Abstract
CD146, also known as melanoma cell adhesion molecule, was initially identified as a marker of melanoma progression and metastasis. Recently many clinical studies investigated overexpression of CD146 predict poor prognosis of solid tumor, however, the results was inconclusive, partly due to small numbers of patients included. This present meta-analysis was therefore performed utilizing the results of all clinical studies concerned to determine the prognostic value of CD146 expression in solid tumors. Relevant articles were identified through searching the PubMed, Web of Science and Embase database. In this meta-analysis, 12 studies involving 2,694 participants were included, and we drew the conclusion that strong significant associations between CD146 expression and all endpoints: overall survival (OS) [hazard ratio (HR) = 2.496, 95% confidence interval (95% CI) 2.115–2.946], time to progression (TTP) (HR = 2.445, 95% CI 1.975–3.027). Furthermore, the subgroup analysis revealed that the associations between CD146 overexpression and the outcome endpoints (OS or TTP) were significant in Mongoloid patients and Caucasian patients, as well in patients with lung cancer and digestive system cancer. In conclusion, these results showed that high CD146 was associated with poor survival in human solid tumors. CD146 may be a valuable prognosis predictive biomarker; nevertheless, whether CD146 could be a potential therapeutic target in human solid tumors needs to be further studied.
Similar content being viewed by others
Introduction
CD146, also referred to as MUC18, MCAM, Mel-CAM, S-Endo-1 and P1H12 antigen1, a transmembrane glycoprotein belonging to the immunoglobulin superfamily that functions as a Ca2+ independent adhesion molecule2, was first identified as a melanoma-specific cell adhesion molecule. CD146 was a 113-kD membrane glycoprotein that contains five immunoglobulin-like domains, a transmembrane region, and a short cytoplasmic tail3. Early research indicated that CD146 is expressed on vascular endothelium, smooth muscle and other cells in normal tissue, and mediates cation-independent adhesion through interactions with an unidentified ligand on the surface of various cells4. Subsequent research manifested CD146 was a multifunctional molecule that participates in several physiological and pathological processes involving in development, immunity, and angiogenesis5. CD146 regulated development of the nervous system, kidney, and retina6,7,8. Knockdown of CD146 protein expression impeded vascular development whereas overexpression of CD146 in zebrafish induces sprouting angiogenesis9. In recent years, cumulated evidence indicated that CD146 overexpression significantly correlates with the progression, angiogenesis, metastasis of some malignant tumors which was observed in esophageal cancer, melanoma, gallbladder adenocarcinoma, ovarian carcinoma, prostate cancer10,11,12,13,14,15,16. However, in oral mucoepidermoid carcinoma, CD146 expression was greater in intermediate/high grade tumors, weaker in patients with local recurrence, regional and distant metastasis17. CD146 was found downregulate in breast cancer and pancreatic cancer progression18, 19. Recently, An increasing number of studies suggested that CD146 is highly expressed in solid tumors, including hepatocellular carcinoma20, leiomyosarcoma21, esophageal squamous cell carcinoma22, lung cancer23,24,25, colorectal cancer26, clear cell renal cell carcinoma27, gastric cancer28, gallbladder adenocarcinoma13, breast cancer29, epithelial ovarian cancer30. These conspicuous indications on the role of CD146 in cancer indicated that the transmembrane glycoprotein would be further considered as a potential marker for outcome of cancer patients.
Plenty studies showed that increased CD146 expression in tumor tissues was associated with poor survival of patients with various cancer types. However, the results of those individual studies were not comprehensive. Therefore, we performed this comprehensive meta-analysis aiming to clarify the prognostic value of CD146 in solid tumors and to support that the protein may be a potential therapeutic oncotarget.
Materials and Methods
Publication search
According to the Preferred Reporting Items for Systematics Reviews and Meta-Analyses guidelines31, this present meta-analysis was performed. A comprehensive literature search was implemented by using the electronic databases PubMed, Embase, and Web of Science databases (up to July 20, 2016) with the search terms: ‘CD146’, ‘MCAM’ and “cancer”/“tumor”/“neoplasm”/“carcinoma” and the following limits: Human, article in English. Wholly potentially eligible studies were retrieved and their bibliographies were carefully scanned to identify other eligible studies and extra studies were identified by a hand search of the references cited in the original studies. When multiple studies of the same patient population were identified, we incorporated the published report into the largest sample size.
