Abstract
Macrophages have important roles in immune surveillance and in the maintenance of kidney homeostasis; their response to renal injury varies enormously depending on the nature and duration of the insult. Macrophages can adopt a variety of phenotypes: at one extreme, M1 pro-inflammatory cells contribute to infection clearance but can also promote renal injury; at the other extreme, M2 anti-inflammatory cells have a reparative phenotype and can contribute to the resolution phase of the response to injury. In addition, bone marrow monocytes can differentiate into myeloid-derived suppressor cells that can regulate T cell immunity in the kidney. However, macrophages can also promote renal fibrosis, a major driver of progression to end-stage renal disease, and the CD206+ subset of M2 macrophages is strongly associated with renal fibrosis in both human and experimental diseases. Myofibroblasts are important contributors to renal fibrosis and recent studies provide evidence that macrophages recruited from the bone marrow can transition directly into myofibroblasts within the injured kidney. This process is termed macrophage-to-myofibroblast transition (MMT) and is driven by transforming growth factor-β1 (TGFβ1)–Smad3 signalling via a Src-centric regulatory network. MMT may serve as a key checkpoint for the progression of chronic inflammation into pathogenic fibrosis.
Key points
-
Macrophages have important roles in kidney homeostasis and in the response to acute and chronic kidney injury.
-
Macrophage phenotype varies enormously depending on the nature and duration of renal injury, ranging from the pro-inflammatory phenotype of M1 cells to the anti-inflammatory phenotype of M2 cells that are involved in tissue repair and fibrosis; monocytic myeloid-derived suppressor cells contribute to immune regulation.
-
Macrophages are plastic cells and their gene expression patterns and functions adapt rapidly to the dynamics of the renal microenvironment.
-
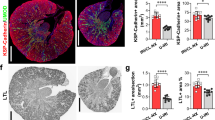
CD206+ M2 macrophages are strongly associated with renal fibrosis in human and experimental kidney diseases.
-
Macrophages derived from bone marrow cells can directly contribute to renal fibrosis through a process termed macrophage-to-myofibroblast transition (MMT).
-
The induction of MMT, via the Src-centric regulatory network mediated by transforming growth factor-β1 (TGFβ1)–Smad3, serves as a key checkpoint in the progression of chronic inflammation to renal fibrosis.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$29.99 / 30 days
cancel any time
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout





Similar content being viewed by others
References
Viehmann, S. F., Bohner, A. M. C., Kurts, C. & Brahler, S. The multifaceted role of the renal mononuclear phagocyte system. Cell. Immunol. 330, 97–104 (2018).
MacPherson, G. G., Murphy, M. J. Jr & Morris, B. The traffic of mononuclear phagocytes through renal allografts in sheep. Transplantation 24, 16–28 (1977).
Cline, M. J., Warner, N. L. & Metcalf, D. Identification of the bone marrow colony mononuclear phagocyte as a macrophage. Blood 39, 327–330 (1972).
Muller, S. et al. Single-cell profiling of human gliomas reveals macrophage ontogeny as a basis for regional differences in macrophage activation in the tumor microenvironment. Genome Biol. 18, 234 (2017).
Lavin, Y. et al. Tissue-resident macrophage enhancer landscapes are shaped by the local microenvironment. Cell 159, 1312–1326 (2014).
Gabius, H. J. & Vehmeyer, K. Effect of microenvironment and cell-line type on carbohydrate-binding proteins of macrophage-like cells. Biochem. Cell Biol. 66, 1169–1176 (1988).
Robertson, M. J. et al. Retinal microenvironment controls resident and infiltrating macrophage function during uveoretinitis. Invest. Ophthalmol. Vis. Sci. 43, 2250–2257 (2002).
Weidenbusch, M. & Anders, H. J. Tissue microenvironments define and get reinforced by macrophage phenotypes in homeostasis or during inflammation, repair and fibrosis. J. Innate Immun. 4, 463–477 (2012).
Knighton, D. R. & Fiegel, V. D. Macrophage-derived growth factors in wound healing: regulation of growth factor production by the oxygen microenvironment. Am. Rev. Respir. Dis. 140, 1108–1111 (1989).
Das, A. et al. Monocyte and macrophage plasticity in tissue repair and regeneration. Am. J. Pathol. 185, 2596–2606 (2015).
Rosenberger, C. M. & Finlay, B. B. Phagocyte sabotage: disruption of macrophage signalling by bacterial pathogens. Nat. Rev. Mol. Cell Biol. 4, 385–396 (2003).
Isbel, N. M. et al. Tubules are the major site of M-CSF production in experimental kidney disease: correlation with local macrophage proliferation. Kidney Int. 60, 614–625 (2001).
Lever, J. M. et al. Parabiosis reveals leukocyte dynamics in the kidney. Lab. Invest. 98, 391–402 (2018).
Gee, J. B., Hinman, L., Stevens, C. & Matthay, R. Human alveolar macrophage and obstructive lung disease. Chest 77, 271–272 (1980).
Gendelman, H. E., Skillman, D. R. & Meltzer, M. S. Interferon alpha (IFN)-macrophage interactions in human immunodeficiency virus (HIV) infection: role of IFN in the tempo and progression of HIV disease. Int. Rev. Immunol. 8, 43–54 (1992).
Li, H. et al. Cigarette smoke extract-treated mast cells promote alveolar macrophage infiltration and polarization in experimental chronic obstructive pulmonary disease. Inhal. Toxicol. 27, 822–831 (2015).
Nikolic-Paterson, D. J., Wang, S. & Lan, H. Y. Macrophages promote renal fibrosis through direct and indirect mechanisms. Kidney Int. Suppl. 4, 34–38 (2014).
Sabelli, M. et al. Human macrophage ferroportin biology and the basis for the ferroportin disease. Hepatology 65, 1512–1525 (2017).
Brune, B., Weigert, A. & Dehne, N. Macrophage polarization in the tumor microenvironment. Redox Biol. 5, 419 (2015).
Han, Y., Ma, F. Y., Tesch, G. H., Manthey, C. L. & Nikolic-Paterson, D. J. c-Fms blockade reverses glomerular macrophage infiltration and halts development of crescentic anti-GBM glomerulonephritis in the rat. Lab. Invest. 91, 978–991 (2011).
Lech, M. et al. Macrophage phenotype controls long-term AKI outcomes—kidney regeneration versus atrophy. J. Am. Soc. Nephrol. 25, 292–304 (2014).
Ma, F. Y. et al. TGF-beta1-activated kinase-1 regulates inflammation and fibrosis in the obstructed kidney. Am. J. Physiol. Renal Physiol. 300, F1410–F1421 (2011).
Ma, R., Jiang, W., Li, Z., Sun, Y. & Wei, Z. Intrarenal macrophage infiltration induced by T cells is associated with podocyte injury in lupus nephritis patients. Lupus 25, 1577–1586 (2016).
Tan, T. K. et al. Macrophage matrix metalloproteinase-9 mediates epithelial-mesenchymal transition in vitro in murine renal tubular cells. Am. J. Pathol. 176, 1256–1270 (2010).
Wise, A. F. et al. Human mesenchymal stem cells alter macrophage phenotype and promote regeneration via homing to the kidney following ischemia-reperfusion injury. Am. J. Physiol. Renal Physiol. 306, F1222–F1235 (2014).
Zhang, X. L., Guo, Y. F., Song, Z. X. & Zhou, M. Vitamin D prevents podocyte injury via regulation of macrophage M1/M2 phenotype in diabetic nephropathy rats. Endocrinology 155, 4939–4950 (2014).
