Abstract
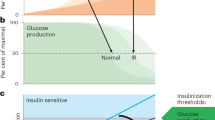
Although it is well-established that reductions in the ratio of insulin to glucagon in the portal vein have a major role in the dysregulation of hepatic glucose metabolism in type-2 diabetes1,2,3, the mechanisms by which glucagon affects hepatic glucose production and mitochondrial oxidation are poorly understood. Here we show that glucagon stimulates hepatic gluconeogenesis by increasing the activity of hepatic adipose triglyceride lipase, intrahepatic lipolysis, hepatic acetyl-CoA content and pyruvate carboxylase flux, while also increasing mitochondrial fat oxidation—all of which are mediated by stimulation of the inositol triphosphate receptor 1 (INSP3R1). In rats and mice, chronic physiological increases in plasma glucagon concentrations increased mitochondrial oxidation of fat in the liver and reversed diet-induced hepatic steatosis and insulin resistance. However, these effects of chronic glucagon treatment—reversing hepatic steatosis and glucose intolerance—were abrogated in Insp3r1 (also known as Itpr1)-knockout mice. These results provide insights into glucagon biology and suggest that INSP3R1 may represent a target for therapies that aim to reverse nonalcoholic fatty liver disease and type-2 diabetes.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$29.99 / 30 days
cancel any time
Subscribe to this journal
Receive 51 print issues and online access
$199.00 per year
only $3.90 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
Data availability
All data generated and analysed in this study are available in the Article and its Supplementary Information files, which include a table containing all raw data. Source Data for Figs. 1–3, Extended Data Figs. 1–8 are included with the paper.
References
Unger, R. H. Glucoregulatory hormones in health and disease. A teleologic model. Diabetes15, 500–506 (1966).
Unger, R. H. Pancreatic glucagon in health and disease. Adv. Intern. Med. 17, 265–288 (1971).
Müller, T. D., Finan, B., Clemmensen, C., DiMarchi, R. D. & Tschöp, M. H. The new biology and pharmacology of glucagon. Physiol. Rev. 97, 721–766 (2017).
Brand, C. L. et al. Immunoneutralization of endogenous glucagon with monoclonal glucagon antibody normalizes hyperglycaemia in moderately streptozotocin-diabetic rats. Diabetologia37, 985–993 (1994).
Sørensen, H. et al. Immunoneutralization of endogenous glucagon reduces hepatic glucose output and improves long-term glycemic control in diabetic ob/ob mice. Diabetes55, 2843–2848 (2006).
Okamoto, H. et al. Glucagon receptor inhibition normalizes blood glucose in severe insulin-resistant mice. Proc. Natl Acad. Sci. USA114, 2753–2758 (2017).
Kazda, C. M. et al. Evaluation of efficacy and safety of the glucagon receptor antagonist LY2409021 in patients with type 2 diabetes: 12- and 24-week phase 2 studies. Diabetes Care39, 1241–1249 (2016).
Guzman, C. B. et al. Treatment with LY2409021, a glucagon receptor antagonist, increases liver fat in patients with type 2 diabetes. Diabetes Obes. Metab. 19, 1521–1528 (2017).
Kazda, C. M. et al. Treatment with the glucagon receptor antagonist LY2409021 increases ambulatory blood pressure in patients with type 2 diabetes. Diabetes Obes. Metab. 19, 1071–1077 (2017).
Liang, Y. et al. Reduction in glucagon receptor expression by an antisense oligonucleotide ameliorates diabetic syndrome in db/db mice. Diabetes 53, 410–417 (2004).
Sloop, K. W. et al. Hepatic and glucagon-like peptide-1-mediated reversal of diabetes by glucagon receptor antisense oligonucleotide inhibitors. J. Clin. Invest. 113, 1571–1581 (2004).
Henderson, S. J. et al. Robust anti-obesity and metabolic effects of a dual GLP-1/glucagon receptor peptide agonist in rodents and non-human primates. Diabetes Obes. Metab. 18, 1176–1190 (2016).
Ozcan, L. et al. Calcium signaling through CaMKII regulates hepatic glucose production in fasting and obesity. Cell Metab. 15, 739–751 (2012).
