Abstract
The adaptive immune response to influenza virus infection is multifaceted and complex, involving antibody and cellular responses at both systemic and mucosal levels. Immune responses to natural infection with influenza virus in humans are relatively broad and long-lived, but influenza viruses can escape from these responses over time owing to their high mutation rates and antigenic flexibility. Vaccines are the best available countermeasure against infection, but vaccine effectiveness is low compared with other viral vaccines, and the induced immune response is narrow and short-lived. Furthermore, inactivated influenza virus vaccines focus on the induction of systemic IgG responses but do not effectively induce mucosal IgA responses. Here, I review the differences between natural infection and vaccination in terms of the antibody responses they induce and how these responses protect against future infection. A better understanding of how natural infection induces broad and long-lived immune responses will be key to developing next-generation influenza virus vaccines.
Similar content being viewed by others
Introduction
Influenza viruses cause mild to severe respiratory infections in humans and are a major public health problem. According to the World Health Organization, seasonal influenza viruses — including the H1N1 and H3N2 influenza A viruses, as well as influenza B viruses — cause approximately 3–5 million severe cases and 290,000–650,000 deaths each year worldwide1,2. In addition, avian influenza viruses, such as H5N1, H7N9 and others, can cause significant numbers of zoonotic infections3,4. At irregular intervals, viruses from the animal reservoir cross the species barrier — usually through a re-assortment step between an avian influenza virus and a human influenza virus, in a process that results in antigenic shift — and cause pandemics5,6,7. The morbidity and mortality associated with these pandemics can exceed that of seasonal influenza virus epidemics, and such pandemics can cause millions of deaths. The prime example is the H1N1 influenza virus pandemic of 1918, which resulted, according to conservative estimates, in 40 million deaths8. The 1918 H1N1 virus pandemic was followed by an H2N2 virus pandemic in 1957, an H3N2 virus pandemic in 1968 and another H1N1 virus pandemic in 2009 (ref.7).
Pandemics are typically caused by viruses that feature surface glycoproteins — haemagglutinin (HA) and neuraminidase (NA) — to which the human immune system is relatively naive. This was the case in 1918, when the majority of the population seemed to be naive for both the H1 HA and the N1 NA, and in 1957, when there was little population immunity to both H2 and N2 (ref.5). In 1968, only the H3 HA was newly introduced to humans, whereas the N2 of the H3N2 pandemic virus was derived from the previously circulating H2N2 virus5,7. In 2009, a seasonal H1N1 virus was circulating in humans, but the incoming pandemic H1N1 virus had antigenically distinct H1 and N1 surface glycoproteins6. Owing to the lack of population immunity, these emerging pandemic viruses initially spread quickly through the human population. However, within a few years they had become seasonal viruses that then typically cause epidemics with lower case fatality rates than pandemics9. Widespread infection during the pandemic phase induces significant population immunity, mostly in the form of antibody responses against HA and NA.
Antibody responses to the influenza virus surface glycoproteins, specifically to HA, have long been known to be protective against influenza virus infection10, and specific antibodies against HA have been identified as a correlate of protection11. Even in the first report describing the isolation of influenza virus in 1933, serum antibody was shown to be protective10. The lack of antibody-based population immunity is the main factor that enables emerging pandemic viruses to spread quickly throughout the whole population. The evolutionary pressure exerted by antibody responses (together with other factors and random events), mostly from natural infection, forces the virus to change its surface antigens, usually by introducing point mutations, in a process known as antigenic drift. Importantly, the influenza virus HA, specifically the globular head region, shows considerable plasticity and is very tolerant to these changes12,13,14. Antigenic drift is the key reason why influenza virus vaccines have to be updated on an annual basis15. If the virus strains used in the vaccine are not antigenically well matched to the circulating virus strains, the vaccine effectiveness decreases sharply16,17. Obviously, this is also true for novel, antigen-shifted pandemic viruses, for which antigenically matched vaccines need to be produced. Therefore, it is hard to overstate the importance of the antibody response to influenza virus. Of note, innate immune responses and T cell responses significantly contribute to protection against influenza viruses and are essential for the induction of robust antibody responses. However, owing to space limitations, this Review focuses only on the antibody response.
Antibody responses to influenza viruses have been studied for a long time. Specifically, in the past few years, with the advent of technologies that enable the analysis of antibodies produced by single human B cells18, we have made quantum leaps in understanding the antibody response to influenza virus. Nevertheless, there are many gaps in our knowledge. We understand that antibody responses induced by natural infection are usually broader and longer-lived than antibody responses induced by vaccination, but the mechanisms behind this are unclear. Uncovering these mechanisms would help to improve current vaccines. We have also recently discovered broadly neutralizing human antibodies that target influenza viruses19. Understanding how these antibodies are induced could be the crucial step towards the holy grail of a universal influenza virus vaccine. Here, I review the antibody response to natural influenza virus infection, the functionality of the different types of antibody, antibody responses to current influenza virus vaccines, antibody responses to avian influenza virus immunogens (which represent an extraordinary challenge for the immune system) and next-generation broadly protective or universal influenza virus vaccines. This discussion touches upon important concepts in influenza virus immunology, including original antigenic sin (OAS)-like phenomena, immunodominance, the structure and function of different antibody isotypes and B cell dynamics, although these topics are not covered in detail owing to space constraints. The majority of this Review focuses on responses to influenza A viruses, but studies of influenza B viruses (recently reviewed elsewhere20,21) are included where appropriate.
Responses to natural infection
The genome of influenza A and B viruses consists of eight genomic segments, which encode 11 or more proteins. All of these proteins could potentially be targeted by the antibody response, but not all are targeted in the same way and the consequences of the immune response depend strongly on the target. To better understand this, it is necessary to familiarize ourselves with the life cycle of the virus (Fig. 1). From this, it becomes clear which viral proteins are easily accessible to antibodies and B cell receptors. Both HA and NA are accessible on virions and infected cells (with a larger number of HA trimers than of NA tetramers being present). Parts of the influenza A virus M2 ion channel are also accessible, mostly on the surface of infected cells. In addition, patches of nucleoprotein (NP) on the surface of infected cells have been reported22. Finally, it is likely that some internal viral proteins — matrix protein (M1), NP, the polymerases (PB1, PB2 and PA), non-structural protein 1 (NS1) and the nuclear export protein (NEP) — become accessible in cells that die after influenza virus infection.
Influenza viruses enter the body via the mucosal surfaces, where they are bound by terminal sialic acid residues on mucins199 through haemagglutinin (HA) on the virion. This is thought to be a natural defence mechanism against host cell binding200. Neuraminidase (NA) releases the trapped virus by cleaving off the terminal sialic acid residues89,201. This helps the virus to penetrate the mucosal fluid and to reach its target cells, where it attaches to sialylated host cell receptors and is endocytosed. During these steps, influenza viruses are visible to the immune system and could potentially induce an antibody response, probably to surface-exposed HA and NA (part a). The target cell endosome is then acidified, triggering HA-mediated fusion of endosomal and viral membranes. The viral genome is released and enters the nucleus, where viral RNA (vRNA), copy RNA (cRNA) and mRNA are generated, leading to protein expression. HA, NA and the influenza A virus M2 ion channel travel to the cell surface via the endoplasmic reticulum and the Golgi apparatus. Internal viral proteins, including matrix protein (M1), nucleoprotein (NP), the polymerases (PB1, PB2 and PA) and nuclear export protein (NEP), are packaged into the budding virus at the cell membrane, with HA and NA on the surface. Non-structural protein 1 (NS1), PB1-F2 and PA-X are typically not packaged into virions. At the cell surface, HA, NA and M2 proteins can be detected by B cells, and an immune response against these proteins can be induced (part b). Viral NP, although typically only found inside cells, has also been detected on patches on the cell surface and could be recognized by B cells there also22 (part c). The nascent virus particles stick to the cell membrane of the host cell as a result of the interaction between HA and sialic acids. This is counteracted by the activity of NA, which releases the virus by cleaving off the terminal sialic acid residues (part d). During this step, HA and NA are accessible, but only a very low copy number of M2 is found on virions, and the virus membrane shields the internal proteins from recognition by B cells. Finally, to yield infectious virus, the HA has to be cleaved into HA1 and HA2 subunits by host proteases that are present in the respiratory tract (this process is slightly different for highly pathogenic avian influenza viruses). Dying cells and cell debris might present all expressed influenza virus proteins in an accessible form to B cells (part e). Pol, polymerase.
Thus, it is evident from studying the life cycle of the influenza virus that not all influenza virus antigens are expressed to similar levels and/or are similarly accessible to B cell receptors. These differences significantly influence the immune response to the virus. Owing to the importance of HA-specific antibodies for immune protection, polyclonal responses to this protein were studied early on using various methods, including the haemagglutination inhibition assay and different forms of neutralization assay. Typically, it is assumed that the majority of antibodies induced by natural infection will target HA, with lower-level responses to NA and internal proteins being induced also. In fact, natural infection has been shown to induce seroconversion in a large majority of infected individuals, as assessed by the haemagglutination inhibition assay and other assays such as the enzyme-linked immunosorbent assay (ELISA) and the microneutralization assay23,24,25,26. Typically, the antibody response to influenza virus as measured by haemagglutination inhibition is relatively robust, although a very small number of individuals may not seroconvert as measured by this assay26.
Finally, it is important to keep in mind that immune responses to influenza virus HA and NA in humans are very complex as a result of prior exposure to historic virus strains, either by infection or vaccination27, which can result in imprinting. Most children under the age of 2 years are likely to have already had an immune response against influenza virus28. Therefore, we must distinguish between a de novo immune response to influenza virus in a naive subject and a (at least partial) recall immune response, which is significantly influenced by prior exposure and the phenomena of imprinting and/or OAS (Box 1).