Wang, S. et al. TGF-beta/Smad3 signalling regulates the transition of bone marrow-derived macrophages into myofibroblasts during tissue fibrosis. Oncotarget 7, 8809–8822 (2016).
Wang, Y. Y. et al. Macrophage-to-myofibroblast transition contributes to interstitial fibrosis in chronic renal allograft injury. J. Am. Soc. Nephrol. 28, 2053–2067 (2017).
Meng, X. M. et al. Inflammatory macrophages can transdifferentiate into myofibroblasts during renal fibrosis. Cell Death Dis. 7, e2495 (2016).
Gordon, S. & Pluddemann, A. Tissue macrophages: heterogeneity and functions. BMC Biol. 15, 53 (2017).
Mills, C. D., Kincaid, K., Alt, J. M., Heilman, M. J. & Hill, A. M. M-1/M-2 macrophages and the Th1/Th2 paradigm. J. Immunol. 164, 6166–6173 (2000).
Kiss, M., Van Gassen, S., Movahedi, K., Saeys, Y. & Laoui, D. Myeloid cell heterogeneity in cancer: not a single cell alike. Cell. Immunol. 330, 188–201 (2018).
Cochain, C. et al. Single-cell RNA-seq reveals the transcriptional landscape and heterogeneity of aortic macrophages in murine atherosclerosis. Circ. Res. 122, 1661–1674 (2018).
Kim, C. C., Nakamura, M. C. & Hsieh, C. L. Brain trauma elicits non-canonical macrophage activation states. J. Neuroinflammation 13, 117 (2016).
Puranik, A. S. et al. Kidney-resident macrophages promote a proangiogenic environment in the normal and chronically ischemic mouse kidney. Sci. Rep. 8, 13948 (2018).
Dai, X. et al. Acute Penicillium marneffei infection stimulates host M1/M2a macrophages polarization in BALB/C mice. BMC Microbiol. 17, 177 (2017).
Khan, J., Sharma, P. K. & Mukhopadhaya, A. Vibrio cholerae porin OmpU mediates M1-polarization of macrophages/monocytes via TLR1/TLR2 activation. Immunobiology 220, 1199–1209 (2015).
Kalish, S. V. et al. Macrophages reprogrammed in vitro towards the M1 phenotype and activated with LPS extend lifespan of mice with Ehrlich ascites carcinoma. Med. Sci. Monit. Basic Res. 21, 226–234 (2015).
Murphy, B. S. et al. Azithromycin alters macrophage phenotype. J. Antimicrob. Chemother. 61, 554–560 (2008).
Ishizuka, E. K. et al. Role of interplay between IL-4 and IFN-gamma in the in regulating M1 macrophage polarization induced by nattectin. Int. Immunopharmacol. 14, 513–522 (2012).
Venturin, G. L., Chiku, V. M., Silva, K. L., de Almeida, B. F. & de Lima, V. M. M1 polarization and the effect of PGE2 on TNF-alpha production by lymph node cells from dogs with visceral leishmaniasis. Parasite Immunol. 38, 698–704 (2016).
Wilson, H. M. et al. Inhibition of macrophage nuclear factor-kappaB leads to a dominant anti-inflammatory phenotype that attenuates glomerular inflammation in vivo. Am. J. Pathol. 167, 27–37 (2005).
Hennemann, B., Kreutz, M., Rehm, A. & Andreesen, R. Effect of granulocyte-macrophage colony-stimulating factor treatment on phenotype, cytokine release and cytotoxicity of circulating blood monocytes and monocyte-derived macrophages. Br. J. Haematol. 102, 1197–1203 (1998).
Karuppagounder, V. et al. Curcumin alleviates renal dysfunction and suppresses inflammation by shifting from M1 to M2 macrophage polarization in daunorubicin induced nephrotoxicity in rats. Cytokine 84, 1–9 (2016).
Lv, L. L. et al. The pattern recognition receptor, Mincle, is essential for maintaining the M1 macrophage phenotype in acute renal inflammation. Kidney Int. 91, 587–602 (2017).
Iacopino, A. M. et al. Phenytoin and cyclosporine A specifically regulate macrophage phenotype and expression of platelet-derived growth factor and interleukin-1 in vitro and in vivo: possible molecular mechanism of drug-induced gingival hyperplasia. J. Periodontol. 68, 73–83 (1997).
Onore, C. E. et al. Inflammatory macrophage phenotype in BTBR T+tf/J mice. Front. Neurosci. 7, 158 (2013).
Vinuesa, E. et al. Macrophage involvement in the kidney repair phase after ischaemia/reperfusion injury. J. Pathol. 214, 104–113 (2008).
Huen, S. C. & Cantley, L. G. Macrophage-mediated injury and repair after ischemic kidney injury. Pediatr. Nephrol. 30, 199–209 (2015).
Lee, S. et al. Distinct macrophage phenotypes contribute to kidney injury and repair. J. Am. Soc. Nephrol. 22, 317–326 (2011).
Alikhan, M. A. et al. Colony-stimulating factor-1 promotes kidney growth and repair via alteration of macrophage responses. Am. J. Pathol. 179, 1243–1256 (2011).
Zhang, M. Z. et al. IL-4/IL-13-mediated polarization of renal macrophages/dendritic cells to an M2a phenotype is essential for recovery from acute kidney injury. Kidney Int. 91, 375–386 (2017).
Cassol, E., Cassetta, L., Rizzi, C., Alfano, M. & Poli, G. M1 and M2a polarization of human monocyte-derived macrophages inhibits HIV-1 replication by distinct mechanisms. J. Immunol. 182, 6237–6246 (2009).
Zhao, X. et al. PI3K/Akt signaling pathway modulates influenza virus induced mouse alveolar macrophage polarization to M1/M2b. PLOS ONE 9, e104506 (2014).
Lisi, L., Stigliano, E., Lauriola, L., Navarra, P. & Dello Russo, C. Proinflammatory-activated glioma cells induce a switch in microglial polarization and activation status, from a predominant M2b phenotype to a mixture of M1 and M2a/B polarized cells. ASN Neuro 6, 171–183 (2014).
Kim, M. G. et al. The role of M2 macrophages in the progression of chronic kidney disease following acute kidney injury. PLOS ONE 10, e0143961 (2015).
Spiller, K. L. et al. The role of macrophage phenotype in vascularization of tissue engineering scaffolds. Biomaterials 35, 4477–4488 (2014).
Lu, J. et al. Discrete functions of M2a and M2c macrophage subsets determine their relative efficacy in treating chronic kidney disease. Kidney Int. 84, 745–755 (2013).
Tang, L. et al. M2A and M2C macrophage subsets ameliorate inflammation and fibroproliferation in acute lung injury through interleukin 10 pathway. Shock 48, 119–129 (2017).
Chaves, L. D. et al. Contrasting effects of systemic monocyte/macrophage and CD4+T cell depletion in a reversible ureteral obstruction mouse model of chronic kidney disease. Clin. Dev. Immunol. 2013, 836989 (2013).
Zhang, M. Z. et al. CSF-1 signaling mediates recovery from acute kidney injury. J. Clin. Invest. 122, 4519–4532 (2012).
Cao, Q. et al. Failed renoprotection by alternatively activated bone marrow macrophages is due to a proliferation-dependent phenotype switch in vivo. Kidney Int. 85, 794–806 (2014).
Menezes, S. et al. The heterogeneity of Ly6C(hi) monocytes controls their differentiation into iNOS(+) macrophages or monocyte-derived dendritic cells. Immunity 45, 1205–1218 (2016).
