Abstract
The noncoding genome is substantially larger than the protein-coding genome but has been largely unexplored by genetic association studies. Here, we performed region-based rare variant association analysis of >25,000 variants in untranslated regions of 6,139 amyotrophic lateral sclerosis (ALS) whole genomes and the whole genomes of 70,403 non-ALS controls. We identified interleukin-18 receptor accessory protein (IL18RAP) 3′ untranslated region (3′UTR) variants as significantly enriched in non-ALS genomes and associated with a fivefold reduced risk of developing ALS, and this was replicated in an independent cohort. These variants in the IL18RAP 3′UTR reduce mRNA stability and the binding of double-stranded RNA (dsRNA)-binding proteins. Finally, the variants of the IL18RAP 3′UTR confer a survival advantage for motor neurons because they dampen neurotoxicity of human induced pluripotent stem cell (iPSC)-derived microglia bearing an ALS-associated expansion in C9orf72, and this depends on NF-κB signaling. This study reveals genetic variants that protect against ALS by reducing neuroinflammation and emphasizes the importance of noncoding genetic association studies.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$29.99 / 30 days
cancel any time
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout







Similar content being viewed by others
Data availability
Human genetics data are publically available from the sequencing consortia that control ethically appropriate usage of data, harmonization across studies and the safety of personal information donated by individuals that contributed their DNA for sequencing: the Project Mine ALS sequencing consortium, the NYGC ALS Consortium, the gnomAD and NHLBI’s TOPMed. Sequencing data are deposited at Gene Expression Omnibus under accession number GSE186757. All Other data used for this manuscript are available in the manuscript. The University of California Santa Cruz gene annotation93, miRBase v20 (ref. 57), RefSeq63, dbNSFP v2.0 (ref. 58) and ANNOVAR95 databases were used in this study. Source data are provided with this paper.
Code availability
Variant annotation scripts are available at GitHub at https://github.com/TsviyaOlender/Non-coding-Variants-in-ALS-genes-.
References
Brown, R. H. & Al-Chalabi, A. Amyotrophic lateral sclerosis. N. Engl. J. Med. 377, 162–172 (2017).
Taylor, J. P., Brown, R. H. Jr. & Cleveland, D. W. Decoding ALS: from genes to mechanism. Nature 539, 197–206 (2016).
Renton, A. E., Chio, A. & Traynor, B. J. State of play in amyotrophic lateral sclerosis genetics. Nat. Neurosci. 17, 17–23 (2014).
Al-Chalabi, A., van den Berg, L. H. & Veldink, J. Gene discovery in amyotrophic lateral sclerosis: implications for clinical management. Nat. Rev. Neurol. 13, 96–104 (2017).
van Rheenen, W. et al. Common and rare variant association analyses in amyotrophic lateral sclerosis identify 15 risk loci with distinct genetic architectures and neuron-specific biology. Nat. Genet. 53, 1636–1648 (2021).
DeJesus-Hernandez, M. et al. Expanded GGGGCC hexanucleotide repeat in noncoding region of C9ORF72 causes chromosome 9p-linked FTD and ALS. Neuron 72, 245–256 (2011).
Renton, A. E. et al. A hexanucleotide repeat expansion in C9ORF72 is the cause of chromosome 9p21-linked ALS-FTD. Neuron 72, 257–268 (2011).
La Spada, A. R. & Taylor, J. P. Repeat expansion disease: progress and puzzles in disease pathogenesis. Nat. Rev. Genet. 11, 247–258 (2010).
Cooper-Knock, J. et al. Rare variant burden analysis within enhancers identifies CAV1 as an ALS risk gene. Cell Rep. 33, 108456 (2020).
Povysil, G. et al. Rare-variant collapsing analyses for complex traits: guidelines and applications. Nat. Rev. Genet. 20, 747–759 (2019).
Cookson, W., Liang, L., Abecasis, G., Moffatt, M. & Lathrop, M. Mapping complex disease traits with global gene expression. Nat. Rev. Genet. 10, 184–194 (2009).
Knight, J. C. Regulatory polymorphisms underlying complex disease traits. J. Mol. Med. 83, 97–109 (2005).
An, J.Y., et al. Genome-wide de novo risk score implicates promoter variation in autism spectrum disorder. Science 362, eaat6576 (2018).
Haramati, S. et al. miRNA malfunction causes spinal motor neuron disease. Proc. Natl Acad. Sci. USA 107, 13111–13116 (2010).
Emde, A. et al. Dysregulated miRNA biogenesis downstream of cellular stress and ALS-causing mutations: a new mechanism for ALS. EMBO J. 34, 2633–2651 (2015).
Eitan, C. & Hornstein, E. Vulnerability of microRNA biogenesis in FTD-ALS. Brain Res. 1647, 105–111 (2016).
Campos-Melo, D., Droppelmann, C. A., He, Z., Volkening, K. & Strong, M. J. Altered microRNA expression profile in amyotrophic lateral sclerosis: a role in the regulation of NFL mRNA levels. Mol. Brain 6, 26 (2013).
Buratti, E. et al. Nuclear factor TDP-43 can affect selected microRNA levels. FEBS J. 277, 2268–2281 (2010).
Kawahara, Y. & Mieda-Sato, A. TDP-43 promotes microRNA biogenesis as a component of the Drosha and Dicer complexes. Proc. Natl Acad. Sci. USA 109, 3347–3352 (2012).