Wang, Y. et al. Inositol-1,4,5-trisphosphate receptor regulates hepatic gluconeogenesis in fasting and diabetes. Nature485, 128–132 (2012).
Ozcan, L. et al. Activation of calcium/calmodulin-dependent protein kinase II in obesity mediates suppression of hepatic insulin signaling. Cell Metab. 18, 803–815 (2013).
Feriod, C. N. et al. Hepatic inositol 1,4,5 trisphosphate receptor type 1 mediates fatty liver. Hepatol. Commun. 1, 23–35 (2017).
Perry, R. J. et al. Leptin mediates a glucose-fatty acid cycle to maintain glucose homeostasis in starvation. Cell172, 234–248 (2018).
Perry, R. J. et al. Hepatic acetyl CoA links adipose tissue inflammation to hepatic insulin resistance and type 2 diabetes. Cell160, 745–758 (2015).
Pagnon, J. et al. Identification and functional characterization of protein kinase A phosphorylation sites in the major lipolytic protein, adipose triglyceride lipase. Endocrinology153, 4278–4289 (2012).
Liljenquist, J. E. et al. Effects of glucagon on lipolysis and ketogenesis in normal and diabetic men. J. Clin. Invest. 53, 190–197 (1974).
Gravholt, C. H., Møller, N., Jensen, M. D., Christiansen, J. S. & Schmitz, O. Physiological levels of glucagon do not influence lipolysis in abdominal adipose tissue as assessed by microdialysis. J. Clin. Endocrinol. Metab. 86, 2085–2089 (2001).
Wu, M. S. et al. Does glucagon increase plasma free fatty acid concentration in humans with normal glucose tolerance? J. Clin. Endocrinol. Metab. 70, 410–416 (1990).
Jensen, M. D., Heiling, V. J. & Miles, J. M. Effects of glucagon on free fatty acid metabolism in humans. J. Clin. Endocrinol. Metab. 72, 308–315 (1991).
Nichols, B. J. & Denton, R. M. Towards the molecular basis for the regulation of mitochondrial dehydrogenases by calcium ions. Mol. Cell. Biochem. 149-150, 203–212 (1995).
Foster, D. W. Malonyl-CoA: the regulator of fatty acid synthesis and oxidation. J. Clin. Invest. 122, 1958–1959 (2012).
Kadam, P. & Bhalerao, S. Sample size calculation. Int. J. Ayurveda Res. 1, 55–57 (2010).
Perry, R. J. et al. Non-invasive assessment of hepatic mitochondrial metabolism by positional isotopomer NMR tracer analysis (PINTA). Nat. Commun. 8, 798 (2017).
Petersen, K. F., Dufour, S., Cline, G. W. & Shulman, G. I. Regulation of hepatic mitochondrial oxidation by glucose–alanine cycling during starvation in humans. J. Clin. Invest. 129, 4671–4675 (2019).
Perry, R. J. et al. Propionate increases hepatic pyruvate cycling and anaplerosis and alters mitochondrial metabolism. J. Biol. Chem. 291, 12161–12170 (2016).
Perry, R. J. et al. Mechanism for leptin’s acute insulin-independent effect to reverse diabetic ketoacidosis. J. Clin. Invest. 127, 657–669 (2017).
Yu, C. et al. Mechanism by which fatty acids inhibit insulin activation of insulin receptor substrate-1 (IRS-1)-associated phosphatidylinositol 3-kinase activity in muscle. J. Biol. Chem. 277, 50230–50236 (2002).
Jurczak, M. J. et al. SGLT2 deletion improves glucose homeostasis and preserves pancreatic β-cell function. Diabetes60, 890–898 (2011).
Bligh, E. G. & Dyer, W. J. A rapid method of total lipid extraction and purification. Can. J. Biochem. Physiol. 37, 911–917 (1959).
Camporez, J. P. et al. ApoA5 knockdown improves whole-body insulin sensitivity in high-fat-fed mice by reducing ectopic lipid content. J. Lipid Res. 56, 526–536 (2015).
