Abstract
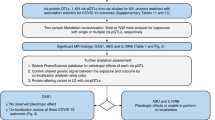
The OAS1/2/3 cluster has been identified as a risk locus for severe COVID-19 among individuals of European ancestry, with a protective haplotype of approximately 75 kilobases (kb) derived from Neanderthals in the chromosomal region 12q24.13. This haplotype contains a splice variant of OAS1, which occurs in people of African ancestry independently of gene flow from Neanderthals. Using trans-ancestry fine-mapping approaches in 20,779 hospitalized cases, we demonstrate that this splice variant is likely to be the SNP responsible for the association at this locus, thus strongly implicating OAS1 as an effector gene influencing COVID-19 severity.
Similar content being viewed by others
Main
The COVID-19 pandemic has impacted the world for over a year. During this period, several large international efforts1,2,3,4,5 have been launched to identify the genetic determinants of COVID-19 susceptibility and severity. These efforts have identified more than a dozen genomic regions associated with severe COVID-19. However, the causal variants in these regions are yet to be identified, hampering our ability to understand COVID-19 pathophysiology.
When risk haplotypes are long, it is more challenging to disentangle causal genetic variants due to linkage disequilibrium (LD). This is especially problematic for haplotypes derived from Neanderthals and Denisovans, which often span several tens of kb or more. Two notable COVID-19 examples are the major risk locus on chromosome 3 (3p21.31) and the OAS1/2/3 locus on chromosome 12 (12q24.13), both carrying haplotypes of Neanderthal origin6,7. The OAS genes encode enzymes catalyzing the synthesis of short polyadenylates, which activate ribonuclease L that in turn degrades intracellular double-stranded RNA and triggers several other antiviral mechanisms8. The protective Neanderthal-derived haplotype confers approximately 23% reduced risk of becoming critically ill on infection with SARS-CoV-2 (ref. 3). Supporting this, a recent Mendelian randomization study found that increased circulating levels of OAS1 were associated with reduced risk of very severe COVID-19, hospitalization for COVID-19 and susceptibility to this disease9. However, other evidence from a transcriptome-wide association study suggested a stronger association with OAS3 levels3. Thus, efforts are required to disentangle the causal gene, or genes, at this locus.
The OAS region was identified as a COVID-19 risk locus in association studies3,5 of mainly individuals of European ancestry. The protective haplotype derived from Neanderthals in individuals of European ancestry is approximately 75 kb and spans the three genes OAS1, OAS2 and OAS3 (ref. 7). A candidate causal variant in the region is rs10774671, which falls in a splice acceptor site at exon 7 of OAS1 and where the protective (G) allele results in a longer and approximately 60% more active OAS1 enzyme10. However, this variant is as associated with COVID-19 severity as many of the hundreds of variants in LD. For example, in individuals of European ancestry, we found 130 variants in strong LD (r2 > 0.8) with the splice acceptor variant (Fig. 1a). Thus, further methods are required to disentangle the causal SNP(s) at this locus, which could help identify the causal gene.
a, Plot of LD in individuals of European ancestry (n = 503) shows that 130 variants are in LD (r2 > 0.8) with the splice acceptor variant rs10774671 (marked in red). b, Same as in a but for individuals of African ancestry (n = 661). No variants were found to be in LD with the splice acceptor variant. Data are from the 1000 Genomes Project11. The x axis shows the hg19 coordinates.
One method to better identify causal SNPs at an associated locus is to test associations in different ancestry groups, particularly when these other populations have different LD structures and shorter haplotypes. Therefore, to examine whether we could identify a population with which we could test this variant independently, we investigated the presence of co-segregating variants in populations in the 1000 Genomes Project11. In individuals of South Asian ancestry, there are 129 such variants, and in individuals of East Asian ancestry, 128 such variants exist. In stark contrast, no variants co-segregate with rs10774671 in individuals of African ancestry at an LD of r2 > 0.6 (Fig. 1b). Thus, populations of African ancestry offer a possibility to independently test whether rs10774671 is associated with COVID-19 severity. We note that the use of a reference panel such as the 1000 Genomes Project does not provide a complete picture of the LD structure of this genomic region for different ancestries. Nevertheless, it is clear that the Neanderthal haplotype is virtually absent among individuals of primarily African ancestry.
