As innovations in the biotechnology sector continue to proliferate, the traditional education of medical students, residents and fellows will need to change to incorporate innovation as a core tenet of training.
The COVID-19 pandemic uncovered pressing needs for improved healthcare access, affordability and quality1. Rising to the challenge, individuals in the biotechnology sector embarked on collaborative ventures to design and implement innovative solutions to pandemic demands, which in many ways were masking inefficiencies in how care was delivered in general2,3,4,5,6. In parallel, the challenges posed by the pandemic spurred medical training programs to re-evaluate the goals and structures of the traditional medical curriculum7,8,9. Didactics and simulations transitioned into remote formats for medical students, and programs strove to reduce the cognitive load for residents and fellows in the setting of a pandemic10,11,12. Yet developments in medical training thus far still focus on the delivery and format of the curriculum, including flipped classroom and case-based models, as opposed to teaching innovation13,14. At this critical juncture, we propose the incorporation of innovation itself as a core tenet of medical training, as the importance of real-time medical innovations in biotechnology cannot be denied.
As the role of the healthcare professional continues to expand, and as healthcare reimbursement increasingly prioritizes value over quantity, acquiring the skill set of an innovator has become more vital and pertinent to all stages of medical training. Innovation in healthcare is defined as the implementation of a novel idea in the advancement of care delivery and health outcomes15. Our previous work demonstrated successful integration of innovation education into ACGME (Accreditation Council for Graduate Medical Education)-accredited residency programs and hospital departments16,17. Here, we delve further into innovation training: the skill sets in demand, potential barriers and opportunities to develop an infrastructure for innovation in medical training. Seizing these opportunities to address the needs of current healthcare trainees may enhance the development of change-markers in the field of biotechnology.
Innovation: a trained skill set
The pandemic placed a spotlight on the impact of innovation generated by healthcare professionals. Trainees are uniquely positioned within care teams to generate ground-level ideas for innovative care. Historically, the novel perspectives of trainees have contributed significantly to several landmark discoveries, from the description of pancreatic islet cells to the extraction of heparin18. Such opportunities are often inspired by trainees’ roles serving as a team’s interface with patients and with the electronic medical system through their administrative responsibilities. However, to a certain extent, current clinical training actively suppresses innovation because established principles and protocols are often promoted as the ‘right’ and the only way (i.e., look for horses, not zebras). The key issue is therefore training professionals to know when and how to innovate. Trainees equipped with the proper skill sets and resources have significant potential to identify, validate and devise solutions to current unmet needs, develop new gold standards of clinical care and reduce potential future problems. Additionally, embedding healthcare innovation programs directly within the academic setting may decrease the risk of premature technology transfer into an industry where the technical, clinical and/or biological expertise may not be fully realized. These risks are notable, as increased internal validation correlates with future commercial value19.
Targeted education is necessary to equip future generations of medical professionals with the ability to innovate efficiently and effectively. Although tangible tools and resources are important, the skill set to use them effectively will serve as the lifelong foundation for innovation. Learning the foundational steps of identifying problems, prototyping and researching the market in conjunction with experiential learning can provide trainees with a blueprint for innovation. From an industry standpoint, key components to successful innovations include establishing product–market fit, understanding the end-user and determining value drivers. The ACGME currently does not mandate any level of innovation-specific training in medical training and education. We believe that a high-quality education in this fundamental skill set of innovation can be incorporated into the training of medical professionals of all levels, regardless of the extent of tangible resources at the training institutions.
Survey
To analyze the current state of innovation education at the medical trainee level, we sent a preliminary survey (see Supplementary Note) to readers of 2 Minute Medicine, a free open-source medical media and news organization20. The survey was created to assess trainees’ perception of innovation across three domains: understanding and participation in innovation, barriers to pursuing innovation and tools needed to pursue innovation. Trainees, including medical students, residents and fellows, answered questions in these domains according to Likert-type scales of 1–5 (such as Unimportant, Slightly Important, Moderately Important, Important and Very Important).
We received 51 responses from medical trainees, who included medical students, residents and fellows (response rate 51/1,142). Women made up 27% of respondents. Thirty percent of respondents described their learning environment as rural or suburban, and 26% of respondents were Hispanic or African-American (Table 1).