Camporez, J. P. et al. Cellular mechanisms by which FGF21 improves insulin sensitivity in male mice. Endocrinology154, 3099–3109 (2013).
Acknowledgements
We thank M. Montminy, T. Sonntag and Y.-S. Yoon for kindly providing the CRTC2 antibody and control samples, and for their advice on the interpretation of the CRTC2 blots; H. S. Sui for generously providing the pATGL antibody; D. Vatner for his advice on these studies; and X. Ma, J. Dong, W. Zhu, M. Kahn, K. Harry and M. Batsu for their expert technical assistance. These studies were funded by grants from the United States Public Health Service (R01 DK113984, P30 DK059635, P30 DK034989, T32 DK101019, K99/R00 CA215315, R01 NS087568, UL1TR000142, T32 DK007058 and F32 DK114954). The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH.
Author information
Authors and Affiliations
Contributions
The study was designed by R.J.P. and G.I.S. Data were collected and analysed by R.J.P., D.Z., M.T.G., A.L.B., L.G., A.R.N., A.R.-C., Y.W., L.P., S.D., Y.Z., X.-M.Z., G.M.B., K.T., Y.N., K.F.P., G.W.C., B.E.E. and M.H.N. The manuscript was written by R.J.P. and G.I.S. with contributions and approval from all authors.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Peer review informationNature thanks Ilya Bezprozvanny and the other, anonymous, reviewer(s) for their contribution to the peer review of this work.
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Extended data figures and tables
Extended Data Fig. 1 Glucagon acutely stimulates hepatic gluconeogenesis by increasing hepatic acetyl-CoA content and PC flux.
a, Body weight (n = 11). b, Expression of INSP3R1 protein in the liver (n = 5). Blots in b, c, e and Figs. 1f, 2a, Extended Data Figs. 3f, g, 4a were stripped and reprobed for all proteins of interest. *P < 0.05 versus Insp3r1-knockout mice not treated with glucagon. c, INSP3R protein expression in cytosolic (c.) and crude mitochondrial (c.m.) fractions from primary hepatocytes, in which VDAC was examined as a marker for mitochondrial protein content, and calreticulin as a marker for non-mitochondria-associated membrane protein. Right, phosphorylation of INSP3R1 in the liver of mice infused with glucagon (n = 5). d, Phosphorylation of CRTC2 in the liver (n = 5). The CRTC2 phosphorylation gel was stripped and reprobed to assess HSP90 (loading control). e, Phosphorylation of CAMKIV in the liver, with or without a 2-h acute infusion of glucagon (n = 5). f, Liver glycogen content (n = 5 wild type – glucagon, otherwise n = 6). No differences were observed using one-way analysis of variance with Bonferroni’s multiple comparisons test. g–i, Plasma [m + 1], [m + 2] and [m + 7]glucose enrichment during a 2-h infusion of [3-13C]lactate and [2H7]glucose (n = 5 wild type and 6 knockout, with the exception of i, for which n = 4 wild type + glucagon at 100 and 110 min). j, k, Plasma total amino acid and alanine concentrations (n = 5 wild type and 6 knockout). In j, k, groups were compared before and after glucagon treatment by two-tailed paired Student’s t-test, and genotypes were compared by two-tailed unpaired Student’s t-test. l, m, Liver total amino acid and alanine concentrations (n = 5). n, o, In vitro glucose production (n = 9) and VPC (n = 4) in isolated hepatocytes. p, q, In vitro glucose production (n = 9) and VPC (n = 4) in isolated hepatocytes with and without 150 pM insulin. Basal data (no insulin) are duplicated from n and o. r, s, In vitro glucose production (n = 8) and VPC (n = 3) in isolated hepatocytes with and without a malic enzyme (ME) inhibitor. **P < 0.01, ****P < 0.0001 versus wild type − glucagon − ME inhibitor. t–v, Plasma connecting peptide, glucagon and glucose concentrations in mice (n = 6 wild type and 7 knockout) treated with somatostatin, basal insulin and glucagon. Comparisons before and after glucagon treatment used a two-tailed paired Student’s t-test. w, x, Endogenous glucose production and VPC (n = 6 wild type and 7 knockout). In all panels, comparisons with and without glucagon, insulin or malic enzyme inhibitor, and wild type versus knockout comparisons were performed using a two-tailed unpaired Student’s t-test, unless otherwise stated. In all panels in which comparisons were performed (that is, all panels with the exception of g, i), if no P value is shown, groups were not significantly different. In all panels, mean ± s.e.m. is shown. All n values refer to numbers of mice.
