Abstract
Cytokine release syndrome (CRS) is a life-threatening complication of several new immunotherapies used to treat cancers and autoimmune diseases1,2,3,4,5. Here we report that atrial natriuretic peptide can protect mice from CRS induced by such agents by reducing the levels of circulating catecholamines. Catecholamines were found to orchestrate an immunodysregulation resulting from oncolytic bacteria and lipopolysaccharide through a self-amplifying loop in macrophages. Myeloid-specific deletion of tyrosine hydroxylase inhibited this circuit. Cytokine release induced by T-cell-activating therapeutic agents was also accompanied by a catecholamine surge and inhibition of catecholamine synthesis reduced cytokine release in vitro and in mice. Pharmacologic catecholamine blockade with metyrosine protected mice from lethal complications of CRS resulting from infections and various biotherapeutic agents including oncolytic bacteria, T-cell-targeting antibodies and CAR-T cells. Our study identifies catecholamines as an essential component of the cytokine release that can be modulated by specific blockers without impairing the therapeutic response.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$29.99 / 30 days
cancel any time
Subscribe to this journal
Receive 51 print issues and online access
$199.00 per year
only $3.90 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout





Similar content being viewed by others
Data availability
Source Data are provided for Figs. 1a, 2c, 3c, 4c, 5b and Extended Data Figs. 1a, 2a, b, 3a, b, 5a, 6a, 7a, 7d, 9h and 10d. The remaining datasets generated during this study are available from the corresponding authors on reasonable request. Unique materials such as the C. novyi strains are available on request to the corresponding authors. The transgenic mouse models and mouse CART constructs used in the study are made available through the original publishing authors.
References
van der Poll, T., van de Veerdonk, F. L., Scicluna, B. P. & Netea, M. G. The immunopathology of sepsis and potential therapeutic targets. Nat. Rev. Immunol. 17, 407–420 (2017).
Hansel, T. T., Kropshofer, H., Singer, T., Mitchell, J. A. & George, A. J. The safety and side effects of monoclonal antibodies. Nat. Rev. Drug Discov. 9, 325–338 (2010).
Rommelfanger, D. M. et al. The efficacy versus toxicity profile of combination virotherapy and TLR immunotherapy highlights the danger of administering TLR agonists to oncolytic virus-treated mice. Mol. Ther. 21, 348–357 (2013).
Maude, S. L., Barrett, D., Teachey, D. T. & Grupp, S. A. Managing cytokine release syndrome associated with novel T cell-engaging therapies. Cancer J. 20, 119–122 (2014).
Parker, B. S., Rautela, J. & Hertzog, P. J. Antitumour actions of interferons: implications for cancer therapy. Nat. Rev. Cancer 16, 131–144 (2016).
Agrawal, N. et al. Bacteriolytic therapy can generate a potent immune response against experimental tumors. Proc. Natl Acad. Sci. USA 101, 15172–15177 (2004).
Peters van Ton, A. M., Kox, M., Abdo, W. F. & Pickkers, P. Precision immunotherapy for sepsis. Front. Immunol. 9, 1926 (2018).
Weber, G. F. et al. Interleukin-3 amplifies acute inflammation and is a potential therapeutic target in sepsis. Science 347, 1260–1265 (2015).
Vollmar, A. M. The role of atrial natriuretic peptide in the immune system. Peptides 26, 1086–1094 (2005).
Kuehne, S. A. & Minton, N. P. ClosTron-mediated engineering of Clostridium. Bioengineered 3, 247–254 (2012).
Burke, J. R. et al. BMS-345541 is a highly selective inhibitor of I kappa B kinase that binds at an allosteric site of the enzyme and blocks NF-kappa B-dependent transcription in mice. J. Biol. Chem. 278, 1450–1456 (2003).
Johnson, J. D. et al. Catecholamines mediate stress-induced increases in peripheral and central inflammatory cytokines. Neuroscience 135, 1295–1307 (2005).
Flierl, M. A. et al. Phagocyte-derived catecholamines enhance acute inflammatory injury. Nature 449, 721–725 (2007).
Shaked, I. et al. Transcription factor Nr4a1 couples sympathetic and inflammatory cues in CNS-recruited macrophages to limit neuroinflammation. Nat. Immunol. 16, 1228–1234 (2015).