Lin, S. L., Castano, A. P., Nowlin, B. T., Lupher, M. L. Jr & Duffield, J. S. Bone marrow Ly6Chigh monocytes are selectively recruited to injured kidney and differentiate into functionally distinct populations. J. Immunol. 183, 6733–6743 (2009).
Rodero, M. P., Hodgson, S. S., Hollier, B., Combadiere, C. & Khosrotehrani, K. Reduced Il17a expression distinguishes a Ly6c(lo)MHCII(hi) macrophage population promoting wound healing. J. Invest. Dermatol. 133, 783–792 (2013).
Clements, M. et al. Differential Ly6C expression after renal ischemia-reperfusion identifies unique macrophage populations. J. Am. Soc. Nephrol. 27, 159–170 (2016).
Carlin, L. M. et al. Nr4a1-dependent Ly6C(low) monocytes monitor endothelial cells and orchestrate their disposal. Cell 153, 362–375 (2013).
Westhorpe, C. L. V. et al. Effector CD4(+) T cells recognize intravascular antigen presented by patrolling monocytes. Nat. Commun. 9, 747 (2018).
Ochando, J., Conde, P. & Bronte, V. Monocyte-derived suppressor cells in transplantation. Curr. Transplant. Rep. 2, 176–183 (2015).
Garcia, M. R. et al. Monocytic suppressive cells mediate cardiovascular transplantation tolerance in mice. J. Clin. Invest. 120, 2486–2496 (2010).
Yang, F. et al. TNFalpha-induced M-MDSCs promote transplant immune tolerance via nitric oxide. J. Mol. Med. 94, 911–920 (2016).
Rogers, N. M., Ferenbach, D. A., Isenberg, J. S., Thomson, A. W. & Hughes, J. Dendritic cells and macrophages in the kidney: a spectrum of good and evil. Nat. Rev. Nephrol. 10, 625–643 (2014).
Gottschalk, C. & Kurts, C. The debate about dendritic cells and macrophages in the kidney. Front. Immunol. 6, 435 (2015).
Isbel, N. M., Nikolic-Paterson, D. J., Hill, P. A., Dowling, J. & Atkins, R. C. Local macrophage proliferation correlates with increased renal M-CSF expression in human glomerulonephritis. Nephrol. Dial. Transplant. 16, 1638–1647 (2001).
Yang, N. et al. Local macrophage proliferation in human glomerulonephritis. Kidney Int. 54, 143–151 (1998).
Nolasco, F. E. et al. Intraglomerular T cells and monocytes in nephritis: study with monoclonal antibodies. Kidney Int. 31, 1160–1166 (1987).
Brasen, J. H. et al. Macrophage density in early surveillance biopsies predicts future renal transplant function. Kidney Int. 92, 479–489 (2017).
Matturri, L., Ghidoni, P., Palazzi, P. & Stasi, P. Renal allograft rejection: immunohistochemistry of inflammatory cellular subsets and vascular lesions. Basic Appl. Histochem. 30, 267–277 (1986).
Kashem, A. et al. Expression of inducible-NOS in human glomerulonephritis: the possible source is infiltrating monocytes/macrophages. Kidney Int. 50, 392–399 (1996).
Noronha, I. L., Kruger, C., Andrassy, K., Ritz, E. & Waldherr, R. In situ production of TNF-alpha, IL-1 beta and IL-2R in ANCA-positive glomerulonephritis. Kidney Int. 43, 682–692 (1993).
Wu, Q., Jinde, K., Endoh, M. & Sakai, H. Clinical significance of costimulatory molecules CD80/CD86 expression in IgA nephropathy. Kidney Int. 65, 888–896 (2004).
D’Souza, M. J. et al. Macrophage depletion by albumin microencapsulated clodronate: attenuation of cytokine release in macrophage-dependent glomerulonephritis. Drug Dev. Ind. Pharm. 25, 591–596 (1999).
Duffield, J. S. et al. Conditional ablation of macrophages halts progression of crescentic glomerulonephritis. Am. J. Pathol. 167, 1207–1219 (2005).
Ferenbach, D. A. et al. Macrophage/monocyte depletion by clodronate, but not diphtheria toxin, improves renal ischemia/reperfusion injury in mice. Kidney Int. 82, 928–933 (2012).
Jo, S. K., Sung, S. A., Cho, W. Y., Go, K. J. & Kim, H. K. Macrophages contribute to the initiation of ischaemic acute renal failure in rats. Nephrol. Dial. Transplant. 21, 1231–1239 (2006).
Jose, M. D., Ikezumi, Y., van Rooijen, N., Atkins, R. C. & Chadban, S. J. Macrophages act as effectors of tissue damage in acute renal allograft rejection. Transplantation 76, 1015–1022 (2003).
Lan, H. Y., Nikolic-Paterson, D. J., Mu, W. & Atkins, R. C. Local macrophage proliferation in the progression of glomerular and tubulointerstitial injury in rat anti-GBM glomerulonephritis. Kidney Int. 48, 753–760 (1995).
Jose, M. D., Le Meur, Y., Atkins, R. C. & Chadban, S. J. Blockade of macrophage colony-stimulating factor reduces macrophage proliferation and accumulation in renal allograft rejection. Am. J. Transplant. 3, 294–300 (2003).
Le Meur, Y. et al. Macrophage accumulation at a site of renal inflammation is dependent on the M-CSF/c-fms pathway. J. Leukoc. Biol. 72, 530–537 (2002).
Lim, A. K. et al. Antibody blockade of c-fms suppresses the progression of inflammation and injury in early diabetic nephropathy in obese db/db mice. Diabetologia 52, 1669–1679 (2009).
Ma, F. Y., Woodman, N., Mulley, W. R., Kanellis, J. & Nikolic-Paterson, D. J. Macrophages contribute to cellular but not humoral mechanisms of acute rejection in rat renal allografts. Transplantation 96, 949–957 (2013).
Tesch, G. H. MCP-1/CCL2: a new diagnostic marker and therapeutic target for progressive renal injury in diabetic nephropathy. Am. J. Physiol. Renal Physiol. 294, F697–F701 (2008).
Lloyd, C. M. et al. RANTES and monocyte chemoattractant protein-1 (MCP-1) play an important role in the inflammatory phase of crescentic nephritis, but only MCP-1 is involved in crescent formation and interstitial fibrosis. J. Exp. Med. 185, 1371–1380 (1997).
Chow, F. Y. et al. Monocyte chemoattractant protein-1-induced tissue inflammation is critical for the development of renal injury but not type 2 diabetes in obese db/db mice. Diabetologia 50, 471–480 (2007).
Chow, F. Y. et al. Monocyte chemoattractant protein-1 promotes the development of diabetic renal injury in streptozotocin-treated mice. Kidney Int. 69, 73–80 (2006).
Kang, Y. S. et al. CCR2 antagonism improves insulin resistance, lipid metabolism, and diabetic nephropathy in type 2 diabetic mice. Kidney Int. 78, 883–894 (2010).
Haller, H., Bertram, A., Nadrowitz, F. & Menne, J. Monocyte chemoattractant protein-1 and the kidney. Curr. Opin. Nephrol. Hypertens. 25, 42–49 (2016).
Li, L. et al. The chemokine receptors CCR2 and CX3CR1 mediate monocyte/macrophage trafficking in kidney ischemia-reperfusion injury. Kidney Int. 74, 1526–1537 (2008).
Peng, X., Zhang, J., Xiao, Z., Dong, Y. & Du, J. CX3CL1-CX3CR1 interaction increases the population of Ly6C(-)CX3CR1(hi) macrophages contributing to unilateral ureteral obstruction-induced fibrosis. J. Immunol. 195, 2797–2805 (2015).