Present medical trainees’ perception of innovation
Even before the COVID-19 pandemic, the role of the medical professional has been expanding. Physicians have strived to influence healthcare beyond the walls of hospitals, leading to increasing numbers of trainees seeking additional degrees in fields such as business and administration, public health and public policy21. Aside from pursuing additional degrees, many trainees have channeled their efforts into social justice activism and government. In such a setting, medical innovation remains an underdeveloped area of training.
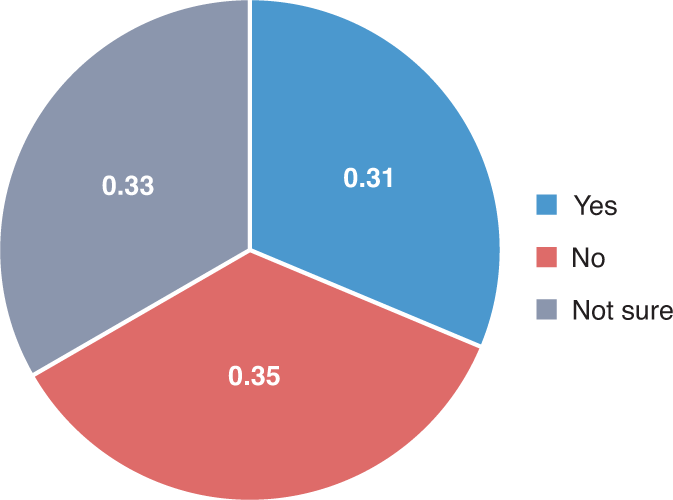
A central question for respondents was, “Do you consider yourself an innovator?” Thirty-one percent of respondents considered themselves innovators, 35% did not consider themselves innovators and 33% were unsure (Fig. 1). A traditional view of an innovator conjures images of a failed maverick seeking to create an intervention, or a social media prodigy changing human connection with a few strokes on a keyboard22. In all of these depictions, innovation is sought as an intrinsic quality, yet this fails to describe reality. Innovation requires a backbone of methodical research, as well as skilled execution to translate an idea from inception to a finished product. Even more, those images fail to account for the multidisciplinary approach required to change care. For trainees interested in innovation, these notions can act as mental and process blocks.
Barriers to healthcare innovation at the trainee level
There are various barriers to medical innovation, including technical-level barriers, public policy barriers, and political and economic barriers23. These range from a lack of understanding of disease processes to lack of education and exposure to the fundamental domains of healthcare innovation, as well as regulatory barriers to technology implementation.
From our survey, we noted the current level of participation, barriers and necessary tools to encourage innovation for medical trainees:
-
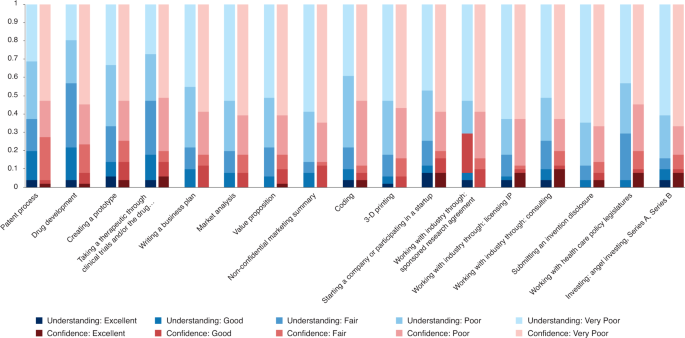
Participation: Trainees had relatively low participation across different forms of innovation. The three activities in which respondents reported the highest participation were improving disease specific outcomes (18%), healthcare delivery and access (16%) and workflow efficiencies (16%). The activities with the lowest participation, 8% in each case, were medical device development, drug development and improving pharmaceutical adherence. Trainees also rated themselves as having lower confidence relative to their stated level of understanding across areas of innovation in Fig. 2.
-
Barriers: Trainees ranked perceived barriers to innovation using the scale described above. The barriers most commonly noted as “Most Important” on the Likert scale included limited time and energy (43%), lack of physical resources (35%) and lack of expertise (31%).
-
Tools: The most beneficial tools for trainees were dedicated time (61%), financial support via grants and start-up funding (49%) and partnership with mentors (47%).