Morlando, M. et al. FUS stimulates microRNA biogenesis by facilitating co-transcriptional Drosha recruitment. EMBO J. 31, 4502–4510 (2012).
Hoye, M. L. et al. MicroRNA profiling reveals marker of motor neuron disease in ALS models. J. Neurosci. 37, 5574–5586 (2017).
Rotem, N. et al. ALS along the axons—expression of coding and noncoding RNA differs in axons of ALS models. Sci Rep. 7, 44500 (2017).
Butovsky, O. et al. Modulating inflammatory monocytes with a unique microRNA gene signature ameliorates murine ALS. J. Clin. Invest. 122, 3063–3087 (2012).
Figueroa-Romero, C. et al. Expression of microRNAs in human post-mortem amyotrophic lateral sclerosis spinal cords provides insight into disease mechanisms. Mol. Cell. Neurosci. 71, 34–45 (2016).
Williams, A. H. et al. MicroRNA-206 delays ALS progression and promotes regeneration of neuromuscular synapses in mice. Science 326, 1549–1554 (2009).
Bartel, D. P. MicroRNAs: target recognition and regulatory functions. Cell 136, 215–233 (2009).
Mayr, C. Regulation by 3′-untranslated regions. Annu. Rev. Genet. 51, 171–194 (2017).
Lee, S., Abecasis, G. R., Boehnke, M. & Lin, X. Rare-variant association analysis: study designs and statistical tests. Am. J. Hum. Genet. 95, 5–23 (2014).
Alboni, S., Cervia, D., Sugama, S. & Conti, B. Interleukin 18 in the CNS. J. Neuroinflammation 7, 9 (2010).
Zhao, W. et al. TDP-43 activates microglia through NF-κB and NLRP3 inflammasome. Exp. Neurol. 273, 24–35 (2015).
Tsutsumi, N. et al. The structural basis for receptor recognition of human interleukin-18. Nat. Commun. 5, 5340 (2014).
Adachi, O. et al. Targeted disruption of the MyD88 gene results in loss of IL-1- and IL-18-mediated function. Immunity 9, 143–150 (1998).
Kato, Z. et al. The structure and binding mode of interleukin-18. Nat. Struct. Biol. 10, 966–971 (2003).
Matsumoto, S. et al. Interleukin-18 activates NF-κB in murine T helper type 1 cells. Biochem. Biophys. Res. Commun. 234, 454–457 (1997).
Robinson, D. et al. IGIF does not drive Th1 development but synergizes with IL-12 for interferon-γ production and activates IRAK and NFκB. Immunity 7, 571–581 (1997).
Kojima, H. et al. An essential role for NF-κB in IL-18-induced IFN-γ expression in KG-1 cells. J Immunol. 162, 5063–5069 (1999).
Morel, J. C., Park, C. C., Kumar, P. & Koch, A. E. Interleukin-18 induces rheumatoid arthritis synovial fibroblast CXC chemokine production through NFκB activation. Lab. Invest. 81, 1371–1383 (2001).
Miyoshi, K., Obata, K., Kondo, T., Okamura, H. & Noguchi, K. Interleukin-18-mediated microglia/astrocyte interaction in the spinal cord enhances neuropathic pain processing after nerve injury. J. Neurosci. 28, 12775–12787 (2008).
Kadhim, H., Deltenre, P., Martin, J. J. & Sebire, G. In-situ expression of interleukin-18 and associated mediators in the human brain of sALS patients: hypothesis for a role for immune–inflammatory mechanisms. Med. Hypotheses 86, 14–17 (2016).
Johann, S. et al. NLRP3 inflammasome is expressed by astrocytes in the SOD1 mouse model of ALS and in human sporadic ALS patients. Glia 63, 2260–2273 (2015).
Italiani, P. et al. Evaluating the levels of interleukin-1 family cytokines in sporadic amyotrophic lateral sclerosis. J. Neuroinflammation 11, 94 (2014).
Huang, F. et al. Longitudinal biomarkers in amyotrophic lateral sclerosis. Ann. Clin. Transl Neurol. 7, 1103–1116 (2020).
Lall, D. & Baloh, R. H. Microglia and C9orf72 in neuroinflammation and ALS and frontotemporal dementia. J. Clin. Invest. 127, 3250–3258 (2017).
Beers, D. R. & Appel, S. H. Immune dysregulation in amyotrophic lateral sclerosis: mechanisms and emerging therapies. Lancet Neurol. 18, 211–220 (2019).
Vahsen, B. F. et al. Non-neuronal cells in amyotrophic lateral sclerosis—from pathogenesis to biomarkers. Nat. Rev. Neurol. 17, 333–348 (2021).
McCauley, M. E. & Baloh, R. H. Inflammation in ALS/FTD pathogenesis. Acta Neuropathol. 137, 715–730 (2019).
Motataianu, A., Barcutean, L. & Balasa, R. Neuroimmunity in amyotrophic lateral sclerosis: focus on microglia. Amyotroph. Lateral Scler. Frontotemporal Degener. 21, 159–166 (2020).
Philips, T. & Robberecht, W. Neuroinflammation in amyotrophic lateral sclerosis: role of glial activation in motor neuron disease. Lancet Neurol. 10, 253–263 (2011).
Kaltschmidt, B. & Kaltschmidt, C. NF-κB in the nervous system. Cold Spring Harb. Perspect. Biol. 1, a001271 (2009).
