Abstract
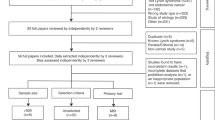
Up to 86% of uterine leiomyomas harbour somatic mutations in mediator complex subunit 12 (MED12). These mutations have been associated with conventional histology, smaller tumour size, and larger number of tumours within the uterus. Prior studies, with limited sample sizes, have failed to detect associations between other clinical features and MED12 mutations. Here, we prospectively collected 763 uterine leiomyomas and the corresponding normal myometrial tissue from 244 hysterectomy patients, recorded tumour characteristics, collected clinical data from medical records, and screened the tissue samples for MED12 mutations to assess potential associations between clinical variables and mutation status. Out of 763 leiomyomas, 599 (79%) harboured a MED12 mutation. In the analysis of tumour characteristics, positive MED12-mutation status was significantly associated with smaller tumour size, conventional histology, and subserous location, relative to intramural. In the analysis of clinical variables, the number of MED12-mutation-positive tumours showed an inverse association with parity, and the number of mutation-negative tumours showed a positive association with a history of pelvic inflammatory disease. This study confirmed the previously reported differences and discovered novel differentiating features for MED12-mutation-positive and -negative leiomyomas. These findings emphasise the relevance of specific driver mutations in genesis and presentation of uterine leiomyomas.
Similar content being viewed by others
Introduction
Uterine leiomyomas are steroid-hormone-dependent benign smooth muscle tumours with an overall 70 to 80% incidence by 50 years of age1. They cause significant morbidity and substantial cost2. Typically, an affected uterus contains multiple leiomyomas ranging from a few millimetres up to 30 centimetres in size3. These lesions are histologically benign, but some display malignant features; these represent rare histopathological variants, such as cellular or mitotically active leiomyomas4. Approximately 25% of women with leiomyomas display symptoms, which depend on the number, location, and size of the tumours5. Even small submucous leiomyomas can cause heavy and irregular menstrual bleeding, whereas large intramural or subserous lesions can lead to pelvic pain, pressure, and urinary distress. Medication such as tranexamic acid and hormone therapy (HT) may relieve the symptoms, however, with a limited effect. Many patients therefore undergo surgical treatment; leiomyomas are the primary indication for hysterectomy.
Well-established risk factors for uterine leiomyomas include African origin, increasing age up to menopause, early menarche, nulliparity, infertility, family history of leiomyomas, and rare tumour susceptibility syndromes, particularly hereditary leiomyomatosis and renal cell cancer (HLRCC)1, 6,7,8,9,10,11,12. Obesity, alcohol intake, HT, reproductive tract infections, hypertension, and hypothyroidism also seem to cause increased risk for leiomyomas, whereas smoking and diabetes reduce their incidence6, 8, 10, 11, 13,14,15. Oral contraceptive users may be at reduced risk6, 10, although contradicting results exist9.
Up to 86% of uterine leiomyomas harbour site-specific mutations in mediator complex subunit 12 (MED12)16,17,18,19,20,21,22,23,24,25,26,27. Based on gene expression profiling, leiomyomas carrying these mutations represent a molecularly distinct subtype28. Furthermore, MED12 mutations are associated with smaller tumour size and larger number of tumours within the uterus, and they are less frequent in histopathological leiomyoma variants16, 17, 20,21,22,23, 25, 27. Earlier studies, with limited sample sizes, have failed to detect underlying associations between other clinical factors and MED12-mutation status, however17, 18, 20, 22, 24. To scrutinise these associations further, we have prospectively collected a series of 763 leiomyomas from 244 hysterectomy patients with comprehensive clinical data. These samples underwent screening for MED12-hotspot mutations, after which we tested the association of the mutation status with tumour characteristics and clinical factors.
Results
Out of 244 patients, 177 (73%) had at least one MED12-mutation-positive leiomyoma, and out of 763 uterine leiomyomas, 6 (1%) harboured a mutation in exon 1 and 593 (78%) in exon 2 (see Supplementary Table S1 for more detailed information). Table 1 presents the frequencies of MED12 mutations for different leiomyoma subgroups. The majority of mutations, observed in 415 (54%) leiomyomas, were missense mutations affecting codon 44 (Fig. 1). All the mutations were heterozygous and somatic.
