1591–1595 (2009).
Matta, N. S., Singman, E. L. & Silbert, D. I. Performance of the Plusoptix vision screener for the detection of amblyopia risk factors in children. J. AAPOS Off. Publ. Am. Assoc. Pediatr. Ophthalmol. Strabismus Am. Assoc. Pediatr. Ophthalmol. Strabismus 12, 490–492 (2008).
Nathan, N. R. & Donahue, S. P. Modification of Plusoptix referral criteria to enhance sensitivity and specificity during pediatric vision screening. J. AAPOS Off. Publ. Am. Assoc. Pediatr. Ophthalmol. Strabismus Am. Assoc. Pediatr. Ophthalmol. Strabismus 15, 551–555 (2011).
Cotter, S. A., Cyert, L. A., Miller, J. M. & Quinn, G. E. & National Expert Panel to the National Center for Children’s Vision and Eye Health. Vision screening for children 36 to <72 months: recommended practices. Optom. Vis. Sci. Off. Publ. Am. Acad. Optom 92, 6–16 (2015).
Varma, R. et al. The multi-ethnic pediatric eye disease study: design and methods. Ophthalmic Epidemiol. 13, 253–262 (2006).
Sachdev, N., Cairns, G. & McGhee, C. N. J. A comparison of autorefractor performance. Optom. Vis. Sci. Off. Publ. Am. Acad. Optom. 82, 9, author reply 9–10 (2005).
Acknowledgements
We thank the children, the corresponding parents or legal guardians and all the members of the Maternal and Child Healthcare Hospital of Yuhuatai District, Nanjing, China, for helpful advice and support. This work is supported by the National Natural Science Foundation of China (Grant No. 81400435 and No. 81673198); the Scientific Research Projects of Jiangsu Provincial Commission of Health and Family Planning (Grant No. H201507); the Natural Science Foundation of Jiangsu Province (Grant No. BK20141027 and No. BK20161595); and a Project Funded by the Priority Academic Program Development of Jiangsu Higher Education Institutions (PAPD, JX10231801). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Author information
Authors and Affiliations
Contributions
H.L. and X.C. designed the study, D.H., X.C., and X.Z. wrote the main manuscript text, H.D. prepared Tables 1–6, X.C. prepared Figure 1, H.D., X.C., X.Z., and H.L. performed data interpretation and analysis interpretation, H.D., Y.W., H.Z., H.D., J.B., J.C., Z.F., and Z.W. performed the ocular examinations.
Corresponding author
Ethics declarations
Competing Interests
The authors declare that they have no competing interests.
Additional information
Publisher's note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Huang, D., Chen, X., Zhang, X. et al. Pediatric vision screening using the plusoptiX A12C photoscreener in Chinese preschool children aged 3 to 4 years. Sci Rep 7, 2041 (2017). https://doi.org/10.1038/s41598-017-02246-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-017-02246-6
This article is cited by
-
Comparison of photorefraction by Plusoptix A12 and cycloplegic autorefraction in children
BMC Ophthalmology (2024)
-
School-based epidemiology study of myopia in Tianjin, China
International Ophthalmology (2020)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.