Inclusion criteria
To be qualified for presence in this meta-analysis and data extraction, studies had to: (a) assess CD146 expression in predicting prognosis in cancer, (b) offer hazard ratios (HRs) with 95% confidence intervals (CIs) or enable calculation of these statistics from the data presented, (c) sort CD146 expression into “high” and “low” or “positive” and “negative”.
Exclusion criteria
Exclusion criteria were: (a) literatures published as letters, editorials, abstracts, reviews, case reports and expert opinions; (b) experiments performed in vitro or in vivo, but not based on patients; (c) articles without the HRs and 95% CI, or not dealing with overall survival, disease-free survival, or the K-M survival curves; (d) studies in which the follow-up duration was shorter than 3 years.
Data extraction
All data included in the present meta-analysis were extracted independently and carefully by two reviewers using a standardized form. Disagreement was resolved through independently extracting data from the original article by the third author, and consensus was reached by discussions. The meta-analysis of CD146 expression was based on two outcome endpoints: OS (overall survival), TTP (time to progression). DFS (disease-free survival) and TTR (time to recurrence) that similar in meaning were combined to use a unified prognostic parameter: time to tumor progression (TTP). Several different parameters, if reported, were extracted from each paper, including the first author’s surname, publication year, country of origin, number of patients analyzed, types of measurement, and score for CD146 assessment, cut-off values to determine CD146 overexpression, OS, TTP. The main features of these eligible studies were summarized in Table 1. The multivariate HR was extracted to assess prognostic value of CD146 expression. For the articles in which prognosis was plotted only with the Kaplan-Meier curves, the Engauge Digitizer V4.1 was then used to extract survival data, and the estimation of the HRs and 95% CIs were calculated with Tierney’s method32. All studies were assessed via Newcastle-Ottawa Scale (NOS). The quality scores ranged from 6 to 9, suggesting that the methodological quality was high.
Statistical analysis
The data collected from each eligible article was used to evaluate the relations between CD146 expression and solid cancer prognosis by meta-analysis. Pooled HRs and 95% CIs for these outcome endpoints (OS, TTP) were calculated. Subgroup analysis was performed when there were at least three studies in each subgroup. Statistical heterogeneity was assessed using the Q test, and a P value > 0.10 suggested a lack of heterogeneity among studies. We also quantified the effect of heterogeneity using I 2 = 100% × (Q − df)/Q. I 2 values of <25% may be considered “low”, values of about 50% may be considered “moderate” and values of >75% may be considered “high”33. According to the absence or presence of heterogeneity, random effects model or fixed effects model was used to merge the HR, respectively. Without statistical heterogeneity, a fixed effects model was employed to calculate the pooled HRs, otherwise random effects model was used34. Funnel plots and the Egger’s test were used to estimate the possible publication bias35. If a publication bias did exist, the Duval and Tweedie’s trim and fill method was then used to assess its influence on the overall effect36. Sensitivity analysis was also conducted to find out if certain individual article could influence the overall result. The Stata 14.0 (StataCorp, College Station, TX) was used to conduct statistical analyses. P values for all comparisons were two-tailed and statistical significance was defined as p < 0.05 for all tests, except those for heterogeneity.
