Abstract
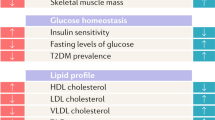
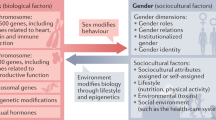
The prevalence of cardiometabolic disorders in both women and men has increased worldwide and is linked to a rise in obesity and obesity-associated associated clustering of other cardiometabolic risk factors such as hypertension, impaired glucose regulation and dyslipidemia. However, the predominance of common types of cardiometabolic disorders such as heart failure, atrial fibrillation and ischemic heart disease is sex specific, and our identification of these and the underlying mechanisms is only just emerging. New evidence suggests that sex hormones, sex-specific molecular mechanisms and gender influence glucose and lipid metabolisms, as well as cardiac energy metabolism, and function. Here we review sex differences in cardiometabolic risk factors, associated preclinical and clinical cardiac disorders and potential therapeutic avenues.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$29.99 / 30 days
cancel any time
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
References
Ng, M. et al. Global, regional, and national prevalence of overweight and obesity in children and adults during 1980–2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet 384, 766–781 (2014).
Razavi, A. C., Potts, K. S., Kelly, T. N. & Bazzano, L. A. Sex, gut microbiome, and cardiovascular disease risk. Biol. Sex. Differ. 10, 29 (2019).
Alpert, M. A., Lavie, C. J., Agrawal, H., Aggarwal, K. B. & Kumar, S. A. Obesity and heart failure: epidemiology, pathophysiology, clinical manifestations, and management. Transl. Res. 164, 345–356 (2014).
Peters, S. A., Huxley, R. R. & Woodward, M. Sex differences in body anthropometry and composition in individuals with and without diabetes in the UK Biobank. BMJ Open 6, e010007 (2016).
Mongraw-Chaffin, M. L., Peters, S. A. E., Huxley, R. R. & Woodward, M. The sex-specific association between BMI and coronary heart disease: a systematic review and meta-analysis of 95 cohorts with 1.2 million participants. Lancet Diabetes Endocrinol. 3, 437–449 (2015).
Peters, S. A., Singhateh, Y., Mackay, D., Huxley, R. R. & Woodward, M. Total cholesterol as a risk factor for coronary heart disease and stroke in women compared with men: a systematic review and meta-analysis. Atherosclerosis 248, 123–131 (2016).
Peters, S. A., Huxley, R. R. & Woodward, M. Diabetes as risk factor for incident coronary heart disease in women compared with men: a systematic review and meta-analysis of 64 cohorts including 858,507 individuals and 28,203 coronary events. Diabetologia 57, 1542–1551 (2014).
EUGenMed Cardiovascular Clinical Study Group et al. Gender in cardiovascular diseases: impact on clinical manifestations, management, and outcomes. Eur. Heart J. 37, 24–34 (2016).
Sharashova, E. et al. Long-term blood pressure trajectories and incident atrial fibrillation in women and men: the Tromso Study. Eur. Heart J. (2019).
Flegal, K. M., Kruszon-Moran, D., Carroll, M. D., Fryar, C. D. & Ogden, C. L. Trends in obesity among adults in the United States, 2005 to 2014. JAMA 315, 2284–2291 (2016).
Marques, A., Peralta, M., Naia, A., Loureiro, N. & de Matos, M. G. Prevalence of adult overweight and obesity in 20 European countries, 2014. Eur. J. Public Health 28, 295–300 (2018).
Mauvais-Jarvis, F. Sex differences in metabolic homeostasis, diabetes, and obesity. Biol. Sex. Differ. 6, 14 (2015).
Fox, C. S. et al. Abdominal visceral and subcutaneous adipose tissue compartments: association with metabolic risk factors in the Framingham Heart Study. Circulation 116, 39–48 (2007).
Despres, J. P. et al. Race, visceral adipose tissue, plasma lipids, and lipoprotein lipase activity in men and women: the Health, Risk Factors, Exercise Training, and Genetics (HERITAGE) family study. Arterioscler. Thromb. Vasc. Biol. 20, 1932–1938 (2000).
