Abstract
Development of a malaria vaccine remains a critical priority to decrease clinical disease and mortality and facilitate eradication. Accordingly, RTS,S, a protein-subunit vaccine, has completed phase III clinical trials and confers ~30% protection against clinical infection over 4 years. Whole-attenuated-sporozoite and viral-subunit vaccines induce between 20% and 100% protection against controlled human malaria infection, but there is limited published evidence to date for durable, high-level efficacy (>50%) against natural exposure. Importantly, fundamental scientific advances related to the potency, durability, breadth and location of immune responses will be required for improving vaccine efficacy with these and other vaccine approaches. In this Review, we focus on the current understanding of immunological mechanisms of protection from animal models and human vaccine studies, and on how these data should inform the development of next-generation vaccines. Furthermore, we introduce the concept of using passive immunization with monoclonal antibodies as a new approach to prevent and eliminate malaria.
Similar content being viewed by others
Main
A first guiding principle for the rational development of any vaccine is to formulate a hypothesis regarding the type of adaptive immune response required to mediate protection. For malaria, understanding the life cycle of the infection and determining the immune responses that confer protection after natural infection provide important insights for vaccine development. Malaria parasites have multiple stages of infection, thus making vaccine design more complex than for most viral and bacterial infections for which effective vaccines have been developed, because protection can occur through different immunological mechanisms depending on the specific stage of infection. Infection is initiated when, via bites by mosquitoes, sporozoites are delivered into the skin and the surrounding microvasculature of the host (Fig. 1). Minutes to hours later, sporozoites migrate to the liver and enter the hepatocytes1. Within an infected hepatocyte, a single Plasmodium falciparum sporozoite can develop into ~30,000 merozoites over a period of ~7 d. Together, this sequence defines the clinically asymptomatic preerythrocytic stage of infection. The blood stage of infection commences when the merozoites enter red blood cells (RBCs) and initiate a continuous cycle of asexual infection that can cause clinical symptoms and mortality. A small number of parasites in the blood develop into sexual-stage gametocytes, which can be taken up by the mosquito and continue the cycle of infection.
Malaria infection is initiated when the bite of an infected mosquito delivers parasites in the form of sporozoites into the skin and local blood vessels of the host. A small number of sporozoites migrate via the blood stream to the liver. At this stage, antibodies can prevent sporozoites from reaching the liver, particularly those targeting the major circumsporozoite surface protein (CSP). After sporozoites have infected hepatocytes, liver-stage parasites can be eliminated by cell-mediated immunological mechanisms. These characteristics define the clinically asymptomatic preerythroctyic stage of infection. Vaccines for the preerythrocytic stage of infection are focused on preventing sporozoites from reaching the liver by inducing antibodies, eliminating parasites in the liver by T cells or both. In the liver, a single sporozoite can expand into ~30,000 merozoites over a period of 7 d for P. falciparum, after which they can emerge from the liver and establish blood-stage infection, which induces morbidity and mortality. In the blood, parasites can be cleared in the spleen and sequestered in the peripheral vasculature by using variant surface antigens. Most blood-stage vaccines focus on developing antibody responses against proteins that are involved in invasion of RBCs. Importantly, RBC invasion is a rapid process with limited time for antibodies to mediate protection. Finally, a subset of blood-stage parasites take a different developmental pathway and become sexual gametocytes, which are taken up by mosquitoes and initiate the mosquito stage of infection.
Naturally acquired immunity refers to whether the infection itself induces protection. Such protection is indeed the case with many viral infections and can provide insight into the type of immune response required for vaccine protection. Natural immunity against malaria develops against the blood stage of infection, thereby providing protection against clinical disease; however, adults remain susceptible to repeated infections, suggesting that there is little or no natural immunity developed against the preerythrocytic stages, i.e., to the parasite in the liver2,3,4,5,6. Of note, blood-stage immunity requires continuous exposure to induce and maintain protection against clinical disease and mortality, and such immunity is not sterilizing2,3. This immunity is mediated largely by antibodies that target Plasmodium antigens on the RBC surface that facilitate adhesion and allow the parasite to avoid clearance by the spleen7,8. However, these blood-stage surface antigens can be highly variable, and this variability limits their potential as targets for vaccine development7,8. Naturally acquired immunity can also target multiple merozoite surface proteins that facilitate RBC adhesion and invasion, although these molecules are often highly polymorphic9. Finally, data from mouse models show that, in addition to antibodies, CD4+ and CD8+ T cells can mediate protective blood-stage immunity10,11,12,13.
Because repeated malaria infection (natural immunity) has limited ability to induce immunity at the preerythrocytic stage and consequently prevent blood-stage infection, investigators have sought to assess other approaches for preventing infection. Although there was some prior evidence in avian malaria that attenuated sporozoites can confer protection against live-parasite challenge14,15, the seminal discovery by Nussenzweig and colleagues in the 1960s that radiation-attenuated sporozoites (RAS) administered to mice induces complete protection at the preerythrocytic stage of infection was the starting point for intensive investigation of this approach16. Importantly, these findings with rodent Plasmodium parasites were confirmed in human studies showing that the bites of hundreds to thousands of irradiated P. falciparum–infected mosquitoes protected subjects after a controlled human malaria infection (CHMI)17,18. RAS vaccination induces production of antibodies that can prevent parasites from reaching the liver and T cell responses that eliminate parasites from hepatocytes19,20,21. It is the cellular immune response that is likely to be necessary and sufficient to mediate durable protection by RAS. The ability of RAS vaccination to mediate protection at the preerythrocytic stage, compared with natural exposure, is likely to be due to the delivery of thousands to millions of sporozoites administered by thousands of mosquito bites or more recently by vaccination, as compared with natural exposure by occasional mosquito bites, in which ~100 sporozoites are delivered per bite22. Moreover, as RAS immunization does not lead to blood-stage infection, as would be the case with natural infection, there is no influence by the immunoregulatory effects that blood-stage infection can have on the development of adaptive immunity23,24.
The life cycle of malaria infection and the analysis of immunity to malaria has led to the development of several vaccine approaches (summarized in Table 1 and Fig. 1). RTS,S, the most advanced malaria subunit-vaccine candidate, aims to induce antibodies that target the circumsporozoite protein (CSP), the most abundant protein on the surface of the sporozoite, thereby preventing them from reaching the liver25. The ability of T cell immunity induced by RAS immunization to provide protection in the liver has provided a rationale for whole-sporozoite and viral-vaccine approaches to protect the host by eliminating infection in the liver. Over the past several years, a variety of whole-sporozoite vaccine approaches have been based on the data from RAS vaccines18. These include the PfSPZ Vaccine, a preparation of RAS that are sterile and cryopreserved, as well as the related approaches of genetically attenuated parasites (GAPs), which self-attenuate at various stages in the liver, and chemotherapy with Plasmodium sporozoites (CPS), in which live sporozoites are administered via mosquito bites or as purified PfSPZ (also termed Cvac), thus allowing for full liver-stage infection before chemoprophylaxis is provided to control blood-stage infection26,27,28. Subunit vaccines based on DNA and viral vectors have also been developed to induce cell-mediated immunity and eliminate infection in the liver. Finally, whole-parasite vaccines, protein-subunit vaccines and, more recently, viral-vector vaccines targeting the blood stage of infection have been developed. Most efficacy studies in humans have been performed with preerythrocytic vaccines to target the asymptomatic stage of infection and either prevent infection or decrease clinical disease. Overall, although both scientific and clinical progress have been made with a variety of vaccines, none of the current approaches are sufficiently effective for long-term sterile protection.
In this Review, we focus on how the magnitude, quality, breadth and location of immune responses affect protection at different stages of P. falciparum infection. On the basis of these data, we highlight the specific scientific hurdles that must be overcome to improve malaria-vaccine efficacy with current approaches. This article is not meant to provide an exhaustive review of all malaria-vaccine trials or to encompass the field of transmission-blocking vaccines (reviewed elsewhere29) but instead is intended to highlight the basic immunological mechanisms that can be harnessed for vaccine-mediated protection.
Cellular mechanisms of protection against preerythrocytic stages
The major focus on cell-mediated immunity for vaccines at the preerythrocytic stage (liver stage) is based on long-standing data from mice and nonhuman primates after RAS immunization20,21,30. These data show that CD8+ T cells are potent effectors capable of clustering around and eliminating infected hepatocytes31,32,33 (Fig. 2). Although most evidence shows that the cytokine IFN-γ is the key mediator of protection, some reports have shown an IFN-γ-independent mechanism34,35. CD4+ T cells are also required for RAS-mediated immunity in some mouse models of malaria infection19,36. CD4+ T cell responses can mediate protective immunity through a variety of mechanisms, such as increasing the survival and proliferation of CD8+ T cells37 (Fig. 2) or acting as direct effectors through production of IFN-γ (refs 36,38,39).
CD8+ T cells are primed by dendritic cells (DCs) that have taken up sporozoites in the spleen after intravenous immunization with RAS vaccines. The magnitude and durability of CD8+ T cell responses may be influenced by CD4+ T cells or γδ T cells during the priming phase. CD8+ memory T cells circulate, and a proportion of them become resident in the liver (TRM cells), as a result of reexposure to antigen (Ag) or local inflammation. TRM cells in the liver migrate in the sinusoids in an LFA-1-dependent manner until they encounter infected hepatocytes. Clusters of CD8+ T cells can form around infected hepatocytes, thus leading to parasite elimination. Inset shows a two-photon image of sporozoite-specific CD8+ TRM cells in the liver patrolling the hepatic sinusoids, which are dark in contrast with the autofluorescent hepatocytes 4 weeks after immunization with RAS. Micrograph reprinted with permission from ref. 66, AAAS. Scale bar, 50 μm.