Antibodies to haemagglutinin
The breadth of the response to HA that is induced by natural influenza virus infection depends on the exposure history of the infected individual. Children typically mount narrower responses than adults, who might — depending on their exposure histories — induce a broader response that includes the induction of antibodies to a historic virus strain to which they have been previously exposed as well as the infecting virus strain (these OAS-type effects are discussed in Box 1). This breadth of the antibody response can be observed in terms of haemagglutination inhibition and microneutralization titres, but it is more evident when antibody binding to HA is assessed24,29. As an example, it has been shown that HA-binding antibody responses after pandemic H1N1 virus infection are very broad, often extending to other group 1 HA proteins, whereas H3N2 virus infection in humans induced a narrower response24. Importantly, HA is composed of two structurally and functionally distinct domains: the variable, immunodominant globular head domain (formed by the central part of HA1) and the conserved, immunosubdominant stalk domain (formed by the carboxyl and amino termini of HA1 plus the ectodomain of HA2)30 (Box 2). Antibodies that bind to the head domain of HA typically have potent neutralizing activity and often have haemagglutination inhibition activity. They target relatively distinct antigenic sites, including Sa, Sb, Ca1, Ca2 and Cb for H1 (ref.31); A, B, C, D and E for H3 (refs32,33); and the 120, 150 and 160 loops and the 190 helix for the HA of influenza B viruses34. However, as a result of antigenic drift, which may include significant rearrangement of N-linked glycans in the HA head domain35 and thus affect glycan shielding, many of these antibodies are strain-specific. Antibodies towards the stalk domain of HA are widely prevalent, although at very low levels, and they can be induced by virus infection to a certain extent28,36,37. HA stalk-specific antibodies, which have been isolated from humans, can bind to a broad range of virus isolates and subtypes. Typically, these antibodies bind within group 1 HA proteins, within group 2 HA proteins or within influenza B virus HA proteins38,39. In addition, rare HA stalk-specific monoclonal antibodies that bind across virus groups, and even across both influenza A and B viruses, have been isolated40,41. Importantly, these antibodies have neutralizing activity and protect animals from lethal virus challenge in passive transfer experiments. This class of antibodies probably forms the majority of the cross-reactive antibodies that are induced by natural infection in some cases24. On a monoclonal level, analysis of the plasmablast response after infection (Box 3) showed that approximately 25–52% of plasmablasts bind to HA after infection with H1N1 or H3N2 viruses42. A proportion of the induced antibodies are cross-reactive with more than one virus strain, which confirms the serological analysis. The first infection with pandemic H1N1 virus in 2009–2010, which is a special case in that it has a highly conserved HA stalk domain that shares epitopes with seasonal H1 protein (see Responses to pandemic and zoonotic viruses), also induced an antibody response to the HA stalk, with monoclonal antibodies binding to several group 1 HA proteins and therefore exhibiting exceptional breadth43.
Antibody responses induced by natural infection can be very long-lived. For example, individuals infected with H1N1 virus in the first half of the 20th century still had positive serum haemagglutination inhibition titres against the 1918 H1N1 virus in 2008 (ref.44). In addition, older individuals were protected against the pandemic H1N1 virus strain in 2009 although they had not been exposed to an antigenically related virus for more than 50 years, whereas younger individuals were not as well protected45,46. In this case, the argument can be made that continuous exposure to antigenically non-related H1N1 viruses kept serum antibody levels high. However, individuals exposed to H1N1 virus before 1957 and who had not been exposed to H1N1 virus between 1957 and 1977 (because no H1N1 virus was circulating) had protective immunity against antigenically similar viruses that re-appeared in 1977 (ref.47). In addition, it has been shown that individuals exposed in the past to H2N2 virus — which disappeared from the population in 1968 — still have high haemagglutination inhibition titres and H2-specific binding titres against H2N2 virus24,48. From these results, it can be concluded that antibody-based immunity to HA induced by natural infection is long-lived (more than 50 years) and might perhaps be lifelong. This is true not only for antibodies that target the globular head domain of HA but likely also for antibodies that target the conserved, immunosubdominant stalk domain (although they are present at lower titres)28,37,49,50.
Antibodies to neuraminidase
Antibodies towards the second surface glycoprotein, NA51, are also induced by natural infection, although typically at lower levels than antibodies to HA. They are usually measured using neuraminidase inhibition assays or ELISA51. NA has been described to be immunosubdominant when presented to the immune system together with HA52 (Box 2). In addition, this phenomenon might be enhanced by the higher copy number of HA on infected cells and virions53. Individuals of all age groups have detectable antibody titres against NA, with older individuals typically having higher titres54, which is similar to findings for HA. At a monoclonal level, the anti-NA response after H1N1 or H3N2 virus infection constitutes approximately 14–35% of the induced plasmablasts42 (Box 3), which is smaller than the plasmablast response to HA. Importantly, a large proportion of the NA-specific monoclonal antibodies isolated after natural infection bound broadly to current and historic virus strains, inhibited NA activity and provided protection in an antibody transfer challenge study in mice42. Of note, the titres of antibodies against N1 (which is a member of the group 1 NA proteins) seem to be lower than the titres of antibodies against N2 (a member of the group 2 NA proteins) or against influenza B virus NA in humans24,54. This might be caused by the lower immunogenicity of N1, but it could also be an artefact of the reagents that are used to measure these antibody titres. Importantly, it is known that antibodies against NA can be broadly reactive, at least within the virus subtype. Similarly to HA-specific antibodies, NA-specific antibodies induced by natural infection seem to be present for many decades54. It is unclear whether this is the result of OAS-like back-boosting when new strains are encountered (Box 1) or is due to persistent levels of plasma cells that secrete antibody without re-stimulation (as in the case of H2-specific antibodies and some H1-specific antibodies).
Antibodies to nucleoprotein
During natural infection, all influenza virus proteins are expressed in infected cells and can potentially induce an antibody response, although some of these proteins are more accessible than others. Antibodies to NP have been reported after natural virus infection and in the serum of healthy individuals. In early work, several groups reported that NP-specific antibody levels after natural infection with H1N1 or H3N2 virus strains increased significantly in 72–88% of individuals55,56,57. The anti-NP response was relatively durable in some individuals, lasting for up to 1 year57. Another study found that between 77% and 83% of healthy influenza vaccine recipients had NP-reactive antibodies at baseline, presumably owing to natural infection58. Interestingly, a recent analysis of memory B cells (Box 3) specific for the influenza A virus NP from four healthy volunteers revealed a high diversity of NP-specific antibody lineages with extensive clonal diversification, which suggests that these B cells have undergone repeated stimulation through exposure to influenza A virus NP59.
Antibodies to M1, M2 and other viral proteins
M1 is also immunogenic, and it has been shown that natural infection with H3N2 virus induces M1-reactive antibodies in approximately 35% of individuals55. However, another study found M1-specific antibody in only 1% of study participants before experimental infection with different H1N1 and H3N2 wild-type and re-assortant viruses, and only 6% of study participants had an increase in M1-specific antibody titre after infection60. Interestingly, it was suggested that the anti-M1 response is greater after influenza B virus infection than after influenza A virus infection61. Recent studies that looked at the effector functions of M1-specific and NP-specific antibodies in human sera after natural virus exposure, as well as in the therapeutic product intravenous immunoglobulin, found that these antibodies are relatively prevalent62,63. For M2 — which presents its ectodomain (M2e) on the surface of infected cells and virions — seroconversion rates after infection have been determined to be between 16% and 45% of individuals, involving relatively low antibody titres and short-lived responses56,64,65. A study examining the anti-M2 response after pandemic H1N1 virus infection detected an increase in antibody titre in 50% of individuals and found a general increase in antibody titres with age and a better induction of M2-specific antibodies in individuals who had pre-existing titres of these antibodies66. In addition to NP, M1 and M2 proteins, there is some evidence from monoclonal antibody isolation and from antigenic fingerprinting that natural infection also induces antibodies against PB2, PB1, PA, NS1, NEP and PB1-F2 proteins, although the magnitude and quality of these responses is not well defined67,68,69,70. Given that most of the influenza A virus internal proteins are highly conserved, it is likely that these antibodies can bind broadly within influenza A virus subtypes.
Mucosal versus systemic responses
The mucosal surfaces of the respiratory tract are the entry port for respiratory pathogens, including influenza viruses. These surfaces feature many natural defence proteins, such as mucins, that have antiviral functions and can interact with antibodies. The types of antibody and antibody titres found at mucosal surfaces are somewhat distinct from those that are found in the serum. Importantly, there are also distinctions between the upper and lower respiratory tracts. The lower respiratory tract is mainly protected by IgG (with an IgG:IgA ratio of 2.5:1), which is probably actively transported there by the neonatal Fc receptor (FcR)71,72. It can be assumed that antibody levels in the lower respiratory tract mirror, to some degree, antibody levels in the serum. The antibody response in the upper respiratory tract is dominated by IgA (with an IgG:IgA ratio of 1:3)71, specifically by dimeric IgA1, which has a secretory component73 (Box 4). These IgA molecules are produced by plasma cells in the mucosa-associated lymphoid tissue, primarily in the lamina propria, and are then actively transported to mucosal surfaces through interactions with the polymeric immunoglobulin receptor. Whereas the systemic immune response to influenza virus infection is relatively well studied, few data are available for mucosal immune responses to natural infection (although more data are available regarding mucosal immune responses to vaccination (see below)). However, it is assumed that the mucosal IgA response targets approximately the same antigens as the IgG response but might produce more broadly reactive antibodies, probably owing to the enhanced avidity that results from their multimeric (mostly dimeric) nature74.
Antibody-based mechanisms of protection
Antibodies to different influenza virus proteins exhibit different antiviral mechanisms, and not all antibodies contribute equally to protection (Fig. 2).
Antibodies can interfere with different stages of the viral life cycle. The upper respiratory tract is mostly protected from influenza virus by secretory IgA1, whereas IgG1 is dominant in the lower respiratory tract. a | Neuraminidase (NA) activity, which frees incoming virions from decoy receptors on mucins, can be blocked by NA-specific antibodies. b | The interaction between haemagglutinin (HA) and sialylated host cell receptors can be blocked by antibodies with haemagglutination inhibition activity that bind to the HA head domain. c | Fusion of viral and endosomal membranes can be blocked by HA stalk-targeted antibodies that lock HA in a pre-fusion conformation (the antibodies bind outside the cell and are taken up with the virus (not shown)). d | NA activity is required for viral release from the host cell as the HA of nascent virions binds to sialic acid on the host cell surface. This activity is blocked by direct binding of antibodies to NA or by steric hindrance mediated by antibodies that bind to the head or the stalk of HA. e | HA needs to be cleaved into HA1 and HA2 subunits to produce infectious virus particles. This typically happens once the virus is released from the cell and is mediated by airway proteases. However, HA stalk-specific antibodies bind close to the cleavage site of HA and inhibit this process. f | Antibodies to the HA stalk and to NA and M2 proteins can trigger Fc receptor (FcR)-mediated effector functions against infected cells, such as antibody-dependent cell-mediated cytotoxicity (ADCC) and antibody-dependent cellular phagocytosis (ADCP). This might also involve ADCP of virions. It is unclear what role antibodies against nucleoprotein (NP) and other internal proteins have with regard to this mechanism. g | Antibodies to the HA stalk have also been shown to activate complement, which can lead to the killing of infected cells. cRNA, copy RNA; M1, matrix protein; NEP, nuclear export protein; NS1, non-structural protein 1; Pol, polymerase; vRNA, viral RNA.