Liu, J. et al. Impact of abdominal visceral and subcutaneous adipose tissue on cardiometabolic risk factors: the Jackson Heart Study. J. Clin. Endocrinol. Metab. 95, 5419–5426 (2010).
Fryar, C.D., Ostchega, Y., Hales, C.M., Zhang, G. & Kruszon-Moran, D. Hypertension prevalence and control among adults: United States, 2015–2016. NCHS Data Brief, 1–8 (2017).
Scuteri, A. et al. Longitudinal perspective on the conundrum of central arterial stiffness, blood pressure, and aging. Hypertension 64, 1219–1227 (2014).
Jackson, C. A., Dobson, A., Tooth, L. & Mishra, G. D. Body mass index and socioeconomic position are associated with 9-year trajectories of multimorbidity: a population-based study. Prev. Med. 81, 92–98 (2015).
Oertelt-Prigione, S. et al. Cardiovascular risk factor distribution and subjective risk estimation in urban women—the BEFRI study: a randomized cross-sectional study. BMC Med. 13, 52 (2015).
Pelletier, R. et al. Sex versus gender-related characteristics: which predicts outcome after acute coronary syndrome in the young? J. Am. Coll. Cardiol. 67, 127–135 (2016).
Pelletier, R., Ditto, B. & Pilote, L. A composite measure of gender and its association with risk factors in patients with premature acute coronary syndrome. Psychosom. Med. 77, 517–526 (2015).
Cho, N. H. et al. IDF Diabetes Atlas: global estimates of diabetes prevalence for 2017 and projections for 2045. Diabetes Res. Clin. Pract. 138, 271–281 (2018).
Al-Salameh, A., Chanson, P., Bucher, S., Ringa, V. & Becquemont, L. Cardiovascular disease in type 2 diabetes: a review of sex-related differences in predisposition and prevention. Mayo Clin. Proc. 94, 287–308 (2019).
Lyon, A., Jackson, E. A., Kalyani, R. R., Vaidya, D. & Kim, C. Sex-specific differential in risk of diabetes-related macrovascular outcomes. Curr. Diab. Rep. 15, 85 (2015).
Juutilainen, A. et al. Gender difference in the impact of type 2 diabetes on coronary heart disease risk. Diabetes Care 27, 2898–2904 (2004).
O’Neill, S. & O’Driscoll, L. Metabolic syndrome: a closer look at the growing epidemic and its associated pathologies. Obes. Rev. 16, 1–12 (2015).
Regitz-Zagrosek, V., Lehmkuhl, E. & Mahmoodzadeh, S. Gender aspects of the role of the metabolic syndrome as a risk factor for cardiovascular disease. Gend. Med. 4(Suppl. B), S162–S177 (2007).
Moore, J. X., Chaudhary, N. & Akinyemiju, T. Metabolic syndrome prevalence by race/ethnicity and sex in the United States, National Health and Nutrition Examination Survey, 1988–2012. Prev. Chronic Dis. 14, E24 (2017).
Resnick, H. E. et al. Metabolic syndrome in American Indians. Diabetes Care 25, 1246–1247 (2002).
Huxley, R., Barzi, F. & Woodward, M. Excess risk of fatal coronary heart disease associated with diabetes in men and women: meta-analysis of 37 prospective cohort studies. BMJ 332, 73–78 (2006).
Devereux, R. B. & Alderman, M. H. Role of preclinical cardiovascular disease in the evolution from risk factor exposure to development of morbid events. Circulation 88, 1444–1455 (1993).
Gerdts, E. et al. Left atrial size and risk of major cardiovascular events during antihypertensive treatment: losartan intervention for endpoint reduction in hypertension trial. Hypertension 49, 311–316 (2007).
Gerdts, E. et al. Left ventricular hypertrophy offsets the sex difference in cardiovascular risk (the Campania Salute Network). Int. J. Cardiol. 258, 257–261 (2018).