Opportunities for innovation integration in medical training programs
These responses indicate the innovation areas in which trainees are interested, the potential barriers and the tools that would help advance their pursuits. Trainees reported a generally low level of confidence in pursuing innovative activities despite relatively higher levels of understanding, which indicates a gap in the ability to translate ideas into skilled practice. As a result, integrated, hands-on programs as previously implemented may be a way to bridge the gap between knowing and building16,17. We recognize that institutions have various levels of resources and participants may seek different intensities of training. Hence, we present three thematic innovation programs, ranging from regimented innovation tracks to supplementary innovation programs that are amenable to integration into medical training.
Innovation tracks
For the most streamlined and direct approach, we advocate for longitudinal learning that provides in-depth teaching and protects time for trainees to pursue ventures. Medical schools and residency programs have incorporated specialty tracks into their curriculum, which have traditionally focused on training in global health, management, urban studies and policy. A longitudinal ‘innovation’ track would provide the time and resources for trainees to pursue ideas and collaborate with other departments and companies. A blueprint for such programs was previously published by the Medically Engineered Solutions in Healthcare (MESH) Incubator, wherein innovation bootcamps are taught in the same structure as traditional medical rotations for residents and fellows throughout the academic year, as well as the MESH Incubator Innovation Teams biodesign program, which integrates traditional multidisciplinary biodesign (medical, engineers, business personnel) into an integrated part-time program in which full-time trainees can participate without the need to step away from their ACGME training. Additional programs that may require dedicated time away from residency or training include the Stanford Biodesign Program, the University of Texas Austin’s Distinction Program for Care Transformation and Emory University’s Medical Innovation Track. These are 10-month to 2-year programs that bring together medical trainees, business personnel and scientists to learn and collaborate on innovative solutions24,25,26,27.
Workshop series
Residency programs and hospitals are also increasingly recognizing the importance of innovation programs. Short, intensive programs in technology development, including classes on intellectual property, have proven to be a venue for innovation training. Massachusetts General Hospital pioneered the first healthcare innovation rotation integrated into an ACGME residency program16. This 1-week rotation is taught to all trainees in all specialties and teaches the basics of artificial intelligence, 3-D printing, prototyping, intellectual property, commercialization, venture funding and much more, with documented outcomes demonstrating effectiveness17. These programs can be adapted and interwoven into the medical curriculum, especially during break and summer months.
Targeted skills
In addition to innovation tracks and workshops, short-term targeted programs can enhance specific trainee skills. The American Medical Association created the Accelerating Change in Medical Education Consortium with 37 medical schools that enroll nearly 24,000 students to bring about a platform for sharing pioneering ideas and solutions28. These schools include New York University, which created the NYU Health Care by the Numbers Curriculum to train medical students in using big data to improve healthcare quality, and Stanford Medical School, which has integrated virtual reality technology to improve educational experiences and promote diversity. Additionally, the creation of virtual innovative spaces in response to crisis, such as the Mass General Brigham COVID Innovation Center29, brings together trainee innovators and experienced investigators, and creates opportunities and fosters connections for trainees in technology, business and life sciences. These groups are low cost and high yield for hospitals and medical schools that have a more moderate level of resources, faculty time and funding.
Conclusions
The modern practice of medicine has extended beyond the examination room to the integration of basic science, innovation and biotechnology research at the bedside at a faster pace than ever before. Physicians, equipped with clinical knowledge, can both identify and address current and emerging gaps in quality healthcare. Our broad survey reveals that trainees interested in medical innovation lack the skills and resources to pursue such ventures. We acknowledge the limitations of our preliminary survey, which include low response rates. Additionally, our respondents might be trainees who routinely consume medical news and might not be representative of all medical trainees. However, using the survey as a soundboard, we can gain insight into the personal and professional barriers that trainees face when pursuing innovative solutions. We examined current pilot methods of incorporating innovation into the medical trainee curriculum. We propose a variety of models for institutions seeking to incorporate innovation into their curriculum, including innovation tracks, workshop groups and targeted skills. Each of these models provides mentorship, education and resources for trainees while accounting for time and financial restraints. The range in intensity, resources and stewardship of these programs allow medical and residency programs to tailor their innovation education models based on their students’ needs and institutional resources. An early introduction to constructive questioning can help train agile thinkers and change-makers in the field of biotechnology. The practice of problem-solving requires trainees to practice the fundamental skills of gathering information, building a diverse team, organizing a strategy and taking a risk to address the problem30. These transferable skills, once honed, extend to patient care within the wards and beyond.