MED12-mutation spectrum in 763 uterine leiomyomas. In addition to negative mutation status (wild-type), missense mutations affecting different codons, and in-frame insertion and/or deletions (indel) in exon 2 or in intron 1- exon 2 junction and in exon 1 or exon 1 - intron 1 junction are shown separately. Codon 44 mutations are represented in more detail.
The median number of leiomyomas was 2 (range 1–16), the median number of MED12-mutation-positive tumours was 2 (range 0–16), and the median number of mutation-negative tumours was 1 (range 0–5) per patient. The number of MED12-mutation-positive and -negative leiomyomas were negatively correlated [Spearman’s correlation coefficient −0.52, P value (P) = 1.6 × 10−18]. In addition, the number of MED12-mutation-positive tumours and the total number of leiomyomas were strongly correlated (Spearman’s correlation coefficient 0.87, P = 1.3 × 10−77), whereas the number of mutation-negative tumours and total number of leiomyomas showed no correlation.
First, to test whether tumour size, location and histotype are associated with the MED12-mutation status of the leiomyomas, we fit a generalised estimating equations (GEE) model. Positive mutation status was significantly associated with smaller tumour size (P = 4.2 × 10−9), conventional histology (P = 0.0013), and subserous relative to intramural location (P = 0.00082, Table 2).
Second, we examined the associations between clinical factors and the number of MED12-mutation-positive leiomyomas. Here, we used negative binomial regression to account for overdispersion in the corresponding Poisson model (overdispersion test P = 7.1 × 10−6). The number of mutation-positive tumours was inversely associated with parity (P = 0.00017, Table 3). In addition, postmenopausal women without HT had fewer mutation-positive tumours, in comparison to premenopausal women; however, after adjusting for multiple testing, the outcome was not statistically significant (P = 0.0080). No associations were observed between the number of mutation-positive leiomyomas and age at hysterectomy, infertility, smoking status, body mass index (BMI), family history of leiomyomas, oral contraceptive use, history of pelvic inflammatory disease (PID) and chlamydia, hypertension, thyroid disorder, diabetes, or prior leiomyoma surgery.
Finally, we assessed the associations between the clinical factors and the number of MED12-mutation-negative leiomyomas with Poisson regression. The number of mutation-negative tumours showed a statistically significant association with a history of PID (P = 0.00024, Table 3). No associations were observed between the number of mutation-negative leiomyomas and any of the other above-mentioned clinical factors.
Discussion
This study examined the associations between MED12-mutation status, tumour characteristics, and various clinical factors in a large sample set of leiomyomas. As novel findings, the MED12-mutation-positive tumours were associated with subserous type and their number was inversely associated with parity, whereas the number of mutation-negative tumours was associated with a history of PID. In addition, our data confirmed the previous findings that MED12-mutation-positive leiomyomas are smaller in size and more often histopathologically conventional than mutation-negative lesions17, 20,21,22,23, 25, 27.
In this prospectively collected leiomyoma series, the frequency of MED12 mutations reached 79%, being among the highest ones reported. Both Finns and patients of non-Finnish origin harboured mutations with similar frequencies. In prior studies with varying sample sizes and patient ethnicities, the mutation frequency in conventional leiomyomas has ranged from 31 to 86%, and in Finns, from 70 to 86%16,17,18, 20,21,22,23,24,25,26,27. The majority of the prior studies have only screened for exon 2 mutations, however. Here, 1% of leiomyomas harboured a mutation in exon 1, which is in line with the literature where the prevalence has ranged from 1 to 2%17, 19. Thus, exclusion of exon 1 mutations explains only a minor proportion of the variation seen in the reported mutation frequencies. One likely contributing factor explaining the different results is size bias: in some sample sets large lesions may have been preferred; this selects against MED12-mutation-positive tumours, ones usually smaller in size.
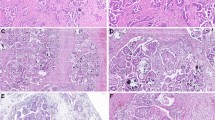
As expected, histopathological leiomyoma variants tended to be MED12-mutation negative. Nevertheless, 42% of the variants harboured a MED12 mutation: a higher frequency than in previous works with mutation frequencies ranging from 0 to 21%21, 23, 25, 27. Due to the small number of leiomyoma variants in this study, however, it is difficult to draw definitive conclusions on their exact mutation frequencies. All three of the lipoleiomyomas were mutation negative. Only one prior study has screened MED12 mutations from lipoleiomyomas, and similarly all four of the studied lesions were mutation negative21. Overall, our results are compatible with the previous notion that mechanisms other than MED12 mutations, such as high mobility group AT-hook 2 (HMGA2) aberrations, drive the majority of histopathological variants while the great majority of common leiomyomas are MED12-mutation positive23, 29,30,31,32.