The current vaccine approaches to induce cell-mediated immunity against the liver stage are with whole-sporozoite and subunit DNA or viral-vector vaccines. Results from several human clinical studies have shown that immunization with the PfSPZ Vaccine confers up to 100% short-term sterile protection after CHMI with homologous parasites and ~60% sterile protection for 1 year after CHMI with homologous parasites or a single heterologous strain in adults in the United States with no prior malaria exposure40,41,42,43. However, in PfSPZ Vaccine studies in adults in Mali who had substantial prior or ongoing malaria exposure, using the same dose and regimen as those used in some of the US trials, the protection at 6 months was found to be ~30% by proportional analysis and ~50% by time-to-event analysis44. In that study, ~100% of subjects in the placebo group were infected over the 6 months after the final immunization, thus demonstrating the difficulties that a malaria vaccine may need to overcome in the setting of such high-level exposure. These data highlight how prior and ongoing malaria exposure may limit optimal immunity and protection with this single-strain vaccine against intense heterogeneous parasite exposure. In terms of defining the immunological correlates of protection after immunization with the PfSPZ Vaccine in humans, it is notable that PfSPZ-specific CD8+ T cells are not consistently induced in the blood of many of the vaccinated subjects that are protected. Moreover, CD8+ T cell responses in the blood are highest after the first immunization, and no additional boosting occurs after subsequent immunizations42. These data suggest that CD8+ T cells are primed in secondary lymphoid organs, such as the spleen, after the primary immunization and immediately migrate to the liver45,46. Indeed, nonhuman-primate studies have shown that PfSPZ-specific CD8 T cell responses can be three to four log units higher in the liver than the blood after intravenous immunization40,41. Thus, understanding the role of CD8+ T cell responses in vaccine-elicited protection may be limited from blood analysis40,41. In contrast to the poor induction of circulating CD8+ T cells, immunization of humans with the PfSPZ Vaccine, CPS or Cvac in adults in the United States or Europe consistently induces a high frequency of multifunctional cytokine or cytolytic CD4+ T cells in the blood, and these effects have been correlated with protection in some of the studies27,28,40,41,42,47.
A remarkable and provocative finding from both preclinical mouse and human trials is the potential role of γδ T cells, notably those expressing Vγ9Vδ2 chains, in protection by sporozoite vaccines or natural infection40,41,47. An older study in mice suggested that γδ T cells may have some protective activity after RAS immunization38. More recently, in two separate studies, the frequency of Vγ9Vδ2 T cells before vaccination with the PfSPZ Vaccine has been found to correlate with protection in adults in the United States and Mali40,41. In agreement with these findings, depletion of γδ at the time of RAS immunization has been found to limit the induction of T cell immunity and subsequent protection in mice; however, their ablation immediately before challenge has no effect on protection48. Together, these data highlight a potentially important role for Vγ9Vδ2 T cells in priming T cell responses with sporozoite vaccines. Indeed, because γδ T cells directly respond to certain phosphoantigens expressed by sporozoites and become activated and secrete IFN-γ, they may provide ‘adjuvant’-like effects that enhance antigen presentation by dendritic cells at the initiation of the response49 (Fig. 2). Importantly, the frequency of Vγ9Vδ2 T cells increases with age but decreases with malaria exposure, thus leading to the possibility that whole-sporozoite vaccines might be less effective in malaria-exposed younger children or infants if such cells have a critical role in T cell priming with the PfSPZ Vaccine50,51.
Subunit vaccines may also generate T cell responses that protect against liver stages. For example whereas RTS,S with the AS01 adjuvant mediates most of its effects through antibodies (as discussed below) there is some evidence that protection may be associated with CD4+ T cells targeting T cell epitopes included in the C terminus of CSP52. The most directed subunit-vaccine approach to elicit T cells to control liver-stage infections is heterologous prime-boost immunization using DNA and recombinant viral vaccines. Although such approaches can protect mice53, in humans they have achieved only ~20% short-term protection after CHMI, and there is no evidence of sustained protection in field studies54,55,56,57. The limited protection in humans with these viral vaccines might be due to the lack of antigenic breadth or to a failure to achieve high frequencies of CD8+ T cells in the liver. Changes in vaccine delivery and defining new protective antigens will be critical for improving viral-vector vaccines.
Magnitude: how many CD8+ T cells are needed for protection?
A critical metric that should facilitate the development of vaccines for infections, such as malaria, which require T cells at specific tissue sites, is to define the frequency of antigen-specific cells required for protection. A major hurdle to inducing protective immunity in the liver by T cell immunity is based on the requirement to have a sufficient frequency of cells to cover all focal areas of infection in a large organ such as the liver58,59. To determine the number of CD8+ T cells required for durable liver-stage protection against malaria challenge in mice, one study has used primed T cells in mice against a well-characterized protective T cell epitope in CSP, by using peptide-pulsed dendritic cells and recombinant Listeria to induce high numbers of cells60. Strikingly, the mice were protected only if more than 10% of total circulating CD8+ T cells were specific for CSP. Current prime-boost approaches in humans with subunit vaccines or whole-sporozoite vaccines do not elicit this number of T cells in blood either as a response to specific antigens or throughout the total sporozoite response, respectively40,55. The most advanced viral-vector-vaccine approach in humans against malaria is with chimpanzee adenovirus 63 (ChAd63) and modified Vaccinia Ankara (MVA) encoding the thrombospondin-related adhesive protein (TRAP) conjugated to a multiepitope (ME) string of other parasite antigens (TRAP–ME). This prime-boost immunization approach induces TRAP–ME-specific T cells in the blood at a peak frequency of ~0.24% of peripheral blood mononuclear cells several weeks after the boost, and it confers ~20% sterile short-term protection by CHMI in malaria-naive individuals55. However, frequencies of ~10% of CD8+ T cells in the blood specific for a single epitope can be seen in humans after human cytomegalovirus (CMV) infection61. The potency and durability of CMV-specific CD8 T cell responses to natural infection in humans has provided the fundamental basis for developing CMV-based vaccine vectors encoding specific antigens for HIV and tuberculosis. Data from nonhuman-primate simian immunodeficiency virus and tuberculosis vaccine and infection models show that rhesus CMV vectors induce high-frequency T cell responses in the blood and other tissues, including the liver62,63. These data suggest that this is platform may potentially be useful for malaria vaccines, if protective T cell epitopes can be defined and if these vectors are able to induce immunity in the majority of individuals who have been exposed to human CMV.
Location: tissue-resident memory T cells in the liver are critical for vaccine protection
Because the liver is the site where parasites must be eliminated to prevent blood-stage malaria infection, vaccines must be able to efficiently generate T cell responses that will be induced in, or migrate to, the liver. Recently, substantial analysis has been performed on the roles of tissue-resident memory cells (TRM cells), a highly specialized population of nonrecirculating cells that act as sentinels and effectors in the tissue sites and are capable of mediating protection against specific pathogens (reviewed in ref. 64). TRM cells induced in the liver have been shown to be powerful mediators of protection against malaria59,65 (Fig. 2). Liver TRM cells have several unique properties compared with those of other TRM cells; in particular, they have a distinct patrolling behavior that allows them to scan the liver sinusoids for pathogens59,66; however, they avoid entering the general circulation by expressing high levels of the adhesion molecule LFA-1 (ref. 66). Therefore, the prevention of preerythrocytic-stage malaria infection is likely to require vaccine strategies that favor a high frequency of TRM cells in the liver.
A major advance for inducing high frequencies of sporozoite-specific CD8+ T cells in the liver has come from comparing immunization with the PfSPZ Vaccine by subcutaneous and intravenous routes in nonhuman primates. Strikingly, intravenous immunization induces high frequencies (~3%) of sporozoite-specific T cells in the liver several months after the final immunization, whereas the subcutaneous route results in nearly undetectable responses40,41,67. This study provided the basis for the first clinical trial assessing the safety, immunogenicity and protection by intravenous immunization as a preventive vaccine in humans. The ability of intravenous immunization to confer ~80% short-term protection by CHMI, in contrast to a prior observation that subcutaneous immunization with the same dose and regimen had limited immunity and protection, provides clear evidence for how the intravenous route is critical for protection against malaria with this vaccine41,67. Subsequently, another conceptually similar vaccine approach is the so-called ‘prime and trap’ strategy in mice. In this protocol, CD8+ T cells are primed with an intravenously delivered antigen targeted to dendritic cells, and are immunized 1 day later with a hepatotropic adeno-associated virus to draw the T cells into the liver and trap them there59. This immunization regimen induces large numbers of liver TRM cells, which are capable of conferring high-level protection in mice; however, this effect was lost when the liver TRM were depleted with an anti-CXCR3 antibody59. On the basis of these data, clinical trials are now in progress with intravenously delivered viral vectors to achieve a similar boost in liver TRM cells. A critical question for vaccine development is the longevity of TRM cell populations in the liver. In some organs, notably the skin, TRM cell populations appear stable over long periods of time68; however, in the lung, TRM cell populations decline rapidly and are replaced from circulating T cell populations69,70. These data suggest that long-lived protective responses might require a sufficient number of TRM cells at the time of infection and an additional reservoir of circulating T cells in secondary lymphoid organs to replenish the TRM cell population. Because there is no current evidence that malaria infection boosts preerythrocytic immunity3, maintaining a protective threshold of TRM cells in the liver might require periodic boosting.