To test the association of splice acceptor variant rs10774671 with COVID-19 outcomes in people of African ancestry, we combined six studies that had assessed COVID-19 severity (UK Biobank (UKB), Penn Medicine BioBank (PMBB), Columbia University Biobank (CUB), Biobanque Québécoise de la COVID-19 (BQC-19), GenOMICC and the VA Million Veteran Program (MVP)), comprising 2,787 cases and 130,997 controls of African ancestry. We found that the rs10774671 G allele conferred protection against COVID-19 hospitalization in individuals of African ancestry (Fig. 2a, P = 0.03) of similar magnitude (odds ratio (OR) = 0.94, 95% confidence interval (CI) = 0.88–0.99) as in individuals of European ancestry (OR = 0.92, 95% CI = 0.90–0.95), in whom the rs10774671 G allele is less common (32% allele frequency among individuals of European ancestry versus 58% among individuals of African ancestry). We found no evidence of heterogeneity across the 5 studies (Cochran’s Q = 3.22, P = 0.67; I2 = 0% (0.0–74.6%); τ2 = 0 (0–0.05), 95% CI in brackets; Methods), and there was no statistical difference (P = 0.72) between the 3 cohorts that used methods that specifically control for unbalanced case–control ratio (that is, regenie or the Scalable and Accurate Implementation of GEneralized mixed model (SAIGE)) and the 3 that did not (Methods). Moreover, a meta-analysis of overlapping individuals of African ancestry performed by the COVID-19 Host Genetics Initiative5 (HGI) yielded similar results (OR = 0.93, 95% CI = 0.87–0.99, P = 0.02; 2,113 cases and 121,925 controls). Thus, the rs10774671 G allele confers protection against COVID-19 severity independently of the variants with which it is associated in non-African populations.
a, ORs for COVID-19 hospitalization for carriers of the ancestral splice variant of African ancestry. The plots show the summary effect in individuals of African ancestry (n = 2,787 cases) by meta-analysis of 6 cohorts shown in this study and by the COVID-19 HGI (n = 2,133 cases). Data are presented as ORs ± 95% CIs. b, PIPs using the summary statistics and LD from individuals of European ancestry. c, Same as b but for individuals of African ancestry, using the European PIPs as prior probabilities. d, Same as c but using scaled CADD-scores as prior probabilities for the first (European) step in the fine-mapping analysis. The error bars in a show the 95% CIs. The x axes in b–d show the genomic coordinates in the hg19.
Although we found nominal statistical support (HGI one-tailed P = 9.0 × 10−3) for the hypothesis of an effect in the same direction for the splice variant among individuals of African ancestry, this association alone does not rule out other causal variants. To test the splice acceptor variant rs10774671 against other candidate variants, we performed stepwise fine-mapping using individuals of both European and African ancestry. Summary statistics and LD for individuals of European ancestry could not resolve the association signal at this locus (Fig. 2b, posterior inclusion probability (PIP) for rs10774671 = 0.31). Using the PIPs from this analysis as prior probabilities when analyzing African ancestry data identified rs10774671 as most likely to be causal (Fig. 2c, PIP = 0.71). Combining both ancestries with in silico prediction of deleteriousness (CADD-scores12, which exist for both synonymous and nonsynonymous variants) brings further support that rs10774671 is the causal variant (Fig. 2d, PIP = 0.90). We also find that one causal variant is more likely than two (P = 0.86 versus P = 0.14).
This observation is compatible with the fact that Neanderthal haplotypes are rare or absent in African populations13,14 and that ancestral alleles seen in Neanderthals, such as the G allele at rs10774671, exist today as a result of their inheritance from the ancestral population common to both modern humans and Neanderthals. In the latter case, such variants have existed in modern humans on the order of approximately half a million years and therefore co-segregate with different variants than when they are derived from gene flow from Neanderthals into modern humans that occurred about 60,000 years ago15. In this study, we leverage this fact to show that the ancestral splice variant, encoding a more active10 and prenylated form of OAS1 with capacity for membrane localization16, is responsible for the protective effect associated with this locus17. These findings provide evidence that the splice site variant at this locus influences COVID-19 outcomes by altering the splicing of OAS1. Furthermore, this insight highlights the importance of including populations of different ancestries in genetic association studies and rapidly sharing data through large, international consortia.