Mattson, M. P. & Meffert, M. K. Roles for NF-κB in nerve cell survival, plasticity, and disease. Cell Death Differ. 13, 852–860 (2006).
Frakes, A. E. et al. Microglia induce motor neuron death via the classical NF-κB pathway in amyotrophic lateral sclerosis. Neuron 81, 1009–1023 (2014).
Uranishi, H. et al. Involvement of the pro-oncoprotein TLS (translocated in liposarcoma) in nuclear factor-κB p65-mediated transcription as a coactivator. J. Biol. Chem. 276, 13395–13401 (2001).
Swarup, V. et al. Deregulation of TDP-43 in amyotrophic lateral sclerosis triggers nuclear factor κB-mediated pathogenic pathways. J. Exp. Med. 208, 2429–2447 (2011).
Project MinE Consortium. Project MinE: study design and pilot analyses of a large-scale whole-genome sequencing study in amyotrophic lateral sclerosis. Eur. J. Hum. Genet. 26, 1537–1546 (2017).
Lee, S. et al. Optimal unified approach for rare-variant association testing with application to small-sample case–control whole-exome sequencing studies. Am. J. Hum. Genet. 91, 224–237 (2012).
Dunckley, T. et al. Whole-genome analysis of sporadic amyotrophic lateral sclerosis. N. Engl. J. Med. 357, 775–788 (2007).
Griffiths-Jones, S., Grocock, R. J., van Dongen, S., Bateman, A. & Enright, A. J. miRBase: microRNA sequences, targets and gene nomenclature. Nucleic Acids Res. 34, D140–D144 (2006).
Liu, X., Jian, X. & Boerwinkle, E. dbNSFP v2.0: a database of human non-synonymous SNVs and their functional predictions and annotations. Hum. Mutat. 34, E2393–E2402 (2013).
Kenna, K. P. et al. NEK1 variants confer susceptibility to amyotrophic lateral sclerosis. Nat. Genet. 48, 1037–1042 (2016).
Rosen, D. R. et al. Mutations in Cu/Zn superoxide dismutase gene are associated with familial amyotrophic lateral sclerosis. Nature 362, 59–62 (1993).
Chio, A. et al. Prevalence of SOD1 mutations in the Italian ALS population. Neurology 70, 533–537 (2008).
van der Spek, R. A. A. et al. The project MinE databrowser: bringing large-scale whole-genome sequencing in ALS to researchers and the public. Amyotroph. Lateral Scler. Frontotemporal Degener. 20, 432–440 (2019).
O’Leary, N. A. et al. Reference sequence (RefSeq) database at NCBI: current status, taxonomic expansion, and functional annotation. Nucleic Acids Res. 44, D733–D745 (2016).
Smith, L. et al. Establishing the UK DNA Bank for motor neuron disease (MND). BMC Genet. 16, 84 (2015).
Shi, Y. et al. Haploinsufficiency leads to neurodegeneration in C9ORF72 ALS/FTD human induced motor neurons. Nat. Med. 24, 313–325 (2018).
Haukedal, H. & Freude, K. Implications of microglia in amyotrophic lateral sclerosis and frontotemporal dementia. J. Mol. Biol. 431, 1818–1829 (2019).
Haenseler, W. et al. A highly efficient human pluripotent stem cell microglia model displays a neuronal-co-culture-specific expression profile and inflammatory response. Stem Cell Reports 8, 1727–1742 (2017).
Peng, S. S., Chen, C. Y., Xu, N. & Shyu, A. B. RNA stabilization by the AU-rich element binding protein, HuR, an ELAV protein. EMBO J. 17, 3461–3470 (1998).
Fan, X. C. & Steitz, J. A. Overexpression of HuR, a nuclear-cytoplasmic shuttling protein, increases the in vivo stability of ARE-containing mRNAs. EMBO J. 17, 3448–3460 (1998).
Stellos, K. et al. Adenosine-to-inosine RNA editing controls cathepsin S expression in atherosclerosis by enabling HuR-mediated post-transcriptional regulation. Nat. Med. 22, 1140–1150 (2016).
Brennan, C. M. & Steitz, J. A. HuR and mRNA stability. Cell. Mol. Life Sci. 58, 266–277 (2001).
Garcia-Dominguez, D. J., Morello, D., Cisneros, E., Kontoyiannis, D. L. & Frade, J. M. Stabilization of Dll1 mRNA by Elavl1/HuR in neuroepithelial cells undergoing mitosis. Mol. Biol. Cell 22, 1227–1239 (2011).
Rothamel, K. et al. ELAVL1 primarily couples mRNA stability with the 3′ UTRs of interferon-stimulated genes. Cell Rep. 35, 109178 (2021).
Mukherjee, N. et al. Integrative regulatory mapping indicates that the RNA-binding protein HuR couples pre-mRNA processing and mRNA stability. Mol. Cell 43, 327–339 (2011).
Fernandopulle, M. S. et al. Transcription factor-mediated differentiation of human iPSCs into neurons. Curr. Protoc. Cell Biol. 79, e51 (2018).
Christian, F., Smith, E.L. & Carmody, R.J. The regulation of NF-κB subunits by phosphorylation. Cells 5, 12 (2016).
Zhong, H., May, M. J., Jimi, E. & Ghosh, S. The phosphorylation status of nuclear NF-κB determines its association with CBP/p300 or HDAC-1. Mol. Cell 9, 625–636 (2002).