Lang, R. M. et al. Recommendations for cardiac chamber quantification by echocardiography in adults: an update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. J. Am. Soc. Echocardiogr. 28, 1–39.e14 (2015).
de Simone, G. et al. Does information on systolic and diastolic function improve prediction of a cardiovascular event by left ventricular hypertrophy in arterial hypertension? Hypertension 56, 99–104 (2010).
Halland, H. et al. Sex differences in subclinical cardiac disease in overweight and obesity (the FATCOR study). Nutr. Metab. Cardiovasc. Dis. 28, 1054–1060 (2018).
Halland, H. et al. Effect of fitness on cardiac structure and function in overweight and obesity (the FATCOR study). Nutr. Metab. Cardiovasc. Dis. 29, 710–717 (2019).
de Simone, G. et al. Target organ damage and incident type 2 diabetes mellitus: the Strong Heart Study. Cardiovasc. Diabetol. 16, 64 (2017).
Bella, J. N. et al. Separate and joint effects of systemic hypertension and diabetes mellitus on left ventricular structure and function in American Indians (the Strong Heart Study). Am. J. Cardiol. 87, 1260–1265 (2001).
de Simone, G., Mancusi, C., Izzo, R., Losi, M. A. & Aldo Ferrara, L. Obesity and hypertensive heart disease: focus on body composition and sex differences. Diabetol. Metab. Syndr. 8, 79 (2016).
Gerdts, E. et al. Correlates of left atrial size in hypertensive patients with left ventricular hypertrophy: the Losartan Intervention For Endpoint Reduction in Hypertension (LIFE) Study. Hypertension 39, 739–743 (2002).
Gerdts, E. et al. Gender differences in left ventricular structure and function during antihypertensive treatment: the Losartan Intervention for Endpoint Reduction in Hypertension Study. Hypertension 51, 1109–1114 (2008).
de Simone, G. et al. Lack of reduction of left ventricular mass in treated hypertension: the Strong Heart Study. J. Am. Heart Assoc. 2, e000144 (2013).
De Simone, G. et al. Sex differences in obesity-related changes in left ventricular morphology: the Strong Heart Study. J. Hypertens. 29, 1431–1438 (2011).
Izzo, R. et al. Development of left ventricular hypertrophy in treated hypertensive outpatients: the Campania Salute Network. Hypertension 69, 136–142 (2017).
Tadic, M. et al. The influence of sex on left ventricular strain in hypertensive population. J. Hypertens. 37, 50–56 (2019).
Bella, J. N. et al. Gender differences in left ventricular systolic function in American Indians (from the Strong Heart Study). Am. J. Cardiol. 98, 834–837 (2006).
Williams, B. et al. 2018 ESC/ESH Guidelines for the management of arterial hypertension. Eur. Heart J. 39, 3021–3104 (2018).
Lew, J. et al. Sex-based differences in cardiometabolic biomarkers. Circulation 135, 544–555 (2017).
Ponikowski, P. et al. 2016 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure: the task force for the diagnosis and treatment of acute and chronic heart failure of the European Society of Cardiology (ESC)—developed with the special contribution of the Heart Failure Association (HFA) of the ESC. Eur. Heart J. 37, 2129–2200 (2016).
Yancy, C. W. et al. 2017 ACC/AHA/HFSA Focused Update of the 2013 ACCF/AHA Guideline for the Management of Heart Failure: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines and the Heart Failure Society of America. Circulation 136, e137–e161 (2017).
Regitz-Zagrosek, V., Lehmkuhl, E., Lehmkuhl, H. B. & Hetzer, R. Gender aspects in heart failure. Pathophysiol. Med. Ther. Arch. Mal. Coeur Vaiss. 97, 899–908 (2004).
Lee, D. S. et al. Relation of disease pathogenesis and risk factors to heart failure with preserved or reduced ejection fraction: insights from the Framingham heart study of the national heart, lung, and blood institute. Circulation 119, 3070–3077 (2009).