This is, to our knowledge, the first study to show that positive MED12-mutation status is associated with subserosal location of leiomyomas. Two prior studies have explored the association between MED12-mutation status and tumour location with negative results, possibly due to different study settings and smaller sample sizes18, 24. Brosens et al. have concluded that submucosal leiomyomas display significantly fewer clonal cytogenetic changes compared to the other types33. Myometrium consists of functionally and structurally distinct layers: the subendometrial myometrium exhibits a cyclic pattern of steroid hormone receptor expression, whereas the outer layers of the uterine wall express these receptors continually34. Taken together, these data suggest that the differences in the myometrial layers influence the molecular mechanisms underlying leiomyoma development.
In addition, our results confirmed the previous findings that smaller tumour size and larger number of tumours are associated with positive MED12-mutation status17, 20, 22, 24. The small size of mutation-positive lesions may result from the coexistence of multiple tumours, which jointly lead to clinical intervention sooner, whereas the solitary, typically intramural, mutation-negative tumours need to grow larger to manifest symptoms. Alternatively, the biological growth process may differ between these leiomyoma subtypes. The multiplicity of MED12-mutation-positive leiomyomas may derive from genetic predisposition and/or environmental factors rendering the myometrium susceptible to selection for MED12 mutations.
Intriguingly, a history of PID was associated with the number of MED12-mutation-negative tumours, whereas chlamydia infection, which can overlap with PID diagnosis, showed no association. A few epidemiological studies have observed an association between reproductive tract infections and increased risk for leiomyomas13, 14. Faerstein et al. observed increased odds for leiomyomas with a history of PID and chlamydia infection, as well as with past intrauterine device use when related to infectious complications, suggesting that inflammation may contribute to increased risk13. Furthermore, Moore et al. observed a negative association between chlamydia infection and multiple leiomyomas, and a similar trend for PID14, which is consistent with our result as mutation-negative leiomyomas are typically solitary. In the context of mutation-negative lesions, this finding is compatible with a proposed hypothesis that leiomyomas can occasionally develop via abnormal response to tissue repair or inflammatory stimuli, leading to cell proliferation and fibrosis35. It is also possible that an infectious agent may have a direct tumourigenic effect, such as the Epstein-Barr virus, which is known to cause leiomyomas and leiomyosarcomas in immunosuppressed patients36.
Evidently, parity reduces the risk of leiomyomas, with risk declining as the number of births increases9, 10. According to one proposed mechanism, remodelling of the uterus after each pregnancy would induce leiomyoma regression; however, direct evidence is lacking37. The inverse association between the number of MED12-mutation-positive leiomyomas and parity suggests that births reduce the risk specifically for this leiomyoma subgroup. As Baird and Dunson reason, uterine involution may be more potent in eliminating small lesions, ones typically mutation-positive, whereas remnants of larger tumours would survive37. In addition, the mutation-positive and -negative tumours may respond differently to the changes in, for example, the hormonal environment during and after pregnancy. Furthermore, postmenopausal women without HT showed a trend towards fewer MED12-mutation-positive leiomyomas than premenopausal women; however, we observed a similar, yet weaker, trend also with mutation-negative tumours, but due to the limited sample size no conclusions can be drawn. It is conceivable that MED12-mutation-positive and -negative leiomyomas may respond differently to hormone-level changes, as well as to treatments, such as selective progesterone receptor modulators.
The strength of this study is the large prospective sample set with comprehensive clinical data. On the other hand, the main shortcoming is the basic problem of any database survey; misclassification of variables is possible because of missing information. In addition, this study pooled all the MED12-mutation-negative leiomyomas into one group, although these lesions are likely to be heterogeneous due to the variety of the underlying genetic drivers38, 39. These include HMGA2 rearrangements and biallelic inactivation of fumarate hydratase (FH), sometimes related to a germline mutation30. These two driver events and MED12 mutations seem to be mutually exclusive and lead to unique gene expression patterns28. It is conceivable that all three leiomyoma subtypes may differ also in view of clinical characters, as it is already established that HLRCC-related FH-deficient tumours often show atypical histological features, develop at an earlier age, and are more numerous7, while HMGA2–aberrant tumours tend to be larger than other leiomyomas40. It remains to be elucidated, how the associations identified in this study relate to all three subgroups. Answering this question would require even larger sample sets due to the rarity of subtypes other than MED12, as well as much more extensive molecular workup to adequately identify the FH and HMGA2 subgroups.