Antigenic breadth is a key determinant of protection: lessons from whole-parasite vaccines
A potential advantage of whole-sporozoite vaccines versus subunit vaccines is that they are composed of as many as ~2,000 proteins71 and may induce responses of greater antigenic breadth. However, because RAS vaccines are fully attenuated, they arrest early and do not undergo the full liver-stage expansion that would increase the breadth of immunity. Thus, to maximize the breadth of the immune response by allowing the sporozoites to expand through the liver; CPS studies were performed with live sporozoites administered by mosquito bites in the presence of chloroquine chemoprophylaxis28,72. This approach allows for full expansion of sporozoites in the liver stage and limited blood-stage infection that is eliminated by the drug. Malaria-naive subjects immunized by CPS had complete protection (ten of ten subjects) against CHMI after three exposures to 15 infectious mosquito bites28. This result provides a striking contrast with protection by RAS vaccination, which has been found to require up to 1,000 mosquito bites18. These data highlight the greater efficiency of CPS for protection after CHMI with a parasite homologous to the vaccine. More recently, complete protection in CHMI has been obtained in a dose-dependent manner by using Cvac, which are cryopreserved live sporozoites administered intravenously with chemoprophylaxis27. These CPS and Cvac studies in adults in the United States and Europe have provided an important proof of concept for the greater efficiency of this approach compared with RAS, per mosquito bite or sporozoite, against homologous CHMI, by using the natural biology of liver-stage expansion to enhance immunity and protection. However, whereas CPS confers complete protection against homologous challenge strains during CHMI, protection against two different heterologous strains has been found to be limited73,74.
The failure of CPS to protect against heterologous parasites is somewhat surprising, given the basic premise that full infection in the liver would increase the magnitude and breadth of T cell responses, as compared with those to RAS26,75. One explanation is that the heterologous parasite strains used for CHMI in these CPS studies (NF135.C10 and NF166.C8) are more infectious than the related NF54 and 3D7 strains used in most CHMI studies73,74. Alternatively, data from an infection and treatment approach in mice show an induction of both T cell and antibody responses to blood-stage antigens, which may contribute to protection26,76. However, no differences have been observed in parasite growth between human subjects receiving CPS immunization and control individuals after direct blood-stage challenge77, thus suggesting that this vaccine approach confers protection exclusively through the liver stage. An alternative hypothesis is that the blood-stage parasites used for the CHMI might contain antigenically diverse parasites, whereas the parasites that emerge from the liver after CPS immunization may be more homogenous, because the variant surface antigens of Plasmodium blood stages are reset during the sexual stages78. Thus, during CPS vaccination, each individual will probably have been repeatedly exposed to the same surface antigens, including at challenge, and these antigens might be the target of potent blood-stage immunity. This hypothesis may account for the strong strain-specific protection induced by CPS and the lack of protection against blood-stage infection in the previous human study. In future studies, fully delineating the mechanisms of protection by CPS or Cvac will be critical. Because Cvac uses purified PfSPZ administered through an intravenous route, it can deliver far greater numbers of sporozoites per immunization than the CPS approach using mosquito bites. Thus, future studies with Cvac using much higher doses of PfSPZ with different drug treatments that can eliminate parasites in the liver or early blood stages should clarify the likely importance of T cells in the liver for mediating protection. Finally, establishing whether Cvac can confer high-level and durable protection against heterogeneous parasites in field studies will be the ultimate test of whether this approach is superior to RAS.
A second approach for enhancing the antigenic breadth of sporozoite vaccines compared with RAS is to use GAPs that arrest at a defined point in the late liver stage71,79. In mouse models, late-arresting GAPs induce a higher frequency of CD8+ T cell responses than RAS vaccination and protect animals at lower immunizing doses than early-arresting parasites75. Thus, late-acting GAP vaccines offer the potential advantage of having more robust immunogenicity and breadth than RAS vaccines, but would not require drug treatment as with Cvac. However, in the first human study with a GAP vaccine containing two gene deletions, breakthrough infection was observed in one of six subjects80. A more recent study using a GAP vaccine bearing three gene deletions that arrests early in the liver stage, which was administered by mosquito bites to humans, had no breakthrough infection81. Ongoing trials with this and other first-generation GAP vaccines that have been purified and administered intravenously will generate important comparative data for assessing PfSPZ vaccines and provide a benchmark for subsequent studies with late-acting GAP vaccines.
In conclusion, given the complex genetic diversity of P. falciparum, it is essential that all sporozoite approaches demonstrate protection against heterogeneous strains in field studies at different sites. We speculate that improving the efficacy of sporozoite vaccines will require using multiple strains from geographically diverse areas to enable cross-strain protection.
Defining the targets of protective cell-mediated immunity
Although whole-sporozoite vaccines provide greater and more consistent protective efficacy than viral-vectored vaccines against CHMI, the protective epitopes have not been clearly delineated. An understanding of these epitopes would provide insight into how sporozoite vaccines mediate protection and should improve vaccine development for viral-vaccine and other subunit-vaccine approaches. Importantly, not all antigen-specific CD8+ T cell responses induced by sporozoite immunization are protective82, probably because target proteins must enter the cytosol of the host cell to be presented on major histocompatibility complex (MHC) class I, thereby limiting the number of potential protective antigens32,83. However the mechanisms mediating export of protein into host hepatocytes are unclear, and Pexel motifs, which define a proteolytic-cleavage site that is critical for this process in infected erythrocytes, have been found to be dispensable for host-cell targeting in the liver stages32,83. Two antigens, CSP and TRAP, have been confirmed as targets of protective immunity in rodent models, although protection depends on the mouse strain carrying an MHC molecule capable of presenting antigen-derived peptides82,84,85. Notably, transgenic mice that express CSP, and are thus tolerant to this antigen, are still protected by multiple immunizations with RAS86. Similarly, RAS immunization can protect against challenge with genetically engineered parasites expressing antigenically distinct CSP molecules87. Both of these studies have shown that anti-CSP T cell responses are not absolutely required for protection. The low frequency of CSP-specific T cells in humans after RAS or PfSPZ vaccination that are protected after CHMI also suggests that additional T cell epitopes are important for mediating protection41,88.
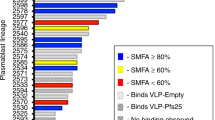
Several studies have determined the breadth of protective antigen responses in mice and humans receiving whole-sporozoite vaccines. In humans immunized with RAS through mosquito bites, T cell responses to 27 candidate antigens have been assessed in the blood in protected and unprotected subjects. The results led to the identification of the Plasmodium cell traversal protein CelTOS as a vaccine candidate, because this antigen was found to elicit elevated T cell responses in protected individuals88. However, follow-up studies using this antigen in mice and humans have shown limited efficacy89. More recently, T cell responses to the antigens CSP, LSA1 and TRAP have been measured in protected subjects who received the PfSPZ Vaccine, although these responses were very low (<50 IFN-γ spot-forming cells per million peripheral blood mononuclear cells)41. Future efforts using large blood volumes from protected and nonprotected individuals across different MHC types, with peptides encompassing the liver-stage proteome, might aid in identifying protective epitopes. On the basis of the current data, protection by whole-sporozoite vaccines is likely to be mediated by either low-level T cell responses to many different antigens or higher responses to specific antigens that have not yet been identified.
Another approach, evaluated in mice, is to identify potential antigens on the basis of either their expression profiles or whether they are the targets of immune responses in humans90,91. In these screens, antigens are formulated as subunit vaccines for an initial assessment of their ability to induce protective immunity, thus leading to the identification of some promising candidates90,91,92. Finally, mass spectrometry techniques could be used to identify parasite epitopes presented by MHC class I molecules on the surfaces of infected hepatocytes. This approach has been used to identify targets of antiviral and antitumor immunity93. However, for malaria, this approach currently remains an elusive goal, because the proportion of infected cells in hepatocyte cultures is too low to allow sufficient material to be obtained. However, continued advances in the sensitivity of mass spectrometry techniques and parasite culture may make this approach feasible in the near future.
Antibody-mediated protection
Most approved vaccines mediate protection against viral and bacterial pathogens through the induction of antibody responses94. Such protection is usually long lasting and is achieved by a variety of vaccine formulations without a requirement for additional boosting. In understanding antibody-mediated immunity, it is critical to define the protective threshold and an antibody-titer ‘inflection point’, i.e., the level at which antibody titers stabilize after the initial antibody spike induced by immunization. After the inflection point, antibody titers generally decline much more slowly95. For current effective vaccines against bacterial and viral infections, the protective threshold is low and well below the inflection point of the vaccine; consequently, protection is long lived96. As such, improving vaccines that prevent sporozoites from reaching the liver, or that block the asexual cycle in the blood, would require raising the inflection point and decreasing the rate of decay of the antibody responses. These requirements could be achieved through improvements in vaccine delivery or regimen and adjuvant approaches that favor more durable immunity. Alternatively, lowering the protective threshold by increasing the potency and breadth of the antibodies induced by vaccination may also be required. In this section, we examine these issues by focusing on antibody responses against the preerythrocytic antigen CSP and the blood-stage antigens AMA-1 and Rh5. These antigens have the most extensive structural and mechanistic immunological data from both mouse and human studies.