Zhong, H., Voll, R. E. & Ghosh, S. Phosphorylation of NF-κB p65 by PKA stimulates transcriptional activity by promoting a novel bivalent interaction with the coactivator CBP/p300. Mol. Cell 1, 661–671 (1998).
Oeckinghaus, A. & Ghosh, S. The NF-κB family of transcription factors and its regulation. Cold Spring Harb. Perspect. Biol. 1, a000034 (2009).
Waelchli, R. et al. Design and preparation of 2-benzamido-pyrimidines as inhibitors of IKK. Bioorg. Med. Chem. Lett. 16, 108–112 (2006).
Ayers, K. L. et al. A loss of function variant in CASP7 protects against Alzheimer’s disease in homozygous APOE ε4 allele carriers. BMC Genomics 17, 445 (2016).
Benitez, B. A. et al. Missense variant in TREML2 protects against Alzheimer’s disease. Neurobiol. Aging 35, 1510.e19-26 (2014).
Jonsson, T. et al. A mutation in APP protects against Alzheimer’s disease and age-related cognitive decline. Nature 488, 96–99 (2012).
Sims, R., et al. Rare coding variants in PLCG2, ABI3, and TREM2 implicate microglial-mediated innate immunity in Alzheimer’s disease. Nat. Genet. 49, 1373–1384 (2017).
Landers, J. E. et al. Reduced expression of the kinesin-associated protein 3 (KIFAP3) gene increases survival in sporadic amyotrophic lateral sclerosis. Proc. Natl Acad. Sci. USA 106, 9004–9009 (2009).
Farhan, S. M. K. et al. Exome sequencing in amyotrophic lateral sclerosis implicates a novel gene, DNAJC7, encoding a heat-shock protein. Nat. Neurosci. 22, 1966–1974 (2019).
Lambrechts, D. et al. VEGF is a modifier of amyotrophic lateral sclerosis in mice and humans and protects motoneurons against ischemic death. Nat. Genet. 34, 383–394 (2003).
Reichenstein, I., et al. Human genetics and neuropathology suggest a link between miR-218 and amyotrophic lateral sclerosis pathophysiology. Sci Transl Med 11, eaav5264 (2019).
Liao, Y., Wang, J., Jaehnig, E. J., Shi, Z. & Zhang, B. WebGestalt 2019: gene set analysis toolkit with revamped UIs and APIs. Nucleic Acids Res. 47, W199–W205 (2019).
Lorenz, R. et al. ViennaRNA package 2.0. Algorithms Mol. Biol. 6, 26 (2011).
Zhan, X., Hu, Y., Li, B., Abecasis, G. R. & Liu, D. J. RVTESTS: an efficient and comprehensive tool for rare variant association analysis using sequence data. Bioinformatics 32, 1423–1426 (2016).
Raczy, C. et al. Isaac: ultra-fast whole-genome secondary analysis on Illumina sequencing platforms. Bioinformatics 29, 2041–2043 (2013).
Tyner, C. et al. The UCSC Genome Browser database: 2017 update. Nucleic Acids Res. 45, D626–D634 (2017).
Danecek, P. et al. The variant call format and VCFtools. Bioinformatics 27, 2156–2158 (2011).
Wang, K., Li, M. & Hakonarson, H. ANNOVAR: functional annotation of genetic variants from high-throughput sequencing data. Nucleic Acids Res. 38, e164 (2010).
Agarwal, V., Bell, G. W., Nam, J. W. & Bartel, D. P. Predicting effective microRNA target sites in mammalian mRNAs. eLife 4, e05005 (2015).
Schildge, S., Bohrer, C., Beck, K. & Schachtrup, C. Isolation and culture of mouse cortical astrocytes. J. Vis. Exp. https://doi.org/10.3791/50079 (2013).
Hsu, P. D. et al. DNA targeting specificity of RNA-guided Cas9 nucleases. Nat. Biotechnol. 31, 827–832 (2013).
Doench, J. G. et al. Optimized sgRNA design to maximize activity and minimize off-target effects of CRISPR–Cas9. Nat. Biotechnol. 34, 184–191 (2016).
Xu, H. et al. Sequence determinants of improved CRISPR sgRNA design. Genome Res. 25, 1147–1157 (2015).
Chari, R., Mali, P., Moosburner, M. & Church, G. M. Unraveling CRISPR–Cas9 genome engineering parameters via a library-on-library approach. Nat. Methods 12, 823–826 (2015).
Erijman, A., Dantes, A., Bernheim, R., Shifman, J. M. & Peleg, Y. Transfer-PCR (TPCR): a highway for DNA cloning and protein engineering. J. Struct. Biol. 175, 171–177 (2011).
Peleg, Y. & Unger, T. Application of the restriction-free (RF) cloning for multicomponents assembly. Methods Mol. Biol. 1116, 73–87 (2014).
Keren-Shaul, H. et al. MARS-seq2.0: an experimental and analytical pipeline for indexed sorting combined with single-cell RNA sequencing. Nat. Protoc. 14, 1841–1862 (2019).
Jaitin, D. A. et al. Massively parallel single-cell RNA-seq for marker-free decomposition of tissues into cell types. Science 343, 776–779 (2014).
Kohen, R. et al. UTAP: user-friendly transcriptome analysis pipeline. BMC Bioinformatics 20, 154 (2019).
Cox, J. & Mann, M. MaxQuant enables high peptide identification rates, individualized p.p.b.-range mass accuracies and proteome-wide protein quantification. Nat. Biotechnol. 26, 1367–1372 (2008).