Zhuang, Q., Cheng, K. & Ming, Y. CX3CL1/CX3CR1 axis, as the therapeutic potential in renal diseases: friend or foe? Curr. Gene Ther. 17, 442–452 (2017).
Ma, Z., Jin, X., He, L. & Wang, Y. CXCL16 regulates renal injury and fibrosis in experimental renal artery stenosis. Am. J. Physiol. Heart Circ. Physiol. 311, H815–H821 (2016).
Lan, H. Y. et al. The pathogenic role of macrophage migration inhibitory factor in immunologically induced kidney disease in the rat. J. Exp. Med. 185, 1455–1465 (1997).
Lan, H. Y. et al. Expression of macrophage migration inhibitory factor in human glomerulonephritis. Kidney Int. 57, 499–509 (2000).
Yu, X. Q. et al. A functional role for osteopontin in experimental crescentic glomerulonephritis in the rat. Proc. Assoc. Am. Physicians 110, 50–64 (1998).
Tesch, G. H. Diabetic nephropathy — is this an immune disorder? Clin. Sci. 131, 2183–2199 (2017).
Alexander, J. J., Chaves, L., Chang, A. & Quigg, R. J. The C5a receptor has a key role in immune complex glomerulonephritis in complement factor H-deficient mice. Kidney Int. 82, 961–968 (2012).
Lopez-Parra, V. et al. Fcgamma receptor deficiency attenuates diabetic nephropathy. J. Am. Soc. Nephrol. 23, 1518–1527 (2012).
Mocsai, A., Ruland, J. & Tybulewicz, V. L. The SYK tyrosine kinase: a crucial player in diverse biological functions. Nat. Rev. Immunol. 10, 387–402 (2010).
McAdoo, S. P. et al. Correlation of disease activity in proliferative glomerulonephritis with glomerular spleen tyrosine kinase expression. Kidney Int. 88, 52–60 (2015).
Ryan, J. et al. Myeloid cell-mediated renal injury in rapidly progressive glomerulonephritis depends upon spleen tyrosine kinase. J. Pathol. 238, 10–20 (2016).
Ryan, J., K., J., Blease, K., Ma, F. Y. & Nikolic-Paterson, D. J. Spleen tyrosine kinase signalling promotes myeloid cell recruitment and kidney damage following renal ischaemia/reperfusion injury. Am. J. Pathol. 186, 2032–2042 (2016).
Ramessur Chandran, S. et al. Inhibition of spleen tyrosine kinase reduces renal allograft injury in a rat model of acute antibody-mediated rejection in sensitized recipients. Transplantation 101, e240–e248 (2017).
Ma, F. Y., Blease, K. & Nikolic-Paterson, D. J. A role for spleen tyrosine kinase in renal fibrosis in the mouse obstructed kidney. Life Sci. 146, 192–200 (2016).
Han, Y., Ma, F. Y., Di Paolo, J. & Nikolic-Paterson, D. J. An inhibitor of spleen tyrosine kinase suppresses experimental crescentic glomerulonephritis. Int. J. Immunopathol. Pharmacol. 32, 2058738418783404 (2018).
Awad, A. S. et al. Macrophage-derived tumor necrosis factor-alpha mediates diabetic renal injury. Kidney Int. 88, 722–733 (2015).
Lan, H. Y., Nikolic-Paterson, D. J., Zarama, M., Vannice, J. L. & Atkins, R. C. Suppression of experimental crescentic glomerulonephritis by the interleukin-1 receptor antagonist. Kidney Int. 43, 479–485 (1993).
Lan, H. Y. et al. TNF-alpha up-regulates renal MIF expression in rat crescentic glomerulonephritis. Mol. Med. 3, 136–144 (1997).
Nikolic-Paterson, D. J., Lan, H. Y., Hill, P. A., Vannice, J. L. & Atkins, R. C. Suppression of experimental glomerulonephritis by the interleukin-1 receptor antagonist: inhibition of intercellular adhesion molecule-1 expression. J. Am. Soc. Nephrol. 4, 1695–1700 (1994).
Timoshanko, J. R., Sedgwick, J. D., Holdsworth, S. R. & Tipping, P. G. Intrinsic renal cells are the major source of tumor necrosis factor contributing to renal injury in murine crescentic glomerulonephritis. J. Am. Soc. Nephrol. 14, 1785–1793 (2003).
Ikezumi, Y., Atkins, R. C. & Nikolic-Paterson, D. J. Interferon-gamma augments acute macrophage-mediated renal injury via a glucocorticoid-sensitive mechanism. J. Am. Soc. Nephrol. 14, 888–898 (2003).
Ikezumi, Y., Hurst, L., Atkins, R. C. & Nikolic-Paterson, D. J. Macrophage-mediated renal injury is dependent on signaling via the JNK pathway. J. Am. Soc. Nephrol. 15, 1775–1784 (2004).
Schroder, K., Sweet, M. J. & Hume, D. A. Signal integration between IFNgamma and TLR signalling pathways in macrophages. Immunobiology 211, 511–524 (2006).
Anders, H. J. et al. Activation of toll-like receptor-9 induces progression of renal disease in MRL-Fas(lpr) mice. FASEB J. 18, 534–536 (2004).
Ryu, M. et al. Bacterial CpG-DNA accelerates Alport glomerulosclerosis by inducing an M1 macrophage phenotype and tumor necrosis factor-alpha-mediated podocyte loss. Kidney Int. 79, 189–198 (2011).
Tomosugi, N. I. et al. Modulation of antibody-mediated glomerular injury in vivo by bacterial lipopolysaccharide, tumor necrosis factor, and IL-1. J. Immunol. 142, 3083–3090 (1989).
Rosin, D. L. & Okusa, M. D. Dangers within: DAMP responses to damage and cell death in kidney disease. J. Am. Soc. Nephrol. 22, 416–425 (2011).
Komada, T. et al. Macrophage uptake of necrotic cell DNA activates the AIM2 inflammasome to regulate a proinflammatory phenotype in CKD. J. Am. Soc. Nephrol. 29, 1165–1181 (2018).
Tian, S. et al. HMGB1 exacerbates renal tubulointerstitial fibrosis through facilitating M1 macrophage phenotype at the early stage of obstructive injury. Am. J. Physiol. Renal Physiol. 308, F69–F75 (2015).
Wu, H. et al. HMGB1 contributes to kidney ischemia reperfusion injury. J. Am. Soc. Nephrol. 21, 1878–1890 (2010).
Chen, X. et al. Blockade of HMGB1 attenuates diabetic nephropathy in mice. Sci. Rep. 8, 8319 (2018).
Horiuchi, S. et al. Pathological roles of advanced glycation end product receptors SR-A and CD36. Ann. NY Acad. Sci. 1043, 671–675 (2005).
Trial, J., Potempa, L. A. & Entman, M. L. The role of C-reactive protein in innate and acquired inflammation: new perspectives. Inflamm. Cell Signal. 3, e1409 (2016).
Li, Z. I. et al. C-Reactive protein promotes acute renal inflammation and fibrosis in unilateral ureteral obstructive nephropathy in mice. Lab. Invest. 91, 837–851 (2011).
Liu, F. et al. C-Reactive protein promotes diabetic kidney disease in a mouse model of type 1 diabetes. Diabetologia 54, 2713–2723 (2011).
You, Y. K. et al. C-reactive protein promotes diabetic kidney disease in db/db mice via the CD32b-Smad3-mTOR signaling pathway. Sci. Rep. 6, 26740 (2016).
Wang, Y. et al. Ex vivo programmed macrophages ameliorate experimental chronic inflammatory renal disease. Kidney Int. 72, 290–299 (2007).
