Abstract
Congenital anomalies of the kidney and urinary tract (CAKUTs) represent the leading cause of chronic kidney disease and end-stage kidney disease in children. Increasing evidence points to critical roles for the urothelium in the developing urinary tract and in the genesis of CAKUTs. The involvement of the urothelium in patterning the urinary tract is supported by evidence that CAKUTs can arise as a result of abnormal urothelial development. Emerging evidence indicates that congenital urinary tract obstruction triggers urothelial remodelling that stabilizes the obstructed kidney and limits renal injury. Finally, the diagnostic potential of radiological findings and urinary biomarkers derived from the urothelium of patients with CAKUTs might aid their contribution to clinical care.
Key points
Interactions between the developing urothelium and its underlying mesenchyme serve critical roles in developmental patterning of the bladder and ureter.
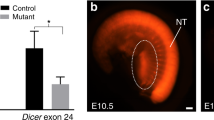
Genetic disruption of signalling pathways that mediate terminal differentiation of urothelium and urothelial–mesenchymal interactions results in phenotypes of congenital abnormalities of the urinary tract in humans and mice.
The urothelial plaque serves a critical protective role in response to congenital urinary tract obstruction.
Urothelium-specific radiological and biochemical markers represent potential means of detecting congenital abnormalities of the urinary tract, but prospective studies are warranted to evaluate their diagnostic accuracy.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$29.99 / 30 days
cancel any time
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
References
Murugapoopathy, V. & Gupta, I. R. A primer on congenital anomalies of the kidneys and urinary tracts (CAKUT). Clin. J. Am. Soc. Nephrol. 15, 723–731 (2020).
Sanna-Cherchi, S., Westland, R., Ghiggeri, G. M. & Gharavi, A. G. Genetic basis of human congenital anomalies of the kidney and urinary tract. J. Clin. Invest. 128, 4–15 (2018).
BDMP/CPHA. Birth Defects Monitoring Program (BDMP)/Commission on Professional and Hospital Activities (CPHA) surveillance data, 1988–1991. Teratology 48, 658–675 (1993).
Garne, E., Dolk, H., Loane, M., Boyd, P. A. & Eurocat EUROCAT website data on prenatal detection rates of congenital anomalies. J. Med. Screen. 17, 97–98 (2010).
MACDP. Metropolitan Atlanta Congenital Defects Program surveillance data, 1988–1991. Teratology 48, 695–709 (1993).
Schulman, J., Edmonds, L. D., McClearn, A. B., Jensvold, N. & Shaw, G. M. Surveillance for and comparison of birth defect prevalences in two geographic areas — United States, 1983–88. MMWR CDC Surveill. Summ. 42, 1–7 (1993).
Postoev, V. A. et al. Congenital anomalies of the kidney and the urinary tract: a Murmansk county birth registry study. Birth Defects Res. A Clin. Mol. Teratol. 106, 185–193 (2016).
Tain, Y. L., Luh, H., Lin, C. Y. & Hsu, C. N. Incidence and risks of congenital anomalies of kidney and urinary tract in newborns: a population-based case-control study in Taiwan. Medicine 95, e2659 (2016).
Harambat, J., van Stralen, K. J., Kim, J. J. & Tizard, E. J. Epidemiology of chronic kidney disease in children. Pediatr. Nephrol. 27, 363–373 (2012).
Sanna-Cherchi, S. et al. Renal outcome in patients with congenital anomalies of the kidney and urinary tract. Kidney Int. 76, 528–533 (2009).
Wuhl, E. et al. Timing and outcome of renal replacement therapy in patients with congenital malformations of the kidney and urinary tract. Clin. J. Am. Soc. Nephrol. 8, 67–74 (2013).
Calderon-Margalit, R. et al. History of childhood kidney disease and risk of adult end-stage renal disease. N. Engl. J. Med. 378, 428–438 (2018).