Methods
Ethics
This study complies with all relevant ethical regulations; the contributing genetic association studies were approved by the VA Central institutional review board (VA MVP), the Jewish General Hospital research ethics board (BQC-19), the institutional review board of the Perelman School of Medicine at the University of Pennsylvania (PMBB), the institutional review board of Columbia University (CUB), the research ethics committees of Scotland (15/SS/0110), England, Wales and Northern Ireland (19/WM/0247) (GenOMICC) and the North West Multi-Centre Research Ethics Committee (UKB).
Study participants
Our analysis pooled hospitalized patients with COVID-19 of African ancestry (n = 2,787) from 6 cohorts. The UKB cohort contained 83 cases and 9,193 controls, the PMBB contained 436 cases and 10,761 controls, the CUB contained 304 cases and 2,246 controls, BQC-19 contained 50 cases and 50 controls, VA MVP contained 1,670 cases and 107,283 controls and GenOMICC contained 244 cases and 1,464 controls. Informed consent was obtained when required and ethical approval was obtained from the relevant research ethics boards. Ancestry was genetically inferred (see below for each cohort).
LD
LD (r2) was calculated using LDlink18 v.4.1 in the genomic region 113.30–113.45 megabases (Mb) (hg19) using data from the 1000 Genomes Project11.
Meta-analysis
The meta-analysis was done using inverse variance weighting in the R package meta v.5.1. Heterogeneity was measured using Cochran’s Q, Higgins–Thompson’s I2 and τ2 using the DerSimonian–Laird estimator.
Fine-mapping
Effect estimates and standard errors in the genomic region 113.30–113.45 Mb were taken from the HGI5 for individuals of European and African ancestry. LD (r2) was obtained from the 1000 Genomes Project11. Fine-mapping with shotgun stochastic search was performed using FINEMAP v.1.4 (ref. 17) with effect size estimates in the region for both ancestries (n = 383), excluding one triallelic variant (rs1051042). Importantly, among the 383 variants in the fine-mapping analysis, all 131 variants with genome-wide significance (P < 5 × 10−8) among individuals of European ancestry were included. First, the European ancestry data were fine-mapped using the equal probabilities of each variant as prior probabilities. The PIPs of this analysis were then used as prior probabilities in an analysis of the African ancestry data. Finally, this stepwise analysis was repeated but using scaled CADD-scores11 v.1.6 as prior probabilities for the first (European ancestry) step. The prior probabilities based on the CADD-scores were normalized so that the sum equaled 1. The variance of the effect size prior was set such that with 95% probability a variant can increase risk by at most an OR of 2 and then scaled using the case–control ratio as described19.
VA MVP summary statistics
The VA MVP is a US-based longitudinal research program investigating how genes, lifestyle and military exposure influence health and illness in veterans, with study recruitment commencing in 2011 (ref. 20). Study participants were genotyped using a customized Affymetrix Axiom Biobank Array (the MVP v.1.0 Genotyping Array) containing 723,305 variants21. Imputation was performed to a hybrid imputation panel consisting of the African Genome Resources panel (https://imputation.sanger.ac.uk/?about=1#referencepanels) and 1000 Genomes Project v3p5. COVID-19 cases were identified using an algorithm developed by the VA COVID National Surveillance Tool22. COVID-19-related hospitalizations were defined as hospital admissions between 7 d before and 30 d after an individual’s positive SARS-CoV-2 test. The association of hospitalized cases with COVID-19 versus all other MVP participants was tested under an additive logistic model and was corrected for age, age2, sex, age-by-sex and ethnicity-specific principal components. Individuals who died before 1 March 2020 were excluded, as was one individual from each related pair. The analysis was restricted to only African American MVP participants (as defined by HARE23), resulting in 1,300 cases and 98,129 controls.
BQC-19 summary statistics
The BQC-19 is a prospective hospital-based biobank recruiting patients with proven or suspected COVID-19 (institutional review board no. 2020–2137). Whole-genome genotyping was performed for all participants, with imputation using the TOPMed Imputation Server24. Individuals of African ancestry were determined by projecting genetic principal components on the 1000 Genomes Project reference panel. Cases (n = 50) were defined as patients hospitalized with COVID-19 or who died from the infection. Controls (n = 50) were other participants of African ancestry, of which 32 had a clinical presentation consistent with COVID-19 but never had a positive test. An additive logistic regression model with the first ten genetic principal components, with age, sex, age2, age-by-sex and age2-by-sex as covariates, was used to determine the effect of the protective G allele on the risk of being a case.