The role of antibodies in preerythrocytic immunity was first established when the passive transfer of sera from RAS-immunized mice was demonstrated to delay patency in Plasmodium berghei infection97. More recently, these results have been substantiated through the transfer of sera from PfSPZ Vaccine– or CPS-immunized human volunteers to P. falciparum–challenged, immunodeficient mice carrying human hepatocytes resulting in a significant decrease in liver parasite burden40,98,99,100. Inhibitory monoclonal antibodies isolated from RAS-immunized mice have been found to target the central-repeat region of CSP, consisting of ~40 NANP amino acid repeats interspersed with approximately four NVDP amino acid repeats mainly concentrated near the N terminus (Fig. 3a), which thus became a leading candidate for subunit-vaccine approaches such as RTS,S101. The RTS,S vaccine contains 18 NANP repeats as well as a truncated C-terminal domain, which has conserved epitopes for inducing CD4 T cell responses that may provide help to B cells25. RTS,S does not contain any portion of the N-terminal domain, junction region or the NVDP repeats, some of which have recently been shown to be targets of protective antibodies102,103,104. In phase III clinical trials, RTS,S has been found to confer up to ~50% protection against clinical infection in the first year after three vaccinations and ~30% protection over a 4-year follow up in infants 5–17 months of age who received an additional booster vaccine105. Protection is correlated with anti-CSP titers, which are initially very high (~200 ELISA units (EU)/ml in infants and ~500 EU/ml in older children) but decline in the first 4 months to ~10% of the peak (the inflection point). This level is well below the estimated protective threshold of 121 EU/ml (Fig. 3b)106, thus providing an explanation for why protection wanes over time. The protective cutoff appears to be one to two orders of magnitude greater than the antibody titers required to protect against tetanus, measles and probably many other viral or bacterial infections94. Such high titers are required because antibodies must block every single parasite within the minutes to hours before they reach the liver, thus limiting the time for an anamnestic response. Finally, antibodies targeting other antigens expressed at the preerythrocytic stage, such as PfMAEBL, have been demonstrated to inhibit sporozoite invasion of human hepatocytes in vitro, although whether such antibodies can protect in vivo remains unclear99. Overall, antibodies against additional antigens may possibly have inhibitory activity that can be additive or synergistic to those against CSP107.
a, Schematic of the structure of CSP, with region 1 (R1) in red, NANP repeats in orange, NVDP repeats in blue and the region 2 (R2) thrombospondin repeats (TSR) in green. The partial NANP repeat and C-terminal domain included within the RTS,S vaccine that are fused to hepatitis B–based virus-like particle are marked (RTS,S vaccine component). b, After three doses of RTS,S at 4-week intervals, 5- to 17-month-old subjects have high titers of antibody specific for CSP (200–500 EU depending on age; data from ref. 106). This titer declines within 1 year to ~10% of the peak titer, which is below the estimated protective threshold of 121 EU/ml. Antibody titers continue to decline but more slowly, with a half-life of ~600 d. Improving immunity and protection by a subunit vaccine designed to induce antibodies would require decreasing the protective-antibody threshold by generating antibodies with greater potency, increasing the inflection point above the protective threshold by using different adjuvants, or altering the vaccine regimen or modifying the immunogen and adjuvant to elicit a more efficient GC reaction, memory B cells and LLPCs.
Given the number of parasites released from the liver and the kinetics of infection of RBCs, blocking blood-stage infection will also require a high titer of antibodies108,109. In blood-stage infection, antibodies do not need to neutralize every parasite but ideally would decrease the replication rate to <1. In addition, there may be an opportunity for recall responses to contribute to protection. A major problem with current blood-stage vaccines (Fig. 1 and Table 1) to date is that most target merozoite surface antigens, which are typically polymorphic and are exposed to antibody for only a few seconds as they move from one RBC to the next110,111. Accordingly, although a blood-stage vaccine targeting the merozoite surface antigen AMA1 was found to be able to elicit titers in excess of 100 μg/ml, it induced only around 20% protection over the study period of 8 months. However, there was an estimated 64% protection against parasites with homologous AMA1 sequences, though the sample size was small109.
Sustaining high titers of antibodies: generating affinity-matured long-lived plasma cells
On the basis of existing preclinical and clinical data, subunit vaccines against preerythrocytic and blood stages of infection will require sustained high antibody titers to protect. Long-term antibody responses are maintained by populations of long-lived plasma cells (LLPCs), a pool of nondividing cells in the bone marrow that continuously produce high-affinity antibodies112,113. As such, successful vaccination will require the development of vaccine strategies that increase the formation of these rare LLPCs to sustain antibodies at the required infection point. LLPCs emerge from germinal center (GC) responses, as do memory B cells that have been activated by follicular helper T cells, thereby facilitating somatic hypermutation and affinity maturation114. However, not all B cells enter GCs after encountering antigen, and some can develop into short-lived plasmablasts, which secrete generally low-affinity antibody as an initial response against invading pathogens114. Notably, short-lived plasmablasts do not survive for more than a few days, and so antibody levels from this type of response decay rapidly114. Inducing such short-lived plasmablast responses by vaccination or infection can therefore limit durable antibody immunity. Thus, vaccines for malaria must improve the generation of LLPCs and memory B cells.
The induction and maintenance of antibodies are controlled by the immunogen formulation, vaccine regimen and immune adjuvants. RTS,S is given with the AS01B adjuvant, containing monophosphoryl lipid A and the saponin QS-21 administered in liposomes25. Although antibody titers after RTS,S and AS01B vaccination are initially high, they diminish over time, thereby limiting the long-term protective efficacy. The half-life of the antibody response to CSP after RTS,S vaccination in human volunteers is approximately 600 days, even after the inflection point (Fig. 3b), a decay much faster than that seen in response to other subunit vaccines such as tetanus vaccine (half-life of 14 years) and diphtheria vaccine (half-life of 27 years). One explanation for the decreasing memory responses to RTS,S and AS01B may relate to the repeat region of CSP not being optimal for engaging B cells and thereby favoring the formation of short-lived plasmablasts. Repeating antigens such as bacterial polysaccharides often induce T cell–independent responses associated with poor B cell memory115. Several recent studies have used isothermal titration calorimetry to show that the CSP repeat can be bound by six to eight antibodies, thus raising the possibility that it might cross-link multiple B cell receptors (BCRs) in a manner akin to polysaccharide antigens102,116,117 (Fig. 4a). In CD28-deficient mice, which are unable to provide CD4 T cell help, there is indeed a T cell–independent component to the CSP-specific B cell response. However, T cell–dependent affinity maturation in GCs does occur in the immune response to this antigen23,116. Interestingly, the process of affinity maturation favors not only mutations that increase binding to CSP but also mutations that enhance Fab–Fab interactions stabilizing the multivalent complex of multiple antibodies bound to a single CSP molecule118. Mutations that increase Fab–Fab interactions also enhance BCR signaling, thus providing functional evidence of cross-linking of multiple BCRs on the B cell surface by CSP118 (Fig. 4b). In contrast, there is also evidence that the GC reaction after sporozoite immunization may be inefficient. Direct sequencing of CSP-specific B cells after Cvac immunization has revealed low numbers of mutations, which in many instances do not increase affinity119. On the basis of these data together with support from mathematical modeling, the low levels of affinity maturation have been proposed to be due to the complexity of the repeat antigen; consequently, many mutations are required for affinity maturation to occur, and the GC reaction accordingly becomes dominated by clones with high-affinity germline (unmutated) BCRs119. An alternative explanation for the low levels of affinity maturation observed is that high-avidity cross-linking of specific BCRs by the CSP repeat may compensate for low-affinity interactions, and B cells consequently receive a signal to exit the GC prematurely (Fig. 4b). Overall, the structure of CSP itself is likely to favor the formation of low-affinity short-lived plasmablasts over a durable high-affinity LLPC response.
a, Structures derived by X-ray crystallography, cryo-EM and modeling approaches of repeat- and junction-binding antibodies (data from refs 102,103,116,117,118). For repeat-binding structures, Fab–peptide structures and structures and models of the whole complex are shown. For junction antibodies, Fab–peptide structures are shown. Ab, antibody; mAb, monoclonal antibody. Images reprinted with permission from ref. 118, AAAS; ref. 117, under Creative Commons license CC BY 4.0; ref. 116, under Creative Commons license CC BY 4.0; ref. 102, Springer Nature America, Inc.; and ref. 103, Springer Nature America, Inc. b, Cross-linking of multiple BCRs by the NANP repeats may lead to B cell responses dominated by short-lived plasmablasts or inefficient GC reactions. c, A possible mechanism of enhanced protection by junction-binding antibodies. (i) A cleavage event at region 1 in CSP allows for the exposure of the thrombospondin repeats in the C-terminal domain to increase the adhesiveness of the CSP molecule. (ii) Anti-junction antibodies may prevent this cleavage from occurring by blocking adhesion in the liver and subsequent invasion of hepatocytes.
Beyond the specific features of the GC reaction to the repeat region of CSP, there is evidence that B cell responses are generally impaired in malaria infection, a finding with implications for vaccine delivery. One consistent finding across several human clinical studies and vaccine platforms is the lower immunogenicity of vaccines in previously exposed individuals and young children and infants than in malaria-naive adults in the United States or Europe41,44,55,56,57,120,121. Several potential mechanisms may explain these observations. First, malaria exposure leads to the induction of circulating antibodies that may limit vaccine responses by binding to antigens contained in the vaccine. For example, the presence of maternal anti-CSP in infants (6–11 weeks of age) might explain their lower antibody responses to RTS,S compared with those in older children105,121. Second, blood-stage infection is immunosuppressive, by inducing potent IFN-γ and tumor necrosis factor responses that in mouse models can suppress the formation of GCs23,122. Third, follicular helper T cells in humans appear to be skewed toward a CXCR3+ type I helper T cell phenotype during malaria infection, which is associated with poor antibody formation123. Evidence that these processes may result in defective B cell memory comes from the observation that malaria-exposed individuals have large numbers of atypical memory B cells that are considered dysfunctional124,125. These problems might not be insurmountable; for example, antibodies to CSP isolated from individuals in endemic areas immunized with the PfSPZ Vaccine show higher concentrations of affinity maturation than cells isolated from similarly vaccinated malaria-naive individuals102,103. These data suggest that the vaccine antibody responses in previously exposed individuals develop from responsive memory cells102,103.