Tomita, N. et al. In vivo administration of a nuclear transcription factor-kappaB decoy suppresses experimental crescentic glomerulonephritis. J. Am. Soc. Nephrol. 11, 1244–1252 (2000).
Bienvenu, L. A. et al. Macrophage mineralocorticoid receptor signaling plays a key role in aldosterone-independent cardiac fibrosis. Endocrinology 153, 3416–3425 (2012).
Tesch, G. H. et al. Intrinsic renal cells are the major source of interleukin-1 beta synthesis in normal and diseased rat kidney. Nephrol. Dial. Transplant. 12, 1109–1115 (1997).
Flanc, R. S. et al. A pathogenic role for JNK signaling in experimental anti-GBM glomerulonephritis. Kidney Int. 72, 698–708 (2007).
Ma, F. Y. et al. Blockade of the c-Jun amino terminal kinase prevents crescent formation and halts established anti-GBM glomerulonephritis in the rat. Lab. Invest. 89, 470–484 (2009).
Arnold, C. E. et al. A critical role for suppressor of cytokine signalling 3 in promoting M1 macrophage activation and function in vitro and in vivo. Immunology 141, 96–110 (2014).
Martin-Fernandez, B. et al. Aldosterone induces renal fibrosis and inflammatory M1-macrophage subtype via mineralocorticoid receptor in rats. PLOS ONE 11, e0145946 (2016).
Huang, L. L. et al. Myeloid mineralocorticoid receptor activation contributes to progressive kidney disease. J. Am. Soc. Nephrol. 25, 2231–2240 (2014).
Bhatt, K. et al. Anti-inflammatory role of microRNA-146a in the pathogenesis of diabetic nephropathy. J. Am. Soc. Nephrol. 27, 2277–2288 (2016).
Abraham, A. P., Ma, F. Y., Mulley, W. R., Nikolic-Paterson, D. J. & Tesch, G. H. Matrix metalloproteinase-12 deficiency attenuates experimental crescentic anti-glomerular basement membrane glomerulonephritis. Nephrology 23, 183–189 (2018).
Kaneko, Y. et al. Macrophage metalloelastase as a major factor for glomerular injury in anti-glomerular basement membrane nephritis. J. Immunol. 170, 3377–3385 (2003).
Moon, D. K. & Geczy, C. L. Recombinant IFN-gamma synergizes with lipopolysaccharide to induce macrophage membrane procoagulants. J. Immunol. 141, 1536–1542 (1988).
Meng, X. M., Nikolic-Paterson, D. J. & Lan, H. Y. TGF-beta: the master regulator of fibrosis. Nat. Rev. Nephrol. 12, 325–338 (2016).
Rockey, D. C., Bell, P. D. & Hill, J. A. Fibrosis—a common pathway to organ injury and failure. N. Engl. J. Med. 372, 1138–1149 (2015).
Mackensen-Haen, S., Bader, R., Grund, K. E. & Bohle, A. Correlations between renal cortical interstitial fibrosis, atrophy of the proximal tubules and impairment of the glomerular filtration rate. Clin. Nephrol. 15, 167–171 (1981).
Risdon, R. A., Sloper, J. C. & De Wardener, H. E. Relationship between renal function and histological changes found in renal-biopsy specimens from patients with persistent glomerular nephritis. Lancet 2, 363–366 (1968).
Danilewicz, M. & Wagrowska-Danielwicz, M. Morphometric and immunohistochemical insight into focal segmental glomerulosclerosis in obese and non-obese patients. Nefrologia 29, 35–41 (2009).
Eardley, K. S. et al. The relationship between albuminuria, MCP-1/CCL2, and interstitial macrophages in chronic kidney disease. Kidney Int. 69, 1189–1197 (2006).
Ikezumi, Y. et al. The sialoadhesin (CD169) expressing a macrophage subset in human proliferative glomerulonephritis. Nephrol. Dial. Transplant. 20, 2704–2713 (2005).
Klessens, C. Q. F. et al. Macrophages in diabetic nephropathy in patients with type 2 diabetes. Nephrol. Dial. Transplant. 32, 1322–1329 (2017).
Ikezumi, Y. et al. Contrasting effects of steroids and mizoribine on macrophage activation and glomerular lesions in rat thy-1 mesangial proliferative glomerulonephritis. Am. J. Nephrol. 31, 273–282 (2010).
Ikezumi, Y. et al. Alternatively activated macrophages in the pathogenesis of chronic kidney allograft injury. Pediatr. Nephrol. 30, 1007–1017 (2015).
Belliere, J. et al. Specific macrophage subtypes influence the progression of rhabdomyolysis-induced kidney injury. J. Am. Soc. Nephrol. 26, 1363–1377 (2015).
Lin, L. & Hu, K. Tissue-type plasminogen activator modulates macrophage M2 to M1 phenotypic change through annexin A2-mediated NF-kappaB pathway. Oncotarget 8, 88094–88103 (2017).
Han, Y., Ma, F. Y., Tesch, G. H., Manthey, C. L. & Nikolic-Paterson, D. J. Role of macrophages in the fibrotic phase of rat crescentic glomerulonephritis. Am. J. Physiol. Renal Physiol. 304, F1043–F1053 (2013).
Ikezumi, Y. et al. Identification of alternatively activated macrophages in new-onset paediatric and adult immunoglobulin A nephropathy: potential role in mesangial matrix expansion. Histopathology 58, 198–210 (2011).
Toki, D. et al. The role of macrophages in the development of human renal allograft fibrosis in the first year after transplantation. Am. J. Transplant. 14, 2126–2136 (2014).
Bellon, T. et al. Alternative activation of macrophages in human peritoneum: implications for peritoneal fibrosis. Nephrol. Dial. Transplant. 26, 2995–3005 (2011).
Braga, T. T. et al. MyD88 signaling pathway is involved in renal fibrosis by favoring a TH2 immune response and activating alternative M2 macrophages. Mol. Med. 18, 1231–1239 (2012).
Kushiyama, T. et al. Alteration in the phenotype of macrophages in the repair of renal interstitial fibrosis in mice. Nephrology 16, 522–535 (2011).
Yamate, J. et al. Participation of different macrophage populations and myofibroblastic cells in chronically developed renal interstitial fibrosis after cisplatin-induced renal injury in rats. Vet. Pathol. 39, 322–333 (2002).
Shen, B., Liu, X., Fan, Y. & Qiu, J. Macrophages regulate renal fibrosis through modulating TGFbeta superfamily signaling. Inflammation 37, 2076–2084 (2014).
Feng, Y. et al. Wnt/beta-catenin-promoted macrophage alternative activation contributes to kidney fibrosis. J. Am. Soc. Nephrol. 29, 182–193 (2018).
Pennathur, S. et al. The macrophage phagocytic receptor CD36 promotes fibrogenic pathways on removal of apoptotic cells during chronic kidney injury. Am. J. Pathol. 185, 2232–2245 (2015).
Du, X. et al. Involvement of matrix metalloproteinase-2 in the development of renal interstitial fibrosis in mouse obstructive nephropathy. Lab. Invest. 92, 1149–1160 (2012).
Eitner, F. et al. PDGF-C is a proinflammatory cytokine that mediates renal interstitial fibrosis. J. Am. Soc. Nephrol. 19, 281–289 (2008).
Henderson, N. C. et al. Galectin-3 expression and secretion links macrophages to the promotion of renal fibrosis. Am. J. Pathol. 172, 288–298 (2008).