Clausen, B. E., Burkhardt, C., Reith, W., Renkawitz, R. & Förster, I. Conditional gene targeting in macrophages and granulocytes using LysMcre mice. Transgenic Res. 8, 265–277 (1999).
Zheng, J. H. et al. Two-step enhanced cancer immunotherapy with engineered Salmonella typhimurium secreting heterologous flagellin. Sci. Transl. Med. 9, eaak9537 (2017).
Surbatovic, M. et al. Cytokine profile in severe Gram-positive and Gram-negative abdominal sepsis. Sci. Rep. 5, 11355 (2015).
Sevmis, S. et al. OKT3 treatment for steroid-resistant acute rejection in kidney transplantation. Transplant. Proc. 37, 3016–3018 (2005).
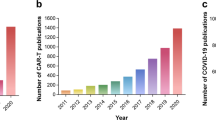
Neelapu, S. S. et al. Chimeric antigen receptor T-cell therapy - assessment and management of toxicities. Nat. Rev. Clin. Oncol. (2017).
Giavridis, T. et al. CAR T cell-induced cytokine release syndrome is mediated by macrophages and abated by IL-1 blockade. Nat. Med. 24, 731–738 (2018).
Norelli, M. et al. Monocyte-derived IL-1 and IL-6 are differentially required for cytokine-release syndrome and neurotoxicity due to CAR T cells. Nat. Med. 24, 739–748 (2018).
Gill, S. et al. Preclinical targeting of human acute myeloid leukemia and myeloablation using chimeric antigen receptor-modified T cells. Blood 123, 2343–2354 (2014).
Ninomiya, S. et al. Tumor indoleamine 2,3-dioxygenase (IDO) inhibits CD19-CAR T cells and is downregulated by lymphodepleting drugs. Blood 125, 3905–3916 (2015).
Wunderlich, M. et al. A xenograft model of macrophage activation syndrome amenable to anti-CD33 and anti-IL-6R treatment. JCI Insight 1, e88181 (2016).
Flierl, M. A. et al. Upregulation of phagocyte-derived catecholamines augments the acute inflammatory response. PLoS One 4, e4414 (2009).
Bao, J. Y., Huang, Y., Wang, F., Peng, Y. P. & Qiu, Y. H. Expression of α-AR subtypes in T lymphocytes and role of the α-ARs in mediating modulation of T cell function. Neuroimmunomodulation 14, 344–353 (2007).
Jackson, C. R. et al. Retinal dopamine mediates multiple dimensions of light-adapted vision. J. Neurosci. 32, 9359–9368 (2012).
Corrodi, H. & Hanson, L. C. Central effects of an inhibitor of tyrosine hydroxylation. Psychopharmacologia 10, 116–125 (1966).
Bettegowda, C. et al. The genome and transcriptomes of the anti-tumor agent Clostridium novyi-NT. Nat. Biotechnol. 24, 1573–1580 (2006).
Lofton, C. E., Newman, W. H. & Currie, M. G. Atrial natriuretic peptide regulation of endothelial permeability is mediated by cGMP. Biochem. Biophys. Res. Commun. 172, 793–799 (1990).
Zhang, X., Goncalves, R. & Mosser, D. M. The isolation and characterization of murine macrophages. Curr. Protoc. Immunol. https://doi.org/10.1002/0471142735.im1401s83 (2008).
Rittirsch, D., Flierl, M. A. & Ward, P. A. Harmful molecular mechanisms in sepsis. Nat. Rev. Immunol. 8, 776–787 (2008).
Berahovich, R. et al. FLAG-tagged CD19-specific CAR-T cells eliminate CD19-bearing solid tumor cells in vitro and in vivo. Front. Biosci. 22, 1644–1654 (2017).
Davila, M. L., Kloss, C. C., Gunset, G. & Sadelain, M. CD19 CAR-targeted T cells induce long-term remission and B cell aplasia in an immunocompetent mouse model of B cell acute lymphoblastic leukemia. PLoS One 8, e61338 (2013).
Lee, J., Sadelain, M. & Brentjens, R. Retroviral transduction of murine primary T lymphocytes. Methods Mol. Biol. 506, 83–96 (2009).