Antibodies to haemagglutinin
Antibodies to the head domain of HA, which includes the receptor-binding domain, typically block the interaction between the virus and its host cell receptor, sialic acid. This blocking may occur through steric hindrance of the HA–receptor interaction or by direct binding of the antibody to the receptor-binding pocket of HA (which is typically achieved by antibodies having a long CDR3 region that mimics sialic acid to a certain degree75). The action of these types of antibody neutralizes the virus before infection is initiated, and it can typically be measured by in vitro neutralization assays or — as a surrogate for neutralization — by haemagglutination inhibition assays that directly measure the inhibition of HA binding to sialic acids on red blood cells. Importantly, not all neutralizing antibodies that bind to the HA head are necessarily active in the haemagglutination inhibition assay76,77. Nevertheless, haemagglutination inhibition titres have been established as a correlate of protection and are widely accepted as a readout for vaccine efficacy studies by regulatory agencies11,78,79. It is assumed that a 1:40 titre of antibodies with haemagglutination inhibition activity will reduce the risk of getting an infection with seasonal H1N1 virus, H3N2 virus or influenza B viruses by 50%. However, this has only been tested with a limited number of virus strains and might not apply to infections with pandemic or zoonotic influenza viruses or to all age groups.
Antibodies to the stalk domain of HA also neutralize incoming viruses, but through a different mechanism and at a different stage of the virus life cycle. Of note, HA stalk-targeting antibodies bind to a broad range of viruses within and across subtypes owing to the conservation of their target antigens39. This is a unique trait and sets these antibodies apart from HA head-specific antibodies, which typically have a narrow binding range. Antibodies to the stalk domain bind to HA on virions but do not block attachment of the virions to host cells or their endocytosis30. However, some of these antibodies lock the HA molecule into the pre-fusion conformation and therefore inhibit fusion of viral and host endosomal membranes and subsequent release of the viral genome80. This neutralization mechanism has also been reported for some HA head-specific antibodies that are not active in haemagglutination inhibition assays81. In addition, HA stalk-specific antibodies, as well as some HA head-specific antibodies, have been implicated in inhibiting viral egress40,82. The mechanism of this activity is unclear and could be caused by direct interaction of the antibody with HA or by steric hindrance of NA (as NA activity is crucial for the release of nascent virions)53. Finally, HA stalk-specific antibodies that bind to HA0 block access of proteases to the HA1–HA2 cleavage site, resulting in virus particles with immature HA0 on their surface, which makes them non-infectious83. Importantly, HA stalk-specific antibody titres measured by ELISA have recently been shown to be an independent correlate of protection against natural influenza virus infection (F.K., unpublished observations). Activity in microneutralization assays — which can be attributed to the activities of HA head-specific antibodies but also HA stalk-specific antibodies (as outlined above) — has also been shown to correlate with protection84,85, but this is not an accepted correlate of protection for regulatory agencies. An additional correlate of protection, the single radial haemolysis titre, is an accepted correlate of protection by the European Medicines Agency (EMA)86,87.
Antibodies to neuraminidase
Antibodies against NA also have direct antiviral activity51. Antibodies targeting NA can inhibit its enzymatic activity, either by direct binding to the active site or by steric hindrance of the NA–substrate interaction. Of note, HA-reactive antibodies (against both the stalk and the head of HA) can also have anti-NA activity by steric hindrance54,88. The inhibition of NA activity can have several consequences. Incoming virions can be bound by mucins and other natural defence proteins that carry sialylated glycans to which HA binds. NA activity is required to free the virus from these decoy receptors to move on and infect cells89. In addition, the HA of budding virus particles can bind to sialic acid on the surface of the infected cells from which the virus particles are trying to detach. NA activity removes sialic acid from the cell surface, which ensures the efficient release of progeny virus53. Also, virus particles may aggregate through binding to glycans on the HA of neighbouring virus particles or through binding to mucins51. Such aggregation could have a negative impact on virus transmission, but NA activity might resolve this aggregate formation. Finally, NA has immunomodulatory activity (for example, by cleaving transforming growth factor-β)90. All of these viral activities can be inhibited by NA-reactive antibodies. Importantly, NA inhibition activity has been identified as an independent correlate of protection in both field studies and human challenge trials26,78,91.
FcR-mediated effector functions
In addition to direct antiviral activity, antibodies to HA and NA might have indirect antiviral effects. In particular, HA stalk-specific antibodies have been shown to have FcR-mediated effector functions, such as antibody-dependent cell-mediated cytotoxicity (ADCC) and antibody-dependent cellular phagocytosis (ADCP), and to mediate complement-dependent lysis92,93. This is also true for some HA head-specific antibodies that do not show haemagglutination inhibition activity77,94. By contrast, haemagglutination inhibition-active monoclonal antibodies usually have only weak FcR-mediated effector functions as they block contact between HA and sialic acid on effector cells (which occurs in addition to the required Fc–FcR interactions), which seems to reduce this activity95,96. Importantly, NA-specific antibodies have also been shown to be active in ADCC reporter assays97. Although FcR-mediated effector functions have not yet been shown to correlate with protection against influenza virus in humans, they have been shown to correlate with the protection of mice that received a passive transfer of human sera followed by virus challenge98. M2-specific antibodies in mice also protect against influenza virus infection via FcR-mediated effector functions99. Again, these have not been shown to correlate with protection in humans thus far, but it is notable that a human M2e-specific monoclonal antibody significantly reduced viral loads in a human challenge study100.
Antibodies to internal proteins
Whereas the protective role of antibodies against HA and NA seems clear, the antiviral activity of antibodies against internal proteins has been less well studied. Owing to the relative inaccessibility of their targets on live, infected cells and viruses, these antibodies have no direct antiviral activity. Interestingly, in a mouse model, antibodies against NP can provide weak protection against influenza virus infection101,102. In addition, M1-specific and NP-specific antibodies have recently been shown to activate immune effector cells (natural killer cells)62. However, no killing activity was observed. Therefore, the protective role of antibodies to internal influenza virus proteins is unclear.
Responses to vaccination
Different types of influenza virus vaccines are currently in use or have been used historically (Box 5), including whole inactivated virus vaccines, split virus and subunit vaccines, live-attenuated influenza virus vaccines (LAIVs) and recombinant HA-based vaccines.
Whole inactivated virus vaccines
Whole inactivated virus vaccines have been used extensively in humans and are very well studied in animal models because they are easy to generate in research laboratories. Of note, this type of vaccine is currently not in use in most parts of the world owing to relatively high levels of reactogenicity (Box 5). Depending on the inactivation method that is used, inactivated viruses represent antigens of live virus relatively well and might preserve functions such as haemagglutination and fusion of HA as well as NA activity. Whole inactivated virus vaccines also contain viral RNA, which might activate innate immune sensors such as retinoic acid inducible gene I (RIG-I), Toll-like receptor 3 (TLR3), TLR7 and TLR8 (ref.103) and potentially others, thereby giving these types of vaccine a self-adjuvanting effect. The immune response induced by these vaccines has been described as being relatively balanced, leading to a response to HA as well as NA in both humans and animal models, with relatively high seroprotection rates in humans (more than 85%)42,104,105,106. However, direct comparisons have shown that split virus vaccines and/or subunit vaccines induce similar immune responses to whole inactivated virus vaccines, at least in terms of seroconversion and geometric mean haemagglutination inhibition titres58,107, with one report even showing that split virus vaccines slightly outperformed whole inactivated virus vaccines108.
Split virus or subunit vaccines
Split virus or subunit vaccines are manufactured using whole inactivated virus that is then treated with detergent and further purified. Depending on the downstream purification process, this results in preparations containing parts of the viral membrane carrying HA and NA (split virus vaccine) or almost pure glycoprotein (HA) preparations (subunit vaccine). Most of the viral RNA is removed during the purification process, which leads to reduced reactogenicity but might also lead to reduced immunogenicity. Furthermore, less is known about the structural integrity of HA and NA proteins in split virus and subunit vaccines and the preservation of crucial antibody-binding epitopes. The NA content of these vaccines is not standardized and was found in some cases to be very low109. The immune response after vaccination with split virus or subunit vaccines is typically targeted towards HA, with haemagglutination inhibition seroconversion rates (defined as a fourfold increase in antibody titre) between 20% and 77% and microneutralization seroconversion rates (also defined as a fourfold increase in antibody titre) between 47% and 90%26,110.
The anti-NA titres induced in response to split virus or subunit vaccines vary and depend on how they are measured. One study reported seroconversion rates between 23% and 73% for antibodies to N1 and N2 proteins, with seroconversion defined as a twofold increase in antibody titre110. However, the increases in antibody titre in this study were only between 0.61-fold (a decrease) and 2.04-fold. In another study, in which seroconversion was defined as a fourfold increase in antibody titre, the seroconversion rate for NA-specific antibodies was determined to be 36.5%26. Antibodies against internal proteins can also be induced by vaccination; however, as for NA, the content of NP, M1 and other internal proteins in split virus and subunit vaccines is likely to depend on the specific vaccine, the season and probably even the batch of vaccine, as vaccine content is standardized only for HA. Increases in NP-specific antibody titres after vaccination have been found in 27–87% of vaccine recipients58,108,111, and significant increases in M1-specific antibody titres have been detected as well111 (although they were not detected in other studies108). The majority of these findings are reflected on a monoclonal level in the plasmablast population. A recent study found that between 81% and 90% of plasmablasts (Box 3) induced in response to split virus or subunit vaccines are HA specific, 1–2% of plasmablasts are NA specific and the remaining cells have other targets, such as internal proteins42. Earlier studies found somewhat lower estimates for HA-specific plasmablasts (40−62.4%)18,112. Nevertheless, it is safe to say that the immune response to split virus and subunit vaccines at both polyclonal and monoclonal levels is dominated by the response to HA. Importantly, vaccine-induced monoclonal antibodies have significantly lower levels of cross-reactivity than do antibodies induced by infections, which confirms serological findings112,113.
The breadth of the antibody response to whole inactivated virus vaccines and to split virus or subunit vaccines has been widely evaluated. These vaccines can induce cross-reactive antibody responses to historic virus strains (Box 1) in adults with pre-existing immunity108,114. However, they typically do not induce significant titres of cross-reactive HA stalk-specific antibodies36,98. Importantly, antigenic mismatches between circulating virus and vaccine virus strains usually result in a marked decrease in vaccine effectiveness16,17,115,116. Compared with natural influenza virus infection, the responses induced by vaccination with whole inactivated virus vaccines or split virus or subunit vaccines are therefore relatively narrow and strain specific.