Results
Demographic characteristics
Through a literature search of the PubMed, Embase, and Web of Science databases, a total of 432 articles were retrieved, using different combinations of key terms, one additional article identified by scanning the reference of the selected studies As showed in the search flow diagram (Fig. 1), 432 records were originally acquired using the predefined search strategy. Owing to repeated data, 71 records were removed. After glancing over the retrieved titles and abstracts, 315 records were excluded because of no relevant endpoint provided. The rest of 47 records were downloaded with full-text and carefully retrieved one by one. Among them, 35 studies were eliminated, including two studies that were experimental study, one was case report, and six without prognosis data, 26 were unrelated. Consequently, 12 published studies counting 2,694 patients that up to the inclusion norm were finally elected for the meta-analysis, which were then used to assess the relevance between CD146 expression and solid tumor prognosis. The median sample-size of these testers was 118, with a wide range from 36 to 1080. Among all cohorts, Mongoloid (n = 9) became the major race of literatures, followed by Caucasian (n = 3). As for the cancer type, one study evaluated hepatocellular carcinoma, one study evaluated uterine leiomyosarcoma, one study evaluated esophageal squamous cell carcinoma, there studies evaluated lung cancer, one study evaluated colorectal cancer, one study evaluated clear cell renal cell carcinoma, one study evaluated gastric cancer, one study evaluated gallbladder cancer, one study evaluated breast canser, one study evaluated epithelial ovarian cancer. Overall, 11 studies focused on OS, four studies focused on TTP.
Evidence synthesis
The meta-analysis of CD146 expression was established in two outcome endpoints: OS, TTP. 11 articles were involved in OS of the meta-analysis. A fixed effects model was utilized to calculate the pooled hazard ratio (HR) and 95% confidence interval (CI) due to the heterogeneity test testified a P value of 0.433 and an I 2 values of 0.8%. The results suggested that CD146 overexpression was related with poor OS of solid tumors (pooled HR = 2.496, 95% CI = 2.115–2.946, P = 0.000) (Fig. 2). Four studies were included in TTP of the meta-analysis. On account of the heterogeneity test reported a P value of 0.745 and an I 2 values of 0.0%, a fixed-effects model was then used. The results showed a significant association between CD146 expression and TTP (pooled HR = 2.445, 95% CI = 1.975–3.027, P = 0.000) (Fig. 3). Subgroup study was then performed, the results suggested that the associations between CD146 overexpression and poor OS and poor TTP were significant in Mongoloid patients (OS: pooled HR = 2.508, 95% CI 2.073–3.034, P < 0.001; TTP: pooled HR = 2.544, 95% CI = 1.998–3.238, P = 0.000), as well as in Caucasian (OS: pooled HR = 2.461, 95% CI 1.759–3.444, P < 0.001). The significant correlation was also spotted between CD146 overexpression and poor OS in patients with lung cancer (OS: pooled HR = 2.172, 95% CI = 1.453–3.246, P < 0.001) and digestive system cancer (pooled HR = 2.661, 95% CI = 2.149–3.295, P < 0.001).
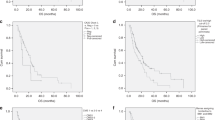
Publication bias and sensitivity analysis
Begg’s funnel plot and Egger’s test were utilized to evaluate the publication bias of these involved literatures. As shown in (Fig. 4), the shapes of the funnel plots for the OS and TTP showed no evidence of obvious heterogeneity, and Egger’s tests revealed no publication bias regarding both OS (P = 0.636) and TTP (P = 0.887). Sensitivity analyses were further done to determine the sturdiness of the results depicted above. No single study controlled this meta-analysis, and removal of any individual study had no significant effect on the overall conclusion (Fig. 5).
Discussions
Overexpression of CD146 had been reported to promote cancer progression and predict poor prognosis of cancer patient. Many clinical studies investigated the prognostic value of CD146 over-expression. Nevertheless, most of these studies, including limited number of patients, remain have incomprehensive conclusions. This current meta-analysis is the first complete overview of all published clinical studies exploring the impact of CD146 expression on prognosis of many solid tumors.
We scientifically estimated survival data of 2,694 solid tumor patients included in 12 different studies. In general, these results clearly indicated that high CD146 expression was a poor prognostic factor in solid tumors, with both results of poor OS (pooled HR = 2.496, 95% CI = 2.115–2.946, P = 0.000) and poor TTP (pooled HR = 2.445, 95% CI = 1.975–3.027, P = 0.000). Similarly, subgroup analysis revealed the associations between CD146 overexpression and poor OS were significant within Mongoloid and Caucasian, and poor TTP within Mongoloid. When data was stratified according to cancer types, the results showed the prognostic value of CD146 over-expression was significant in digestive system neoplasms and lung cancer.