Acknowledgements
We thank N. Minton, C. Brayton, K. Kammers, D. Pardoll, Z. Li, E. Watson, C. Thoburn, S. Roy and N. Forbes-McBean for scientific and technical support. This work was supported by NINDS R25NS065729 (V.S.), NCI 1K08CA230179-01 (V.S.), Francis S. Collins Scholar Program (V.S.), DHART-SPORE IN4689861JHU (V.S.), 1R03CA178118-01A1 (R.-Y.B.), BVD (S.Z, R.-Y.B.), the Virginia and D.K. Ludwig Fund for Cancer Research (N.P., K.W.K., B.V., S.Z.), the BKI at Johns Hopkins, and CA062924 (S.Z.).
Reviewer information
Nature thanks K. Tracey and the anonymous reviewer(s) for their contribution to the peer review of this work.
Author information
Authors and Affiliations
Contributions
V.S. and R.-Y.B. originated the concept, designed and performed experiments, analysed the data and wrote the manuscript. K.K. and P.B.R. provided scientific advice. M.D. and M.L.D. provided animal models and scientific advice. B.V. and S.Z. designed the study, interpreted the data and wrote the manuscript. G.J.R., K.W.K. and N.P. contributed to the manuscript. All authors approved the final manuscript.
Corresponding authors
Ethics declarations
Competing interests
A patent application on CRS prevention listing V.S., R.-Y.B., G.J.R., K.W.K., N.P., S.Z. and B.V. as co-inventors has been provisionally filed by Johns Hopkins University. Under a licensing agreement between BVD Inc. and Johns Hopkins University, K.W.K., B.V. and S.Z. are entitled to a share of royalties managed by Johns Hopkins University. B.V., K.W.K. and NP are members of the Scientific Advisory Board of Sysmex and are founders of PapGene and Personal Genome Diagnostics. B.V. is also an advisor to Camden Partners. The terms of all these arrangements are managed by Johns Hopkins University in accordance with its conflict of interest policies. P.B.R. serves on Merck’s board of directors.
Additional information
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Extended data figures and tables
Extended Data Fig. 1 In vitro and in vivo studies of ANP-C. novyi-NT.
a, Kaplan–Meier curves of mice with large subcutaneous CT26 tumours (600–900 mm3), treated with 12 × 106 C. novyi-NT spores and the indicated agents: anti-IL-6R (n = 10), metronidazole (n = 5), dexamethasone (n = 6), anti-IL3 (n = 6) and anti-TNF (n = 5) injected intratumourally, compared to controls (n = 5). Survival differences were analysed by two-sided log-rank test. b and c, Selected clones of ANP-C. novyi-NT were analysed for ANP secretion, shown as the average of a triplicate, (b) and for cGMP induction (n = 3) using bovine aortic endothelial cells (c). d, Growth pattern of several clones compared to the parental C. novyi-NT. The average of a triplicate is shown. e–g, Levels of plasma ANP (left to right, n = 7, 8, 7, 5 independent samples per column) (e), plasma cGMP (n = 5, 5, 4, 4 samples per column) (f) and germinated C. novyi strains in tumour tissue (n = 4 samples per column) based on quantification cycle (Cq) from RT–PCR of germination-specific NT01CX1854 gene (g), measured at 36 h after spore injection. h, Representative haematoxylin and eosin as well as anti-CD11b antibody stained sections from the lungs, liver, spleen and bone marrow of mice treated with ANP-C. novyi-NT (n = 3), C. novyi-NT (n = 3) and C. novyi-NT plus ANP (n = 2) compared to normal controls (n = 2). i–m, Pulmonary permeability (n = 4 mice per group), lung wet–dry ratio (n = 3 mice per group) (i) as well as levels of cytokines (n = 6 independent samples per column) (j), dopamine (n = 3 independent samples per column) (k), haematocrit (n = 3, 5, 4, 4 samples per column) (l) and calculated plasma volume (n = 3, 5, 4, 4 samples per column) (m) measured 36 h after spore treatment. Data are presented as mean ± s.d. with individual data points shown, analysed by two-tailed t-test (c, e–g, i–m). BAEC, bovine aortic endothelial cells.