PMBB summary statistics
The PMBB contains approximately 60,000 prospectively consented participants, all patients of the Penn Medicine hospitals, for whom DNA samples were obtained and on whom extensive phenotypic information was generated from the electronic health record (EHR). A total of 20,079 participants were genotyped using the Illumina Global Screening Array v.2.0 and further imputed using the TOPMed Imputation Server. SNPs with a call rate <1%, minor allele frequency (MAF) <1% or imputation info score <0.3 were excluded from further analysis. To define each ancestral group, principal component analysis (PCA) was performed after merging the PMBB data with the 1000 Genomes Project reference dataset using the smartpca module of the Eigensoft package (version 7.2)25,26. We performed quantitative discriminant analysis on all samples using the 1000 Genomes Project samples as a training sets to generate ancestry calls for all PMBB samples included in the analysis. Ultimately 9,015 African ancestry genotyped samples were identified and included in our association study. All PMBB participants were followed for SARS-CoV-2 infection and hospitalization, with COVID-19 infection defined as any patient with a positive SARS-CoV-2 nasal swab or for whom the International Classification of Diseases billing code U07.1 was coded in the EHR and with COVID-19-related hospitalizations defined as the subset of these patients who had been admitted to hospital in the previous year with U07.1 as the admission diagnosis code or who had been admitted for COVID-19-related symptoms as determined by manual chart review. Association analyses were performed using the Firth logistic regression test as implemented in regenie27, including age, age2, sex, age-by-sex and the first six ancestry-specific principal components of the genomic data as covariates.
CUB summary statistics
The COVID-19 CUB was established in response to the New York City infection surge in March 2020. The biobank recruited COVID-19 cases of diverse ancestry among all patients who were treated at Columbia University Irving Medical Center between March and May 2020. All cases were diagnosed by positive SARS-CoV-2 PCR test based on nasopharyngeal samples. The mean age of cases was 62.9 years and the percentage of females was 43%. The DNA of whole-blood samples was extracted using standard procedures and genotyping was performed using the Illumina Global Diversity Array chip. The controls were genotyped using the Illumina Multi-Ethnic Global Ancestry chip. The analysis of intensity clusters and genotype calls was performed with the Illumina Genome Studio software (version 2.0); all SNPs were called on forward DNA strand and standard quality control filters were applied, including a per-SNP genotyping rate >95%, per-individual genotyping rate >90%, MAF > 0.01, and Hardy–Weinberg equilibrium test P > 10−8 in controls. The duplicates and cryptic relatedness in the given cohort were determined and excluded based on an estimated pairwise kinship coefficient >0.0884. After quality control, the dataset consisted of 6,757 individuals (1,029 cases and 5,728 controls) genotyped for 1,096,321 SNPs with an overall genotyping rate of 99.9%. The imputation analysis was performed with the TOPMed Imputation Server. A total of 13,439,413 common markers imputed at high quality (r2 > 0.8 and MAF > 0.01) were used in the downstream analyses. To define the African ancestry cluster, we used PCA against the 1000 Genomes Project reference populations followed by k-means clustering on significant principal components of ancestry. The African ancestry cluster contained 332 cases positive for SARS-CoV-2 and 2,246 population controls. Of the 332 cases of African ancestry, 304 had severe COVID-19 requiring hospitalization. Among the 304 cases included, 78 (26%) had respiratory failure requiring intubation and invasive ventilatory support and 86 (28%) died due to COVID-19. We then tested the effect of rs10774671 G on the risk of hospitalization using SAIGE28, after adjustment for sex and five principal components of ancestry. The collection of samples was approved under institutional review board protocol no. AAAS7370, while the genetic analyses were approved under institutional review board protocol no. AAAS7948.