Ho, J. E. et al. Predictors of new-onset heart failure: differences in preserved versus reduced ejection fraction. Circ. Heart Fail. 6, 279–286 (2013).
Savji, N. et al. The association of obesity and cardiometabolic traits with incident HFpEF and HFrEF. JACC Heart Fail. 6, 701–709 (2018).
Costantino, S. et al. Obesity-induced activation of JunD promotes myocardial lipid accumulation and metabolic cardiomyopathy. Eur. Heart J. 40, 997–1008 (2019).
Murphy, E., Amanakis, G., Fillmore, N., Parks, R. J. & Sun, J. Sex differences in metabolic cardiomyopathy. Cardiovasc. Res. 113, 370–377 (2017).
Schulze, P. C., Drosatos, K. & Goldberg, I. J. Lipid use and misuse by the heart. Circ. Res. 118, 1736–1751 (2016).
Ng, A. C. T. et al. Impact of epicardial adipose tissue, left ventricular myocardial fat content, and interstitial fibrosis on myocardial contractile function. Circ. Cardiovasc. Imaging 11, e007372 (2018).
Kellman, P. et al. Multiecho Dixon fat and water separation method for detecting fibrofatty infiltration in the myocardium. Magn. Reson. Med. 61, 215–221 (2009).
Wei, J. et al. Myocardial steatosis as a possible mechanistic link between diastolic dysfunction and coronary microvascular dysfunction in women. Am. J. Physiol. Heart Circ. Physiol. 310, H14–H19 (2016).
Eugene, A. R. Metoprolol dose equivalence in adult men and women based on gender differences: pharmacokinetic modeling and simulations. Med. Sci. (Basel) 4, (18 (2016).
Santema, B. T. et al. Identifying optimal doses of heart failure medications in men compared with women: a prospective, observational, cohort study. Lancet 394, 1254–1263 (2019).
Bots, S. H. et al. Adverse drug reactions to guideline-recommended heart failure drugs in women: a systematic review of the literature. JACC Heart Fail. 7, 258–266 (2019).
Moss, A. J. et al. Cardiac-resynchronization therapy for the prevention of heart-failure events. N. Engl. J. Med. 361, 1329–1338 (2009).
Tang, A. S. et al. Cardiac-resynchronization therapy for mild-to-moderate heart failure. N. Engl. J. Med. 363, 2385–2395 (2010).
Gillis, A. M. Atrial fibrillation and ventricular arrhythmias: sex differences in electrophysiology, epidemiology, clinical presentation, and clinical outcomes. Circulation 135, 593–608 (2017).
Kirchhof, P. et al. 2016 ESC Guidelines for the management of atrial fibrillation developed in collaboration with EACTS. Eur. Heart J. 37, 2893–2962 (2016).
Ball, J. et al. Sex differences in the impact of body mass index on the risk of future atrial fibrillation: insights from the longitudinal population-based Tromso Study. J. Am. Heart Assoc. 7, e008414 (2018).
Huxley, R. R. et al. Absolute and attributable risks of atrial fibrillation in relation to optimal and borderline risk factors: the Atherosclerosis Risk in Communities (ARIC) study. Circulation 123, 1501–1508 (2011).
Tsang, T. S. et al. Obesity as a risk factor for the progression of paroxysmal to permanent atrial fibrillation: a longitudinal cohort study of 21 years. Eur. Heart J. 29, 2227–2233 (2008).
Lavie, C. J., Pandey, A., Lau, D. H., Alpert, M. A. & Sanders, P. Obesity and atrial fibrillation prevalence, pathogenesis, and prognosis: effects of weight loss and exercise. J. Am. Coll. Cardiol. 70, 2022–2035 (2017).
Conen, D., Glynn, R. J., Sandhu, R. K., Tedrow, U. B. & Albert, C. M. Risk factors for incident atrial fibrillation with and without left atrial enlargement in women. Int. J. Cardiol. 168, 1894–1899 (2013).