Increasing antibody breadth and potency
Given the challenges in increasing the magnitude and durability of malaria-specific B cell responses to CSP, another approach to improving vaccine efficacy is decreasing the protective threshold by increasing the potency and breadth of antibody responses. This goal can be achieved by altering the vaccine regimen, enhancing the effector function of antibodies or improving immunogen design. As an example of how the vaccine regimen can alter the quality of protective antibody responses, administration of RTS,S and AS01B at 0, 4 and 28 weeks, as compared with the standard regimen of 0, 4 and 8 weeks, has been found to significantly improve short-term protection120. Importantly, the final vaccination at 28 weeks contained 20% of the vaccine and adjuvant dose. This so-called ‘split dose’ regimen, compared with the traditional regimen, induces antibodies with increased somatic hypermutation120. Whether the differences in responses seen with this regimen are due to the increased interval before the third immunization or the split dose remains unclear. However, whereas 26 of 30 subjects who underwent CHMI 3 weeks after the last split-dose immunization were protected, only 3 of 7 were protected after being rechallenged 8 months later without receiving an additional booster dose. Thus, ongoing field trials will determine whether this split-dose regimen confers improved durable protection by the RTS.S vaccine versus the conventional regimen.
Antibody responses might also be improved by generating highly functional antibodies that can fix complement or mediate cytolytic functions through Fc-mediated binding of other cell types. Notably, the presence of complement-fixing antibodies that bind both sporozoites and merozoites has been associated with naturally acquired immunity126,127. Memory IgM antibodies, which are multivalent and capable of fixing complement, have also been proposed as potent first responders to blood stages128. Finally, IgM antibodies to CSP are produced after PfSPZ vaccination and can limit hepatocyte invasion in vitro129.
Structure-based vaccine design
A major paradigm that has transformed vaccine development for many viral infections is ‘structure-based vaccine design’, in which newly discovered neutralizing monoclonal antibodies from vaccinated or infected humans are isolated and used to define new sites of vulnerability on the protein on the basis of defined structural analysis. This paradigm has led to improved vaccine design for respiratory syncytial virus and is being actively used for next-generation HIV and universal influenza vaccines130. With regard to malaria, whereas protective monoclonal antibodies against NANP-repeat regions of CSP were isolated almost 30 years ago and provided the basis for the RTS,S vaccine101, relatively few non-NANP-repeat human antibodies to CSP have shown potent in vivo function104. The recent isolation of human monoclonal antibodies from memory B cells and plasmablasts from subjects receiving the PfSPZ Vaccine or Cvac, or from malaria-infected individuals, has defined additional neutralizing sites on CSP and improved the resolution of binding to NANP-repeat regions102,103,117,131,132. Two studies have independently revealed that highly potent antibodies enhance binding at the junction of the N-terminal domain and repeat region of CSP102,103 (Fig. 4a). These results have defined a new site of neutralization on CSP referred to as the junctional epitope. Mouse antibodies that bind just upstream of this region have also been shown to have potent inhibitory activity, because they block a cysteine-protease-mediated cleavage event at a conserved site called region 1 in the CSP molecule104,133 (Fig. 4c). In striking contrast, antibodies specific to the C terminus may not be protective134,135,136. Importantly, the N-terminal domain and some of the repeat domain, such as the junctional regions, are not present in the current RTS,S vaccine. On the basis of these new findings, next-generation protein-based vaccines targeting the preerythrocytic stage will include the junctional epitopes and potentially other regions of the N terminus to enhance the breadth and potency of the antibody response to CSP.
A similar issue of antibody breadth and potency affects protective immune responses to blood-stage infection. Immunization with Ama-1 in complex with its binding partner Ron2 induces Ama-1-targeting antibodies that are more potent than those elicited by immunization with Ama-1 alone137, and immunization with Ama-1–Ron2 complexes confers superior protection in Aotus monkeys challenged with homologous parasites138. In the search for a less variable blood-stage antigen, attention has also been focused on the PfRh5–PfRipr–CyRPA complex, which binds Basigin on the RBC surface during invasion139,140. PfRh5 is highly conserved and is required for parasite viability, thus making it a major vaccine candidate140. The level of anti-Rh5 in the sera of vaccinated volunteers required to achieve infection blocking in an in vitro growth-inhibition assay is approximately five- to tenfold less than that for Ama1-targeting antibodies141. Moreover, monoclonal antibodies against PfRh5 appear capable of blocking growth (half-maximal effective concentration) at relatively low concentrations of ~10–15 μg/ml (ref. 142). Finally, the solution of the structures of PfRh5 and its partner CyRPA in complex with blocking antibodies raises the possibility of structure-guided vaccine design for this antigen143,144,145. Structural analysis has revealed that although some antibodies to PfRh5 can bind the Basigin-binding site, the most potent antibodies to PfRh5 and CyRPA bind away from this site and might mediate their effects by disrupting the overall complex143,145.
Passive transfer of neutralizing antibodies: a new solution for malaria prevention and elimination
Given the current and potential future challenges to developing highly effective and durable malaria vaccines (Box 1), an alternative solution for short-term protection up to 6 months is passive immunization with monoclonal antibodies102,103,117,146. The passive transfer of monoclonal antibodies bypasses the immunoregulatory effects of malaria infection and other obstacles to vaccination by directly providing the desired immune response. A similar passive prevention strategy is now being tested for the prevention of HIV, by using highly potent broadly neutralizing antibodies147,148. As a proof of principle for malaria prevention, the critical first step will be to demonstrate whether a single antibody directed against the NANP or the junctional region of CSP can protect humans after passive transfer and CHMI. This study would define the pharmacokinetics and protective threshold for the antibody. A critical question will be whether a single antibody is sufficient to mediate protection or whether additional antibodies to different sites on CSP, or antibodies to other antigens, may also be required. This approach could potentially be used for travelers, military personnel or health workers, for whom protection would be needed for up to 6 months. Antibodies could also be used to prevent seasonal infection in specific geographic areas.
The most important application of passive prevention is in the context of malaria elimination. For this application, drug treatment would be given to completely eliminate the malaria reservoir in the host, and antibodies would be administered at the same time to maintain high-level protection for at least 6 months. This approach would be efficient, because both steps can be done simultaneously and would not require the series of immunizations likely to be needed with any of the current vaccine candidates. At present, the level or duration of protection that would be required for successful elimination is unclear and would need to be determined by modeling and field studies. Finally, for longer-term protection over many years, for example, repeated immunizations could be given, or antibodies could be delivered by mRNA or adeno-associated virus, which has been shown to be protective in mice149.
Challenges and future directions
Although the development of RTS,S, whole-sporozoite and viral-based vaccines has provided important scientific and clinical insights, none of these approaches mediate durable immunity that can facilitate eradication. Nonetheless, regarding the challenges of developing immunity to a complex pathogen with multiple modes of immune evasion, important progress has been made. Most encouragingly, the successes and failures have provided a scientific roadmap for future vaccine design. Notably, improved vaccine efficacy may be achieved by inducing higher frequencies of CD8+ TRM cells through intravenous administration. Achieving greater antigenic breadth will require either multiple strains of sporozoites, developing late-acting GAP sporozoite vaccines and defining conserved T cell epitopes for viral-based vaccines. Second-generation preerythrocytic subunit vaccines targeted toward preventing parasites from reaching the liver will require greater potency and breadth of antibody responses beyond RTS,S. In addition, a multistage vaccine approach targeting the preerythrocytic and blood stages of the infection may prove additive or synergistic in mediating protection. Continued progress will depend on integrating the data from translational efforts in humans with basic-science efforts to define mechanisms in experimental mouse models that can ideally lead to the prevention and elimination of malaria.
References
Yamauchi, L. M., Coppi, A., Snounou, G. & Sinnis, P. Plasmodium sporozoites trickle out of the injection site. Cell. Microbiol. 9, 1215–1222 (2007).
Langhorne, J., Ndungu, F. M., Sponaas, A. M. & Marsh, K. Immunity to malaria: more questions than answers. Nat. Immunol. 9, 725–732 (2008).
Tran, T. M. et al. An intensive longitudinal cohort study of Malian children and adults reveals no evidence of acquired immunity to Plasmodium falciparum infection. Clin. Infect. Dis. 57, 40–47 (2013).
Owusu-Agyei, S. et al. Incidence of symptomatic and asymptomatic Plasmodium falciparum infection following curative therapy in adult residents of northern Ghana. Am. J. Trop. Med. Hyg. 65, 197–203 (2001).
Sagara, I. et al. A high malaria reinfection rate in children and young adults living under a low entomological inoculation rate in a periurban area of Bamako, Mali. Am. J. Trop. Med. Hyg. 66, 310–313 (2002).
Sokhna, C. S., Faye, F. B. K., Dieng, H. & Trape, J. F. Rapid reappearance of Plasmodium falciparum after drug treatment among Senegalese adults exposed to moderate seasonal transmission. Am. J. Trop. Med. Hyg. 65, 167–170 (2001).
Bull, P. C. et al. Parasite antigens on the infected red cell surface are targets for naturally acquired immunity to malaria. Nat. Med. 4, 358–360 (1998).
Chan, J. A. et al. Targets of antibodies against Plasmodium falciparum-infected erythrocytes in malaria immunity. J. Clin. Invest. 122, 3227–3238 (2012).
Fowkes, F. J., Richards, J. S., Simpson, J. A. & Beeson, J. G. The relationship between anti-merozoite antibodies and incidence of Plasmodium falciparum malaria: a systematic review and meta-analysis. PLoS Med. 7, e1000218 (2010).
Pinzon-Charry, A. et al. Low doses of killed parasite in CpG elicit vigorous CD4+ T cell responses against blood-stage malaria in mice. J. Clin. Invest. 120, 2967–2978 (2010).
Süss, G., Eichmann, K., Kury, E., Linke, A. & Langhorne, J. Roles of CD4- and CD8-bearing T lymphocytes in the immune response to the erythrocytic stages of Plasmodium chabaudi. Infect. Immun. 56, 3081–3088 (1988).
Horne-Debets, J. M. et al. PD-1 dependent exhaustion of CD8+ T cells drives chronic malaria. Cell Rep. 5, 1204–1213 (2013).
Imai, T. et al. Involvement of CD8+ T cells in protective immunity against murine blood-stage infection with Plasmodium yoelii 17XL strain. Eur. J. Immunol. 40, 1053–1061 (2010).