Extended Data Fig. 2 Survival of mice treated with ANP and IκB kinase inhibitor BMS345541.
a, Survival of mice with subcutaneously implanted GL-261 tumours, treated with 12 × 106 of ANP-C. novyi-NT spores (n = 10 animals per group). b, Survival of mice with CT26 tumours treated with C. novyi-NT and IκB kinase inhibitor BMS345541 (n = 5 mice per group). Survival differences were analysed by two-sided log-rank test (b, c).
Extended Data Fig. 3 Adrenaline enhances the inflammatory response.
a, Survival of BALB/c mice implanted with the indicated catecholamine pump and stimulated with a sublethal dose of LPS (n = 14 mice per group) compared to LPS alone (n = 19 mice). Survival differences were analysed by Gehan–Breslow–Wilcoxon test. b, Survival of BALB/c mice with indicated catecholamine pump without LPS stimulation (n = 5 mice per group). c, d, 24 h plasma levels of adrenaline (left to right, n = 3, 4, 3, 3, 3, 4, 4, 3 per column), noradrenaline (n = 3, 3, 3, 3, 3, 4, 4, 3) and dopamine (n = 3, 3, 3, 3, 3, 4, 4, 3) (c) as well as levels of IL-6 (n = 4 per column), TNF (n = 5 per column) and KC (n = 4 per column) (d) in mice receiving the indicated treatments. e, Dopamine concentration in LPS- and adrenaline-treated peritoneal macrophages pre-incubated with ANP or MTR (n = 3 per column), measured after 24 h. f, g, Levels of catecholamines (n = 3 independent samples per column) (f) and several cytokines (n = 3 independent samples per column) (g) in adrenaline (15 ng ml–1)-treated peritoneal macrophages pre-incubated with ANP or MTR and measured after 24 h. Data are presented as mean ± s.d. with individual data points shown, analysed by two-tailed t-test (c–g).
Extended Data Fig. 4 Catecholamines modulate the cytokine release in macrophages in vitro.
a, b, Human U937 macrophage-like cells were pre-treated with ANP or MTR for 10 min, then stimulated with LPS at 1 µg ml–1 and/or adrenaline at 15 ng ml–1. Culture supernatants were analysed for catecholamines (n = 3 per column) (a) as well as the indicated cytokines (n = 3 per column) (b). c, TH expression of baseline and LPS-stimulated Th+/+ or ThΔLysM macrophages (n = 3 per group), analysed by RT–PCR; results are normalized to ubiquitin C (UBC) expression. d, e, Supernatants of collected peritoneal macrophages from Th+/+ or ThΔLysM mice, stimulated with LPS at 50 µg ml–1, adrenaline 15 µg ml–1 or both for 24 h, were analysed for levels of adrenaline (n = 3), noradrenaline (n = 3) (d) and cytokines IL-6 (n = 3), KC (n = 3), MIP-2 (n = 3) and TNF (n = 3) (e). All data are presented as mean ± s.d. with individual data points shown, analysed by two-tailed t-test.
Extended Data Fig. 5 Modulation of catecholamine synthesis by MTR dose-dependently determines survival and cytokine release.
a, Survival of BALB/c mice stimulated with a lethal dose of LPS and treated with the indicated dose of MTR: MTR 20 mg kg–1 (n = 5 mice per group); MTR 30 mg kg–1 (n = 10 mice), MTR 40 mg kg–1 (n = 12) compared to LPS (n = 10 mice). Survival differences were analysed by two-sided log-rank test. b, c, Levels of plasma catecholamines (n = 4 per column) (b) and IL-6 (n = 4 per column), KC (left to right, n = 4, 4, 3 per column), IFN-γ (n = 4) and TNF (n = 4, 4, 3) (c) at different MTR doses measured 24 h after LPS injection. d, e, 24-h-time course of circulating adrenaline (n = 5, 5, 5, 4, 5, 4, 5, 5), noradrenaline (n = 5) and dopamine (n = 5) (d) and corresponding levels of IL-6 (n = 4), KC (n = 7, 7, 7, 6, 5, 4, 5, 5), IFN-γ (n = 6, 6, 6, 8, 4, 8, 6, 4) and TNF (n = 6, 6, 6, 6, 6, 4, 7, 7) (e) in LPS-treated mice receiving MTR 40 mg kg–1. Data are presented as mean ± s.d. with individual data points shown, analysed by two-tailed t-test (b–e).