References
Demeke, H. B. et al. MMWR Morb. Mortal. Wkly. Rep. 70, 240–244 (2021).
Woolliscroft, J. O. Acad. Med. 95, 1140–1142 (2020).
Lee, S. M. & Trimi, S. J. Bus. Res. 123, 14–22 (2021).
Chonde, D. B. et al. J. Am. Coll. Radiol. 18, 1000–1008 (2021).
Sapoval, M. et al. Diagn. Interv. Imaging 101, 413–415 (2020).
Imbrie-Moore, A. M. et al. Health Care (Don Mills) 8, 225 (2020).
Sabzwari, S. MedEdPublish 9, 80 (2020).
Gaur, U. et al. Clin. Med. (Lond.) 2, 1992–1997 (2020).
Chan, A. K., Wu, C., Cheung, A. & Succi, M. D. J. Med. Internet Res. 23, e26666 (2021).
Hartsough, E. M., Arries, C., Amin, K. & Powell, D. Acad. Pathol. 8, 23742895211010265 (2021).
Asselin, M. et al. MedEdPORTAL 17, 11134 (2021).
Sukumar, S. et al. MedEdPORTAL 17, 11106 (2021).
McLean, S. F. J. Med. Educ. Curric. Dev. 3, JMECD.S20377 (2016).
Hew, K. F. & Lo, C. K. BMC Med. Educ. 18, 38 (2018).
Kimble, L. E. & Massoud, E. M. J. EMJ Innov. 1, 89–91 (2017).
Succi, M. D. et al. J. Am. Coll. Radiol. 17, 1329–1333 (2020).
Succi, M. D., Uppot, R. N., Gee, M. S., McLoud, T. C. & Brink, J. A. J. Am. Coll. Radiol. 15, 892–896 (2018).
Bettany, K. Br. Med. J. 348, g2138 (2014).
Toner, M. & Tompkins, R. G. Surgery 143, 168–171 (2008).
2 Minute Medicine; https://www.2minutemedicine.com/
Brill, J. V. Gastroenterology 144, 655 (2013).
Jeske, M. Engag. Sci. Technol. Soc. 6, 306 (2020).
Aspden, P. (ed.). Medical Innovation in the Changing Healthcare Marketplace: Conference Summary (National Academies Press, 2002).
Augustin, D. A. et al. Surgery 167, 535–539 (2020).
The University of Texas at Austin–Dell Medical School. Advancing Care Transformation; https://dellmed.utexas.edu/education/academics/graduate-medical-education/distinction-program-for-care-transformation
Harvard University. Harvard HealthTech Innovation in Healthcare; https://projects.iq.harvard.edu/healthtechfellowship/home
Emory University School of Medicine. Medical Innovation Track; https://www.med.emory.edu/education/gme/housestaff/residency-tracks/medical-innovation.html
Members of the Accelerating Change in Medical Education Consortium. Accelerating Change in Medical Education; https://www.ama-assn.org/education/accelerating-change-medical-education/member-schools-consortium
Center for COVID Innovation; https://covidinnovation.partners.org/
Green, M. J. et al. J. Med. Humanit. 37, 475–483 (2016).
Acknowledgements
This research did not receive any specific grant from funding agencies in the public, commercial or not-for-profit sectors. It was approved with exemption by the Institutional Review Board of Massachusetts General Brigham.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Supplementary information
Supplementary Information
Survey sent to 1,000 medical trainees
Rights and permissions
About this article
Cite this article
Boms, O., Shi, Z., Mallipeddi, N. et al. Integrating innovation as a core objective in medical training. Nat Biotechnol 40, 434–437 (2022). https://doi.org/10.1038/s41587-022-01253-x
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41587-022-01253-x
This article is cited by
-
Integrating a healthcare innovation bootcamp into an international medical conference to democratize innovation learning
Nature Biotechnology (2023)
-
A strategy to incentivize innovation in the health care system: the innovation RVU
Nature Biotechnology (2023)
-
The need for need-finding in medical education
Nature Biotechnology (2023)
-
Innovating on innovation training with the Virtual Magic Wand (VMW) program: a qualitative study
Archives of Dermatological Research (2022)