Cox, J. & Mann, M. Quantitative, high-resolution proteomics for data-driven systems biology. Annu. Rev. Biochem. 80, 273–299 (2011).
Cox, J., Michalski, A. & Mann, M. Software lock mass by two-dimensional minimization of peptide mass errors. J. Am. Soc. Mass Spectrom. 22, 1373–1380 (2011).
Cox, J. et al. Accurate proteome-wide label-free quantification by delayed normalization and maximal peptide ratio extraction, termed MaxLFQ. Mol. Cell. Proteomics 13, 2513–2526 (2014).
Tyanova, S. et al. The Perseus computational platform for comprehensive analysis of (prote)omics data. Nat. Methods 13, 731–740 (2016).
Krach, F. et al. Transcriptome–pathology correlation identifies interplay between TDP-43 and the expression of its kinase CK1E in sporadic ALS. Acta Neuropathol. 136, 405–423 (2018).
Thompson, L. iMN (Exp 2)—ALS, SMA and control (unaffected) iMN cell lines differentiated from iPS cell lines using a long differentiation protocol—RNA-seq. LINCS (collection) http://identifiers.org/lincs.data/LDG-1338 (2017).
Acknowledgements
We gratefully acknowledge the contributions of all participants and the investigators who provided biological samples and data for the Project Mine ALS sequencing consortium, the NYGC ALS Consortium, the gnomAD and TOPMed of the NHLBI (https://www.nhlbiwgs.org/topmed-banner-authorship). We thank M. Ward (NINDS, NIH) for sharing human inducible i3LMN cells. Samples used in this research were in part obtained from the UK National DNA Bank for MND Research, funded by the MND Association and the Wellcome Trust. We acknowledge sample management undertaken by Biobanking Solutions funded by the Medical Research Council at the Centre for Integrated Genomic Medical Research, University of Manchester. We would like to thank the NINDS Biorepository at Coriell Institute for iPSC cell lines used in this study. We thank B. Oldak and J. Hanna for microglia differentiation protocols, N. Kozer and H. Barr for assistance with live-cell imaging, A. Savidor and Y. Levin for mass spectrometry and M. Shmueli, Y. Merbl and R. Rotkof for advice and protocols. We thank LSE for language and scientific editing. Some illustrations were created with BioRender. The Hornstein lab is supported by friends of S. Brenner. E.H. is Head of Andi and Larry Wolfe Center for Research on Neuroimmunology and Neuromodulation and incumbent of Ira & Gail Mondry Professorial chair. This work is funded by Legacy Heritage Fund (828/17), Bruno and Ilse Frick Foundation for Research on ALS, the RADALA Foundation for ALS research, Teva Pharmaceutical Industries., Ltd., as part of the Israeli National Network of Excellence in Neuroscience (NNE) and Minna-James-Heineman Stiftung through Minerva, the European Research Council under the European Union’s Seventh Framework Programme (FP7/2007-2013)/ERC grant agreement number 617351, Israel Science Foundation (135/16, 3497/21); Target ALS 118945, the Minerva Foundation, with funding from the Federal German Ministry for Education and Research, the ALS-Therapy Alliance, AFM Telethon (20576 to E.H.), Motor Neuron Disease Association (UK), The Thierry Latran Foundation for ALS research, ERA-Net for Research Programmes on Rare Diseases (FP7), via the Israel Ministry of Health. A. Alfred Taubman through IsrALS, Yeda-Sela, Yeda-CEO, Israel Ministry of Trade and Industry, Y. Leon Benoziyo Institute for Molecular Medicine, Kekst Family Institute for Medical Genetics, David and Fela Shapell Family Center for Genetic Disorders Research, Crown Human Genome Center, Nathan, Shirley, Philip and Charlene Vener New Scientist Fund, Julius and Ray Charlestein Foundation, Fraida Foundation, Wolfson Family Charitable Trust, Adelis Foundation, Merck (UK), Maria Halphen, Estates of Fannie Sherr, Lola Asseof, Lilly Fulop, Andi and Larry Wolfe Center for Research on Neuroimmunology and Neuromodulation and Benoziyo center for Neurological diseases, Weizmann—Brazil Center for Research on Neurodegeneration at The Weizmann Institute of Science, Redhill Foundation—Sam and Jean Rothberg Charitable Trust, Edward and Janie Moravitz, the Israeli Council for Higher Education via the Weizmann Data Science Research Center and a research grant from the Estate of Tully and Michele Plesser and M. Judith Ruth Institute for Preclinical Brain Research. A.A.-C. received funding from Neurodegenerative Disease Research (JPND), Medical Research Council (MR/L501529/1, STRENGTH, MR/R024804/1, BRAIN-MEND), Economic and Social Research Council (ES/L008238/1, ALS-CarE), MND Association, National Institute for Health Research (NIHR) Biomedical Research Centre at South London and Maudsley NHS Foundation Trust and King’s College London. This project has received funding from the European Research Council (ERC) under the European Union’s Horizon 2020 research and innovation programme (grant agreement number 772376, EScORIAL). The collaboration project is cofunded by the PPP Allowance made available by Health~Holland, Top Sector Life Sciences & Health to stimulate public–private partnerships. This study was supported