Extended Data Fig. 6 Blockage of α1-adrenoceptor mediates the survival in experimental systemic inflammatory syndrome.
a, Kaplan–Meier curve of LPS-injected BALB/c mice treated with the indicated adrenoreceptor blockers (n = 15 animals per group). Survival differences were analysed by two-sided log-rank test. b, c, Levels of adrenaline, noradrenaline (left to right, n = 3, 5, 8 per column) and dopamine (n = 5, 4, 7) (b) as well as indicated cytokines (n = 3, 5, 8) (c) measured 24 h after LPS administration. Data are presented as mean ± s.d. with individual data points shown, analysed by two-tailed t-test (b, c).
Extended Data Fig. 7 Suppression of catecholamines with MTR reduces toxicity of oncolytic bacterium C. novyi-NT and polymicrobial sepsis.
a, Survival (top panel) and therapeutic response (bottom panel) of CT26 tumour-bearing BALB/c mice undergoing C. novyi-NT treatment with or without MTR pre-treatment (n = 13 mice per group). Survival differences were analysed with two-sided log-rank test. b, c, Corresponding plasma levels of adrenaline (n = 3 independent samples per column), noradrenaline (n = 3), dopamine (n = 3) (b) and indicated cytokines (left to right, n = 3, 3, 6, 7 independent samples per column) (c), measured at baseline and 36 h after treatment. d, Survival of C57Bl/6 mice undergoing CLP, with the indicated treatments (CLP, n = 20 mice; MTR, n = 22; imipenem, n = 19; MTR + imipenem, n = 20 mice per group). Survival differences were analysed with two-sided log-rank test. e, Plasma levels of adrenaline (n = 3), noradrenaline (n = 3) and dopamine (n = 3) at the indicated time points after CLP, with or without MTR pre-treatment. f, Levels of indicated cytokines (n = 3) at baseline and 24 h after CLP, with or without MTR pre-treatment. g, h, Levels of plasma dopamine (left to right, n = 3, 8, 8 independent samples per column) (g) and KC (n = 6, 6, 6, 5), IL-2 (n = 6, 6, 6, 5) and IFN-γ (n = 6) (h) measured 24 h after α-CD3 treatment, with or without MTR. Data are presented as mean ± s.d. with individual data points shown, analysed by two-tailed t-test (b, c, e–h).
Extended Data Fig. 8 Adrenaline stimulates cytokine release during hCART19–Raji cell interaction in vitro.
a, Levels of catecholamines measured individually in supernatants of Raji cells (n = 3), hCART19 (n = 3) and UT-T (n = 3 per column) at baseline and when exposed to adrenaline. b, c, Co-cultures of hCART19 and Raji with or without MTR or ANP pre-treatment were stimulated with 15 ng ml–1 of adrenaline. Culture supernatants were collected after 24 h and analysed for adrenaline (left to right, n = 4, 4, 4, 3, 3, 3, 2, 2 per column) and noradrenaline (n = 4, 4, 3, 3, 3, 3, 2, 2). Adrenaline (old): adrenaline at 15 ng ml–1 was incubated at 37 °C for 24 h in the cell-free medium. Adrenaline (new): adrenaline at 15 ng ml–1 was added into the cell-free medium and immediately measured (b). Corresponding cytokine levels of MIP-1α (n = 4, 4, 3, 4, 3, 3, 3, 3, 3), IFN-γ (n = 4, 4, 3, 4, 3, 4, 4, 4, 4), IL-2 (n = 4, 4, 3, 4, 3, 3, 3, 3, 3) and TNF (n = 4, 4, 3, 4, 3, 3, 3, 3, 3) (c). UT-T served as control. d, e, As above, co-cultures of hCART19 and Raji with or without CHX were stimulated with 15 ng ml–1 of adrenaline in vitro. Levels of catecholamines (n = 3, 3, 3, 3, 3, 3, 3, 3, 3, 3, 3, 3, 1, 1) (d) and indicated human cytokines (n = 3) (e) were measured after 24 h. Data are presented as mean ± s.d. with individual data points shown, analysed by two-tailed t-test.