Chesnaye, N. et al. Demographics of paediatric renal replacement therapy in Europe: a report of the ESPN/ERA-EDTA registry. Pediatr. Nephrol. 29, 2403–2410 (2014).
van der Ven, A. T., Vivante, A. & Hildebrandt, F. Novel insights into the pathogenesis of monogenic congenital anomalies of the kidney and urinary tract. J. Am. Soc. Nephrol. 29, 36–50 (2018).
Hsu, C. W., Yamamoto, K. T., Henry, R. K., De Roos, A. J. & Flynn, J. T. Prenatal risk factors for childhood CKD. J. Am. Soc. Nephrol. 25, 2105–2111 (2014).
Dart, A. B., Ruth, C. A., Sellers, E. A., Au, W. & Dean, H. J. Maternal diabetes mellitus and congenital anomalies of the kidney and urinary tract (CAKUT) in the child. Am. J. Kidney Dis. 65, 684–691 (2015).
Parikh, C. R., McCall, D., Engelman, C. & Schrier, R. W. Congenital renal agenesis: case–control analysis of birth characteristics. Am. J. Kidney Dis. 39, 689–694 (2002).
Pryde, P. G., Sedman, A. B., Nugent, C. E. & Barr, M. Jr. Angiotensin-converting enzyme inhibitor fetopathy. J. Am. Soc. Nephrol. 3, 1575–1582 (1993).
Wu, X. R., Kong, X. P., Pellicer, A., Kreibich, G. & Sun, T. T. Uroplakins in urothelial biology, function, and disease. Kidney Int. 75, 1153–1165 (2009).
Acharya, P. et al. Distribution of the tight junction proteins ZO-1, occludin, and claudin-4, -8, and -12 in bladder epithelium. Am. J. Physiol. Renal Physiol. 287, F305–F318 (2004).
Lavelle, J. et al. Bladder permeability barrier: recovery from selective injury of surface epithelial cells. Am. J. Physiol. Renal Physiol. 283, F242–F253 (2002).
Smith, N. J. et al. The human urothelial tight junction: claudin 3 and the ZO-1α+ switch. Bladder 2, e9 (2015).
Hu, P. et al. Role of membrane proteins in permeability barrier function: uroplakin ablation elevates urothelial permeability. Am. J. Physiol. Renal Physiol. 283, F1200–F1207 (2002).
Mathai, J. C. et al. Hypercompliant apical membranes of bladder umbrella cells. Biophys. J. 107, 1273–1279 (2014).
Truschel, S. T. et al. Stretch-regulated exocytosis/endocytosis in bladder umbrella cells. Mol. Biol. Cell 13, 830–846 (2002).
Merrill, L., Gonzalez, E. J., Girard, B. M. & Vizzard, M. A. Receptors, channels, and signalling in the urothelial sensory system in the bladder. Nat. Rev. Urol. 13, 193–204 (2016).
Bohnenpoll, T. et al. Diversification of cell lineages in ureter development. J. Am. Soc. Nephrol. 28, 1792–1801 (2017).
Jackson, A. R. et al. Krt5+ urothelial cells are developmental and tissue repair progenitors in the kidney. Am. J. Physiol. Renal Physiol. 317, F757–F766 (2019).
Schoenwolf, G. C., Bleyl, S. B., Brauer, P. R. & Francis-West, P. H. Larsen’s Human Embryology 5th edn (Elsevier/Churchill Livingstone, 2015).
Gandhi, D. et al. Retinoid signaling in progenitors controls specification and regeneration of the urothelium. Dev. Cell 26, 469–482 (2013).
Mysorekar, I. U., Isaacson-Schmid, M., Walker, J. N., Mills, J. C. & Hultgren, S. J. Bone morphogenetic protein 4 signaling regulates epithelial renewal in the urinary tract in response to uropathogenic infection. Cell Host Microbe 5, 463–475 (2009).
Tash, J. A., David, S. G., Vaughan, E. E. & Herzlinger, D. A. Fibroblast growth factor-7 regulates stratification of the bladder urothelium. J. Urol. 166, 2536–2541 (2001).
Papafotiou, G. et al. KRT14 marks a subpopulation of bladder basal cells with pivotal role in regeneration and tumorigenesis. Nat. Commun. 7, 11914 (2016).