As far as we known, this present study is the first and most all-sided meta-analysis systematically discovering the possible prognostic role of CD146 up-regulation in solid tumors. Our assessable results strongly reinforced the current mainstream perspective that an adverse impact of CD146 redundancy was associated with the OS and TTP. Also, several important insinuations in this meta-analysis were presented. First, high CD146 expression may be a common poor prognostic marker in solid tumors. In this meta-analysis, we incorporated ten different cancer types, including hepatocellular carcinoma20, leiomyosarcoma21, esophageal squamous cell carcinoma22, lung cancer23,24,25, colorectal cancer26, clear cell renal cell carcinoma27, gastric cancer28, gallbladder adenocarcinoma13, breast cancer29, epithelial ovarian cancer30. The pooled results from these cancer types confirmed that high CD146 expression was associated with poor OS and TTP, and this finding can be extended to all solid tumors. Second, we verified that high CD146 expression associated with poor OS in Mongoloid and Caucasian patients, as well in digestive system neoplasms and lung cancer, and TTP in Mongoloid patients. Finally, it underlines the potential to develop CD146 as a valuable therapeutic target and prognostic biomarker for solid tumors, though it needs to be further studied.
Aside from the inspiring outcomes, limitations still lay in this assessable meta-analysis. First of all, most of the included studies were designed as retrospective studies, and such studies were more likely to be published if they have positive results than if which have negative one. Furthermore, the method assessing CD146 expression and defining CD146 positivity were inconsistent. Consequently, our estimation of the associations between overexpression of CD146 and outcomes may have been overestimated.
To sum up, high CD146 expression in solid tumor tissues association with poor survival was clearly demonstrated in the present meta-analysis. We suggest that CD146 may be a useful prognostic biomarker, but if it would be a promising therapeutic target for solid tumors still need to be ulteriorly researched. Furthermore, further studies related to specific tumor types and perspectives are required to corroborate the clinical utility of CD146 expression in solid tumors.
References
Lehmann, J. M., Riethmuller, G. & Johnson, J. P. MUC18, a marker of tumor progression in human melanoma, shows sequence similarity to the neural cell adhesion molecules of the immunoglobulin superfamily. Proceedings of the National Academy of Sciences of the United States of America 86, 9891–9895 (1989).
Delorme, B. et al. Specific plasma membrane protein phenotype of culture-amplified and native human bone marrow mesenchymal stem cells. Blood 111, 2631–2635, doi:10.1182/blood-2007-07-099622 (2008).
Sers, C., Kirsch, K., Rothbacher, U., Riethmuller, G. & Johnson, J. P. Genomic organization of the melanoma-associated glycoprotein MUC18: implications for the evolution of the immunoglobulin domains. Proceedings of the National Academy of Sciences of the United States of America 90, 8514–8518 (1993).
Ouhtit, A. et al. Towards understanding the mode of action of the multifaceted cell adhesion receptor CD146. Biochimica et biophysica acta 1795, 130–136, doi:10.1016/j.bbcan.2009.01.002 (2009).
Wang, Z. & Yan, X. CD146, a multi-functional molecule beyond adhesion. Cancer letters 330, 150–162, doi:10.1016/j.canlet.2012.11.049 (2013).
Taira, E., Kohama, K., Tsukamoto, Y., Okumura, S. & Miki, N. Gicerin/CD146 is involved in neurite extension of NGF-treated PC12 cells. Journal of cellular physiology 204, 632–637, doi:10.1002/jcp.20365 (2005).
Takaha, N. et al. Expression of gicerin in development, oncogenesis and regeneration of the chick kidney. Differentiation; research in biological diversity 58, 313–320, doi:10.1046/j.1432-0436.1995.5850313.x (1995).
Tsukamoto, Y. et al. Expression of gicerin, a cell adhesion molecule, in the abnormal retina in silver plumage color mutation of Japanese quail (Coturnix japonica). Neuroscience letters 266, 53–56 (1999).
Chan, B., Sinha, S., Cho, D., Ramchandran, R. & Sukhatme, V. P. Critical roles of CD146 in zebrafish vascular development. Developmental dynamics: an official publication of the American Association of Anatomists 232, 232–244, doi:10.1002/dvdy.20220 (2005).