by the ALS Foundation Netherlands. For P.V.D., Project MinE Belgium was supported by a grant from IWT (number 140935), the ALS Liga België, the National Lottery of Belgium and the KU Leuven Opening the Future Fund. P.V.D. holds a senior clinical investigatorship of FWO-Vlaanderen and is supported by E. von Behring Chair for Neuromuscular and Neurodegenerative Disorders, the ALS Liga België and the KU Leuven funds ‘Een Hart voor ALS’, ‘Laeversfonds voor ALS Onderzoek’ and the ‘Valéry Perrier Race against ALS Fund’. Several authors of this publication are members of the European Reference Network for Rare Neuromuscular Diseases. P.J.S. received funding from the Medical Research Council, MND Association, NIHR Senior Investigator Award, NIHR Sheffield Biomedical Research Centre and NIHR Sheffield Clinical Research Facility. P.M.A. received funding from the Knut and Alice Wallenberg Foundation, the Swedish Brain Foundation, the Swedish Science Council and the Ulla-Carin Lindquist Foundation. H.P.P. and sequencing activities at NYGC were supported by the ALS Association and The Tow Foundation. C.E. was supported by a scholarship from Teva Pharmaceutical Industries, Ltd., as part of the NNE. S.M.K.F. is supported by the ALS Canada Tim E. Noël Postdoctoral Fellowship. R.H.B.J. was funded by the ALS Association, ALS Finding a Cure, Angel Fund, ALS-One, Cellucci Fund and NIH grants (R01 NS104022, R01 NS073873 and NS111990-01 to R.H.B.J.). J.K.I. is a New York Stem Cell Foundation-Robertson Investigator. N.S.Y. was supported by the Israeli Council for Higher Education via the Weizmann Data Science Research Center, by a research grant from the Estate of Tully and Michele Plesser and by Maccabim Foundation. Work in the J.K.I. lab was supported by NIH grant R01NS097850, U.S. Department of Defense grant W81XWH-19-PRARP-CSRA and grants from the Tau Consortium, the New York Stem Cell Foundation, the ALS Association and the John Douglas French Alzheimer’s Foundation. R.L.McL. received funding from the Science Foundation Ireland (17/CDA/4737), and A.N.B. received funding from the Suna and Inan Kirac Foundation. J.E.L. received funding from the National Institute of Health/NINDS (R01 NS073873).
Author information
Authors and Affiliations
Consortia
Contributions
C.E. and A. Siany led the project. C.E. and A. Siany contributed to research conception, design and interpretations and wrote the manuscript with E.H. C.E., E.B., T.O., K.R.V.E., M.M., S.M.K.F., N.S.Y., J.C.-K., K.P.K., R.A.A.V.D.S., W.S., A.A.K., A.I., A. Shatunov, A.R.J., E.C., D.R., O.W., R.H.B.J., P.J.S., P.V.D., L.H.v.d.B., H.P., E.S., A.A.-C. and J.H.V. collected samples, were involved in the sequence analysis pipeline, phenotyping, variant calling, provided expertise or were involved in the genetic association analysis of rare noncoding variants in individuals with ALS. S.-T.H. and J.K.I. provided stem cells and initial data. S.B.-D., E.A., G.B. and H.M.-K. were involved in the design, generation and validation of CRISPR-edited IL18RAP isogenic iPSCs. H.M.-K. and Y.M.D. performed the pulldown experiments of IL18RAP 3′UTR RNA-associated proteins and analyzed the proteomic data. A. Siany and C.E. established human iPSC-derived microglia differentiation and culturing protocols, performed motor neuron survival experiments and interpreted data. A. Siany, N.R. and C.E. performed molecular biology studies in LCLs and U2OS cell lines, including reporter assays, qPCR and protein quantification by western blotting. E.Y. performed the bulk MARS-seq experiment. C.-H.Y., C.L. and S.L.M. provided expertise and processed mouse cortex samples for flow cytometry. Y.C., Y.E.-A., S.W. and D.P.S. helped perform research. E.H. conceived and supervised the study and wrote the manuscript with C.E. and A. Siany. All coauthors provided approval of the manuscript.
Corresponding author
Ethics declarations
Competing interests
J.K.I. is a cofounder of AcuraStem Incorporated. J.K.I. declares that he is bound by confidentiality agreements that prevent him from disclosing details of his financial interests in this work. J.H.V. and L.H.v.d.B. report to have sponsored research agreements with Biogen. E.H. is an inventor on pending patent family PCT/IL2016/050328 entitled ‘Methods of treating motor neuron diseases’. All other authors declare that they have no competing interests.
Peer review
Peer review information
Nature Neuroscience thanks Aaron Gitler, Donna Werling, and the other, anonymous, reviewer(s) for their contribution to the peer review of this work.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Extended data
Extended Data Fig. 1 Study design.
(a) Flow chart of approach for discovery of region-based rare-variants in non-coding genomic regions via association studies and (b) diagram depicting regions of interest comprising of 1,750 autosomal human pre-miRNA genes, 295 open reading frames encoding for proteins of interest, and 295 3′UTRs.
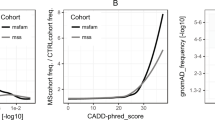
Extended Data Fig. 2 Region-based rare-variant association analyses.