Faa, G. et al. Morphogenesis and molecular mechanisms involved in human kidney development. J. Cell. Physiol. 227, 1257–1268 (2012).
Michos, O. Kidney development: from ureteric bud formation to branching morphogenesis. Curr. Opin. Genet. Dev. 19, 484–490 (2009).
Baskin, L. S., Hayward, S. W., Young, P. & Cunha, G. R. Role of mesenchymal-epithelial interactions in normal bladder development. J. Urol. 156, 1820–1827 (1996).
Cao, M., Liu, B., Cunha, G. & Baskin, L. Urothelium patterns bladder smooth muscle location. Pediatr. Res. 64, 352–357 (2008).
Shiroyanagi, Y. et al. Urothelial sonic hedgehog signaling plays an important role in bladder smooth muscle formation. Differentiation 75, 968–977 (2007).
Jenkins, D., Winyard, P. J. & Woolf, A. S. Immunohistochemical analysis of Sonic hedgehog signalling in normal human urinary tract development. J. Anat. 211, 620–629 (2007).
Cao, M. et al. Urothelium-derived Sonic hedgehog promotes mesenchymal proliferation and induces bladder smooth muscle differentiation. Differentiation 9, 244–250 (2010).
DeSouza, K. R., Saha, M., Carpenter, A. R., Scott, M. & McHugh, K. M. Analysis of the Sonic Hedgehog signaling pathway in normal and abnormal bladder development. PLoS One 8, e53675 (2013).
Cheng, W. et al. Sonic Hedgehog mediator Gli2 regulates bladder mesenchymal patterning. J. Urol. 180, 1543–1550 (2008).
Yu, J., Carroll, T. J. & McMahon, A. P. Sonic hedgehog regulates proliferation and differentiation of mesenchymal cells in the mouse metanephric kidney. Development 129, 5301–5312 (2002).
Bohnenpoll, T. et al. A SHH-FOXF1-BMP4 signaling axis regulating growth and differentiation of epithelial and mesenchymal tissues in ureter development. PLoS Genet. 13, e1006951 (2017).
Mamo, T. M. et al. BMP4 uses several different effector pathways to regulate proliferation and differentiation in the epithelial and mesenchymal tissue compartments of the developing mouse ureter. Hum. Mol. Genet. 26, 3553–3563 (2017).
Cain, J. E., Islam, E., Haxho, F., Blake, J. & Rosenblum, N. D. GLI3 repressor controls functional development of the mouse ureter. J. Clin. Invest. 121, 1199–1206 (2011).
David, S. G., Cebrian, C., Vaughan, E. D. Jr & Herzlinger, D. c-kit and ureteral peristalsis. J. Urol. 173, 292–295 (2005).
Iskander, S. M., Feeney, M. M., Yee, K. & Rosenblum, N. D. Protein kinase 2β is expressed in neural crest-derived urinary pacemaker cells and required for pyeloureteric contraction. J. Am. Soc. Nephrol. 29, 1198–1209 (2018).
Feeney, M. M. & Rosenblum, N. D. Urinary tract pacemaker cells: current knowledge and insights from nonrenal pacemaker cells provide a basis for future discovery. Pediatr. Nephrol. 29, 629–635 (2014).
Sheybani-Deloui, S. et al. Activated hedgehog-GLI signaling causes congenital ureteropelvic junction obstruction. J. Am. Soc. Nephrol. 29, 532–544 (2018).
Trowe, M. O. et al. Canonical Wnt signaling regulates smooth muscle precursor development in the mouse ureter. Development 139, 3099–3108 (2012).
Aydogdu, N. et al. TBX2 and TBX3 act downstream of canonical WNT signaling in patterning and differentiation of the mouse ureteric mesenchyme. Development 145, dev171827 (2018).
Zupancic, D. & Romih, R. Heterogeneity of uroplakin localization in human normal urothelium, papilloma and papillary carcinoma. Radiol. Oncol. 47, 338–345 (2013).
Jenkins, D. et al. De novo uroplakin IIIa heterozygous mutations cause human renal adysplasia leading to severe kidney failure. J. Am. Soc. Nephrol. 16, 2141–2149 (2005).