Extended Data Fig. 2 Glucagon-stimulated glucose production requires activation of the PLC and PKA pathways, converging to activate INSP3 signalling.
a–p, In vitro glucose production and VPC in isolated hepatocytes with and without ET-18-OCH3 (n = 3) (a, b), U-73122 (n = 3, except for knockout − glucagon-U-73122 in d (n = 2)) (c, d), H-89 (n = 6) (e, f), vasopressin (n = 3) (g, h), 2-APB (n = 3) (i, j), caffeine (n = 3) (k, l), KN-93 (n = 6) (m, n) and thapsigargin (n = 3) (o, p). In all panels, *P < 0.05, **P < 0.01 and ***P < 0.001 versus wild type − glucagon − drug; §P < 0.05, §§P < 0.01 and §§§P < 0.001 versus wild type + glucagon − drug by two-tailed unpaired Student’s t-test. If no statistical comparison is denoted, the groups were not significantly different. Mean ± s.e.m. is shown.
Extended Data Fig. 3 Glucagon stimulates HGP independently of transcriptional regulation, and has a key role in the maintenance of blood glucose levels during a prolonged fast.
a–c, Liver Pc, Pepck and G6Pase mRNA expression (n = 5). d, e, Liver PC and PEPCK protein (n = 5, except for knockout + glucagon (n = 6)). f, g, Liver pACC/ACC and pAMPK/AMPK ratios (n = 5). Blots in f, g and Figs. 1f, 2a, Extended Data Figs. 1b, c, e, 4a were stripped and reprobed for all proteins of interest. h, Plasma NEFA (n = 5, except for knockout + glucagon (n = 6)). i, Liver malonyl-CoA (n = 6). j–l, Plasma glucose, insulin and glucagon concentrations in mice fasted for 48 h (n = 5). m–o, Liver long-chain-, acetyl- and malonyl-CoA content (n = 5). In all panels, genotypes and groups ± glucagon were compared using a two-tailed unpaired Student’s t-test. If no statistical comparison is denoted, the groups were not significantly different. In all panels, mean ± s.e.m. is shown. All n values refer to numbers of mice.
Extended Data Fig. 4 Glucagon acutely stimulates gluconeogenesis by activating intrahepatic, but not white adipose tissue, lipolysis.
a, Liver HSL phosphorylation (n = 5). These blots, and blots in Figs. 1f, 2a, Extended Data Figs. 1b, c, e, 3f, g, were stripped and reprobed for all proteins of interest. In a–c, groups were compared using a two-tailed unpaired Student’s t-test. b, c, In vitro NEFA (n = 14 wild type and 15 knockout) and glycerol production (n = 5 wild type and 6 knockout) from isolated hepatocytes. d, Plasma NEFA concentrations in mice treated with somatostatin, replacement basal insulin and glucagon (n = 6 wild type and 7 knockout). No significant differences were observed between genotypes using a two-tailed unpaired Student t-test, or before versus after glucagon treatment using a two-tailed paired Student’s t-test. e, f, NEFA production and VPC in isolated hepatocytes incubated in the ATGL inhibitor atglistatin (n = 6). g–n, NEFA production from isolated hepatocytes treated with ET-18-OCH3 (n = 3), U-73122 (n = 3), H-89 (n = 6), vasopressin (n = 3), KN-93 (n = 6), 2-APB (n = 3), caffeine (n = 3) and thapsigargin (n = 3). In all panels, *P < 0.05, **P < 0.01 and ***P < 0.001 versus the same genotype − glucagon − drug; §P < 0.05, §§ P < 0.01 and §§§ P < 0.001 versus the same genotype + glucagon − drug by two-tailed unpaired Student’s t-test. If no statistical comparison is denoted, the groups were not significantly different. Error bars represent s.e.m. All n values refer to numbers of mice.