Jones, L. K. et al. IL-1RI deficiency ameliorates early experimental renal interstitial fibrosis. Nephrol. Dial. Transplant. 24, 3024–3032 (2009).
Lan, H. Y., Nikolic-Paterson, D. J., Mu, W., Vannice, J. L. & Atkins, R. C. Interleukin-1 receptor antagonist halts the progression of established crescentic glomerulonephritis in the rat. Kidney Int. 47, 1303–1309 (1995).
Niu, H. et al. Matrix metalloproteinase 12 modulates high-fat-diet induced glomerular fibrogenesis and inflammation in a mouse model of obesity. Sci. Rep. 6, 20171 (2016).
Tan, T. K. et al. Matrix metalloproteinase-9 of tubular and macrophage origin contributes to the pathogenesis of renal fibrosis via macrophage recruitment through osteopontin cleavage. Lab. Invest. 93, 434–449 (2013).
Vesey, D. A., Cheung, C., Endre, Z., Gobe, G. & Johnson, D. W. Role of protein kinase C and oxidative stress in interleukin-1beta-induced human proximal tubule cell injury and fibrogenesis. Nephrology 10, 73–80 (2005).
Barrera-Chimal, J. et al. The myeloid mineralocorticoid receptor controls inflammatory and fibrotic responses after renal injury via macrophage interleukin-4 receptor signaling. Kidney Int. 93, 1344–1355 (2018).
Rickard, A. J. et al. Deletion of mineralocorticoid receptors from macrophages protects against deoxycorticosterone/salt-induced cardiac fibrosis and increased blood pressure. Hypertension 54, 537–543 (2009).
Hochst, B. et al. Differential induction of Ly6G and Ly6C positive myeloid derived suppressor cells in chronic kidney and liver inflammation and fibrosis. PLOS ONE 10, e0119662 (2015).
Luan, Y. et al. Monocytic myeloid-derived suppressor cells accumulate in renal transplant patients and mediate CD4(+) Foxp3(+) Treg expansion. Am. J. Transplant. 13, 3123–3131 (2013).
Lebrun, A. et al. CCR2(+) monocytic myeloid-derived suppressor cells (M-MDSCs) inhibit collagen degradation and promote lung fibrosis by producing transforming growth factor-beta1. J. Pathol. 243, 320–330 (2017).
Bryant, A. J. et al. Myeloid-derived suppressor cells are necessary for development of pulmonary hypertension. Am. J. Respir. Cell. Mol. Biol. 58, 170–180 (2018).
Klingberg, F., Hinz, B. & White, E. S. The myofibroblast matrix: implications for tissue repair and fibrosis. J. Pathol. 229, 298–309 (2013).
Falke, L. L., Gholizadeh, S., Goldschmeding, R., Kok, R. J. & Nguyen, T. Q. Diverse origins of the myofibroblast-implications for kidney fibrosis. Nat. Rev. Nephrol. 11, 233–244 (2015).
LeBleu, V. S. et al. Origin and function of myofibroblasts in kidney fibrosis. Nat. Med. 19, 1047–1053 (2013).
Qu, X. et al. Resolvins E1 and D1 inhibit interstitial fibrosis in the obstructed kidney via inhibition of local fibroblast proliferation. J. Pathol. 228, 506–519 (2012).
Yang, N. et al. Local macrophage and myofibroblast proliferation in progressive renal injury in the rat remnant kidney. Nephrol. Dial. Transplant. 13, 1967–1974 (1998).
Broekema, M. et al. Bone marrow-derived myofibroblasts contribute to the renal interstitial myofibroblast population and produce procollagen I after ischemia/reperfusion in rats. J. Am. Soc. Nephrol. 18, 165–175 (2007).
Haudek, S. B. et al. Bone marrow-derived fibroblast precursors mediate ischemic cardiomyopathy in mice. Proc. Natl Acad. Sci. USA 103, 18284–18289 (2006).
Jang, H. S., Kim, J. I., Han, S. J. & Park, K. M. Recruitment and subsequent proliferation of bone marrow-derived cells in the postischemic kidney are important to the progression of fibrosis. Am. J. Physiol. Renal Physiol. 306, F1451–F1461 (2014).
Jang, H. S. et al. Bone marrow-derived cells play a major role in kidney fibrosis via proliferation and differentiation in the infiltrated site. Biochim. Biophys. Acta 1832, 817–825 (2013).
Li, J., Deane, J. A., Campanale, N. V., Bertram, J. F. & Ricardo, S. D. The contribution of bone marrow-derived cells to the development of renal interstitial fibrosis. Stem Cells 25, 697–706 (2007).
Phua, Y. L., Martel, N., Pennisi, D. J., Little, M. H. & Wilkinson, L. Distinct sites of renal fibrosis in Crim1 mutant mice arise from multiple cellular origins. J. Pathol. 229, 685–696 (2013).
Grimm, P. C. et al. Neointimal and tubulointerstitial infiltration by recipient mesenchymal cells in chronic renal-allograft rejection. N. Engl. J. Med. 345, 93–97 (2001).
Gomez, I. G. & Duffield, J. S. The FOXD1 lineage of kidney perivascular cells and myofibroblasts: functions and responses to injury. Kidney Int. Suppl. 4, 26–33 (2014).
Buchtler, S. et al. Cellular origin and functional relevance of collagen I production in the kidney. J. Am. Soc. Nephrol. 29, 1859–1873 (2018).
Lin, S. L., Kisseleva, T., Brenner, D. A. & Duffield, J. S. Pericytes and perivascular fibroblasts are the primary source of collagen-producing cells in obstructive fibrosis of the kidney. Am. J. Pathol. 173, 1617–1627 (2008).
Kramann, R. et al. Parabiosis and single-cell RNA sequencing reveal a limited contribution of monocytes to myofibroblasts in kidney fibrosis. JCI Insight 3, 99561 (2018).
Bucala, R., Spiegel, L. A., Chesney, J., Hogan, M. & Cerami, A. Circulating fibrocytes define a new leukocyte subpopulation that mediates tissue repair. Mol. Med. 1, 71–81 (1994).
Herzog, E. L. & Bucala, R. Fibrocytes in health and disease. Exp. Hematol. 38, 548–556 (2010).
Reich, B. et al. Fibrocytes develop outside the kidney but contribute to renal fibrosis in a mouse model. Kidney Int. 84, 78–89 (2013).
Tang, P. M. et al. TGF-beta signalling in renal fibrosis: from Smads to non-coding RNAs. J. Physiol. 596, 3493–3503 (2018).
Mezzano, S. A. et al. Overexpression of chemokines, fibrogenic cytokines, and myofibroblasts in human membranous nephropathy. Kidney Int. 57, 147–158 (2000).
Chihara, Y. et al. Roles of TGF-beta1 and apoptosis in the progression of glomerulosclerosis in human IgA nephropathy. Clin. Nephrol. 65, 385–392 (2006).
Brennan, E. P. et al. Next-generation sequencing identifies TGF-beta1-associated gene expression profiles in renal epithelial cells reiterated in human diabetic nephropathy. Biochim. Biophys. Acta 1822, 589–599 (2012).
Schena, F. P. & Gesualdo, L. Pathogenetic mechanisms of diabetic nephropathy. J. Am. Soc. Nephrol. 16, S30–S33 (2005).
Meng, X. M., Tang, P. M., Li, J. & Lan, H. Y. Macrophage phenotype in kidney injury and repair. Kidney Dis. 1, 138–146 (2015).
Anders, H. J. & Ryu, M. Renal microenvironments and macrophage phenotypes determine progression or resolution of renal inflammation and fibrosis. Kidney Int. 80, 915–925 (2011).