Riedel, I. et al. Urothelial umbrella cells of human ureter are heterogeneous with respect to their uroplakin composition: different degrees of urothelial maturity in ureter and bladder? Eur. J. Cell Biol. 84, 393–405 (2005).
Haraguchi, R. et al. Molecular analysis of coordinated bladder and urogenital organ formation by Hedgehog signaling. Development 134, 525–533 (2007).
Haraguchi, R. et al. The hedgehog signal induced modulation of bone morphogenetic protein signaling: an essential signaling relay for urinary tract morphogenesis. PLoS One 7, e42245 (2012).
He, J. L. et al. Mutation screening of BMP4 and Id2 genes in Chinese patients with congenital ureteropelvic junction obstruction. Eur. J. Pediatr. 171, 451–456 (2012).
Reis, G. S. et al. Study of the association between the BMP4 gene and congenital anomalies of the kidney and urinary tract. J. Pediatr. 90, 58–64 (2014).
Weber, S. et al. SIX2 and BMP4 mutations associate with anomalous kidney development. J. Am. Soc. Nephrol. 19, 891–903 (2008).
Dubourg, C. et al. Molecular screening of SHH, ZIC2, SIX3, and TGIF genes in patients with features of holoprosencephaly spectrum: mutation review and genotype-phenotype correlations. Hum. Mutat. 24, 43–51 (2004).
Hilger, A. C. et al. Targeted resequencing of 29 candidate genes and mouse expression studies implicate ZIC3 and FOXF1 in human VATER/VACTERL association. Hum. Mutat. 36, 1150–1154 (2015).
van der Ven, A. T. et al. Whole-exome sequencing identifies causative mutations in families with congenital anomalies of the kidney and urinary tract. J. Am. Soc. Nephrol. 29, 2348–2361 (2018).
Kolvenbach, C. M. et al. Rare variants in BNC2 are implicated in autosomal-dominant congenital lower urinary-tract obstruction. Am. J. Hum. Genet. 104, 994–1006 (2019).
Bhoj, E. J. et al. Human balanced translocation and mouse gene inactivation implicate basonuclin 2 in distal urethral development. Eur. J. Hum. Genet. 19, 540–546 (2011).
Yang, A. et al. p63, a p53 homolog at 3q27-29, encodes multiple products with transactivating, death-inducing, and dominant-negative activities. Mol. Cell 2, 305–316 (1998).
Cheng, W. et al. DeltaNp63 plays an anti-apoptotic role in ventral bladder development. Development 133, 4783–4792 (2006).
Ching, B. J. et al. p63 (TP73L) a key player in embryonic urogenital development with significant dysregulation in human bladder exstrophy tissue. Int. J. Mol. Med. 26, 861–867 (2010).
Wilkins, S. et al. Insertion/deletion polymorphisms in the DeltaNp63 promoter are a risk factor for bladder exstrophy epispadias complex. PLoS Genet. 8, e1003070 (2012).
Kong, X. T. et al. Roles of uroplakins in plaque formation, umbrella cell enlargement, and urinary tract diseases. J. Cell Biol. 167, 1195–1204 (2004).
Carpenter, A. R. et al. Uroplakin 1b is critical in urinary tract development and urothelial differentiation and homeostasis. Kidney Int. 89, 612–624 (2016).
Carpenter, A. R. & McHugh, K. M. Role of renal urothelium in the development and progression of kidney disease. Pediatr. Nephrol. 32, 557–564 (2017).
Hu, P. et al. Ablation of uroplakin III gene results in small urothelial plaques, urothelial leakage, and vesicoureteral reflux. J. Cell Biol. 151, 961–972 (2000).
Deng, F. M. et al. Uroplakin IIIb, a urothelial differentiation marker, dimerizes with uroplakin Ib as an early step of urothelial plaque assembly. J. Cell Biol. 159, 685–694 (2002).
Rudat, C. et al. Upk3b is dispensable for development and integrity of urothelium and mesothelium. PLoS One 9, e112112 (2014).