Recombinant haemagglutinin vaccines
Recombinant HA vaccines have been licensed only recently but have been studied extensively in human clinical trials. As they contain only HA, the immune response targets only HA. These vaccines contain higher doses of HA (45 μg of HA per strain) than split virus or subunit vaccines, but it is important to note that as the HA is expressed in insect cells, the antigens have smaller glycans117. Nevertheless, it has been shown that the antibody response to these recombinant vaccines is at least comparable to that induced by whole inactivated virus vaccines or split virus or subunit vaccines. There is some evidence to suggest that recombinant HA vaccines induce broader responses and better protection, specifically in elderly individuals118,119. In addition, as the HA is expressed recombinantly, it does not contain the mismatches that can occur in regular vaccine seed strains owing to virus adaptation to growth in eggs115 (Box 5).
Live-attenuated virus vaccines
The vaccines detailed above are typically administered intramuscularly and sometimes intradermally, and it is unclear whether these routes of administration induce mucosal immune responses in the upper respiratory tract120. It is possible that some degree of mucosal immunity in the upper respiratory tract is induced through these vaccination routes in humans who have been primed by natural influenza virus infection. By contrast, LAIVs are typically administered to the nose and replicate in the upper respiratory tract. The immune response to LAIVs is multifaceted and does not necessarily involve a serum antibody response; LAIVs have been licensed on the basis of efficacy trials that measure protection rather than correlates of protection. Studies in adult recipients of LAIVs found seroconversion rates of 3–7% for haemagglutination inhibition, 3–13% for neutralization and 0–17% for NA inhibition110. Slightly higher rates of seroconversion (21.2%, 16.7% and 6.2%, respectively) have been found in another study in adults26. Seroconversion in adults in terms of mucosal IgA responses seems to be higher (at 33%) than serum antibody-based seroconversion121. By contrast, LAIVs can induce serum antibody responses, including relatively high haemagglutination inhibition titres,122,123 as well as mucosal IgA responses123,124 in children. Antibody titres towards the stalk domain of HA have been detected after LAIV administration in children, but these antibodies were not induced to high levels122.
As discussed above, natural infection with influenza viruses can induce long-lived immune responses that potentially provide lifelong protection against specific virus strains. It has been reported that the antibody response to vaccination is much more short-lived and that vaccine effectiveness and antibody titres can wane even within a season125,126,127,128,129,130,131. A direct comparison between inactivated virus vaccines and LAIVs in children suggests that antibody responses induced by LAIVs persist significantly longer123. The differences in immune responses to natural influenza virus infection and vaccination are compared in Table 1.
Responses to pandemic and zoonotic viruses
Humans are typically exposed to seasonal influenza viruses, including H1N1 virus, H3N2 virus and influenza B viruses, through natural infection and/or vaccination. A proportion of the general population has also been exposed to H2N2 virus, which circulated between 1957 and 1968. The introduction of a new pandemic virus strain, as occurred in 2009 with the pandemic H1N1 virus, poses an extraordinary challenge to the immune system. Before 2009, humans had been widely exposed to seasonal H1N1 viruses. The HA expressed by these seasonal viruses is markedly different from the HA expressed by the 2009 pandemic H1N1 virus, although they are of the same HA subtype. However, the differences are not equally distributed within the H1 HA protein. The head domains of seasonal and pandemic H1 proteins differ greatly (having ~68% amino acid identity), whereas the stalk domains are highly conserved (having ~88% amino acid identity). In addition, some specific epitopes of the head domain are shared between seasonal and pandemic H1 proteins. Therefore, first exposure to the 2009 pandemic H1N1 virus triggered a recall response of those B cells that recognized the conserved, shared epitopes, which led to a significant response to the HA stalk (Box 1). This response was observed after both natural infection and vaccination43,113,132,133,134,135. It has been hypothesized that this increase in the production of cross-reactive antibodies led to the disappearance of seasonal H1N1 viruses after the emergence of the 2009 pandemic H1N1 virus43.
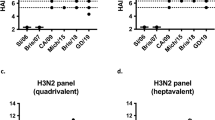
In rare cases, humans with pre-existing immunity to seasonal influenza virus strains are also exposed to zoonotic infections — for example, with H5N1, H6N1, H7N9 or H10N8 virus strains. In addition, owing to the pandemic potential of H5N1 and H7N9 viruses, vaccines against those virus subtypes have been manufactured and tested on a relatively large scale in humans. For the human immune system, these antigens are at least partially novel. Humans typically do not have pre-existing immunity to the head domains of H5 or H7 proteins. However, the stalk domain of the H5 HA (a group 1 HA) has conserved epitopes shared with H1 and H2 HA proteins (also group 1 HA proteins), and the stalk domain of H7 HA (a group 2 HA) has conserved epitopes shared with H3 HA (also a group 2 HA). Upon exposure to H5 HA, the immune system recognizes the HA stalk and induces a recall response of stalk-specific memory B cells, which results in a large expansion of stalk-specific plasmablasts and a significant antibody response to the HA stalk136,137 (Box 1). Similar observations have been made for H7N9 virus infection and vaccination77,138,139,140. However, whereas vaccination with H5 mostly induces a pan-group 1 HA anti-stalk response that is skewed towards the VH1-69 antibody germ line, exposure to H7 can induce a much broader antibody response that might target both group 1 and group 2 HA proteins using a more diverse set of antibody germ lines, including VH1-18, VH6-1 and VH3-53 (refs141,142). It remains to be clarified why these responses to H5 and H7 HAs are different. Of note, it has been observed that the primary immune response to vaccines containing H5 HA is usually of a greater magnitude than the response to vaccines containing H7 HA, which might be explained by the fact that antibody titres and B cell numbers that cross-react with H5 HA are higher at baseline than those reacting to H7 HA141,142. If an H5N1 virus vaccine or H7N9 virus vaccine is given a second time, the immune system restores its preference for the head domain of the HA, for which it has now been primed, and produces antibodies that target the HA head domain, including antibodies with haemagglutination inhibition activity136. Importantly, that does not mean that the serum antibody response against the HA stalk domain is necessarily suppressed. Universal influenza virus vaccine candidates that optimally exploit this phenomenon, which is based on OAS (Box 1), have been designed and are currently in clinical trials. Most likely as a result of this phenomenon, vaccines that contain H5 or H7 HA have to be given at least twice and typically at higher doses or with strong adjuvants to reach high titres of haemagglutination inhibition.
Next-generation influenza virus vaccines
Major efforts are currently underway to design and develop broadly protective or universal influenza virus vaccines143,144,145. These vaccines would abolish the need for annual reformulation and re-administration of seasonal vaccines, would make influenza virus vaccines accessible to low-income and middle-income countries and would markedly increase our pandemic preparedness146. Several antibody targets for these vaccines have been identified, including the stalk domain of HA and conserved epitopes in the head domains of HA and NA and the ectodomain of M2 (ref.147). In addition, T cell-based vaccines that mostly focus on NP and M1 are under development147. Vaccines based on the HA stalk fall into two main categories: stalk-only or headless HA constructs, in which the immunodominant HA head domain is eliminated148,149,150, and chimeric HA constructs, which refocus the immune response from the HA head towards the HA stalk through sequential vaccination151,152,153. Both of these vaccine strategies probably depend on and benefit from pre-existing immunity. Other vaccine approaches, such as the computationally optimized broadly reactive antigen (COBRA) approach, aim to induce broad antibody responses with haemagglutination inhibition activity against the HA head domain, usually within a certain virus subtype154,155. These approaches might be heavily influenced by the phenomenon of head-epitope-specific imprinting (Box 1), which could have beneficial or detrimental effects on the vaccine response, depending on the imprinting and exposure history of the vaccine recipient. Vaccines based on M2e were developed early on, and these could also be a potential option towards a broadly protective or universal influenza virus vaccine156. Finally, NA has emerged as a new vaccine target after studies showed that anti-NA immune responses can be relatively broad, at least within a virus subtype42,51,109. These different vaccine approaches induce different mechanisms of antibody-based protection. Virus neutralization and FcR-mediated antibody effector functions are induced in the case of HA stalk-targeted vaccines; the induction of antibodies with haemagglutination inhibition activity is the aim of broadly protective HA head-based vaccines; FcR-mediated antibody effector functions are the mechanism of action in the case of M2e-based vaccines; and direct inhibition of NA activity and FcR-mediated effector functions are induced by NA-based vaccines. What all of these approaches have in common is that they need to induce long-lived antibody responses to be successful. A universal influenza virus vaccine that only protects for 12 months is of very limited use. Therefore, we should apply the lessons learned from studying long-lived immune responses to natural infection with influenza virus and translate this knowledge into designing vaccines that also induce long-lived, ideally lifelong, immunity. This might be achieved by using better adjuvants that stimulate the right innate immune sensors in exactly the right cell types or by delivering vaccines in ways that increase antigen and epitope integrity. We might have to optimize vaccines to enable persistent antigen presentation over many days in the presence of adequate innate immune stimuli. Finally, we need to find better ways to present antigen to the immune system at mucosal surfaces in the respiratory tract.
Conclusions
The antibody response to influenza virus infection is multifaceted and fascinating. Although this response has been studied for decades, many questions remain unanswered. Our understanding of the dynamics between B cell subsets — memory B cells, long-lived plasma cells and plasmablasts — is still rudimentary, and we lack the tools to rationally influence these dynamics during vaccination. The molecular mechanisms and consequences of imprinting are largely unknown, and, until we have a better understanding of this family of phenomena, we cannot use them to our advantage. The role and mechanisms of the mucosal antibody response to influenza virus antigens need further investigation, and vaccines that induce robust mucosal immune responses need to be developed. The molecular basis of immunodominance is largely unknown, and, without understanding this, we cannot design vaccines that refocus antibody responses to our epitopes of choice. The factors that drive long-lived immunity are not well understood, but this knowledge will be crucial to design vaccines that provide long-lived protection. A better understanding of how different antiviral functions correlate with protection against infection and the establishment of novel correlates of protection will be crucial for future vaccines that do not rely on the induction of antibodies with haemagglutination inhibition activity. Finally, better insights as to how sex differences influence the antibody response after infection and vaccination are needed. These differences are not well understood, but they might be important in terms of inducing optimal protection in a sex-specific manner157,158,159. In addition, there are countless other questions that thus far remain unanswered. In conclusion, the antibody response to natural influenza virus infection seems to be broader and longer-lived than the antibody response induced by influenza virus vaccines. A better understanding of the questions listed above and the differences between natural virus infection and vaccination will allow us to design better vaccines. The ultimate goal is to develop a universal influenza virus vaccine that induces long-lived protection against drifted seasonal, zoonotic and pandemic influenza virus infections.