Richards, W. H. Active immunization of chicks against Plasmodium gallinaceum by inactivated homologous sporozoites and erythrocytic parasites. Nature 212, 1492–1494 (1966).
Mulligan, H. W., Russell, P. F. & Mohan, B. N. Active immunization of fowls against Plasmodium gallinacemn by injections of killed homologous sporozoites. J. Malar. Inst. India 4, 25–34 (1941).
Nussenzweig, R. S., Vanderberg, J., Most, H. & Orton, C. Protective immunity produced by the injection of X-irradiated sporozoites of plasmodium berghei. Nature 216, 160–162 (1967).
Clyde, D. F. Immunization of man against falciparum and vivax malaria by use of attenuated sporozoites. Am. J. Trop. Med. Hyg. 24, 397–401 (1975).
Luke, T. C. & Hoffman, S. L. Rationale and plans for developing a non-replicating, metabolically active, radiation-attenuated Plasmodium falciparum sporozoite vaccine. J. Exp. Biol. 206, 3803–3808 (2003).
Rodrigues, M., Nussenzweig, R. S. & Zavala, F. The relative contribution of antibodies, CD4+ and CD8+ T cells to sporozoite-induced protection against malaria. Immunology 80, 1–5 (1993).
Schofield, L. et al. Gamma interferon, CD8+ T cells and antibodies required for immunity to malaria sporozoites. Nature 330, 664–666 (1987).
Weiss, W. R., Sedegah, M., Beaudoin, R. L., Miller, L. H. & Good, M. F . CD8+ T cells(cytotoxic/suppressors) are required for protection in mice immunized with malaria sporozoites. Proc. Natl. Acad. Sci. USA 85, 573–576 (1988).
Hafalla, J. C., Sano, G., Carvalho, L. H., Morrot, A. & Zavala, F. Short-term antigen presentation and single clonal burst limit the magnitude of the CD8+ T cell responses to malaria liver stages. Proc. Natl. Acad. Sci. USA 99, 11819–11824 (2002).
Keitany, G. J. et al. Blood stage malaria disrupts humoral immunity to the pre-erythrocytic stage circumsporozoite protein. Cell Rep. 17, 3193–3205 (2016).
Ocaña-Morgner, C., Mota, M. M. & Rodriguez, A. Malaria blood stage suppression of liver stage immunity by dendritic cells. J. Exp. Med. 197, 143–151 (2003).
Casares, S., Brumeanu, T. D. & Richie, T. L. The RTS,S malaria vaccine. Vaccine 28, 4880–4894 (2010).
Belnoue, E. et al. Vaccination with live Plasmodium yoelii blood stage parasites under chloroquine cover induces cross-stage immunity against malaria liver stage. J. Immunol. 181, 8552–8558 (2008).
Mordmüller, B. et al. Sterile protection against human malaria by chemoattenuated PfSPZ vaccine. Nature 542, 445–449 (2017).
Roestenberg, M. et al. Protection against a malaria challenge by sporozoite inoculation. N. Engl. J. Med. 361, 468–477 (2009).
Wu, Y., Sinden, R. E., Churcher, T. S., Tsuboi, T. & Yusibov, V. Development of malaria transmission-blocking vaccines: from concept to product. Adv. Parasitol. 89, 109–152 (2015).
Weiss, W. R. & Jiang, C. G. Protective CD8+ T lymphocytes in primates immunized with malaria sporozoites. PLoS One 7, e31247 (2012).
Cockburn, I. A. et al. In vivo imaging of CD8+ T cell-mediated elimination of malaria liver stages. Proc. Natl. Acad. Sci. USA 110, 9090–9095 (2013).
Kimura, K. et al. CD8+ T cells specific for a malaria cytoplasmic antigen form clusters around infected hepatocytes and are protective at the liver stage of infection. Infect. Immun. 81, 3825–3834 (2013).
Rodrigues, M., Nussenzweig, R. S., Romero, P. & Zavala, F. The in vivo cytotoxic activity of CD8+ T cell clones correlates with their levels of expression of adhesion molecules. J. Exp. Med. 175, 895–905 (1992).
Butler, N. S., Schmidt, N. W. & Harty, J. T. Differential effector pathways regulate memory CD8 T cell immunity against Plasmodium berghei versus P. yoelii sporozoites. J. Immunol. 184, 2528–2538 (2010).
Chakravarty, S., Baldeviano, G. C., Overstreet, M. G. & Zavala, F. Effector CD8+ T lymphocytes against liver stages of Plasmodium yoelii do not require gamma interferon for antiparasite activity. Infect. Immun. 76, 3628–3631 (2008).
Oliveira, G. A. et al. Class II-restricted protective immunity induced by malaria sporozoites. Infect. Immun. 76, 1200–1206 (2008).
Carvalho, L. H. et al. IL-4-secreting CD4+ T cells are crucial to the development of CD8+ T-cell responses against malaria liver stages. Nat. Med. 8, 166–170 (2002).
Tsuji, M. et al. Gamma delta T cells contribute to immunity against the liver stages of malaria in alpha beta T-cell-deficient mice. Proc. Natl. Acad. Sci. USA 91, 345–349 (1994).
Rénia, L. et al. Effector functions of circumsporozoite peptide-primed CD4+ T cell clones against Plasmodium yoelii liver stages. J. Immunol. 150, 1471–1478 (1993).
Ishizuka, A. S. et al. Protection against malaria at 1 year and immune correlates following PfSPZ vaccination. Nat. Med. 22, 614–623 (2016).
Seder, R. A. et al. Protection against malaria by intravenous immunization with a nonreplicating sporozoite vaccine. Science 341, 1359–1365 (2013).
Lyke, K. E. et al. Attenuated PfSPZ Vaccine induces strain-transcending T cells and durable protection against heterologous controlled human malaria infection. Proc. Natl. Acad. Sci. USA 114, 2711–2716 (2017).
Epstein, J. E. et al. Protection against Plasmodium falciparum malaria by PfSPZ Vaccine. JCI Insight 2, e89154 (2017).
Sissoko, M. S. et al. Safety and efficacy of PfSPZ Vaccine against Plasmodium falciparum via direct venous inoculation in healthy malaria-exposed adults in Mali: a randomised, double-blind phase 1 trial. Lancet Infect. Dis. 17, 498–509 (2017).
Chakravarty, S. et al. CD8+ T lymphocytes protective against malaria liver stages are primed in skin-draining lymph nodes. Nat. Med. 13, 1035–1041 (2007).
Lau, L. S. et al. CD8+ T cells from a novel T cell receptor transgenic mouse induce liver-stage immunity that can be boosted by blood-stage infection in rodent malaria. PLoS Pathog. 10, e1004135 (2014).
Bijker, E. M. et al. Cytotoxic markers associate with protection against malaria in human volunteers immunized with Plasmodium falciparum sporozoites. J. Infect. Dis. 210, 1605–1615 (2014).
Zaidi, I. et al. γδ T cells are required for the induction of sterile immunity during irradiated sporozoite vaccinations. J. Immunol. 199, 3781–3788 (2017).
Sandstrom, A. et al. The intracellular B30.2 domain of butyrophilin 3A1 binds phosphoantigens to mediate activation of human Vγ9Vδ2 T cells. Immunity 40, 490–500 (2014).
De Rosa, S. C. et al. Ontogeny of gamma delta T cells in humans. J. Immunol. 172, 1637–1645 (2004).
Jagannathan, P. et al. Loss and dysfunction of Vδ2+ γδ T cells are associated with clinical tolerance to malaria. Sci. Transl. Med. 6, 251ra117 (2014).
Kazmin, D. et al. Systems analysis of protective immune responses to RTS,S malaria vaccination in humans. Proc. Natl. Acad. Sci. USA 114, 2425–2430 (2017).
Li, S. et al. Priming with recombinant influenza virus followed by administration of recombinant vaccinia virus induces CD8+ T-cell-mediated protective immunity against malaria. Proc. Natl. Acad. Sci. USA 90, 5214–5218 (1993).
Chuang, I. et al. DNA prime/Adenovirus boost malaria vaccine encoding P. falciparum CSP and AMA1 induces sterile protection associated with cell-mediated immunity. PLoS One 8, e55571 (2013).
Ewer, K. J. et al. Protective CD8+ T-cell immunity to human malaria induced by chimpanzee adenovirus-MVA immunisation. Nat. Commun. 4, 2836 (2013).
Mensah, V. A. et al. Safety and immunogenicity of malaria vectored vaccines given with routine expanded program on immunization vaccines in Gambian infants and neonates: a randomized controlled trial. Front. Immunol. 8, 1551 (2017).
Ogwang, C. et al. Prime-boost vaccination with chimpanzee adenovirus and modified vaccinia Ankara encoding TRAP provides partial protection against Plasmodium falciparum infection in Kenyan adults. Sci. Transl. Med. 7, 286re5 (2015).
Cockburn, I. A., Tse, S. W. & Zavala, F. CD8+ T cells eliminate liver-stage Plasmodium berghei parasites without detectable bystander effect. Infect. Immun. 82, 1460–1464 (2014).
Fernandez-Ruiz, D. et al. Liver-resident memory CD8+ T cells form a front-line defense against malaria liver-stage infection. Immunity 45, 889–902 (2016).
Schmidt, N. W. et al. Memory CD8 T cell responses exceeding a large but definable threshold provide long-term immunity to malaria. Proc. Natl. Acad. Sci. USA 105, 14017–14022 (2008).
Gillespie, G. M. et al. Functional heterogeneity and high frequencies of cytomegalovirus-specific CD8+ T lymphocytes in healthy seropositive donors. J. Virol. 74, 8140–8150 (2000).
Hansen, S. G. et al. Profound early control of highly pathogenic SIV by an effector memory T-cell vaccine. Nature 473, 523–527 (2011).