Clinical and molecular classification of uterine leiomyomas is likely to be important for developing targeted management strategies such as more effective drugs. This study confirmed the association of MED12 mutations with smaller leiomyoma size, multiplicity and conventional histotype, and revealed novel associations between the MED12-mutation status and leiomyoma location, PID, and parity. These findings emphasise the relevance of specific driver mutations in genesis and presentation of uterine leiomyomas.
Methods
Subjects
This study was approved by the appropriate Ethics Review Board of the Helsinki University Hospital (HUH), Finland, and conducted in accordance with the Declaration of Helsinki. All patients gave signed informed consents before entering the study. We collected uterine leiomyoma (n = 763) and corresponding normal myometrial tissue samples from patients (n = 244) who had ultrasound-diagnosed uterine leiomyomas and underwent hysterectomy in HUH during October 2013 and November 2015 for any medical indication. Pathologists (A.P. and R.B.) dissected the hysterectomy specimens and recorded the location and size (the largest diameter) of the tumours. All feasible distinct tumours ≥1 cm in diameter and a piece of the corresponding normal myometrial tissue were harvested and stored as fresh frozen. In addition, a formalin-fixed paraffin-embedded (FFPE) block from each tumour was prepared. The dissected hysterectomy specimens underwent routine diagnostic pathological scrutiny, and the pathology reports provided the histopathological diagnosis for the study samples. A gynaecological pathologist (R.B.) reviewed haematoxylin-eosin-stained FFPE-tissue sections of all suspected (based on the pathology reports) leiomyoma variants and classified them according to the WHO 2014 criteria4.
Clinical data came from a retrospective review of medical records of all study subjects, and for 70 patients, from an additional designed questionnaire. Data included demographic information and medical and gynaecological history (Table 3).
Mutation analysis
All tumour and normal tissue samples underwent genomic DNA extraction with FastDNA Kit (MP Biomedicals LLC, Solon, OH, USA) and screening for MED12 exon 1 and 2 mutations by Sanger sequencing using 5′ to 3′ primers CCTCCGGAACGTTTCATAGAT (forward) and TTCGGGACTTTTGCTCTCAC (reverse), and GCCCTTTCACCTTGTTCCTT (forward) and TGTCCCTATAAGTCTTCCCAACC (reverse), respectively. PCR products were sequenced using Big Dye Terminator v.3.1 sequencing chemistry (Applied Biosystems, Foster City, CA, USA) on an ABI3730 Automatic DNA Sequencer. We analysed sequence graphs manually and with Mutation Surveyor software (Softgenetics, State College, PA, USA).
Statistical methods
We employed R version 3.2.3 to perform statistical analyses41. Continuous variables were summarised as medians and ranges or inter quartile ranges (IQRs) due to non-normal distribution, and categorical variables as counts and percentages (Tables 2 and 3). We applied GEE, as well as Poisson and negative binomial regression, to obtain multivariable-adjusted effect size estimates (regression coefficients) accompanied by 95% confidence intervals (see Supplementary Information online for detailed information on the statistical models). In tumour-level analysis, MED12-mutation status (a binary variable) was predicted by tumour characteristics (size, location and histotype). Considering that multiple leiomyomas within a uterus may not be independent, we applied the GEE method with exchangeable correlation structure (80 observations deleted due to missing information, n = 683). The model was fit assuming the binomial random component and logit link function (geeglm function in R package geepack)42,43,44. Inferences of the GEE parameters were based on the Wald statistic. To model MED12-mutation-negative-leiomyoma counts, we applied Poisson regression (glm function in R, three observations deleted due to missing information, n = 241). In the model for MED12-mutation-positive leiomyoma counts, we assumed the negative binomial distribution with quadratic variance function (glm.nb function in R package MASS, three observations deleted due to missing information, n = 241) to account for overdispersion in the corresponding Poisson model (evaluated using dispersiontest function in R package AER)45, 46. To assess whether the negative binomial distribution provided a better fit to these data, we used the likelihood ratio test to compare negative binomial and Poisson regression models (odTest function in R package pscl)47. The generalised Pearson statistic and model deviance were used to assess Poisson and negative binomial goodness of fit. In both models for tumour counts, we considered explanatory variables previously associated with leiomyoma risk and putative confounding variables [African origin, age at hysterectomy, menarche, menopausal status (premenopausal/current use of HT/postmenopausal, no HT), parity, infertility, smoking status, alcohol use, BMI, family history of leiomyomas, oral contraceptive use, history of PID and chlamydia, hypertension, thyroid disorder, diabetes, and prior leiomyoma surgery]. Variables with >10 missing values (menarche and alcohol use) or <5 cases (African origin) were omitted. Spearman correlation matrix (R package PerformanceAnalytics) and variance inflation factors (vif function in R package car) were computed to evaluate possible collinearity among explanatory variables48, 49. A total of 34 statistical tests were undertaken to investigate the relationships between patient- or tumour-level variables and MED12 mutations. To adjust for multiple comparisons, we applied the Bonferroni correction (α = 0.05/34); two-sided P < 0.00147 indicated statistical significance.