References
World Health Organization. Influenza (seasonal). WHO https://www.who.int/en/news-room/fact-sheets/detail/influenza-(seasonal) (2018).
Krammer, F. et al. Influenza. Nat. Rev. Dis. Primers 4, 3 (2018).
Subbarao, K. Avian influenza H7N9 viruses: a rare second warning. Cell Res. 28, 1–2 (2018).
Krammer, F. Emerging influenza viruses and the prospect of a universal influenza virus vaccine. Biotechnol. J. 10, 690–701 (2015).
Palese, P. Influenza: old and new threats. Nat. Med. 10, S82–87 (2004).
Smith, G. et al. Origins and evolutionary genomics of the 2009 swine-origin H1N1 influenza A epidemic. Nature 459, 1122–1125 (2009).
Guan, Y. et al. The emergence of pandemic influenza viruses. Protein Cell 1, 9–13 (2010).
Saunders-Hastings, P. R. & Krewski, D. Reviewing the history of pandemic influenza: understanding patterns of emergence and transmission. Pathogens 5, 66 (2016).
Gasparini, R., Amicizia, D., Lai, P. L. & Panatto, D. Clinical and socioeconomic impact of seasonal and pandemic influenza in adults and the elderly. Hum. Vaccin. Immunother. 8, 21–28 (2012).
Smith, W., Andrewes, C. H. & Laidlaw, P. P. A virus obtained from influenza patients. Lancet 222, 66–68 (1933).
Hobson, D., Curry, R. L., Beare, A. S. & Ward-Gardner, A. The role of serum haemagglutination-inhibiting antibody in protection against challenge infection with influenza A2 and B viruses. J. Hyg. (Lond.) 70, 767–777 (1972).
Doud, M. B. & Bloom, J. D. Accurate measurement of the effects of all amino-acid mutations on influenza hemagglutinin. Viruses 8, 155 (2016). This study explores the antigenic flexibility of influenza virus HA using a library of single amino acid mutants.
Heaton, N. S., Sachs, D., Chen, C. J., Hai, R. & Palese, P. Genome-wide mutagenesis of influenza virus reveals unique plasticity of the hemagglutinin and NS1 proteins. Proc. Natl Acad. Sci. USA 110, 20248–20253 (2013). This paper explores the antigenic flexibility of influenza virus using a five-amino-acid insertion library.
Kirkpatrick, E., Qiu, X., Wilson, P. C., Bahl, J. & Krammer, F. The influenza virus hemagglutinin head evolves faster than the stalk domain. Sci. Rep. 8, 10432 (2018).
Gerdil, C. The annual production cycle for influenza vaccine. Vaccine 21, 1776–1779 (2003).
de Jong, J. C., Beyer, W. E., Palache, A. M., Rimmelzwaan, G. F. & Osterhaus, A. D. Mismatch between the 1997/1998 influenza vaccine and the major epidemic A(H3N2) virus strain as the cause of an inadequate vaccine-induced antibody response to this strain in the elderly. J. Med. Virol. 61, 94–99 (2000).
Xie, H. et al. H3N2 mismatch of 2014–2015 northern hemisphere influenza vaccines and head-to-head comparison between human and ferret antisera derived antigenic maps. Sci. Rep. 5, 15279 (2015).
Wrammert, J. et al. Rapid cloning of high-affinity human monoclonal antibodies against influenza virus. Nature 453, 667–671 (2008).
Wu, N. C. & Wilson, I. A. Structural insights into the design of novel anti-influenza therapies. Nat. Struct. Mol. Biol. 25, 115–121 (2018).
van de Sandt, C. E., Bodewes, R., Rimmelzwaan, G. F. & de Vries, R. D. Influenza B viruses: not to be discounted. Future Microbiol. 10, 1447–1465 (2015).
Tan, J., Asthagiri Arunkumar, G. & Krammer, F. Universal influenza virus vaccines and therapeutics: where do we stand with influenza B virus? Curr. Opin. Immunol. 53, 45–50 (2018).
Bodewes, R. et al. In vitro assessment of the immunological significance of a human monoclonal antibody directed to the influenza a virus nucleoprotein. Clin. Vaccine Immunol. 20, 1333–1337 (2013).
Wang, M. et al. Antibody dynamics of 2009 influenza A (H1N1) virus in infected patients and vaccinated people in China. PLOS ONE 6, e16809 (2011).
Nachbagauer, R. et al. Defining the antibody cross-reactome directed against the influenza virus surface glycoproteins. Nat. Immunol. 18, 464–473 (2017). This study characterizes the breadth of the immune response to HA and NA in three animal models and humans across all HA subtypes.
Li, Z. N. et al. IgM, IgG, and IgA antibody responses to influenza A(H1N1)pdm09 hemagglutinin in infected persons during the first wave of the 2009 pandemic in the United States. Clin. Vaccine Immunol. 21, 1054–1060 (2014).
Monto, A. S. et al. Antibody to influenza virus neuraminidase: an independent correlate of protection. J. Infect. Dis. 212, 1191–1199 (2015). This paper describes NA-specific antibody titres as an independent correlate of protection against influenza virus infection in humans.
Lewnard, J. A. & Cobey, S. Immune history and influenza vaccine effectiveness. Vaccines (Basel) 6, 28 (2018). This interesting review discusses pre-existing immunity to influenza virus and its effects on vaccination.
Nachbagauer, R. et al. Age dependence and isotype specificity of influenza virus hemagglutinin stalk-reactive antibodies in humans. mBio 7, e01996–15 (2016).
Baz, M. et al. Seroconversion to seasonal influenza viruses after A(H1N1)pdm09 virus infection, Quebec, Canada. Emerg. Infect. Dis. 18, 1132–1134 (2012).
Krammer, F. & Palese, P. Influenza virus hemagglutinin stalk-based antibodies and vaccines. Curr. Opin. Virol. 3, 521–530 (2013).
Gerhard, W., Yewdell, J., Frankel, M. E. & Webster, R. Antigenic structure of influenza virus haemagglutinin defined by hybridoma antibodies. Nature 290, 713–717 (1981).
Webster, R. G. & Laver, W. G. Determination of the number of nonoverlapping antigenic areas on Hong Kong (H3N2) influenza virus hemagglutinin with monoclonal antibodies and the selection of variants with potential epidemiological significance. Virology 104, 139–148 (1980).
Skehel, J. J. et al. A carbohydrate side chain on hemagglutinins of Hong Kong influenza viruses inhibits recognition by a monoclonal antibody. Proc. Natl Acad. Sci. USA 81, 1779–1783 (1984).
Wang, Q., Cheng, F., Lu, M., Tian, X. & Ma, J. Crystal structure of unliganded influenza B virus hemagglutinin. J. Virol. 82, 3011–3020 (2008).
Medina, R. A. et al. Glycosylations in the globular head of the hemagglutinin protein modulate the virulence and antigenic properties of the H1N1 influenza viruses. Sci. Transl Med. 5, 187ra170 (2013).
Margine, I. et al. H3N2 influenza virus infection induces broadly reactive hemagglutinin stalk antibodies in humans and mice. J. Virol. 87, 4728–4737 (2013).
Sui, J. et al. Wide prevalence of heterosubtypic broadly neutralizing human anti-influenza A antibodies. Clin. Infect. Dis. 52, 1003–1009 (2011).
Throsby, M. et al. Heterosubtypic neutralizing monoclonal antibodies cross-protective against H5N1 and H1N1 recovered from human IgM+memory B cells. PLOS ONE 3, e3942 (2008).
Ekiert, D. C. & Wilson, I. A. Broadly neutralizing antibodies against influenza virus and prospects for universal therapies. Curr. Opin. Virol. 2, 134–141 (2012).
Dreyfus, C. et al. Highly conserved protective epitopes on influenza B viruses. Science 337, 1343–1348 (2012).
Corti, D. et al. A neutralizing antibody selected from plasma cells that binds to group 1 and group 2 influenza A hemagglutinins. Science 333, 850–856 (2011).
Chen, Y. Q. et al. Influenza infection in humans induces broadly cross-reactive and protective neuraminidase-reactive antibodies. Cell 173, 417–429 (2018). This study describes the first NA-specific antibodies isolated from humans and characterizes differences between natural infection with influenza virus and vaccination.
Pica, N. et al. Hemagglutinin stalk antibodies elicited by the 2009 pandemic influenza virus as a mechanism for the extinction of seasonal H1N1 viruses. Proc. Natl Acad. Sci. USA 109, 2573–2578 (2012).
Yu, X. et al. Neutralizing antibodies derived from the B cells of 1918 influenza pandemic survivors. Nature 455, 532–536 (2008).
Fisman, D. N. et al. Older age and a reduced likelihood of 2009 H1N1 virus infection. N. Engl. J. Med. 361, 2000–2001 (2009).
Hancock, K. et al. Cross-reactive antibody responses to the 2009 pandemic H1N1 influenza virus. N. Engl. J. Med. 361, 1945–1952 (2009).
Kendal, A. P. et al. Laboratory-based surveillance of influenza virus in the United States during the winter of 1977–1978. I. Periods of prevalence of H1N1 and H3N2 influenza A strains, their relative rates of isolation in different age groups, and detection of antigenic variants. Am. J. Epidemiol. 110, 449–461 (1979).
Babu, T. M. et al. Population serologic immunity to human and avian H2N2 viruses in the United States and Hong Kong for pandemic risk assessment. J. Infect. Dis. 218, 1054–1060 (2018).
Miller, M. S. et al. Neutralizing antibodies against previously encountered influenza virus strains increase over time: a longitudinal analysis. Sci. Transl Med. 5, 198ra107 (2013).
Miller, M. S. et al. 1976 and 2009 H1N1 influenza virus vaccines boost anti-hemagglutinin stalk antibodies in humans. J. Infect. Dis. 207, 98–105 (2012).
Krammer, F. et al. NAction! How can neuraminidase-based immunity contribute to better influenza virus vaccines? mBio 9, e02332–17 (2018).
Johansson, B. E., Moran, T. M. & Kilbourne, E. D. Antigen-presenting B cells and helper T cells cooperatively mediate intravirionic antigenic competition between influenza A virus surface glycoproteins. Proc. Natl Acad. Sci. USA 84, 6869–6873 (1987).