Kim, J. S. et al. Influence of sex on the association between epicardial adipose tissue and left atrial transport function in patients with atrial fibrillation: a multislice computed tomography study. J. Am. Heart Assoc. 6, e006077 (2017).
Blum, S. et al. Prospective assessment of sex-related differences in symptom status and health perception among patients with atrial fibrillation. J. Am. Heart Assoc. 6, e005401 (2017).
January, C. T. et al. 2014 AHA/ACC/HRS guideline for the management of patients with atrial fibrillation: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines and the Heart Rhythm Society. J. Am. Coll. Cardiol. 64, e1–e76 (2014).
Zylla, M. M. et al. Sex-related outcome of atrial fibrillation ablation: Insights from the German Ablation Registry. Heart Rhythm 13, 1837–1844 (2016).
Shaw, L. J., Bugiardini, R. & Merz, C. N. Women and ischemic heart disease: evolving knowledge. J. Am. Coll. Cardiol. 54, 1561–1575 (2009).
Garcia, M., Mulvagh, S. L., Merz, C. N., Buring, J. E. & Manson, J. E. Cardiovascular disease in women: clinical perspectives. Circ. Res. 118, 1273–1293 (2016).
Berger, J. S. et al. Sex differences in mortality following acute coronary syndromes. JAMA 302, 874–882 (2009).
Lonnebakken, M. T. et al. Impact of aortic stiffness on myocardial ischaemia in non-obstructive coronary artery disease. Open Heart 6, e000981 (2019).
Eskerud, I., Gerdts, E., Larsen, T. H. & Lonnebakken, M. T. Left ventricular hypertrophy contributes to Myocardial Ischemia in Non-obstructive Coronary Artery Disease (the MicroCAD study). Int. J. Cardiol. 286, 1–6 (2019).
Albrektsen, G. et al. Risk of incident myocardial infarction by gender: interactions with serum lipids, blood pressure and smoking. The Tromso Study 1979–2012. Atherosclerosis 261, 52–59 (2017).
Mieres, J. H. et al. Signs and symptoms of suspected myocardial ischemia in women: results from the What is the Optimal Method for Ischemia Evaluation in WomeN? Trial. J. Women’s. Health (Larchmt.) 20, 1261–1268 (2011).
Sulo, G. et al. Trends in incident acute myocardial infarction in Norway: an updated analysis to 2014 using national data from the CVDNOR project. Eur. J. Prev. Cardiol. 25, 1031–1039 (2018).
Shah, A. S. et al. High sensitivity cardiac troponin and the under-diagnosis of myocardial infarction in women: prospective cohort study. BMJ 350, g7873 (2015).
Labounty, T. M. et al. Body mass index and the prevalence, severity, and risk of coronary artery disease: an international multicentre study of 13,874 patients. Eur. Heart J. Cardiovasc. Imaging 14, 456–463 (2013).
Schulman-Marcus, J. et al. Sex-specific associations between coronary artery plaque extent and risk of major adverse cardiovascular events: the CONFIRM long-term registry. JACC Cardiovasc. Imaging 9, 364–372 (2016).
Taqueti, V. R. et al. Excess cardiovascular risk in women relative to men referred for coronary angiography is associated with severely impaired coronary flow reserve, not obstructive disease. Circulation 135, 566–577 (2017).
Ventura-Clapier, R. et al. Sex in basic research: concepts in the cardiovascular field. Cardiovasc. Res. 113, 711–724 (2017).
Shungin, D. et al. New genetic loci link adipose and insulin biology to body fat distribution. Nature 518, 187–196 (2015).
Stocco, C. Tissue physiology and pathology of aromatase. Steroids 77, 27–35 (2012).
Jankowska, E. A. et al. Circulating estradiol and mortality in men with systolic chronic heart failure. JAMA 301, 1892–1901 (2009).
Kararigas, G. et al. Transcriptome characterization of estrogen-treated human myocardium identifies myosin regulatory light chain interacting protein as a sex-specific element influencing contractile function. J. Am. Coll. Cardiol. 59, 410–417 (2012).