References
Baird, D. D., Dunson, D. B., Hill, M. C., Cousins, D. & Schectman, J. M. High cumulative incidence of uterine leiomyoma in black and white women: Ultrasound evidence. Obstet. Gynecol. 188, 100–107 (2003).
Cardozo, E. R. et al. The estimated annual cost of uterine leiomyomata in the United States. Obstet. Gynecol. 206, 211.e1–211.e9 (2012).
Cramer, S. F. & Patel, A. The frequency of uterine leiomyomas. Am. J. Clin. Pathol. 94, 435–438 (1990).
Oliva, E. et al. Mesenchymal tumours In World Heatlh Organization Classification of Tumours of Female Reproductive Organs (eds Kurman, R. J., Carcangiu, M. L., Herrington, C. S. & Young, R. H.) 135–138 (IARC Press, 2014).
Stovall, D. W. Clinical symptomatology of uterine leiomyomas. Clin. Obstet. Gynecol. 44, 364–371 (2001).
Faerstein, E., Szklo, M. & Rosenshein, N. Risk factors for uterine leiomyoma: a practice-based case-control study. I. African-American heritage, reproductive history, body size, and smoking. Am. J. Epidemiol. 153, 1–10 (2001).
Lehtonen, H. J. Hereditary leiomyomatosis and renal cell cancer: update on clinical and molecular characteristics. Fam. Cancer 10, 397–411 (2011).
Marshall, L. M. et al. Variation in the Incidence of Uterine Leiomyoma Among Premenopausal Women by Age and Race. Obstet. Gynecol. 90, 967–973 (1997).
Marshall, L. M. et al. A prospective study of reproductive factors and oral contraceptive use in relation to the risk of uterine leiomyomata. Fertil. Steril. 70, 432–439 (1998).
Ross, R. K. et al. Risk factors for uterine fibroids: reduced risk associated with oral contraceptives. Br. Med. J. (Clin. Res. Ed.) 293, 359–362 (1986).
Templeman, C. et al. Risk factors for surgically removed fibroids in a large cohort of teachers. Fertil. Steril. 92, 1436–1446 (2009).
Vikhlyaeva, E. M., Khodzhaeva, Z. S. & Fantschenko, N. D. Familial predisposition to uterine leiomyomas. Int. J. Gynecol. Obstet. 51, 127–131 (1995).
Faerstein, E., Szklo, M. & Rosenshein, N. B. Risk Factors for Uterine Leiomyoma: A Practice-based Case-Control Study. II. Atherogenic Risk Factors and Potential Sources of Uterine Irritation. Am. J. Epidemiol. 153, 11–19 (2001).
Moore, K. R. et al. Self-Reported Reproductive Tract Infections and Ultrasound Diagnosed Uterine Fibroids in African-American Women. J. Womens Health. (Larchmt) 24, 489–495 (2015).
Ott, J. et al. Overt hypothyroidism is associated with the presence of uterine leiomyoma: a retrospective analysis. Eur. J. Obstet. Gynecol. Reprod. Biol. 177, 19–22 (2014).
Croce, S. & Chibon, F. MED12 and uterine smooth muscle oncogenesis: State of the art and perspectives. Eur. J. Cancer 51, 1603–1610 (2015).