Wohlbold, T. J. & Krammer, F. In the shadow of hemagglutinin: a growing interest in influenza viral neuraminidase and its role as a vaccine antigen. Viruses 6, 2465–2494 (2014).
Rajendran, M. et al. Analysis of anti-influenza virus neuraminidase antibodies in children, adults, and the elderly by ELISA and enzyme inhibition: evidence for original antigenic sin. mBio 8, e02281–16 (2017).
Haaheim, R. Single-radial-complement-fixation: a new immunodiffusion technique. 2. Assay of the antibody response to the internal antigens (MP and NP) of influenza A virus in human sera after vaccination and infection. Dev. Biol. Stand. 39, 481–484 (1977).
Black, R. A., Rota, P. A., Gorodkova, N., Klenk, H. D. & Kendal, A. P. Antibody response to the M2 protein of influenza A virus expressed in insect cells. J. Gen. Virol. 74, 143–146 (1993).
Sukeno, N. et al. Anti-nucleoprotein antibody response in influenza A infection. Tohoku J. Exp. Med. 128, 241–249 (1979).
de Boer, G. F., Back, W. & Osterhaus, A. D. An ELISA for detection of antibodies against influenza A nucleoprotein in humans and various animal species. Arch. Virol. 115, 47–61 (1990).
Reiche, S. et al. High inter-individual diversity of point mutations, insertions, and deletions in human influenza virus nucleoprotein-specific memory B cells. PLOS ONE 10, e0128684 (2015).
Cretescu, L., Beare, A. S. & Schild, G. C. Formation of antibody to matrix protein in experimental human influenza A virus infections. Infect. Immun. 22, 322–327 (1978).
Joassin, L., Reginster, M. & Vaira, D. Anti M-protein antibody response to type A or B natural influenza detected by solid phase enzyme linked immunosorbent assay and by complement fixation. Arch. Virol. 76, 15–23 (1983).
Vanderven, H. A. et al. What lies beneath: antibody dependent natural killer cell activation by antibodies to internal influenza virus proteins. EBioMedicine 8, 277–290 (2016). This interesting paper characterizes the FcR-mediated effector functions of antibodies to NP and M1.
Jegaskanda, S. et al. Induction of H7N9-cross-reactive antibody-dependent cellular cytotoxicity antibodies by human seasonal influenza A viruses that are directed toward the nucleoprotein. J. Infect. Dis. 215, 818–823 (2017).
Feng, J. et al. Influenza A virus infection engenders a poor antibody response against the ectodomain of matrix protein 2. Virol. J. 3, 102 (2006).
Grandea, A. G. et al. Human antibodies reveal a protective epitope that is highly conserved among human and nonhuman influenza A viruses. Proc. Natl Acad. Sci. USA 107, 12658–12663 (2010).
Zhong, W. et al. Serum antibody response to matrix protein 2 following natural infection with 2009 pandemic influenza A(H1N1) virus in humans. J. Infect. Dis. 209, 986–994 (2014).
Khurana, S. et al. Antigenic fingerprinting of H5N1 avian influenza using convalescent sera and monoclonal antibodies reveals potential vaccine and diagnostic targets. PLOS Med. 6, e1000049 (2009).
Krejnusová, I. et al. Antibodies to PB1-F2 protein are induced in response to influenza A virus infection. Arch. Virol. 154, 1599–1604 (2009).
Yodsheewan, R. et al. Human monoclonal ScFv specific to NS1 protein inhibits replication of influenza viruses across types and subtypes. Antiviral Res. 100, 226–237 (2013).
Thathaisong, U. et al. Human monoclonal single chain antibodies (HuScFv) that bind to the polymerase proteins of influenza A virus. Asian Pac. J. Allergy Immunol. 26, 23–35 (2008).
Reynolds, H. Y. Immunoglobulin G and its function in the human respiratory tract. Mayo Clin. Proc. 63, 161–174 (1988).
Spiekermann, G. M. et al. Receptor-mediated immunoglobulin G transport across mucosal barriers in adult life: functional expression of FcRn in the mammalian lung. J. Exp. Med. 196, 303–310 (2002).
Pakkanen, S. H. et al. Expression of homing receptors on IgA1 and IgA2 plasmablasts in blood reflects differential distribution of IgA1 and IgA2 in various body fluids. Clin. Vaccine Immunol. 17, 393–401 (2010).
Suzuki, T. et al. Relationship of the quaternary structure of human secretory IgA to neutralization of influenza virus. Proc. Natl Acad. Sci. USA 112, 7809–7814 (2015).
Ekiert, D. C. et al. Cross-neutralization of influenza A viruses mediated by a single antibody loop. Nature 489, 526–532 (2012).
DiLillo, D. J., Palese, P., Wilson, P. C. & Ravetch, J. V. Broadly neutralizing anti-influenza antibodies require Fc receptor engagement for in vivo protection. J. Clin. Invest. 126, 605–610 (2016). This paper shows the importance of Fc–FcR interactions for protection mediated by HA stalk-reactive antibodies.
Henry Dunand, C. J. et al. Both neutralizing and non-neutralizing human H7N9 influenza vaccine-induced monoclonal antibodies confer protection. Cell Host Microbe 19, 800–813 (2016). This interesting manuscript describes non-neutralizing human HA-reactive antibodies that protect against infection with H7N9 virus.
Couch, R. B. et al. Antibody correlates and predictors of immunity to naturally occurring influenza in humans and the importance of antibody to the neuraminidase. J. Infect. Dis. 207, 974–981 (2013).
Ohmit, S. E., Petrie, J. G., Cross, R. T., Johnson, E. & Monto, A. S. Influenza hemagglutination-inhibition antibody titer as a correlate of vaccine-induced protection. J. Infect. Dis. 204, 1879–1885 (2011).
Brandenburg, B. et al. Mechanisms of hemagglutinin targeted influenza virus neutralization. PLOS ONE 8, e80034 (2013).
Chai, N. et al. Two escape mechanisms of influenza A virus to a broadly neutralizing stalk-binding antibody. PLOS Pathog. 12, e1005702 (2016).
Tan, G. S. et al. Characterization of a broadly neutralizing monoclonal antibody that targets the fusion domain of group 2 influenza a virus hemagglutinin. J. Virol. 88, 13580–13592 (2014).
Ekiert, D. C. et al. Antibody recognition of a highly conserved influenza virus epitope. Science 324, 246–251 (2009).
Verschoor, C. P. et al. Microneutralization assay titres correlate with protection against seasonal influenza H1N1 and H3N2 in children. PLOS ONE 10, e0131531 (2015).
Tsang, T. K. et al. Association between antibody titers and protection against influenza virus infection within households. J. Infect. Dis. 210, 684–692 (2014).
Trombetta, C. M., Perini, D., Mather, S., Temperton, N. & Montomoli, E. Overview of serological techniques for influenza vaccine evaluation: past, present and future. Vaccines (Basel) 2, 707–734 (2014).
Trombetta, C. M., Remarque, E. J., Mortier, D. & Montomoli, E. Comparison of hemagglutination inhibition, single radial hemolysis, virus neutralization assays, and ELISA to detect antibody levels against seasonal influenza viruses. Influenza Other Respir. Viruses 12, 675–686 (2018).
Wohlbold, T. J. et al. Hemagglutinin stalk- and neuraminidase-specific monoclonal antibodies protect against lethal H10N8 influenza virus infection in mice. J. Virol. 90, 851–861 (2015).
Yang, X. et al. A beneficiary role for neuraminidase in influenza virus penetration through the respiratory mucus. PLOS ONE 9, e110026 (2014).
Schultz-Cherry, S. & Hinshaw, V. S. Influenza virus neuraminidase activates latent transforming growth factor beta. J. Virol. 70, 8624–8629 (1996).
Memoli, M. J. et al. Evaluation of antihemagglutinin and antineuraminidase antibodies as correlates of protection in an influenza A/H1N1 virus healthy human challenge model. mBio 7, e00417–16 (2016).
Dilillo, D. J., Tan, G. S., Palese, P. & Ravetch, J. V. Broadly neutralizing hemagglutinin stalk-specific antibodies require FcγR interactions for protection against influenza virus in vivo. Nat. Med. 20, 143–151 (2014).
Terajima, M. et al. Complement-dependent lysis of influenza a virus-infected cells by broadly cross-reactive human monoclonal antibodies. J. Virol. 85, 13463–13467 (2011).
Tan, G. S. et al. Broadly-reactive neutralizing and non-neutralizing antibodies directed against the H7 influenza virus hemagglutinin reveal divergent mechanisms of protection. PLOS Pathog. 12, e1005578 (2016).
Leon, P. E. et al. Optimal activation of Fc-mediated effector functions by influenza virus hemagglutinin antibodies requires two points of contact. Proc. Natl Acad. Sci. USA 113, E5944–E5951 (2016). This study describes the two-contact model for FcR-mediated effector functions of antibodies towards influenza virus antigens.
Cox, F. et al. HA antibody-mediated FcγRIIIa activity is both dependent on FcR engagement and interactions between HA and sialic acids. Front. Immunol. 7, 399 (2016).
Wohlbold, T. J. et al. Broadly protective murine monoclonal antibodies against influenza B virus target highly conserved neuraminidase epitopes. Nat. Microbiol. 2, 1415–1424 (2017).
Jacobsen, H. et al. Influenza virus hemagglutinin stalk-specific antibodies in human serum are a surrogate marker for in vivo protection in a serum transfer mouse challenge model. mBio 8, e01463–17 (2017).
El Bakkouri, K. et al. Universal vaccine based on ectodomain of matrix protein 2 of influenza A: Fc receptors and alveolar macrophages mediate protection. J. Immunol. 186, 1022–1031 (2011).
Ramos, E. L. et al. Efficacy and safety of treatment with an anti-M2e monoclonal antibody in experimental human influenza. J. Infect. Dis. 211, 1038–1044 (2014).
Lamere, M. W. et al. Regulation of antinucleoprotein IgG by systemic vaccination and its effect on influenza virus clearance. J. Virol. 85, 5027–5035 (2011).
LaMere, M. W. et al. Contributions of antinucleoprotein IgG to heterosubtypic immunity against influenza virus. J. Immunol. 186, 4331–4339 (2011).
García-Sastre, A. Induction and evasion of type I interferon responses by influenza viruses. Virus Res. 162, 12–18 (2011).
Ehrlich, H. J. et al. Pre-vaccination immunity and immune responses to a cell culture-derived whole-virus H1N1 vaccine are similar to a seasonal influenza vaccine. Vaccine 30, 4543–4551 (2012).