Hansen, S. G. et al. Prevention of tuberculosis in rhesus macaques by a cytomegalovirus-based vaccine. Nat. Med. 24, 130–143 (2018).
Gebhardt, T., Palendira, U., Tscharke, D. C. & Bedoui, S. Tissue-resident memory T cells in tissue homeostasis, persistent infection, and cancer surveillance. Immunol. Rev. 283, 54–76 (2018).
Tse, S. W., Radtke, A. J., Espinosa, D. A., Cockburn, I. A. & Zavala, F. The chemokine receptor CXCR6 is required for the maintenance of liver memory CD8+ T cells specific for infectious pathogens. J. Infect. Dis. 210, 1508–1516 (2014).
McNamara, H. A. et al. Up-regulation of LFA-1 allows liver-resident memory T cells to patrol and remain in the hepatic sinusoids. Sci. Immunol. 2, eaa1996 (2017).
Epstein, J. E. et al. Live attenuated malaria vaccine designed to protect through hepatic CD8+ T cell immunity. Science 334, 475–480 (2011).
Mackay, L. K. et al. Long-lived epithelial immunity by tissue-resident memory T (TRM) cells in the absenceof persisting local antigen presentation. Proc. Proc. Natl. Acad. Sci. USA 109, 7037–7042 (2012).
Slutter, B. et al. Dynamics of influenza-induced lung-resident memory T cells underlie waning heterosubtypic immunity. Sci. Immunol. 2, eaag2031 (2017).
Wu, T. et al. Lung-resident memory CD8 T cells (TRM) are indispensable for optimal cross-protection against pulmonary virus infection. J. Leukoc. Biol. 95, 215–224 (2014).
Tarun, A. S. et al. A combined transcriptome and proteome survey of malaria parasite liver stages. Proc. Natl. Acad. Sci. USA 105, 305–310 (2008).
Roestenberg, M. et al. Long-term protection against malaria after experimental sporozoite inoculation: an open-label follow-up study. Lancet 377, 1770–1776 (2011).
Schats, R. et al. Heterologous protection against malaria after immunization with Plasmodium falciparum sporozoites. PLoS One 10, e0124243 (2015).
Walk, J. et al. Modest heterologous protection after Plasmodium falciparum sporozoite immunization: a double-blind randomized controlled clinical trial. BMC Med. 15, 168 (2017).
Butler, N. S. et al. Superior antimalarial immunity after vaccination with late liver stage-arresting genetically attenuated parasites. Cell Host Microbe 9, 451–462 (2011).
Nahrendorf, W. et al. Blood-stage immunity to Plasmodium chabaudi malaria following chemoprophylaxis and sporozoite immunization. eLife 4, e05165 (2015).
Bijker, E. M. et al. Protection against malaria after immunization by chloroquine prophylaxis and sporozoites is mediated by preerythrocytic immunity. Proc. Natl. Acad. Sci. USA 110, 7862–7867 (2013).
Peters, J. et al. High diversity and rapid changeover of expressed var genes during the acute phase of Plasmodium falciparum infections in human volunteers. Proc. Natl. Acad. Sci. USA 99, 10689–10694 (2002).
Vaughan, A. M. et al. Type II fatty acid synthesis is essential only for malaria parasite late liver stage development. Cell. Microbiol. 11, 506–520 (2009).
Spring, M. et al. First-in-human evaluation of genetically attenuated Plasmodium falciparum sporozoites administered by bite of Anopheles mosquitoes to adult volunteers. Vaccine 31, 4975–4983 (2013).
Kublin, J. G. et al. Complete attenuation of genetically engineered Plasmodium falciparum sporozoites in human subjects. Sci. Transl. Med. 9, eaad9099 (2017).
Doll, K. L., Pewe, L. L., Kurup, S. P. & Harty, J. T. Discriminating protective from nonprotective Plasmodium-specific CD8+ T cell responses. J. Immunol. 196, 4253–4262 (2016).
Cockburn, I. A. et al. Dendritic cells and hepatocytes use distinct pathways to process protective antigen from plasmodium in vivo. PLoS Pathog. 7, e1001318 (2011).
Romero, P. et al. Cloned cytotoxic T cells recognize an epitope in the circumsporozoite protein and protect against malaria. Nature 341, 323–326 (1989).
Hafalla, J. C. et al. Identification of targets of CD8+ T cell responses to malaria liver stages by genome-wide epitope profiling. PLoS Pathog. 9, e1003303 (2013).
Kumar, K. A. et al. The circumsporozoite protein is an immunodominant protective antigen in irradiated sporozoites. Nature 444, 937–940 (2006).
Grüner, A. C. et al. Sterile protection against malaria is independent of immune responses to the circumsporozoite protein. PLoS One 2, e1371 (2007).
Doolan, D. L. et al. Identification of Plasmodium falciparum antigens by antigenic analysis of genomic and proteomic data. Proc. Natl. Acad. Sci. USA 100, 9952–9957 (2003).
Draper, S. J. et al. Recent advances in recombinant protein-based malaria vaccines. Vaccine 33, 7433–7443 (2015).
Schussek, S. et al. Novel Plasmodium antigens identified via genome-based antibody screen induce protection associated with polyfunctional T cell responses. Sci. Rep. 7, 15053 (2017).
Speake, C. et al. Identification of novel pre-erythrocytic malaria antigen candidates for combination vaccines with circumsporozoite protein. PLoS One 11, e0159449 (2016).
Longley, R. J. et al. Comparative assessment of vaccine vectors encoding ten malaria antigens identifies two protective liver-stage candidates. Sci. Rep. 5, 11820 (2015).
Shao, W. et al. The SysteMHC Atlas project. Nucleic Acids Res. 46, D1237–D1247 (2018).
Plotkin, S. A. Vaccines: correlates of vaccine-induced immunity. Clin. Infect. Dis. 47, 401–409 (2008).
Amanna, I. J., Carlson, N. E. & Slifka, M. K. Duration of humoral immunity to common viral and vaccine antigens. N. Engl. J. Med. 357, 1903–1915 (2007).
Plotkin, S. A. Correlates of protection induced by vaccination. Clin. Vaccine Immunol. 17, 1055–1065 (2010).
Nussenzweig, R. S., Vanderberg, J. P., Sanabria, Y. & Most, H. Plasmodium berghei: accelerated clearance of sporozoites from blood as part of immune-mechanism in mice. Exp. Parasitol. 31, 88–97 (1972).
Behet, M. C. et al. Sporozoite immunization of human volunteers under chemoprophylaxis induces functional antibodies against pre-erythrocytic stages of Plasmodium falciparum. Malar. J. 13, 136 (2014).
Peng, K. et al. Breadth of humoral response and antigenic targets of sporozoite-inhibitory antibodies associated with sterile protection induced by controlled human malaria infection. Cell. Microbiol. 18, 1739–1750 (2016).
Sack, B. K. et al. Humoral protection against mosquito bite-transmitted Plasmodium falciparum infection in humanized mice. NPJ Vaccines 2, 27 (2017).
Zavala, F. et al. Rationale for development of a synthetic vaccine against Plasmodium falciparum malaria. Science 228, 1436–1440 (1985).
Kisalu, N. K. et al. A human monoclonal antibody prevents malaria infection by targeting a new site of vulnerability on the parasite. Nat. Med. 24, 408–416 (2018).
Tan, J. et al. A public antibody lineage that potently inhibits malaria infection through dual binding to the circumsporozoite protein. Nat. Med. 24, 401–407 (2018).
Espinosa, D. A. et al. Proteolytic cleavage of the Plasmodium falciparum circumsporozoite protein is a target of protective antibodies. J. Infect. Dis. 212, 1111–1119 (2015).
RTS,S Clinical Trials Partnership. Efficacy and safety of RTS,S/AS01 malaria vaccine with or without a booster dose in infants and children in Africa: final results of a phase 3, individually randomised, controlled trial. Lancet 386, 31–45 (2015).
White, M. T. et al. Immunogenicity of the RTS,S/AS01 malaria vaccine and implications for duration of vaccine efficacy: secondary analysis of data from a phase 3 randomised controlled trial. Lancet Infect. Dis. 15, 1450–1458 (2015).
Dups, J. N., Pepper, M. & Cockburn, I. A. Antibody and B cell responses to Plasmodium sporozoites. Front. Microbiol. 5, 625 (2014).
Douglas, A. D. et al. A PfRH5-based vaccine is efficacious against heterologous strain blood-stage Plasmodium falciparum infection in aotus monkeys. Cell Host Microbe 17, 130–139 (2015).
Thera, M. A. et al. A field trial to assess a blood-stage malaria vaccine. N. Engl. J. Med. 365, 1004–1013 (2011).
Dvorak, J. A., Miller, L. H., Whitehouse, W. C. & Shiroishi, T. Invasion of erythrocytes by malaria merozoites. Science 187, 748–750 (1975).
Gilson, P. R. & Crabb, B. S. Morphology and kinetics of the three distinct phases of red blood cell invasion by Plasmodium falciparum merozoites. Int. J. Parasitol. 39, 91–96 (2009).
Manz, R. A., Thiel, A. & Radbruch, A. Lifetime of plasma cells in the bone marrow. Nature 388, 133–134 (1997).
Slifka, M. K., Antia, R., Whitmire, J. K. & Ahmed, R. Humoral immunity due to long-lived plasma cells. Immunity 8, 363–372 (1998).
Nutt, S. L., Hodgkin, P. D., Tarlinton, D. M. & Corcoran, L. M. The generation of antibody-secreting plasma cells. Nat. Rev. Immunol. 15, 160–171 (2015).
Clutterbuck, E. A. et al. Pneumococcal conjugate and plain polysaccharide vaccines have divergent effects on antigen-specific B cells. J. Infect. Dis. 205, 1408–1416 (2012).