Loges, S. et al. Determination of microvessel density by quantitative real-time PCR in esophageal cancer: correlation with histologic methods, angiogenic growth factor expression, and lymph node metastasis. Clinical cancer research: an official journal of the American Association for Cancer Research 13, 76–80, doi:10.1158/1078-0432.CCR-06-1324 (2007).
Lei, X., Guan, C. W., Song, Y. & Wang, H. The multifaceted role of CD146/MCAM in the promotion of melanoma progression. Cancer cell international 15, 3, doi:10.1186/s12935-014-0147-z (2015).
Wu, G. J. & Dickerson, E. B. Frequent and increased expression of human METCAM/MUC18 in cancer tissues and metastatic lesions is associated with the clinical progression of human ovarian carcinoma. Taiwanese journal of obstetrics & gynecology 53, 509–517, doi:10.1016/j.tjog.2014.03.003 (2014).
Wang, W., Yang, Z. L., Liu, J. Q., Jiang, S. & Miao, X. Y. Identification of CD146 expression, angiogenesis, and lymphangiogenesis as progression, metastasis, and poor-prognosis related markers for gallbladder adenocarcinoma. Tumour biology: the journal of the International Society for Oncodevelopmental Biology and Medicine 33, 173–182, doi:10.1007/s13277-011-0260-8 (2012).
Wu, G. J. et al. Isolation and characterization of the major form of human MUC18 cDNA gene and correlation of MUC18 over-expression in prostate cancer cell lines and tissues with malignant progression. Gene 279, 17–31 (2001).
Watson-Hurst, K. & Becker, D. The role of N-cadherin, MCAM and beta3 integrin in melanoma progression, proliferation, migration and invasion. Cancer biology & therapy 5, 1375–1382 (2006).
Garcia, S. et al. Poor prognosis in breast carcinomas correlates with increased expression of targetable CD146 and c-Met and with proteomic basal-like phenotype. Human pathology 38, 830–841, doi:10.1016/j.humpath.2006.11.015 (2007).
Pires, F. R., Shih Ie, M., da Cruz Perez, D. E., de Almeida, O. P. & Kowalski, L. P. Mel-CAM (CD146) expression in parotid mucoepidermoid carcinoma. Oral oncology 39, 277–281 (2003).
Shih, L. M., Hsu, M. Y., Palazzo, J. P. & Herlyn, M. The cell-cell adhesion receptor Mel-CAM acts as a tumor suppressor in breast carcinoma. The American journal of pathology 151, 745–751 (1997).
Zheng, B. et al. CD146 attenuation in cancer-associated fibroblasts promotes pancreatic cancer progression. Molecular carcinogenesis, doi:10.1002/mc.22409 (2015).
Jiang, G. et al. CD146 promotes metastasis and predicts poor prognosis of hepatocellular carcinoma. Journal of experimental & clinical cancer research: CR 35, 38, doi:10.1186/s13046-016-0313-3 (2016).
Zhou, Y. et al. CD146 as an adverse prognostic factor in uterine sarcoma. European journal of medical research 20, 67, doi:10.1186/s40001-015-0160-2 (2015).
Li, Y. et al. Correlation of CD146 expression and clinicopathological characteristics in esophageal squamous cell carcinoma. Oncology letters 8, 859–863, doi:10.3892/ol.2014.2227 (2014).
Zhang, X. et al. MCAM expression is associated with poor prognosis in non-small cell lung cancer. Clinical & translational oncology: official publication of the Federation of Spanish Oncology Societies and of the National Cancer Institute of Mexico 16, 178–183, doi:10.1007/s12094-013-1057-6 (2014).
Oka, S., Uramoto, H., Chikaishi, Y. & Tanaka, F. The expression of CD146 predicts a poor overall survival in patients with adenocarcinoma of the lung. Anticancer research 32, 861–864 (2012).
Kristiansen, G. et al. Expression of the cell adhesion molecule CD146/MCAM in non-small cell lung cancer. Analytical cellular pathology: the journal of the European Society for Analytical Cellular Pathology 25, 77–81 (2003).