Fritz, R. et al. A vero cell-derived whole-virus H5N1 vaccine effectively induces neuraminidase-inhibiting antibodies. J. Infect. Dis. 205, 28–34 (2012).
van der Velden, M. V. et al. Cell culture (Vero cell) derived whole-virus non-adjuvanted H5N1 influenza vaccine induces long-lasting cross-reactive memory immune response: homologous or heterologous booster response following two dose or single dose priming. Vaccine 30, 6127–6135 (2012).
Beyer, W. E. P., Palache, A. M. & Osterhaus, A. D. M. E. Comparison of serology and reactogenicity between influenza subunit vaccines and whole virus or split vaccines: a review and meta-analysis of the literature. Clin. Drug Investig. 15, 1–12 (1998).
Oxford, J. S., Schild, G. C., Potter, C. W. & Jennings, R. The specificity of the anti-haemagglutinin antibody response induced in man by inactivated influenza vaccines and by natural infection. J. Hyg. (Lond.) 82, 51–61 (1979).
Wohlbold, T. J. et al. Vaccination with adjuvanted recombinant neuraminidase induces broad heterologous, but not heterosubtypic, cross-protection against influenza virus infection in mice. mBio 6, e02556 (2015).
Couch, R. B. et al. Randomized comparative study of the serum antihemagglutinin and antineuraminidase antibody responses to six licensed trivalent influenza vaccines. Vaccine 31, 190–195 (2012).
Cox, R. J. & Brokstad, K. A. The postvaccination antibody response to influenza virus proteins. APMIS 107, 289–296 (1999).
Moody, M. A. et al. H3N2 influenza infection elicits more cross-reactive and less clonally expanded anti-hemagglutinin antibodies than influenza vaccination. PLOS ONE 6, e25797 (2011).
Andrews, S. F. et al. Immune history profoundly affects broadly protective B cell responses to influenza. Sci. Transl Med. 7, 316ra192 (2015).
Fonville, J. M. et al. Antibody landscapes after influenza virus infection or vaccination. Science 346, 996–1000 (2014).
Zost, S. J. et al. Contemporary H3N2 influenza viruses have a glycosylation site that alters binding of antibodies elicited by egg-adapted vaccine strains. Proc. Natl Acad. Sci. USA 114, 12578–12583 (2017). This interesting paper shows the effect of egg adaptation on immune responses to different influenza virus vaccines.
Flannery, B. et al. Interim estimates of 2017–2018 seasonal influenza vaccine effectiveness - United States, February 2018. MMWR Morb. Mortal. Wkly Rep. 67, 180–185 (2018).
Krammer, F. & Palese, P. Advances in the development of influenza virus vaccines. Nat. Rev. Drug Discov. 14, 167–182 (2015).
Dunkle, L. M. & Izikson, R. Recombinant hemagglutinin influenza vaccine provides broader spectrum protection. Expert Rev. Vaccines 15, 957–966 (2016).
Dunkle, L. M. et al. Efficacy of recombinant influenza vaccine in adults 50 years of age or older. N. Engl. J. Med. 376, 2427–2436 (2017).
Su, F., Patel, G. B., Hu, S. & Chen, W. Induction of mucosal immunity through systemic immunization: phantom or reality? Hum. Vaccin. Immunother. 12, 1070–1079 (2016).
Barría, M. I. et al. Localized mucosal response to intranasal live attenuated influenza vaccine in adults. J. Infect. Dis. 207, 115–124 (2013).
Islam, S. et al. Influenza A haemagglutinin specific IgG responses in children and adults after seasonal trivalent live attenuated influenza vaccination. Vaccine 35, 5666–5673 (2017).
Johnson, P. R., Feldman, S., Thompson, J. M., Mahoney, J. D. & Wright, P. F. Comparison of long-term systemic and secretory antibody responses in children given live, attenuated, or inactivated influenza A vaccine. J. Med. Virol. 17, 325–335 (1985).
Ambrose, C. S., Wu, X., Jones, T. & Mallory, R. M. The role of nasal IgA in children vaccinated with live attenuated influenza vaccine. Vaccine 30, 6794–6801 (2012).
Belongia, E. A. et al. Waning vaccine protection against influenza A (H3N2) illness in children and older adults during a single season. Vaccine 33, 246–251 (2015).
Kissling, E. et al. Low and decreasing vaccine effectiveness against influenza A(H3) in 2011/12 among vaccination target groups in Europe: results from the I-MOVE multicentre case-control study. Euro Surveill. 18, 20390 (2013).
Kissling, E. et al. I-MOVE multicentre case-control study 2010/11 to 2014/15: is there within-season waning of influenza type/subtype vaccine effectiveness with increasing time since vaccination? Euro Surveill. 21, 30201 (2016).
Puig-Barberà, J. et al. Waning protection of influenza vaccination during four influenza seasons, 2011/2012 to 2014/2015. Vaccine 35, 5799–5807 (2017).
Ferdinands, J. M. et al. Intraseason waning of influenza vaccine protection: evidence from the US Influenza Vaccine Effectiveness Network, 2011–2012 through 2014–2015. Clin. Infect. Dis. 64, 544–550 (2017).
Petrie, J. G., Ohmit, S. E., Johnson, E., Truscon, R. & Monto, A. S. Persistence of antibodies to influenza hemagglutinin and neuraminidase following one or two years of influenza vaccination. J. Infect. Dis. 212, 1914–1922 (2015).
Petrie, J. G. et al. Modest waning of influenza vaccine efficacy and antibody titers during the 2007–2008 influenza season. J. Infect. Dis. 214, 1142–1149 (2016).
Wrammert, J. et al. Broadly cross-reactive antibodies dominate the human B cell response against 2009 pandemic H1N1 influenza virus infection. J. Exp. Med. 208, 181–193 (2011).
Li, G. M. et al. Pandemic H1N1 influenza vaccine induces a recall response in humans that favors broadly cross-reactive memory B cells. Proc. Natl Acad. Sci. USA 109, 9047–9052 (2012).
Thomson, C. A. et al. Pandemic H1N1 influenza infection and vaccination in humans induces cross-protective antibodies that target the hemagglutinin stem. Front. Immunol. 3, 87 (2012).
Qiu, C. et al. Boosting heterosubtypic neutralization antibodies in recipients of 2009 pandemic H1N1 influenza vaccine. Clin. Infect. Dis. 54, 17–24 (2012).
Ellebedy, A. H. et al. Induction of broadly cross-reactive antibody responses to the influenza HA stem region following H5N1 vaccination in humans. Proc. Natl Acad. Sci. USA 111, 13133–13138 (2014).
Nachbagauer, R. et al. Induction of broadly reactive anti-hemagglutinin stalk antibodies by an H5N1 vaccine in humans. J. Virol. 88, 13260–13268 (2014). This study and that of Ellebedy et al. (2014) show that H5N1 virus vaccination induces HA stalk-specific antibodies in humans.
Krammer, F. et al. An H7N1 influenza virus vaccine induces broadly reactive antibody responses against H7N9 in humans. Clin. Vaccine Immunol. 21, 1153–1163 (2014).
Liu, L. et al. Induction of broadly cross-reactive stalk-specific antibody responses to influenza group 1 and group 2 hemagglutinins by natural H7N9 virus infection in humans. J. Infect. Dis. 215, 518–528 (2017).
Stadlbauer, D. et al. Vaccination with a recombinant H7 hemagglutinin-based influenza virus vaccine induces broadly reactive antibodies in humans. mSphere 2, e00502–17 (2017).
Stadlbauer, D., Nachbagauer, R., Meade, P. & Krammer, F. Universal influenza virus vaccines: what can we learn from the human immune response following exposure to H7 subtype viruses? Front. Med. 11, 471–479 (2017).
Andrews, S. F. et al. Preferential induction of cross-group influenza A hemagglutinin stem-specific memory B cells after H7N9 immunization in humans. Sci. Immunol. 2, eaan2676 (2017).
Erbelding, E. J. et al. A universal influenza vaccine: the strategic plan for the National Institute of Allergy and Infectious Diseases. J. Infect. Dis. 218, 347–354 (2018). This very informative manuscript describes plans by the US National Institute of Allergy and Infectious Diseases to develop a universal influenza virus vaccine.
Paules, C. I., Marston, H. D., Eisinger, R. W., Baltimore, D. & Fauci, A. S. The pathway to a universal influenza vaccine. Immunity 47, 599–603 (2017).
Paules, C. I., Sullivan, S. G., Subbarao, K. & Fauci, A. S. Chasing seasonal influenza - the need for a universal influenza vaccine. N. Engl. J. Med. 378, 7–9 (2018).
Krammer, F., García-Sastre, A. & Palese, P. Is it possible to develop a “universal” influenza virus vaccine? Potential target antigens and critical aspects for vaccine development. Cold Spring Harb. Perspect. Biol. 10, a028845 (2017).
Nachbagauer, R. & Krammer, F. Universal influenza virus vaccines and therapeutic antibodies. Clin. Microbiol. Infect. 23, 222–228 (2017). This review describes the universal influenza virus vaccine candidates that are in clinical trials.
Krammer, F. The quest for a universal flu vaccine: headless HA 2.0. Cell Host Microbe 18, 395–397 (2015).
Impagliazzo, A. et al. A stable trimeric influenza hemagglutinin stem as a broadly protective immunogen. Science 349, 1301–1306 (2015).
Yassine, H. M. et al. Hemagglutinin-stem nanoparticles generate heterosubtypic influenza protection. Nat. Med. 21, 1065–1070 (2015).
Krammer, F., Pica, N., Hai, R., Margine, I. & Palese, P. Chimeric hemagglutinin influenza virus vaccine constructs elicit broadly protective stalk-specific antibodies. J. Virol. 87, 6542–6550 (2013).
Nachbagauer, R. et al. A chimeric haemagglutinin-based influenza split virion vaccine adjuvanted with AS03 induces protective stalk-reactive antibodies in mice. NPJ Vaccines 1, 16015 (2016).
Nachbagauer, R. et al. A universal influenza virus vaccine candidate confers protection against pandemic H1N1 infection in preclinical ferret studies. NPJ Vaccines 2, 26 (2017).
Carter, D. M. et al. Design and characterization of a computationally optimized broadly reactive hemagglutinin vaccine for H1N1 influenza viruses. J. Virol. 90, 4720–4734 (2016).
Wong, T. M. et al. Computationally optimized broadly reactive hemagglutinin elicits hemagglutination inhibition antibodies against a panel of H3N2 influenza virus cocirculating variants. J. Virol. 91, e01581–17 (2017).