Fisher, C. R. et al. T-dependent B cell responses to Plasmodium induce antibodies that form a high-avidity multivalent complex with the circumsporozoite protein. PLoS Pathog. 13, e1006469 (2017).
Oyen, D. et al. Structural basis for antibody recognition of the NANP repeats in Plasmodium falciparum circumsporozoite protein. Proc. Natl. Acad. Sci. USA 114, E10438–E10445 (2017).
Imkeller, K. et al. Antihomotypic affinity maturation improves human B cell responses against a repetitive epitope. Science 360, 1358–1362 (2018).
Murugan, R. et al. Clonal selection drives protective memory B cell responses in controlled human malaria infection. Sci. Immunol. 3, eaap8029 (2018).
Regules, J. A. et al. Fractional third and fourth dose of RTS,S/AS01 malaria candidate vaccine: a phase 2a controlled human malaria parasite infection and immunogenicity study. J. Infect. Dis. 214, 762–771 (2016).
RTS,S Clinical Trials Partnership. Efficacy and safety of the RTS,S/AS01 malaria vaccine during 18 months after vaccination: a phase 3 randomized, controlled trial in children and young infants at 11 African sites. PLoS Med. 11, e1001685 (2014).
Ryg-Cornejo, V. et al. Severe malaria infections impair germinal center responses by inhibiting T follicular helper cell differentiation. Cell Rep. 14, 68–81 (2016).
Obeng-Adjei, N. et al. Circulating Th1-cell-type Tfh cells that exhibit impaired B cell help are preferentially activated during acute malaria in children. Cell Rep. 13, 425–439 (2015).
Portugal, S. et al. Malaria-associated atypical memory B cells exhibit markedly reduced B cell receptor signaling and effector function. eLife 4, 07218 (2015).
Weiss, G. E. et al. The Plasmodium falciparum-specific human memory B cell compartment expands gradually with repeated malaria infections. PLoS Pathog. 6, e1000912 (2010).
Kurtovic, L. et al. Human antibodies activate complement against Plasmodium falciparum sporozoites, and are associated with protection against malaria in children. BMC Med. 16, 61 (2018).
Boyle, M. J. et al. Human antibodies fix complement to inhibit Plasmodium falciparum invasion of erythrocytes and are associated with protection against malaria. Immunity 42, 580–590 (2015).
Krishnamurty, A. T. et al. Somatically hypermutated Plasmodium-specific IgM+ memory B cells are rapid, plastic, early responders upon malaria rechallenge. Immunity 45, 402–414 (2016).
Zenklusen, I. et al. Immunization of malaria-preexposed volunteers with PfSPZ Vaccine elicits long-lived IgM invasion-inhibitory and complement-fixing antibodies. J. Infect. Dis. 217, 1569–1578 (2018).
Kwong, P. D. What are the most powerful immunogen design vaccine strategies? A structural biologist’s perspective. Cold Spring Harb. Perspect. Biol. 9, a029470 (2017).
Foquet, L. et al. Vaccine-induced monoclonal antibodies targeting circumsporozoite protein prevent Plasmodium falciparum infection. J. Clin. Invest. 124, 140–144 (2014).
Triller, G. et al. Natural parasite exposure induces protective human anti-malarial antibodies. Immunity 47, 1197–1209.e1110 (2017).
Coppi, A. et al. The malaria circumsporozoite protein has two functional domains, each with distinct roles as sporozoites journey from mosquito to mammalian host. J. Exp. Med. 208, 341–356 (2011).
Scally, S. W. et al. Rare PfCSP C-terminal antibodies induced by live sporozoite vaccination are ineffective against malaria infection. J. Exp. Med. 215, 63–75 (2018).
Chaudhury, S. et al. The biological function of antibodies induced by the RTS,S/AS01 malaria vaccine candidate is determined by their fine specificity. Malar. J. 15, 301 (2016).
Chaudhury, S. et al. Delayed fractional dose regimen of the RTS,S/AS01 malaria vaccine candidate enhances an IgG4 response that inhibits serum opsonophagocytosis. Sci. Rep. 7, 7998 (2017).
Srinivasan, P. et al. Disrupting malaria parasite AMA1-RON2 interaction with a small molecule prevents erythrocyte invasion. Nat. Commun. 4, 2261 (2013).
Srinivasan, P. et al. A malaria vaccine protects Aotus monkeys against virulent Plasmodium falciparum infection. NPJ Vaccines 2, 14 (2017).
Crosnier, C. et al. Basigin is a receptor essential for erythrocyte invasion by Plasmodium falciparum. Nature 480, 534–537 (2011).
Volz, J. C. et al. Essential role of the PfRh5/PfRipr/CyRPA complex during Plasmodium falciparum invasion of erythrocytes. Cell Host Microbe 20, 60–71 (2016).
Payne, R. O. et al. Human vaccination against RH5 induces neutralizing antimalarial antibodies that inhibit RH5 invasion complex interactions. JCI Insight 2, 96381 (2017).
Douglas, A. D. et al. Neutralization of Plasmodium falciparum merozoites by antibodies against PfRH5. J. Immunol. 192, 245–258 (2014).
Chen, L. et al. Structural basis for inhibition of erythrocyte invasion by antibodies to Plasmodium falciparum protein CyRPA. eLife 6, e21347 (2017).
Favuzza, P. et al. Structure of the malaria vaccine candidate antigen CyRPA and its complex with a parasite invasion inhibitory antibody. eLife 6, 20383 (2017).
Wright, K. E. et al. Structure of malaria invasion protein RH5 with erythrocyte basigin and blocking antibodies. Nature 515, 427–430 (2014).
Foquet, L. et al. Plasmodium falciparum liver stage infection and transition to stable blood stage infection in liver-humanized and blood-humanized FRGN KO mice enables testing of blood stage inhibitory antibodies (reticulocyte-binding protein homolog 5) in vivo. Front. Immunol. 9, 524 (2018).
Caskey, M. et al. Viraemia suppressed in HIV-1-infected humans by broadly neutralizing antibody 3BNC117. Nature 522, 487–491 (2015).
Lynch, R. M. et al. Virologic effects of broadly neutralizing antibody VRC01 administration during chronic HIV-1 infection. Sci. Transl. Med. 7, 319ra206 (2015).
Deal, C. et al. Vectored antibody gene delivery protects against Plasmodium falciparum sporozoite challenge in mice. Proc. Natl. Acad. Sci. USA 111, 12528–12532 (2014).
Olotu, A. et al. Advancing global health through development and clinical trials partnerships: a randomized, placebo-controlled, double-blind assessment of safety, tolerability, and immunogenicity of PfSPZ vaccine for malaria in healthy Equatoguinean men. Am. J. Trop. Med. Hyg. 98, 308–318 (2018).
Bergmann-Leitner, E. S. et al. Immunization with pre-erythrocytic antigen CelTOS from Plasmodium falciparum elicits cross-species protection against heterologous challenge with Plasmodium berghei. PLoS One 5, e12294 (2010).
de Barra, E. et al. A phase Ia study to assess the safety and immunogenicity of new malaria vaccine candidates ChAd63 CS administered alone and with MVA CS. PLoS One 9, e115161 (2014).
Collins, K. A., Snaith, R., Cottingham, M. G., Gilbert, S. C. & Hill, A. V. S. Enhancing protective immunity to malaria with a highly immunogenic virus-like particle vaccine. Sci. Rep. 7, 46621 (2017).
Esen, M. et al. Safety and immunogenicity of GMZ2: a MSP3-GLURP fusion protein malaria vaccine candidate. Vaccine 27, 6862–6868 (2009).
Remarque, E. J., Faber, B. W., Kocken, C. H. & Thomas, A. W. A diversity-covering approach to immunization with Plasmodium falciparum apical membrane antigen 1 induces broader allelic recognition and growth inhibition responses in rabbits. Infect. Immun. 76, 2660–2670 (2008).
Olugbile, S. et al. Vaccine potentials of an intrinsically unstructured fragment derived from the blood stage-associated Plasmodium falciparum protein PFF0165c. Infect. Immun. 77, 5701–5709 (2009).
Lusingu, J. P. et al. Satisfactory safety and immunogenicity of MSP3 malaria vaccine candidate in Tanzanian children aged 12-24 months. Malar. J. 8, 163 (2009).
Palacpac, N. M. et al. Phase 1b randomized trial and follow-up study in Uganda of the blood-stage malaria vaccine candidate BK-SE36. PLoS One 8, e64073 (2013).
Nielsen, M. A. et al. The influence of sub-unit composition and expression system on the functional antibody response in the development of a VAR2CSA based Plasmodium falciparum placental malaria vaccine. PLoS One 10, e0135406 (2015).
Li, Y. et al. Enhancing immunogenicity and transmission-blocking activity of malaria vaccines by fusing Pfs25 to IMX313 multimerization technology. Sci. Rep. 6, 18848 (2016).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Cockburn, I.A., Seder, R.A. Malaria prevention: from immunological concepts to effective vaccines and protective antibodies. Nat Immunol 19, 1199–1211 (2018). https://doi.org/10.1038/s41590-018-0228-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41590-018-0228-6
This article is cited by
-
B cell memory: from generation to reactivation: a multipronged defense wall against pathogens
Cell Death Discovery (2024)
-
Establishing RTS,S/AS01 as a benchmark for comparison to next-generation malaria vaccines in a mouse model
npj Vaccines (2024)
-
A candidate antibody drug for prevention of malaria
Nature Medicine (2024)
-
Elicitation of T-cell-derived IFN-γ-dependent immunity by highly conserved Plasmodium ovale curtisi Duffy binding protein domain region II (PocDBP-RII)
Parasites & Vectors (2023)
-
In-silico analysis of potent Mosquirix vaccine adjuvant leads
Journal of Genetic Engineering and Biotechnology (2023)