Heinonen, H. R. et al. MED12 mutation frequency in unselected sporadic uterine leiomyomas. Fertil. Steril. 102, 1137–1142 (2014).
Je, E. M., Kim, M. R., Min, K. O., Yoo, N. J. & Lee, S. H. Mutational analysis of MED12 exon 2 in uterine leiomyoma and other common tumors. Int. J. Cancer 131, E1044–7 (2012).
Kämpjärvi, K. et al. Mutations in Exon 1 highlight the role of MED12 in uterine leiomyomas. Hum. Mutat. 35, 1136–1141 (2014).
Markowski, D. N., Helmke, B. M., Bartnitzke, S., Loning, T. & Bullerdiek, J. Uterine fibroids: do we deal with more than one disease? Int. J. Gynecol. Pathol. 33, 568–572 (2014).
Matsubara, A. et al. Prevalence of MED12 mutations in uterine and extrauterine smooth muscle tumours. Histopathology 62, 657–661 (2013).
Mäkinen, N. et al. MED12, the mediator complex subunit 12 gene, is mutated at high frequency in uterine leiomyomas. Science 334, 252–255 (2011).
Mäkinen, N. et al. MED12 exon 2 mutations in histopathological uterine leiomyoma variants. Eur. J. Hum. Genet. 21, 1300–1303 (2013).
Osinovskaya, N. S. et al. Frequency and Spectrum of MED12 Exon 2 Mutations in Multiple Versus Solitary Uterine Leiomyomas From Russian Patients. Int. J. Gynecol. Pathol. 35, 509–515 (2016).
Perot, G. et al. MED12 alterations in both human benign and malignant uterine soft tissue tumors. PLoS One 7, e40015 (2012).
Sadeghi, S. et al. The study of MED12 gene mutations in uterine leiomyomas from Iranian patients. Tumour Biol. 37, 1567–1571 (2016).
Zhang, Q. et al. Molecular analyses of 6 different types of uterine smooth muscle tumors: Emphasis in atypical leiomyoma. Cancer 120, 3165–3177 (2014).
Mehine, M. et al. Integrated data analysis reveals uterine leiomyoma subtypes with distinct driver pathways and biomarkers. Proc. Natl. Acad. Sci. USA 113, 1315–1320 (2016).
Fukushima, M., Schaefer, I. M. & Fletcher, C. D. Myolipoma of Soft Tissue: Clinicopathologic Analysis of 34 Cases. Am. J. Surg. Pathol. 41, 153–160 (2017).
Mehine, M., Mäkinen, N., Heinonen, H. R., Aaltonen, L. A. & Vahteristo, P. Genomics of uterine leiomyomas: insights from high-throughput sequencing. Fertil. Steril. 102, 621–629 (2014).
Nilbert, M. et al. Ring formation and structural rearrangements of chromosome 1 as secondary changes in uterine leiomyomas with t(12;14)(q14–15;q23–24). Cancer Genet. Cytogenet. 36, 183–190 (1988).
Pedeutour, F. et al. Dysregulation of HMGIC in a uterine lipoleiomyoma with a complex rearrangement including chromosomes 7, 12, and 14. Genes Chromosomes Cancer 27, 209–215 (2000).
Brosens, I., Deprest, J., Dal Cin, P. & Van den Berghe, H. Clinical significance of cytogenetic abnormalities in uterine myomas. Fertil. Steril. 69, 232–235 (1998).
Noe, M., Kunz, G., Herbertz, M., Mall, G. & Leyendecker, G. The cyclic pattern of the immunocytochemical expression of oestrogen and progesterone receptors in human myometrial and endometrial layers: characterization of the endometrial–subendometrial unit. Hum. Reprod. 14, 190–197 (1999).
Wegienka, G. Are uterine leiomyoma a consequence of a chronically inflammatory immune system? Med. Hypotheses 79, 226–231 (2012).
Purgina, B., Rao, U. N., Miettinen, M. & Pantanowitz, L. AIDS-Related EBV-Associated Smooth Muscle Tumors: A Review of 64 Published Cases. Patholog. Res. Int. 2011, 561548 (2011).
Baird, D. D. & Dunson, D. B. Why is parity protective for uterine fibroids? Epidemiology 14, 247–250 (2003).
Mehine, M. et al. Characterization of Uterine Leiomyomas by Whole-Genome Sequencing. N. Engl. J. Med. 369, 43–53 (2013).