Extended Data Fig. 5 Glucagon requires INSP3-mediated intrahepatic lipolysis to promote VPC and hepatic gluconeogenesis.
a, Body weight in mice treated with an adeno-associated virus to knock down liver Atgl (n = 6). b, Representative western blots. Blots from the same tissue (liver or white adipose tissue (WAT)) were stripped and reprobed for all proteins shown. c, White adipose tissue and liver ATGL protein expression. In c–e, n = 6, except for wild type + Atgl knockdown and knockout (n = 4). d, e, Hepatic PC and PEPCK protein expression. f–h, Plasma glucagon (n = 6, except for wild type + Atgl knockdown (n = 5), NEFA (n = 6, except for wild type + Atgl knockdown and knockout (n = 5), and glycerol concentrations (n = 6, except for wild type + Atgl knockdown (n = 5) in mice treated with an adeno-associated virus to knock down ATGL in a liver-specific manner. Groups were compared before and after glucagon treatment by two-tailed unpaired Student’s t-test. i, j, Liver glycogen and malonyl-CoA content (n = 6, except for wild type + ATGL knockdown (n = 5)). All comparisons were performed using a two-tailed unpaired Student’s t-test, unless otherwise stated. If no statistical comparison is denoted, the groups were not significantly different. Error bars represent s.e.m. All n values refer to numbers of mice.
Extended Data Fig. 6 Glucagon stimulates mitochondrial oxidation through hepatocellular calcium signalling.
a, Representative mitochondrial response to glucagon, which was added where denoted by the ‘glucagon’ bar. b, Maximum mitochondrial response to glucagon (n = 324 wild type and 167 knockout). Groups in b, d, f and h were compared by two-tailed unpaired Student’s t-test. c, Representative cytosolic response to glucagon. d, Maximum cytosolic response to glucagon (n = 146 wild type and 175 knockout). e, Representative mitochondrial response to the INSP3R agonist vasopressin. f, Amplitude of the mitochondrial response to vasopressin (n = 73 wild type and 42 knockout). g, Representative cytosolic response to vasopressin. h, Amplitude of the cytosolic response to vasopressin (n = 119 wild type and 53 knockout). i, Representative mitochondrial responses to glucagon (added where denoted by the bar) in wild-type hepatocytes incubated in the PKA inhibitor H-89 or the PLC inhibitor U-73122. j, Amplitude of the mitochondrial response (n = 79 control, 39 H-89 and 127 U-73122). Groups were compared to the control in j, l, m using a two-tailed unpaired Student’s t-test. k, Representative cytosolic responses to glucagon ± H-89 or U-73122. l, Amplitude of the cytosolic response (n = 182 control, 27 H-89 and 187 U-73122). m, Percentage of cells with a cytosolic response (>110% baseline) to glucagon ± H-89 or U-73122 (n = 11 control, 8 H-89 and 3 U-73122). n, o, Hepatic VPDH and VPK in vivo (n = 5 wild type − glucagon, 6 wild type + glucagon, 6 knockout − glucagon and 5 knockout + glucagon). In n, o, groups were compared (with versus without glucagon treament, and wild type versus knockout) using a two-tailed unpaired Student’s t-test. p, Liver VCS in mice infused with somatostatin, basal insulin and glucagon (n = 5). q, In vitro oxygen consumption in isolated hepatocytes incubated ± 100 nM glucagon (n = 113 wild type − glucagon, 144 knockout − glucagon, 149 wild type + glucagon and 210 knockout + glucagon). r, Liver triglyceride content (without glucagon infusion) (n = 11). If no statistical comparison is denoted, the groups were not significantly different. Error bars represent s.e.m. All n values refer to numbers of mice.