Liao, Y. et al. Uroplakins play conserved roles in egg fertilization and acquired additional urothelial functions during mammalian divergence. Mol. Biol. Cell. 29, 3128–3143 (2018).
Mahbub Hasan, A. K. et al. The egg membrane microdomain-associated uroplakin III-Src system becomes functional during oocyte maturation and is required for bidirectional gamete signaling at fertilization in Xenopus laevis. Development 141, 1705–1714 (2014).
Mahbub Hasan, A. K. et al. Uroplakin III, a novel Src substrate in Xenopus egg rafts, is a target for sperm protease essential for fertilization. Dev. Biol. 286, 483–492 (2005).
Sakakibara, K. et al. Molecular identification and characterization of Xenopus egg uroplakin III, an egg raft-associated transmembrane protein that is tyrosine-phosphorylated upon fertilization. J. Biol. Chem. 280, 15029–15037 (2005).
Mitra, S. et al. Requirement for a uroplakin 3a-like protein in the development of zebrafish pronephric tubule epithelial cell function, morphogenesis, and polarity. PLoS One 7, e41816 (2012).
Thumbikat, P. et al. Bacteria-induced uroplakin signaling mediates bladder response to infection. PLoS Pathog. 5, e1000415 (2009).
Schonfelder, E. M. et al. Mutations in uroplakin IIIA are a rare cause of renal hypodysplasia in humans. Am. J. Kidney Dis. 47, 1004–1012 (2006).
Jiang, S. et al. Lack of major involvement of human uroplakin genes in vesicoureteral reflux: implications for disease heterogeneity. Kidney Int. 66, 10–19 (2004).
Kelly, H. et al. Uroplakin III is not a major candidate gene for primary vesicoureteral reflux. Eur. J. Hum. Genet. 13, 500–502 (2005).
Jenkins, D. et al. Mutation analyses of uroplakin II in children with renal tract malformations. Nephrol. Dial. Transplant. 21, 3415–3421 (2006).
Fujita, H., Hamazaki, Y., Noda, Y., Oshima, M. & Minato, N. Claudin-4 deficiency results in urothelial hyperplasia and lethal hydronephrosis. PLoS One 7, e52272 (2012).
Fogelgren, B. et al. Urothelial defects from targeted inactivation of exocyst Sec10 in mice cause ureteropelvic junction obstructions. PLoS One 10, e0129346 (2015).
Martin-Urdiroz, M., Deeks, M. J., Horton, C. G., Dawe, H. R. & Jourdain, I. The Exocyst complex in health and disease. Front. Cell Dev. Biol. 4, 24 (2016).
Lee, A. J. et al. Fibroproliferative response to urothelial failure obliterates the ureter lumen in a mouse model of prenatal congenital obstructive nephropathy. Sci. Rep. 6, 31137 (2016).
Hou, T. et al. Aberrant differentiation of urothelial cells in patients with ureteropelvic junction obstruction. Int. J. Clin. Exp. Pathol. 7, 5837–5845 (2014).
Chiou, Y. Y., Shieh, C. C., Cheng, H. L. & Tang, M. J. Intrinsic expression of Th2 cytokines in urothelium of congenital ureteropelvic junction obstruction. Kidney Int. 67, 638–646 (2005).
Huang, W. Y., Olumi, A. F. & Rosen, S. Urothelial mucosal malformation: a rare cause for ureteropelvic junction obstruction. Pediatr. Dev. Pathol. 9, 72–74 (2006).
Romih, R., Korosec, P., de Mello, W. Jr & Jezernik, K. Differentiation of epithelial cells in the urinary tract. Cell Tissue Res. 320, 259–268 (2005).
Becknell, B. et al. Molecular basis of renal adaptation in a murine model of congenital obstructive nephropathy. PLoS One 8, e72762 (2013).
Jackson, A. R. et al. The uroplakin plaque promotes renal structural integrity during congenital and acquired urinary tract obstruction. Am. J. Physiol. Renal Physiol. 315, F1019–F1031 (2018).