Yatsenko, S. A. et al. Highly heterogeneous genomic landscape of uterine leiomyomas by whole exome sequencing and genome-wide arrays. Fertil. Steril. 107, 457–466.e9 (2017).
Hennig, Y. et al. Chromosomal translocations affecting 12q14–15 but not deletions of the long arm of chromosome 7 associated with a growth advantage of uterine smooth muscle cells. Mol. Hum. Reprod. 5, 1150–1154 (1999).
R Core Team. R: A Language and Environment for Statistical Computing (R Foundation for Statistical Computing, Vienna, Austria, 2015).
Højsgaard, S., Halekoh, U. & Yan, J. The R Package geepack for Generalized Estimating Equations. J. Stat. Softw. 15/2, 1–11 (2006).
Yan, J. & Fine, J. P. Estimating Equations for Association Structures. Stat. Med. 23, 859–880 (2004).
Yan, J. geepack: Yet Another Package for Generalized Estimating Equations. R-News 2/3, 12–14 (2002).
Kleiber, C. & Zeileis, A. Applied Econometrics with R (Springer, New York, USA, 2008).
Venables, W. N. & Ripley, B. D. Modern Applied Statistics with S Edn. 4 (Springer, New York, USA, 2002).
Jackman, S. pscl: Classes and Methods for R Developed in the Political Science Computational Laboratory, Stanford University. (Department of Political Science, Stanford University: Stanford, California, USA, 2015).
Peterson, B. G. & Carl, P. PerformanceAnalytics: Econometric tools for performance and risk analysis (R package version 1.4.3541, 2014).
Fox, J. & Weisberg, S. In An R Companion to Applied Regression (Sage, Thousand Oaks, California, USA, 2011).
Acknowledgements
We sincerely thank Alison Ollikainen, Elina Pörsti, Heikki Metsola, Iina Vuoristo, Inga-Lill Svedberg, Marjo Rajalaakso, Salla Välipakka, and Sini Nieminen from the Department of Medical and Clinical Genetics and Genome-Scale Biology Research Program, University of Helsinki, as well as Pirjo Ikonen and the rest of the staff of the Kätilöopisto Maternity Hospital, and the staff of the Department of Pathology, University of Helsinki for technical assistance. This study was supported by the European Research Council (ERC, 695727) and the Academy of Finland (Centre of Excellence in Cancer Genetics Research 2012–2017, 250345), as well as the Nordic Information for Action eScience Centre (NIASC), the Nordic Centre of Excellence financed by NordForsk (project 62721, personal grant to KP), the Biomedicum Helsinki Foundation, the Cancer Society of Finland, the Emil Aaltonen Foundation, the Finnish Medical Society Duodecim, the Finnish-Norwegian Medical Foundation, the Ida Montin Foundation, Kliinisen kemian tutkimussäätiö, the Maud Kuistila Memorial Foundation, and Oskar Öflunds stiftelse (personal grants to HH).
Author information
Authors and Affiliations
Contributions
H.-R.H.: study conception and design, acquisition, analysis and interpretation of data, and drafting the manuscript. A.P. and R.B.: study conception and design, acquisition of data. O.H., P.V., J.S. and L.A.A.: study conception and design. T.T., K.P., J.T. and E.P.: analysis and interpretation of data. N.M.: study conception and design, acquisition, analysis and interpretation of data. All authors critically reviewed the article and approved the submitted version.
Corresponding author
Ethics declarations
Competing Interests
The authors declare that they have no competing interests.
Additional information
Publisher's note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Heinonen, HR., Pasanen, A., Heikinheimo, O. et al. Multiple clinical characteristics separate MED12-mutation-positive and -negative uterine leiomyomas. Sci Rep 7, 1015 (2017). https://doi.org/10.1038/s41598-017-01199-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-017-01199-0
This article is cited by
-
Myometrial oxidative stress drives MED12 mutations in leiomyoma
Cell & Bioscience (2022)
-
Frequency of MED12 Mutation in Relation to Tumor and Patient’s Clinical Characteristics: a Meta-analysis
Reproductive Sciences (2022)
-
Alterations in lipid profile upon uterine fibroids and its recurrence
Scientific Reports (2021)
-
Parity associates with chromosomal damage in uterine leiomyomas
Nature Communications (2021)
-
Global metabolomic profiling of uterine leiomyomas
British Journal of Cancer (2017)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.