Nelson, J. K. et al. The deubiquitylase USP2 regulates the LDLR pathway by counteracting the E3-ubiquitin ligase IDOL. Circ. Res. 118, 410–419 (2016).
Fliegner, D. et al. Female sex and estrogen receptor-beta attenuate cardiac remodeling and apoptosis in pressure overload. Am. J. Physiol. Regul. Integr. Comp. Physiol. 298, R1597–R1606 (2010).
Witt, H. et al. Sex-specific pathways in early cardiac response to pressure overload in mice. J. Mol. Med. (Berl.) 86, 1013–1024 (2008).
Kararigas, G. et al. Sex-dependent regulation of fibrosis and inflammation in human left ventricular remodelling under pressure overload. Eur. J. Heart Fail. 16, 1160–1167 (2014).
Rattanasopa, C., Phungphong, S., Wattanapermpool, J. & Bupha-Intr, T. Significant role of estrogen in maintaining cardiac mitochondrial functions. J. Steroid Biochem. Mol. Biol. 147, 1–9 (2015).
Sun, L. Y. et al. MicroRNA-23a mediates mitochondrial compromise in estrogen deficiency-induced concentric remodeling via targeting PGC-1alpha. J. Mol. Cell Cardiol. 75, 1–11 (2014).
Rettberg, J. R., Yao, J. & Brinton, R. D. Estrogen: a master regulator of bioenergetic systems in the brain and body. Front. Neuroendocrinol. 35, 8–30 (2014).
Irwin, R. W. et al. Selective oestrogen receptor modulators differentially potentiate brain mitochondrial function. J. Neuroendocrinol. 24, 236–248 (2012).
Chen, J. Q., Eshete, M., Alworth, W. L. & Yager, J. D. Binding of MCF-7 cell mitochondrial proteins and recombinant human estrogen receptors alpha and beta to human mitochondrial DNA estrogen response elements. J. Cell Biochem. 93, 358–373 (2004).
Zhai, P., Eurell, T. E., Cooke, P. S., Lubahn, D. B. & Gross, D. R. Myocardial ischemia-reperfusion injury in estrogen receptor-alpha knockout and wild-type mice. Am. J. Physiol. Heart Circ. Physiol. 278, H1640–H1647 (2000).
Zhai, P. et al. Effect of estrogen on global myocardial ischemia-reperfusion injury in female rats. Am. J. Physiol. Heart Circ. Physiol. 279, H2766–H2775 (2000).
Miller, V. M. & Duckles, S. P. Vascular actions of estrogens: functional implications. Pharmacol. Rev. 60, 210–241 (2008).
Stirone, C., Duckles, S. P., Krause, D. N. & Procaccio, V. Estrogen increases mitochondrial efficiency and reduces oxidative stress in cerebral blood vessels. Mol. Pharmacol. 68, 959–965 (2005).
Essop, M. F., Chan, W. Y. & Taegtmeyer, H. Metabolic gene switching in the murine female heart parallels enhanced mitochondrial respiratory function in response to oxidative stress. FEBS J. 274, 5278–5284 (2007).
Diedrich, M. et al. Heart protein expression related to age and sex in mice and humans. Int. J. Mol. Med. 20, 865–874 (2007).
Liu, H., Yanamandala, M., Lee, T. C. & Kim, J. K. Mitochondrial p38beta and manganese superoxide dismutase interaction mediated by estrogen in cardiomyocytes. PLoS One 9, e85272 (2014).
Zhang, L., Fujii, S. & Kosaka, H. Effect of oestrogen on reactive oxygen species production in the aortas of ovariectomized Dahl salt-sensitive rats. J. Hypertens. 25, 407–414 (2007).
Lagranha, C. J., Deschamps, A., Aponte, A., Steenbergen, C. & Murphy, E. Sex differences in the phosphorylation of mitochondrial proteins result in reduced production of reactive oxygen species and cardioprotection in females. Circ. Res. 106, 1681–1691 (2010).