Girshovich, A. et al. Ureteral obstruction promotes proliferation and differentiation of the renal urothelium into a bladder-like phenotype. Kidney Int. 82, 428–435 (2012).
Chen, W. Y. et al. IL-33/ST2 axis mediates hyperplasia of intrarenal urothelium in obstructive renal injury. Exp. Mol. Med. 50, 36 (2018).
Sorantin, E., Fotter, R., Aigner, R., Ring, E. & Riccabona, M. The sonographically thickened wall of the upper urinary tract system: correlation with other imaging methods. Pediatr. Radiol. 27, 667–671 (1997).
Tain, Y. L. Renal pelvic wall thickening in childhood urinary tract infections — evidence of acute pyelitis or vesicoureteral reflux? Scand. J. Urol. Nephrol. 37, 28–30 (2003).
Nicolet, V. et al. Thickening of the renal collecting system: a nonspecific finding at US. Radiology 168, 411–413 (1988).
Birnholz, J. C. & Merkel, F. K. Submucosal edema of the collecting system: a new ultrasonic sign of severe, acute renal allograft rejection. A clinical note. Radiology 154, 190 (1985).
Avni, E. F. et al. US demonstration of pyelitis and ureteritis in children. Pediatr. Radiol. 18, 134–139 (1988).
Gordon, Z. N. et al. Uroepithelial thickening improves detection of vesicoureteral reflux in infants with prenatal hydronephrosis. J. Pediatr. Urol. 12, 257 e251–e257 (2016).
Gordon, Z. N., McLeod, D. J., Becknell, B., Bates, D. G. & Alpert, S. A. Uroepithelial thickening on sonography improves detection of vesicoureteral reflux in children with first febrile urinary tract infection. J. Urol. 194, 1074–1079 (2015).
Wallace, S. S. et al. Renal ultrasound for infants younger than 2 months with a febrile urinary tract infection. AJR Am. J. Roentgenol. 205, 894–898 (2015).
Li, B. et al. Inflammation drives renal scarring in experimental pyelonephritis. Am. J. Physiol. Renal Physiol. 312, F43–F53 (2017).
Gupta, S. et al. Urinary antimicrobial peptides: potential novel biomarkers of obstructive uropathy. J. Pediatr. Urol. 14, 238e231–238e236 (2018).
Chromek, M. et al. The antimicrobial peptide cathelicidin protects the urinary tract against invasive bacterial infection. Nat. Med. 12, 636–641 (2006).
Makino, T., Kawashima, H., Konishi, H., Nakatani, T. & Kiyama, H. Elevated urinary levels and urothelial expression of hepatocarcinoma-intestine-pancreas/pancreatitis-associated protein in patients with interstitial cystitis. Urology 75, 933–937 (2010).
Spencer, J. D. et al. Expression and significance of the HIP/PAP and RegIIIγ antimicrobial peptides during mammalian urinary tract infection. PLoS One 10, e0144024 (2015).
Acknowledgements
The authors’ research work is supported by National Institutes of Health grants F32DK115085 (A.R.J.), K08-DK122119 (C.B.C.), R01DK085242 (K.M.M.), K08-DK102594 (B.B.) and R01-DK125469 (B.B.). B.B. is also supported by a Norman Siegel Research Scholar Grant from the American Society of Nephrology Foundation for Kidney Research.
Author information
Authors and Affiliations
Contributions
All authors researched data for the article, wrote the draft, participated in discussions of its content and reviewed and/or edited the manuscript before submission.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Peer review information
Nature Reviews Urology thanks C. Mendelsohn and the other, anonymous, reviewer(s) for their contribution to the peer review of this work.
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Jackson, A.R., Ching, C.B., McHugh, K.M. et al. Roles for urothelium in normal and aberrant urinary tract development. Nat Rev Urol 17, 459–468 (2020). https://doi.org/10.1038/s41585-020-0348-2
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41585-020-0348-2
This article is cited by
-
Ahnak is required to balance calcium ion homeostasis and smooth muscle development in the urinary system
Cell & Bioscience (2023)
-
The urothelium: a multi-faceted barrier against a harsh environment
Mucosal Immunology (2022)