(a-d) QQ (quantile-quantile) probability plot, of obtained and expected P-values (log scale) gained by region-based rare-variant association analysis of different genomic regions, comprised of (a) 295 candidate protein-coding regions listed in Supplementary Table 3. These ORFs encode for ALS-relevant proteins or proteins that are associated with miRNA biogenesis or activity. Variants were depicted if predicted to cause frameshifting, alternative splicing, abnormal stop codon or a deleterious non-synonymous amino acid substitution, in ≥ 3 of 7 independent dbNSFP prediction algorithms (genomic inflation λ = 0.96), (b) All known pre-miRNA genes in the human genome (genomic inflation λ = 1.31), (c) predicted networks, comprised of aggregated variants detected on a specific mature miRNA sequence and its cognate downstream 3’UTR targets (genomic inflation λ = 1.16), and (d) variants in 3′UTRs of the same 295 genes listed in Supplementary Table 3 (genomic inflation λ = 1.08). Data was obtained from 3,955 ALS cases and 1,819 controls (Project MinE). Features positioned on the diagonal line represent results obtained under the null hypothesis. Open-reading frames of 10 known ALS genes (blue). IL18RAP 3′UTR (red). P-values, calculated with SKAT-O.
Extended Data Fig. 3 3′UTR-based rare-variant association analysis, using different algorithms, and illustration of rare variants identified in the IL18RAP 3′UTR.
(a-d) QQ plot of obtained and expected P-values (log scale) gained by region-based rare-variant association analysis of genomic regions comprised of 295 3′UTRs listed in Supplementary Table 3, in the Project MinE cohort (3,955 ALS cases and 1,819 non-ALS controls). Features positioned on the diagonal line represent results obtained under the null hypothesis. IL18RAP 3′UTR (red) is the most significant 3’UTR associated with ALS using different algorithms: (a) Sequence Kernel Association Test, SKAT (genomic inflation λ = 1.02), (b) Combined Multivariate and Collapsing, CMC (genomic inflation λ = 1.34), (c) Variable Threshold with permutation analysis, VT (genomic inflation λ = 1.03). (d) IL18RAP 3′UTR also ranked as the top hit when aggregating variants abrogating or gaining miRNA recognition elements (MREs) in 3’UTRs (genomic inflation λ = 1.04). (e) Schematic of the IL18RAP transcript and 3′UTR (5′ to 3ʹ) showing the number of control (upper) or ALS (lower) samples in which variants (black arrow) were identified in the Project MinE discovery cohort (Supplementary Table 6).
Extended Data Fig. 4 Restricting rare-variant association analysis to the proximal part of 3’UTRs does not improve the association signal.
(a) Scatter plot with SKAT-O P-values (log scale) calculated for region-based rare-variant association analysis of the full 3’UTRs on the x-axis versus the 3’UTRs proximal quadrant on the y-axis, for the 295 3′UTRs listed in Supplementary Table 3, in the Project MinE cohort (3,955 ALS cases and 1,819 non-ALS controls) (Pearson correlation coefficient (r=0.61) and P-value ****<0.0001). The 45-degree diagonal line represents a perfect correlation of r=1. IL18RAP 3′UTR (red). (b) A Difference plot showing the difference between the two P-value measurements (3’UTRs proximal quadrant minus the full 3’UTRs, for the cohort of N=295 3’UTRs). The bias (difference between means) is only 0.03. Overall the P-values gained from the 3’UTRs proximal quadrant were comparable to that of the full 3’UTRs in the cohort of 295 3’UTRs. For box plot, the median is indicated by the central line, upper and lower quartiles are indicated by the box, and maximum/minimum values are indicated by the whiskers (Wilcoxon matched-pairs P-value > 0.05, Cohen’s d effect size = 0.1). Hence, the apparent spatial distribution of variants in IL18RAP 3’UTR seems to be a particular case, rather than part of a global pattern.
Extended Data Fig. 5 IL18RAP and p-NF-κB expression is elevated in lymphoblastoid cells from patients with the C9orf72 repeat expansion.
(a) IL18RAP mRNA expression (qPCR normalized to IPO8 mRNA levels) and (b) IL18RAP or (c) p-NF-κB protein expression (Western blots, normalized to Tubulin). Extracts from eight different human lymphoblastoid cell lines (listed in Supplementary Table 8): Four lines of healthy individuals (without ALS) carrying the canonical IL18RAP 3’UTR sequence (Control; Canonical IL18RAP 3’UTR, black) and four C9orf72 ALS patients carrying the canonical IL18RAP 3’UTR sequence (C9orf72; Canonical IL18RAP 3’UTR, red). (d) Representative blots processed with anti-IL18RAP, anti p-NF-κB and anti-Tubulin antibodies. Mann-Whitney test (A) or one-sided student’s t-test with Welch’s correction on log-transformed data (P = 0.056 for panel B; P = 0.0065 for panel C), was conducted based on the mean value of three independent passages for each of the eight human lymphoblastoid cell lines (Source Data Extended Data Fig. 5). Scatter dot plot with mean and SEM. **P<0.01.
Extended Data Fig. 6 IL18RAP 3’UTR variants attenuate IL-18 - NF-κB signaling in U2OS cells.
Diagram (a) and quantification (b) of NF-κB reporter assays in human U2OS cell line. To determine the ability of the IL18RAP variants V3 and V1 to induce NF-κB activity, U2OS cells were co-transfected with different IL18RAP coding region (CDS) and 3’UTR constructs (GFP, Canonical, V3, V1, n=9; 3CDS, n=4), along with an NF-κB activity reporter that drives luciferase (Luc2P) transcription via five copies of the NF-κB response element. NF-κB signaling was induced by adding human recombinant IL-18 to the medium. Variants V3 and V1 of the IL18RAP 3’UTR reduced NF-κB activity by ~10% and ~21%, respectively, relative to the WT IL18RAP 3’UTR. GFP vector and a dominant-negative coding mutant E210A-Y212A-Y214A CDS + WT 3’UTR (3CDS)31, served as controls. Luciferase expression was normalized to transfected U2OS cells that were not induced with human recombinant IL-18. One-way ANOVA followed by Dunnett’s multiple comparison test was performed on square root-transformed data. For box plots, the median is indicated by the central line, upper and lower quartiles are indicated by the box, and maximum/minimum values are indicated by the whiskers. * P<0.05; *** P<0.001. The experiment was repeated independently three times with similar results.