GenOMICC summary statistics
A total of 3,893 critically ill cases with confirmed COVID-19 were recruited through the GenOMICC study in 208 intensive care units across the UK; 682 additional hospitalized cases with confirmed COVID-19 were recruited through the International Severe Acute Respiratory Infection Consortium (Coronavirus Clinical Characterisation Consortium). Current and previous versions of the study protocol are available at https://genomicc.org/protocol/. All participants gave informed consent (https://genomicc.org/protocol/#informed-consent). DNA extraction, sample quality control, genotype quality control, kinship estimation and imputation were performed with the pipelines described in Pairo-Castineira et al.3. Ancestry was inferred using ADMIXTURE and the superpopulations defined in the 1000 Genomes Project (European, South Asian, East Asian, African and American). When one individual had a probability >80% of pertaining to one ancestry, they were assigned to this ancestry; otherwise, they were assigned to the ‘admixed’ ancestry. After these steps, there were 244 unrelated individuals of African ancestry. Principal components were calculated according to the procedure outlined in Pairo-Castineira et al.3 for GenOMICC participants and UKB individuals. UKB participants were considered as potential controls if they were not identified by the UKB as outliers based on either genotyping missingness rate or heterogeneity; their sex was inferred from the genotypes that matched their self-reported sex. After excluding participants who had received PCR tests for COVID-19, based on the information downloaded from the UKB in August 2020, five random UKB individuals with matching inferred ancestry were sampled for each GenOMICC participant as controls. After sampling each control, individuals related up to the third degree were removed from the pool of potential further controls. Test for association between case–control status and allele dosage at the variant rs10774671 G was performed by fitting a logistic regression model using PLINK v.2.00 with sex, age, mean-centered age2, deprivation score decile of residential postcode and the first 10 genomic principal components as covariates. This research was conducted using the UKB resource under project no. 788.
UKB summary statistics
Association analyses were performed using the Firth logistic regression test implemented in regenie, including age, age2, sex, age-by-sex, age2-by-sex and ten ancestry-informative principle components as covariates. Data were downloaded from https://rgc-covid19.regeneron.com/results (23 March 2021). Continental ancestries were determined by projecting each sample onto principal components calculated from the HapMap3 reference panel, followed by kernel density estimation yielding a likelihood that a given sample belonged to each continental ancestry, as described previously29.
Reporting Summary
Further information on research design is available in the Nature Research Reporting Summary linked to this article.
Data availability
COVID-19 summary statistics for individuals of African ancestry are available at https://www.covid19hg.org/results/r6/ and CADD-scores v.1.6 can be accessed at https://cadd.gs.washington.edu/score. Genomes from the 1000 Genomes Project are available at https://www.internationalgenome.org/data. The fine-mapping association summary statistics produced in this study are available at https://doi.org/10.5281/zenodo.5708333. Source data are provided with this paper.
Code availability
The code used for the fine-mapping analysis can be found at https://doi.org/10.5281/zenodo.5708333.
References
COVID-19 Host Genetics InitiativeThe COVID-19 Host Genetics Initiative, a global initiative to elucidate the role of host genetic factors in susceptibility and severity of the SARS-CoV-2 virus pandemic.Eur. J. Hum. Genet. 28, 715–718 (2020).
Ellinghaus, D. et al. Genomewide association study of severe Covid-19 with respiratory failure. N. Engl. J. Med. 383, 1522–1534 (2020).
Pairo-Castineira, E. et al. Genetic mechanisms of critical illness in COVID-19. Nature 591, 92–98 (2021).
Zhang, Q. et al. Inborn errors of type I IFN immunity in patients with life-threatening COVID-19.Science 370, eabd4570 (2020).
COVID-19 Host Genetics Initiative Mapping the human genetic architecture of COVID-19. Nature https://doi.org/10.1038/s41586-021-03767-x (2021).
Zeberg, H. & Pääbo, S. The major genetic risk factor for severe COVID-19 is inherited from Neanderthals. Nature 587, 610–612 (2020).
Zeberg, H. & Pääbo, S. A genomic region associated with protection against severe COVID-19 is inherited from Neandertals. Proc. Natl Acad. Sci. USA 118, e2026309118 (2021).
Choi, U. Y., Kang, J.-S., Hwang, Y. S. & Kim, Y.-J. Oligoadenylate synthase-like (OASL) proteins: dual functions and associations with diseases. Exp. Mol. Med. 47, e144 (2015).
Zhou, S. et al. A Neanderthal OAS1 isoform protects individuals of European ancestry against COVID-19 susceptibility and severity. Nat. Med. 27, 659–667 (2021).