Extended Data Fig. 9 MTR and ANP prevent cytokine release in Raji/hCART19 mouse model.
a, Bioluminescent images (BLI) of Raji-bearing NSGS mice with high tumour burden. At day 0, tumour engraftment was quantified by BLI and mice were assigned to the treatment groups (untreated, MTR, hCART19, hCART19+MTR, n = 5 mice per group; UT-T, n = 4). b, c, Levels of dopamine (left to right, n = 3, 3, 3, 4, 4, 4, 3, 4, 4, 4 per column) (b) and indicated cytokines (n = 4) (c) measured in mice (with high tumour burden) 24 and 72 h after hCART19 and UT-T injection. d, BLI of Raji-bearing NSGS mice with low tumour burden. At day 0, mice were randomly assigned based on tumour burden to receive hCART19, with or without MTR (n = 10 mice per group) or UT-T, with or without MTR (n = 5 mice per group). e, Levels of HsIL-2 (n = 4, 4, 3) and MmMIP-2 (n = 3, 3, 4) assessed 72 h after hCART19 injection in mice with low tumour burden. f, g, NSGS mice were injected with hCART19 4 days after Raji implantation and treated with ANP delivered via subcutaneously implanted osmotic pumps. Levels of circulating catecholamines (n = 4 per column) (f) and MmIL-6, MmKC and MmMIP-2 (n = 4, 4, 3, 4) as well as HsIL-2 (n = 4) (g) were assessed 24 h after hCART19 administration. h, Survival of Raji cell-bearing NSGS mice treated with hCART19 and ANP (n = 5 per group); analysed by two-sided log-rank test. i, Level of circulating hCART19 10 days after treatment, determined by Cq from RT–PCR and analysed in triplicates (n = 4 per group). Data are presented as mean ± s.d. with individual data points shown, analysed by two-tailed t-test (b, c, e–i).
Extended Data Fig. 10 MTR and ANP prevent cytokine release in syngeneic Eμ-ALL model without compromising anti-tumour efficacy.
a, b, Circulating catecholamines (left to right, n = 3, 4, 3, 4, 4, 4, 3, 4, 3, 4, 4, 4 per column/graph) (a) and murine cytokines IL-6 (n = 3 per column), KC (n = 3, 3, 3, 4, 3, 3, 4, 4, 3 per column), IL-1a (n = 3, 3, 3, 4, 3, 3, 4, 3, 3 per column) and G-CSF (n = 3, 3, 3, 4, 4, 3, 4, 3, 3 per column) (b), assessed at 24 and 72 h after mCART19 injection. Data are presented as means ± s.d. with individual data points shown, analysed by two-tailed t-test. c, BLI was performed before and 10 days after mCART19 cell injection, with or without ANP and MTR pre-treatment (n = 5 animals per group). BLI radiance was used to quantify the tumour burden during the treatment course (right). d, Percentage survival of Eμ-ALL-mice after mCART19 cell transfer (n = 8 mice per group). Survival differences were analysed by two-sided log-rank test.
Supplementary information
Source data
Rights and permissions
About this article
Cite this article
Staedtke, V., Bai, RY., Kim, K. et al. Disruption of a self-amplifying catecholamine loop reduces cytokine release syndrome. Nature 564, 273–277 (2018). https://doi.org/10.1038/s41586-018-0774-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41586-018-0774-y
Keywords
This article is cited by
-
The cancer-immune dialogue in the context of stress
Nature Reviews Immunology (2024)
-
CAR-cell therapy in the era of solid tumor treatment: current challenges and emerging therapeutic advances
Molecular Cancer (2023)
-
Insights gained from single-cell analysis of chimeric antigen receptor T-cell immunotherapy in cancer
Military Medical Research (2023)
-
Dynamic RBM47 ISGylation confers broad immunoprotection against lung injury and tumorigenesis via TSC22D3 downregulation
Cell Death Discovery (2023)
-
Suppression of cytokine release syndrome during CAR-T-cell therapy via a subcutaneously injected interleukin-6-adsorbing hydrogel
Nature Biomedical Engineering (2023)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.