Extended Data Fig. 7 IL18RAP is mainly expressed on mouse microglia cells.
(a-c) Flow cytometry was used to characterize IL18RAP expression levels in dissociated wild-type mouse cortex cells. The expression of IL-18RAP (IL-18Rβ) was expressed as Mean Fluorescence Intensity (MFI) and % frequency after gating for the following cell types: immune cells (CD45hi), microglia (MG: CD45int CD11hi), neurons (CD45- CD11b- NeuN+), and astrocytes (CD45- CD11b- GFAP+). FACS analysis reveals that IL18RAP is mainly expressed on microglia cells. A scatter dot plot with mean and SEM values for the median fluorescence intensity (MFI) and percentage of IL18RAP+ cells is shown. One-way ANOVA followed by Tukey’s multiple comparison test. ** P<0.01, *** P<0.001, **** P<0.0001.
Extended Data Fig. 8 Evaluation of IL18RAP and IL-18 mRNA expression in motor neurons of patients with ALS.
(a-b) mRNA expression of IL18RAP (a) and IL-18 (b), as reads per kilobase million (RPKM), from NGS study of laser capture microdissection–enriched surviving motor neurons from lumbar spinal cords of patients with sALS with rostral onset and caudal progression (n = 12) and non-neurodegeneration controls (n = 9112; GSE76220). Two-sided Student’s t test with Welch’s correction on log-transformed data (P = 0.0138 for panel A; P = 0.0056 for panel B). (c) IL-18 mRNA expression, as log2-normalized counts, from NGS study of induced ALS motor neurons (n = 4 different donors in duplicates) or non-neurodegeneration controls (n=3 different donors in duplicates113; DESeq analysis, P = 0.0417). For box plots, the median is indicated by the central line, upper and lower quartiles are indicated by the box, and maximum/minimum values are indicated by the whiskers. *P < 0.05; **P < 0.01.
Extended Data Fig. 9 iPSC-derived microglia express the microglial-specific marker, TMEM119.
Immunofluorescence staining of TMEM119 (green) and DAPI (blue), in two different C9orf72 iPSC-derived progenitor microglia lines. Lens, ×20; scale bar, 100 μm.
Extended Data Fig. 10 Differentially bound RNA binding proteins to variant 3’UTR (V3) relative to canonical 3’UTR.
(a) Volcano plot of protein abundance associated with the canonical relative to variant (V3) IL18RAP 3’UTR (x-axis log2 scale), analyzed by MS. Y-axis depicts P-values (−log10 scale). Proteins significantly enriched in association with canonical/variant 3’UTR are colored (gray/orange). Features above the horizontal dashed line demarcate proteins with adjusted p < 0.05, in student’s t-test with FDR correction to multiple hypotheses. Vertical dashed lines are of 2 or ½ fold change (Supplementary Table 9). (b) Prediction of 3’UTR secondary structure by RNA Fold90, suggests a minor change to the structure of the sequence harboring a V3 variant (red), relative to the canonical 3’UTR (green).
Supplementary information
Supplementary Table
Supplementary Tables 1–18 and consortium member lists.
Supplementary Video 1
Motor neuron survival was significantly improved in the presence of microglia harboring variant IL18RAP 3′UTR relative to canonical IL18RAP 3′UTR.
Source data
Source Data Fig. 3
Source data for IL18RAP and p-NF-κB western blot studies in LCLs (Fig. 3d).
Source Data Fig. 4
Source data for IL18RAP western blot studies in isogenic microglia (Fig. 4b).
Source Data Fig. 6
Source data for motor neuron survival assays (Fig. 6b,c).
Source Data Fig. 7
Source data for p-NF-κB western blot studies in isogenic microglia following microglia activation (Fig. 7b).
Source Data Extended Data Fig. 5
Source data for IL18RAP and p-NF-κB western blot studies in control versus C9orf72 LCLs (Extended Data Fig. 5d).
Rights and permissions
About this article
Cite this article
Eitan, C., Siany, A., Barkan, E. et al. Whole-genome sequencing reveals that variants in the Interleukin 18 Receptor Accessory Protein 3′UTR protect against ALS. Nat Neurosci 25, 433–445 (2022). https://doi.org/10.1038/s41593-022-01040-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41593-022-01040-6
This article is cited by
-
Massively parallel screen uncovers many rare 3′ UTR variants regulating mRNA abundance of cancer driver genes
Nature Communications (2024)
-
Unsupervised machine learning identifies distinct ALS molecular subtypes in post-mortem motor cortex and blood expression data
Acta Neuropathologica Communications (2023)
-
Opinion: more mouse models and more translation needed for ALS
Molecular Neurodegeneration (2023)
-
Microglia in neurodegenerative diseases: mechanism and potential therapeutic targets
Signal Transduction and Targeted Therapy (2023)
-
Amyotrophic lateral sclerosis: translating genetic discoveries into therapies
Nature Reviews Genetics (2023)