Bonnevie-Nielsen, V. et al. Variation in antiviral 2′,5′-oligoadenylate synthetase (2′5′AS) enzyme activity is controlled by a single-nucleotide polymorphism at a splice-acceptor site in the OAS1 gene.Am. J. Hum. Genet. 76, 623–633 (2005).
Auton, A. et al. A global reference for human genetic variation. Nature 526, 68–74 (2015).
Rentzsch, P., Schubach, M., Shendure, J. & Kircher, M. CADD-Splice—improving genome-wide variant effect prediction using deep learning-derived splice scores. Genome Med. 13, 31 (2021).
Green, R. E. et al. A draft sequence of the Neandertal genome. Science 328, 710–722 (2010).
Chen, L., Wolf, A. B., Fu, W., Li, L. & Akey, J. M. Identifying and interpreting apparent Neanderthal ancestry in African individuals. Cell 180, 677–687.e16 (2020).
Sankararaman, S., Patterson, N., Li, H., Pääbo, S. & Reich, D. The date of interbreeding between Neandertals and modern humans. PLoS Genet. 8, e1002947 (2012).
Wickenhagen, A. et al. A prenylated dsRNA sensor protects against severe COVID-19.Science 374, eabj3624 (2021).
Sams, A. J. et al. Adaptively introgressed Neandertal haplotype at the OAS locus functionally impacts innate immune responses in humans. Genome Biol. 17, 246 (2016).
Machiela, M. J. & Chanock, S. J. LDlink: a web-based application for exploring population-specific haplotype structure and linking correlated alleles of possible functional variants. Bioinformatics 31, 3555–3557 (2015).
Benner, C. et al. FINEMAP: efficient variable selection using summary data from genome-wide association studies. Bioinformatics 32, 1493–1501 (2016).
Gaziano, J. M. et al. Million Veteran Program: a mega-biobank to study genetic influences on health and disease. J. Clin. Epidemiol. 70, 214–223 (2016).
Hunter-Zinck, H. et al. Genotyping array design and data quality control in the Million Veteran Program. Am. J. Hum. Genet. 106, 535–548 (2020).
Chapman, A. et al. A natural language processing system for national COVID-19 surveillance in the US Department of Veterans Affairs. In Proc. 1st Workshop on NLP for COVID-19 at ACL 2020 (Association for Computational Linguistics, 2020).
Fang, H. et al. Harmonizing genetic ancestry and self-identified race/ethnicity in genome-wide association studies. Am. J. Hum. Genet. 105, 763–772 (2019).
Kowalski, M. H. et al. Use of >100,000 NHLBI Trans-Omics for Precision Medicine (TOPMed) Consortium whole genome sequences improves imputation quality and detection of rare variant associations in admixed African and Hispanic/Latino populations. PLoS Genet. 15, e1008500 (2019).
Patterson, N., Price, A. L. & Reich, D. Population structure and eigenanalysis. PLoS Genet. 2, e190 (2006).
Price, A. L. et al. Principal components analysis corrects for stratification in genome-wide association studies. Nat. Genet. 38, 904–909 (2006).
Mbatchou, J. et al. Computationally efficient whole-genome regression for quantitative and binary traits. Nat. Genet. 53, 1097–1103 (2021).
Zhou, W. et al. Efficiently controlling for case-control imbalance and sample relatedness in large-scale genetic association studies. Nat. Genet. 50, 1335–1341 (2018).
Kosmicki, J. A. et al. Pan-ancestry exome-wide association analyses of COVID-19 outcomes in 586,157 individuals. Am. J. Hum. Genet. 108, 1350–1355 (2021).