Gong, D. et al. TGFbeta signaling plays a critical role in promoting alternative macrophage activation. BMC Immunol. 13, 31 (2012).
Sanjabi, S., Oh, S. A. & Li, M. O. Regulation of the immune response by TGF-beta: from conception to autoimmunity and infection. Cold Spring Harb. Perspect. Biol. 9, a022236 (2017).
Shull, M. M. et al. Targeted disruption of the mouse transforming growth factor-beta 1 gene results in multifocal inflammatory disease. Nature 359, 693–699 (1992).
Fujimoto, M. et al. Mice lacking Smad3 are protected against streptozotocin-induced diabetic glomerulopathy. Biochem. Biophys. Res. Commun. 305, 1002–1007 (2003).
Moon, J. A., Kim, H. T., Cho, I. S., Sheen, Y. Y. & Kim, D. K. IN-1130, a novel transforming growth factor-beta type I receptor kinase (ALK5) inhibitor, suppresses renal fibrosis in obstructive nephropathy. Kidney Int. 70, 1234–1243 (2006).
Sato, M., Muragaki, Y., Saika, S., Roberts, A. B. & Ooshima, A. Targeted disruption of TGF-beta1/Smad3 signaling protects against renal tubulointerstitial fibrosis induced by unilateral ureteral obstruction. J. Clin. Invest. 112, 1486–1494 (2003).
Chen, J., Xia, Y., Lin, X., Feng, X. H. & Wang, Y. Smad3 signaling activates bone marrow-derived fibroblasts in renal fibrosis. Lab. Invest. 94, 545–556 (2014).
Mia, S., Warnecke, A., Zhang, X. M., Malmstrom, V. & Harris, R. A. An optimized protocol for human M2 macrophages using M-CSF and IL-4/IL-10/TGF-beta yields a dominant immunosuppressive phenotype. Scand. J. Immunol. 79, 305–314 (2014).
Zhang, F. et al. TGF-beta induces M2-like macrophage polarization via SNAIL-mediated suppression of a pro-inflammatory phenotype. Oncotarget 7, 52294–52306 (2016).
Guo, X. et al. Hypoxia promotes glioma-associated macrophage infiltration via periostin and subsequent M2 polarization by upregulating TGF-beta and M-CSFR. Oncotarget 7, 80521–80542 (2016).
Saha, B., Kodys, K. & Szabo, G. Hepatitis C virus-induced monocyte differentiation into polarized M2 macrophages promotes stellate cell activation via TGF-beta. Cell. Mol. Gastroenterol. Hepatol. 2, 302–316 (2016).
Tang, P. M. et al. The proto-oncogene tyrosine protein kinase Src is essential for macrophage-myofibroblast transition during renal scarring. Kidney Int. 93, 173–187 (2018).
Anguita, E. & Villalobo, A. Ca(2+) signaling and Src-kinases-controlled cellular functions. Arch. Biochem. Biophys. 650, 59–74 (2018).
Skhirtladze, C. et al. Src kinases in systemic sclerosis: central roles in fibroblast activation and in skin fibrosis. Arthritis Rheum. 58, 1475–1484 (2008).
Wang, J. & Zhuang, S. Src family kinases in chronic kidney disease. Am. J. Physiol. Renal Physiol. 313, F721–F728 (2017).
Yan, Y. et al. Src inhibition blocks renal interstitial fibroblast activation and ameliorates renal fibrosis. Kidney Int. 89, 68–81 (2016).
Chen, Y. et al. Src-mediated ligand release-independent EGFR transactivation involves TGF-beta-induced Smad3 activation in mesangial cells. Biochem. Biophys. Res. Commun. 493, 914–920 (2017).
Wei, C. et al. Genomic analysis of kidney allograft injury identifies hematopoietic cell kinase as a key driver of renal fibrosis. J. Am. Soc. Nephrol. 28, 1385–1393 (2017).
Gieseck, R. L. III, Wilson, M. S. & Wynn, T. A. Type 2 immunity in tissue repair and fibrosis. Nat. Rev. Immunol. 18, 62–76 (2018).
Liu, L. et al. CD4+T Lymphocytes, especially Th2 cells, contribute to the progress of renal fibrosis. Am. J. Nephrol. 36, 386–396 (2012).
Liang, H. et al. The IL-4 receptor alpha has a critical role in bone marrow-derived fibroblast activation and renal fibrosis. Kidney Int. 92, 1433–1443 (2017).
Yan, J., Zhang, Z., Yang, J., Mitch, W. E. & Wang, Y. JAK3/STAT6 stimulates bone marrow-derived fibroblast activation in renal fibrosis. J. Am. Soc. Nephrol. 26, 3060–3071 (2015).
de Zeeuw, D. et al. The effect of CCR2 inhibitor CCX140-B on residual albuminuria in patients with type 2 diabetes and nephropathy: a randomised trial. Lancet Diabetes Endocrinol. 3, 687–696 (2015).
Xia, Y., Entman, M. L. & Wang, Y. CCR2 regulates the uptake of bone marrow-derived fibroblasts in renal fibrosis. PLOS ONE 8, e77493 (2013).
Chen, G. et al. CXCL16 recruits bone marrow-derived fibroblast precursors in renal fibrosis. J. Am. Soc. Nephrol. 22, 1876–1886 (2011).
Sakai, N. et al. Secondary lymphoid tissue chemokine (SLC/CCL21)/CCR7 signaling regulates fibrocytes in renal fibrosis. Proc. Natl Acad. Sci. USA 103, 14098–14103 (2006).
Bahjat, F. R. et al. An orally bioavailable spleen tyrosine kinase inhibitor delays disease progression and prolongs survival in murine lupus. Arthritis Rheum. 58, 1433–1444 (2008).
McAdoo, S. P. et al. Spleen tyrosine kinase inhibition attenuates autoantibody production and reverses experimental autoimmune GN. J. Am. Soc. Nephrol. 25, 2291–2302 (2014).
Ma, T. K., McAdoo, S. P. & Tam, F. W. Spleen tyrosine kinase: a crucial player and potential therapeutic target in renal disease. Nephron 133, 261–269 (2016).
Peyraud, F., Cousin, S. & Italiano, A. CSF-1R inhibitor development: current clinical status. Curr. Oncol. Rep. 19, 70 (2017).
Kanellis, J. et al. JNK signalling in human and experimental renal ischaemia/reperfusion injury. Nephrol. Dial. Transplant. 25, 2898–2908 (2010).
Ma, F. Y. et al. A pathogenic role for c-Jun amino-terminal kinase signaling in renal fibrosis and tubular cell apoptosis. J. Am. Soc. Nephrol. 18, 472–484 (2007).
van der Velden, J. L. et al. JNK inhibition reduces lung remodeling and pulmonary fibrotic systemic markers. Clin. Transl Med. 5, 36 (2016).
Olgen, S. Design strategies, structures and molecular interactions of small molecule Src inhibitors. Anticancer Agents Med. Chem. 16, 992–1002 (2016).
Berthier, C. C. et al. Enhanced expression of Janus kinase-signal transducer and activator of transcription pathway members in human diabetic nephropathy. Diabetes 58, 469–477 (2009).
Brosius, F. C. III & He, J. C. JAK inhibition and progressive kidney disease. Curr. Opin. Nephrol. Hypertens. 24, 88–95 (2015).
Tuttle, K. R. et al. JAK1/JAK2 inhibition by baricitinib in diabetic kidney disease: results from a phase 2 randomized controlled clinical trial. Nephrol. Dial. Transplant. 33, 1950–1959 (2018).