Tian, B., Zhang, Y. & Li, N. CD146 protein as a marker to predict postoperative liver metastasis in colorectal cancer. Cancer biotherapy & radiopharmaceuticals 28, 466–470, doi:10.1089/cbr.2012.1426 (2013).
Feng, G. et al. CD146 gene expression in clear cell renal cell carcinoma: a potential marker for prediction of early recurrence after nephrectomy. International urology and nephrology 44, 1663–1669, doi:10.1007/s11255-012-0255-4 (2012).
Liu, W. F. et al. CD146 expression correlates with epithelial-mesenchymal transition markers and a poor prognosis in gastric cancer. International journal of molecular sciences 13, 6399–6406, doi:10.3390/ijms13056399 (2012).
Zabouo, G. et al. CD146 expression is associated with a poor prognosis in human breast tumors and with enhanced motility in breast cancer cell lines. Breast cancer research: BCR 11, R1, doi:10.1186/bcr2215 (2009).
Aldovini, D. et al. M-CAM expression as marker of poor prognosis in epithelial ovarian cancer. International journal of cancer 119, 1920–1926, doi:10.1002/ijc.22082 (2006).
Moher, D., Liberati, A., Tetzlaff, J., Altman, D. G. & Group, P. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. International journal of surgery 8, 336–341, doi:10.1016/j.ijsu.2010.02.007 (2010).
Tierney, J. F., Stewart, L. A., Ghersi, D., Burdett, S. & Sydes, M. R. Practical methods for incorporating summary time-to-event data into meta-analysis. Trials 8, 16, doi:10.1186/1745-6215-8-16 (2007).
Higgins, J. P., Thompson, S. G., Deeks, J. J. & Altman, D. G. Measuring inconsistency in meta-analyses. Bmj 327, 557–560, doi:10.1136/bmj.327.7414.557 (2003).
DerSimonian, R. & Laird, N. Meta-analysis in clinical trials. Controlled clinical trials 7, 177–188 (1986).
Egger, M., Davey Smith, G., Schneider, M. & Minder, C. Bias in meta-analysis detected by a simple, graphical test. Bmj 315, 629–634 (1997).
Duval, S. & Tweedie, R. Trim and fill: A simple funnel-plot-based method of testing and adjusting for publication bias in meta-analysis. Biometrics 56, 455–463 (2000).
Acknowledgements
This work is supported by the National Natural Science Foundation (81472786, 81472305), the Six Talents Peak Project of Jiangsu Province (2012-WSN-012, 2014-WSW-061), Kunshan Science and Technology Program (KS1418, KS1528), the Foundation of tumor clinical and basic research team (KYC005).
Author information
Authors and Affiliations
Contributions
Conceived and designed the experiments: Min-Bin Chen, Pei-Hua Lu. Analyzed the data: Ping Zeng, HaiLi, Pei-Hua Lu. Prepared figures: Ping Zeng, Hai Li, Min-Bin Chen. Contributed to the writing of the paper: Ping Zeng,Hai Li, Min-Bin Chen. Helped edit the manuscript: Li-Na Zhou, Min Tang, Chao-Ying Liu.
Corresponding authors
Ethics declarations
Competing Interests
The authors declare that they have no competing interests.
Additional information
Publisher's note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Zeng, P., Li, H., Lu, PH. et al. Prognostic value of CD146 in solid tumor: A Systematic Review and Meta-analysis. Sci Rep 7, 4223 (2017). https://doi.org/10.1038/s41598-017-01061-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-017-01061-3
This article is cited by
-
Anti-proliferative, antioxidant effects of methanol extract of Calotropis procera leaf on lung cancer cells (H1299) and its ameliorative effect on expression of CD146 on blood cells
Clinical Phytoscience (2021)
-
CD146 T cells in lung cancer: its function, detection, and clinical implications as a biomarker and therapeutic target
Cancer Cell International (2019)
-
Effects of pericytes and colon cancer stem cells in the tumor microenvironment
Cancer Cell International (2019)
-
CD146 is highly expressed in glioma stem cells and acts as a cell cycle regulator
Journal of Neuro-Oncology (2019)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.