Acknowledgements
We thank the COVID-19 Host Genetics Initiative and Regeneron for making the data from the genome-wide association study available. Genotyping and phenotyping of the Columbia University cohort was made possible by the Columbia University COVID-19 Biobank Genomics Workgroup members, including R. Mayeux, M. P. Reilly, W. Chung, D. B. Goldstein, C. K. Garcia, I. Ionita-Laza, A. Califano, S. M. O’Byrne, D. Pendrick, S. Sengupta, P. Sims and A.-C. Uhlemann. The Columbia University COVID-19 Biobank was supported by Columbia University and the National Center for Advancing Translational Sciences (NCATS), National Institutes of Health (NIH), through grant no. UL1TR001873. A.K. was supported by grant no. K25(K25DK128563) from the NIH/National Institute of Diabetes and Digestive and Kidney Diseases and grant no. TL1(UL1TR001873) from NIH/NCATS. The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH. The Richards research group is supported by the Canadian Institutes of Health Research (CIHR) (grant nos. 365825 and 409511), the Lady Davis Institute of the Jewish General Hospital, the Canadian Foundation for Innovation, the NIH Foundation, Cancer Research UK, Genome Québec, the Public Health Agency of Canada, the McGill Interdisciplinary Initiative in Infection and Immunity and the Fonds de Recherche du Québec Santé (FRQS). G.B.-L. is supported by a CIHR scholarship and a joint FRQS and Québec Ministry of Health and Social Services scholarship. T.N. is supported by a research fellowship of the Japan Society for the Promotion of Science for Young Scientists. J.B.R. is supported by an FRQS Clinical Research Scholarship. We acknowledge support from Calcul Québec and Compute Canada. TwinsUK is funded by the Wellcome Trust, the Medical Research Council, the European Union, the National Institute for Health Research-funded BioResource and the Clinical Research Facility and Biomedical Research Centre based at Guy’s and St. Thomas’ NHS Foundation Trust in partnership with King’s College London. The Biobanque Québec COVID-19 is funded by FRQS, Genome Québec and the Public Health Agency of Canada, the McGill Interdisciplinary Initiative in Infection and Immunity and FRQS. GenOMICC controls were obtained using UK Biobank Resource under project 788 funded by Roslin Institute Strategic Programme Grants from the BBSRC (BBS/E/D/10002070 and BBS/E/D/30002275) and Health Data Research UK (references HDR-9004 and HDR-9003). The PMBB is funded by a gift from the Smilow family, the NCATS of the NIH under Clinical and Translational Science Award no. UL1TR001878 and the Perelman School of Medicine at the University of Pennsylvania. H.Z. is supported by the Jeanssons and Magnus Bergsvalls Foundations the Swedish Research Council (2021-03050). We thank the PMBB team members who made this work possible, including D. Rader, M. Ritchie, Y. Bradford, S. Setia Verma, A. Lucas and B. Li. We thank S. Pääbo for careful reading of the manuscript and helpful comments. The funding agencies had no role in the design, implementation or interpretation of this study.
Author information
Authors and Affiliations
Consortia
Contributions
H.Z. conceptualized the study. J.B.R. and H.Z. devised the methodology. J.E.H., G.B.-L., A.K., E.P.-C., T.G.D., G.M.P., T.N., A.G., A.V., J.K.B., K.K., J.B.R. and H.Z. carried out the investigation. J.B.R. and H.Z. wrote the original manuscript draft. J.E.H., G.B.-L., A.K., E.P.-C., T.G.D., G.M.P., T.N., A.G., A.V., J.K.B., K.K., J.B.R. and H.Z. reviewed and edited the draft.
Corresponding author
Ethics declarations
Competing interests
J.B.R. has served as an advisor to GlaxoSmithKline and Deerfield Capital. His institution has received investigator-initiated grant funding from Eli Lilly, GlaxoSmithKline and Biogen for projects unrelated to this research. He is the founder of 5 Prime Sciences. The other authors declare no competing interests.
Peer review information
Nature Genetics thanks Rasika Mathias and the other, anonymous, reviewer(s) for their contribution to the peer review of this work. Peer reviewer reports are available.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Source data
Source Data Fig. 1
LD in the OAS1/2/3 region.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Huffman, J.E., Butler-Laporte, G., Khan, A. et al. Multi-ancestry fine mapping implicates OAS1 splicing in risk of severe COVID-19. Nat Genet 54, 125–127 (2022). https://doi.org/10.1038/s41588-021-00996-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41588-021-00996-8
This article is cited by
-
Priority index for critical Covid-19 identifies clinically actionable targets and drugs
Communications Biology (2024)
-
Role of OAS gene family in COVID-19 induced heart failure
Journal of Translational Medicine (2023)
-
Angiotensin-converting enzyme 2 (ACE2) polymorphisms and susceptibility of severe SARS-CoV-2 in a subset of Pakistani population
Virology Journal (2023)
-
Alternative splicing in lung influences COVID-19 severity and respiratory diseases
Nature Communications (2023)
-
Genetics and epigenetics of primary Sjögren syndrome: implications for future therapies
Nature Reviews Rheumatology (2023)