Westphal, C. et al. CYP2J2 overexpression protects against arrhythmia susceptibility in cardiac hypertrophy. PLoS One 8, e73490 (2013).
Muller, D. N. et al. Mouse Cyp4a isoforms: enzymatic properties, gender- and strain-specific expression, and role in renal 20-hydroxyeicosatetraenoic acid formation. Biochem. J. 403, 109–118 (2007).
Lehti, M. et al. High-density lipoprotein maintains skeletal muscle function by modulating cellular respiration in mice. Circulation 128, 2364–2371 (2013).
Ferrara, L. A. et al. Cardiometabolic risk in overweight subjects with or without relative fat-free mass deficiency: the Strong Heart Study. Nutr. Metab. Cardiovasc. Dis. 24, 271–276 (2014).
Bohm, C. et al. Sexual dimorphism in obesity-mediated left ventricular hypertrophy. Am. J. Physiol. Heart Circ. Physiol. 305, H211–H218 (2013).
Petrov, G. et al. Maladaptive remodeling is associated with impaired survival in women but not in men after aortic valve replacement. JACC Cardiovasc. Imaging 7, 1073–1080 (2014).
Petrov, G. et al. Regression of myocardial hypertrophy after aortic valve replacement: faster in women? Circulation 122, S23–S28 (2010).
Tiyerili, V. et al. Estrogen improves vascular function via peroxisome-proliferator-activated-receptor-gamma. J. Mol. Cell Cardiol. 53, 268–276 (2012).
Dworatzek, E. et al. Sex-specific regulation of collagen I and III expression by 17beta-estradiol in cardiac fibroblasts: role of estrogen receptors. Cardiovasc. Res. 115, 315–327 (2019).
Sanchez-Ruderisch, H. et al. Sex-specific regulation of cardiac microRNAs targeting mitochondrial proteins in pressure overload. Biol. Sex. Differ. 10, 8 (2019).
Srivastava, S. et al. Estrogen decreases TNF gene expression by blocking JNK activity and the resulting production of c-Jun and JunD. J. Clin. Invest. 104, 503–513 (1999).
Czubryt, M. P., McAnally, J., Fishman, G. I. & Olson, E. N. Regulation of peroxisome proliferator-activated receptor gamma coactivator 1 alpha (PGC-1 alpha) and mitochondrial function by MEF2 and HDAC5. Proc. Natl Acad. Sci. USA 100, 1711–1716 (2003).
Author information
Authors and Affiliations
Contributions
E.G. and V.R-Z. both drafted and contributed to the manuscript and approved the final version.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Peer review information Hannah Stower was the primary editor on this article and managed its editorial process and peer review in collaboration with the rest of the editorial team.
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Gerdts, E., Regitz-Zagrosek, V. Sex differences in cardiometabolic disorders. Nat Med 25, 1657–1666 (2019). https://doi.org/10.1038/s41591-019-0643-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41591-019-0643-8
This article is cited by
-
The explanation of educational disparities in adiposity by lifestyle, socioeconomic and mental health mediators: a multiple mediation model
European Journal of Clinical Nutrition (2024)
-
Gender Differences in Cardiac Organ Damage in Arterial Hypertension: Assessing the Role of Drug Nonadherence
High Blood Pressure & Cardiovascular Prevention (2024)
-
Sex-Stratified Predictors of Prolonged Operative Time and Hospital Admission in Outpatient Parathyroidectomy
Indian Journal of Otolaryngology and Head & Neck Surgery (2024)
-
Association of clinical, laboratory and imaging biomarkers with the occurrence of acute myocardial infarction in patients without standard modifiable risk factors – rationale and design of the “Beyond-SMuRFs Study”
BMC Cardiovascular Disorders (2023)
-
Sexual dimorphism in mitochondrial dysfunction and diabetes mellitus: evidence from a population-based cohort study
Diabetology & Metabolic Syndrome (2023)