Extended Data Fig. 7 Chronic increases in mitochondrial oxidation with a ten-day glucagon infusion lead to reversal of nonalcoholic fatty liver disease and improvements in glucose tolerance.
a, Plasma glucagon concentrations on the last day of infusion (n = 6 in a–g). b, Hepatic VCS. In b–g, measurements were performed while the glucagon infusion continued. c, d, VPC/VEGP and VPC/VCS ratios. e–g, Hepatic VPDH, VFAO and VPK. h, Food intake during the glucagon infusion (n = 8 control and 10 glucagon), determined twice during the ten-day infusion (on day 4 and day 9) by weighing the food in the cage; the data points are the averages of the two food-intake measurements for each rat. i, Body weight after ten days of glucagon or saline infusion (n = 6). j, k, Plasma glucose and insulin concentrations (n = 6) measured two hours after cessation of the glucagon infusion, after a six-hour fast. l–n, Liver TAG (n = 6), DAG (n = 8) and ceramide (n = 8) concentrations. In a–k, n = 6. o, Hepatic PKCε translocation (n = 6 control and 7 glucagon). p–r, Liver glycogen (n = 6), acetyl-CoA (n = 8) and malonyl-CoA content (n = 8). s, t, Plasma glucose concentrations and area under the curve (AUC) during an intraperitoneal glucose tolerance test, which began two hours after completing a ten-day continuous infusion of glucagon or saline (n = 6). In s, u, *P < 0.05, **P < 0.01, ***P < 0.001. Data are mean ± s.e.m. u, v, Plasma insulin and insulin area under the curve during the glucose tolerance test. In all panels, error bars represent s.e.m, and groups were compared using a two-tailed unpaired Student’s t-test. If no statistical comparison is denoted, the groups are not significantly different. All n values refer to numbers of rats.
Extended Data Fig. 8 Chronic glucagon treatment reverses nonalcoholic fatty liver disease and glucose intolerance in wild-type, but not Insp3r1-knockout, mice.
a, Body weight (n = 10 wild type − glucagon, 11 wild type + glucagon, 8 knockout − glucagon and 8 knockout + glucagon). b, c, Food and water intake. In b–g, n = 8 wild type − glucagon, 9 wild type + glucagon, 7 knockout − glucagon and 8 knockout + glucagon. d, Energy expenditure. e, f, Oxygen consumption and carbon dioxide production. g, Activity. h, Plasma NEFA. In h–j, n = 10 wild type − glucagon, 11 wild type + glucagon, 8 knockout − glucagon and 8 knockout + glucagon. i, j, Glucose and insulin area under the curve during an intraperitoneal glucose tolerance test. In all panels, mean ± s.e.m. is shown. Statistical comparisons were performed using a two-tailed unpaired Student’s t-test. If no statistical comparison is denoted, the groups were not significantly different. All n values refer to numbers of mice.
Extended Data Fig. 9 Schematic summary.
Mechanism by which glucagon acutely stimulates intrahepatic lipolysis, hepatic gluconeogenesis and hepatic mitochondrial oxidation.
Supplementary information
Supplementary Figures
This file contains uncropped gel blot scans.
Supplementary Tables
This file contains Supplementary Tables 1-6 in PDF format.
Supplementary Tables
This file contains Supplementary Tables 1-6 in Excel format.
Source data
Rights and permissions
About this article
Cite this article
Perry, R.J., Zhang, D., Guerra, M.T. et al. Glucagon stimulates gluconeogenesis by INSP3R1-mediated hepatic lipolysis. Nature 579, 279–283 (2020). https://doi.org/10.1038/s41586-020-2074-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41586-020-2074-6
This article is cited by
-
Glucose controls lipolysis through Golgi PtdIns4P-mediated regulation of ATGL
Nature Cell Biology (2024)
-
Advances in the clinical measurement of glucagon: from diagnosis to therapy
Diabetology International (2024)
-
Metabolic Messengers: glucagon
Nature Metabolism (2023)
-
Famsin, a novel gut-secreted hormone, contributes to metabolic adaptations to fasting via binding to its receptor OLFR796
Cell Research (2023)
-
Hepatic p38α MAPK controls gluconeogenesis via FOXO1 phosphorylation at S273 during glucagon signalling in mice
Diabetologia (2023)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.