Tan, K. C. B. et al. Galectin-3 is independently associated with progression of nephropathy in type 2 diabetes mellitus. Diabetologia 61, 1212–1219 (2018).
Meng, X. M. et al. Treatment of renal fibrosis by rebalancing TGF-beta/Smad signaling with the combination of asiatic acid and naringenin. Oncotarget 6, 36984–36997 (2015).
Wu, H. et al. Single-cell transcriptomics of a human kidney allograft biopsy specimen defines a diverse inflammatory response. J. Am. Soc. Nephrol. 29, 2069–2080 (2018).
Souma, T. et al. Plasticity of renal erythropoietin-producing cells governs fibrosis. J. Am. Soc. Nephrol. 24, 1599–1616 (2013).
Zeisberg, E. M. et al. Endothelial-to-mesenchymal transition contributes to cardiac fibrosis. Nat. Med. 13, 952–961 (2007).
Zeisberg, E. M., Potenta, S. E., Sugimoto, H., Zeisberg, M. & Kalluri, R. Fibroblasts in kidney fibrosis emerge via endothelial-to-mesenchymal transition. J. Am. Soc. Nephrol. 19, 2282–2287 (2008).
Chen, Y. T. et al. Platelet-derived growth factor receptor signaling activates pericyte-myofibroblast transition in obstructive and post-ischemic kidney fibrosis. Kidney Int. 80, 1170–1181 (2011).
Li, J., Qu, X. & Bertram, J. F. Endothelial-myofibroblast transition contributes to the early development of diabetic renal interstitial fibrosis in streptozotocin-induced diabetic mice. Am. J. Pathol. 175, 1380–1388 (2009).
Iwano, M. et al. Evidence that fibroblasts derive from epithelium during tissue fibrosis. J. Clin. Invest. 110, 341–350 (2002).
Jinde, K. et al. Tubular phenotypic change in progressive tubulointerstitial fibrosis in human glomerulonephritis. Am. J. Kidney Dis. 38, 761–769 (2001).
Ng, Y. Y. et al. Tubular epithelial-myofibroblast transdifferentiation in progressive tubulointerstitial fibrosis in 5/6 nephrectomized rats. Kidney Int. 54, 864–876 (1998).
Anders, H. J. et al. The macrophage phenotype and inflammasome component NLRP3 contributes to nephrocalcinosis-related chronic kidney disease independent from IL-1-mediated tissue injury. Kidney Int. 93, 656–669 (2018).
Fukasawa, M., Campeau, J. D., Yanagihara, D. L., Rodgers, K. E. & Dizerega, G. S. Mitogenic and protein synthetic activity of tissue repair cells: control by the postsurgical macrophage. J. Invest. Surg. 2, 169–180 (1989).
Tamura, M., Aizawa, R., Hori, M. & Ozaki, H. Progressive renal dysfunction and macrophage infiltration in interstitial fibrosis in an adenine-induced tubulointerstitial nephritis mouse model. Histochem. Cell Biol. 131, 483–490 (2009).
Pan, B., Liu, G., Jiang, Z. & Zheng, D. Regulation of renal fibrosis by macrophage polarization. Cell Physiol. Biochem. 35, 1062–1069 (2015).
Quiroga, B., Arroyo, D. & de Arriba, G. Present and future in the treatment of diabetic kidney disease. J. Diabetes Res. 2015, 801348 (2015).
Saito, H. et al. Persistent expression of neutrophil gelatinase-associated lipocalin and M2 macrophage markers and chronic fibrosis after acute kidney injury. Physiol. Rep. 6, e13707 (2018).
Ma, T. K., McAdoo, S. P. & Tam, F. W. Targeting the tyrosine kinase signalling pathways for treatment of immune-mediated glomerulonephritis: from bench to bedside and beyond. Nephrol. Dial. Transplant. 32, i129–i138 (2017).
Dai, X. Y. et al. Targeting c-fms kinase attenuates chronic aristolochic acid nephropathy in mice. Oncotarget 7, 10841–10856 (2016).
Grynberg, K., Ma, F. Y. & Nikolic-Paterson, D. J. The JNK signaling pathway in renal fibrosis. Front. Physiol. 8, 829 (2017).
Brosius, F. C., Tuttle, K. R. & Kretzler, M. JAK inhibition in the treatment of diabetic kidney disease. Diabetologia 59, 1624–1627 (2016).
Perez-Gomez, M. V. et al. Horizon 2020 in diabetic kidney disease: the clinical trial pipeline for add-on therapies on top of renin angiotensin system blockade. J. Clin. Med. 4, 1325–1347 (2015).
Acknowledgements
The authors’ work is supported by grants from the Lui Che Woo Institute of Innovative Medicine (CARE programme), the Research Grants Council of Hong Kong (GRF 14106518, 14117418, 14117815, 14121816, 14163317, C7018-16G and TRS T12-402/13 N), the Health and Medical Research Fund (03140486 and 14152321), the Major State Basic Research Development Program of China (2012CB517705), a Direct Grant for Research from the Chinese University of Hong Kong (2017.002) and the National Health and Medical Research Council of Australia (1122073).
Reviewer information
Nature Reviews Nephrology thanks S. Ricardo, B. Conway and the other anonymous reviewer(s) for their contribution to the peer review of this work.
Author information
Authors and Affiliations
Contributions
P.M.-K.T. and D.J.N.-P. drafted the manuscript. H.-Y.L. and D.J.N.-P. supervised the design, writing and content of the manuscript. All authors reviewed and/or edited the final version of the manuscript and agree to be accountable for all aspects of the work.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Glossary
- Clodronate liposomes
-
Phospholipid bilayers (that is, liposomes) that encapsulate the cytotoxic drug clodronate; these liposomes are used for the depletion of phagocytic cells as they are selectively taken up by phagocytes and cause cell death.
- Fibrocytes
-
A population of immature myeloid cells in the bone marrow that differentiate into CD45+type I collagen+ fibroblast-like cells that are released into the circulation and can promote wound repair and tissue fibrosis.
- Tumour-associated macrophages
-
A subset of macrophages in the tumour microenvironment that inhibit immune cell-mediated destruction of tumour cells and promote tumour growth via stimulation of angiogenesis.
- Asiatic acid
-
A triterpenoid component extracted from Centella asiatica, which has anti-inflammatory and antifibrotic actions, including the increase in Smad7 expression.
- Naringenin
-
A flavonoid from grapefruit and citrus fruits that has anti-inflammatory properties, including inhibition of Smad3 function.
Rights and permissions
About this article
Cite this article
Tang, P.MK., Nikolic-Paterson, D.J. & Lan, HY. Macrophages: versatile players in renal inflammation and fibrosis. Nat Rev Nephrol 15, 144–158 (2019). https://doi.org/10.1038/s41581-019-0110-2
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41581-019-0110-2
This article is cited by
-
SP1 transcriptionally activates HTR2B to aggravate traumatic spinal cord injury by shifting microglial M1/M2 polarization
Journal of Orthopaedic Surgery and Research (2024)
-
The disruptor of telomeric silencing 1-like (DOT1L) promotes peritoneal fibrosis through the upregulation and activation of protein tyrosine kinases
Molecular Biomedicine (2024)
-
The pathogenic role of succinate-SUCNR1: a critical function that induces renal fibrosis via M2 macrophage
Cell Communication and Signaling (2024)
-
Atg5 deficiency in macrophages protects against kidney fibrosis via the CCR6-CCL20 axis
Cell Communication and Signaling (2024)
-
Endothelial CXCR2 deficiency attenuates renal inflammation and glycocalyx shedding through NF-κB signaling in diabetic kidney disease
Cell Communication and Signaling (2024)