Schepens, B., De Vlieger, D. & Saelens, X. Vaccine options for influenza: thinking small. Curr. Opin. Immunol. 53, 22–29 (2018).
Fink, A. L., Engle, K., Ursin, R. L., Tang, W. Y. & Klein, S. L. Biological sex affects vaccine efficacy and protection against influenza in mice. Proc. Natl Acad. Sci. USA 115, 12477–12482 (2018).
Fink, A. L. & Klein, S. L. The evolution of greater humoral immunity in females than males: implications for vaccine efficacy. Curr. Opin. Physiol. 6, 16–20 (2018).
Klein, S. L. & Pekosz, A. Sex-based biology and the rational design of influenza vaccination strategies. J. Infect. Dis. 209, S114–119 (2014).
Francis, T. On the doctrine of original antigenic sin. Proc. Am. Philos. Soc. 104, 572–578 (1960).
Lessler, J. et al. Evidence for antigenic seniority in influenza A (H3N2) antibody responses in southern China. PLOS Pathog. 8, e1002802 (2012).
Li, Y. et al. Immune history shapes specificity of pandemic H1N1 influenza antibody responses. J. Exp. Med. 210, 1493–1500 (2013).
Gostic, K. M., Ambrose, M., Worobey, M. & Lloyd-Smith, J. O. Potent protection against H5N1 and H7N9 influenza via childhood hemagglutinin imprinting. Science 354, 722–726 (2016). This interesting paper hypothesizes that imprinting might protect from severe infection with H5N1 virus or H7N9 virus.
Petrie, J. G. & Monto, A. S. Untangling the effects of prior vaccination on subsequent influenza vaccine effectiveness. J. Infect. Dis. 215, 841–843 (2017).
Zarnitsyna, V. I. et al. Masking of antigenic epitopes by antibodies shapes the humoral immune response to influenza. Philos. Trans. R Soc. B 370, 20140248 (2015).
Guthmiller, J. J. & Wilson, P. C. Harnessing immune history to combat influenza viruses. Curr. Opin. Immunol. 53, 187–195 (2018).
Cobey, S. & Hensley, S. E. Immune history and influenza virus susceptibility. Curr. Opin. Virol. 22, 105–111 (2017).
Angeletti, D. et al. Defining B cell immunodominance to viruses. Nat. Immunol. 18, 456–463 (2017). This report shows the immunodominance of antigenic sites in H1 HA in mice.
Liu, S. T. et al. Antigenic sites in influenza H1 hemagglutinin display species-specific immunodominance. J. Clin. Invest. 128, 4992–4996 (2018). This report shows the immunodominance of antigenic sites in H1 HA in several animal models and humans.
Broecker, F. et al. Immunodominance of antigenic site B in the hemagglutinin of the current H3N2 influenza virus in humans and mice. J. Virol. 92, e01100–18 (2018). This report shows the immunodominance of antigenic sites in H3 HA in several animal models and humans.
Sun, W. et al. Antibody responses toward the major antigenic sites of influenza B virus hemagglutinin in mice, ferrets and humans. J. Virol. 93, e01673–18 (2018). This report shows the immunodominance of influenza B virus antigenic sites in several animal models and humans.
Altman, M. O., Bennink, J. R., Yewdell, J. W. & Herrin, B. R. Lamprey VLRB response to influenza virus supports universal rules of immunogenicity and antigenicity. eLife 4, e07467 (2015).
Ellebedy, A. H. et al. Defining antigen-specific plasmablast and memory B cell subsets in human blood after viral infection or vaccination. Nat. Immunol. 17, 1226–1234 (2016).
Lau, D. et al. Low CD21 expression defines a population of recent germinal center graduates primed for plasma cell differentiation. Sci. Immunol. 2, eaai8153 (2017).
Lee, J. et al. Molecular-level analysis of the serum antibody repertoire in young adults before and after seasonal influenza vaccination. Nat. Med. 22, 1456–1464 (2016).
Schroeder, H. W. & Cavacini, L. Structure and function of immunoglobulins. J. Allergy Clin. Immunol. 125, S41–52 (2010).
El-Madhun, A. S., Cox, R. J. & Haaheim, L. R. The effect of age and natural priming on the IgG and IgA subclass responses after parenteral influenza vaccination. J. Infect. Dis. 180, 1356–1360 (1999).
Frasca, D. et al. Effects of age on H1N1-specific serum IgG1 and IgG3 levels evaluated during the 2011–2012 influenza vaccine season. Immun. Ageing 10, 14 (2013).
Manenti, A. et al. Comparative analysis of influenza A(H3N2) virus hemagglutinin specific IgG subclass and IgA responses in children and adults after influenza vaccination. Vaccine 35, 191–198 (2017).
Vidarsson, G., Dekkers, G. & Rispens, T. IgG subclasses and allotypes: from structure to effector functions. Front. Immunol. 5, 520 (2014).
Maurer, M. A. et al. Glycosylation of human IgA directly inhibits influenza A and other sialic-acid-binding viruses. Cell Rep. 23, 90–99 (2018).
Cox, M. M., Izikson, R., Post, P. & Dunkle, L. Safety, efficacy, and immunogenicity of Flublok in the prevention of seasonal influenza in adults. Ther. Adv. Vaccines 3, 97–108 (2015).
Berlanda Scorza, F. Advancing new vaccines against pandemic influenza in low-resource countries. Vaccine 35, 5397–5402 (2017).
Robertson, C. A. et al. Fluzone® high-dose influenza vaccine. Expert Rev. Vaccines 15, 1495–1505 (2016).
Tsai, T. F. Fluad®-MF59®-adjuvanted influenza vaccine in older adults. Infect. Chemother. 45, 159–174 (2013).
Isakova-Sivak, I. et al. Genetic bases of the temperature-sensitive phenotype of a master donor virus used in live attenuated influenza vaccines: A/Leningrad/134/17/57 (H2N2). Virology 412, 297–305 (2011).
Kiseleva, I. V. et al. PB2 and PA genes control the expression of the temperature-sensitive phenotype of cold-adapted B/USSR/60/69 influenza master donor virus. J. Gen. Virol. 91, 931–937 (2010).
Mossad, S. B. Demystifying FluMist, a new intranasal, live influenza vaccine. Cleve Clin. J. Med. 70, 801–806 (2003).
Manini, I. et al. Flucelvax (Optaflu) for seasonal influenza. Expert Rev. Vaccines 14, 789–804 (2015).
Talon, J. et al. Influenza A and B viruses expressing altered NS1 proteins: a vaccine approach. Proc. Natl Acad. Sci. USA 97, 4309–4314 (2000).
Mössler, C. et al. Phase I/II trial of a replication-deficient trivalent influenza virus vaccine lacking NS1. Vaccine 31, 6194–6200 (2013).
Bahl, K. et al. Preclinical and clinical demonstration of immunogenicity by mRNA vaccines against H10N8 and H7N9 influenza viruses. Mol. Ther. 25, 1316–1327 (2017).
Scorza, F. B. & Pardi, N. New kids on the block: RNA-based influenza virus vaccines. Vaccines (Basel) 6, E20 (2018). This excellent review discusses mRNA vaccines for influenza virus.
Lee, L. Y. Y., Izzard, L. & Hurt, A. C. A. Review of DNA vaccines against influenza. Front. Immunol. 9, 1568 (2018).
López-Macías, C. Virus-like particle (VLP)-based vaccines for pandemic influenza: Performance of a VLP vaccine during the 2009 influenza pandemic. Hum. Vaccin. Immunother. 8, 411–414 (2012).
Tregoning, J. S., Russell, R. F. & Kinnear, E. Adjuvanted influenza vaccines. Hum. Vaccin. Immunother. 14, 550–564 (2018).
Sebastian, S. & Lambe, T. Clinical advances in viral-vectored influenza vaccines. Vaccines (Basel) 6, E29 (2018).
Sano, K., Ainai, A., Suzuki, T. & Hasegawa, H. Intranasal inactivated influenza vaccines for the prevention of seasonal influenza epidemics. Expert Rev. Vaccines 17, 687–696 (2018).
Ma, J., Rubin, B. K. & Voynow, J. A. Mucins, mucus, and goblet cells. Chest 154, 169–176 (2017).
McAuley, J. L. et al. The cell surface mucin MUC1 limits the severity of influenza A virus infection. Mucosal Immunol. 10, 1581–1593 (2017).
Cohen, M. et al. Influenza A penetrates host mucus by cleaving sialic acids with neuraminidase. Virol. J. 10, 321 (2013).
Acknowledgements
The author thanks P. Wilson, A. Ellebedy and R. Nachbagauer for providing helpful comments and suggestions and J. Bragg for editing the manuscript. The author apologizes to all the colleagues whose great studies could not be cited here owing to space limitations. Work on influenza virus immunology and vaccines in the laboratory of F.K. is funded by the US National Institute of Allergy and Infectious Diseases (NIAID), the US Department of Defense, the Bill and Melinda Gates Foundation, PATH and GlaxoSmithKline. In particular, the author highlights support from the NIAID through the Centers of Excellence for Influenza Research and Surveillance (CEIRS), which has catalysed many of the recent significant advancements in the field.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The Icahn School of Medicine at Mount Sinai has filed patent applications regarding influenza virus vaccines that name F.K. as inventor. The laboratory of F.K. has received funding for a research programme from GlaxoSmithKline.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Glossary
- Zoonotic infections
-
Infections caused by an agent with an animal reservoir that can be transmitted from an animal to a human — for example, H5N1 or H7N9 influenza A viruses.
- Antigenic shift
-
Describes marked changes in the antigenicity of influenza viruses that are caused by the exchange of genomic segments encoding surface glycoproteins, usually involving a change from one virus subtype to another.
- Pandemics
-
Infections caused by a new influenza virus subtype that spreads throughout the human population worldwide.
- Influenza virus epidemics
-
Seasonal outbreaks of influenza virus infection that typically occur during winter months.
- Population immunity
-
Also known as community immunity or herd immunity. Describes a situation in which a large proportion of the population is immune to a virus, thus limiting or completely inhibiting its spread, even to naive individuals.
- Correlate of protection
-
A measurable parameter that correlates with protection of an individual from infection and/or disease.
- Antigenic drift
-
Describes small changes in the antigenicity of influenza viruses that are usually caused by mutations in their surface glycoproteins, mostly in haemagglutinin (HA), leading to immune escape.
- Vaccine effectiveness
-
The ability of a vaccine to reduce disease and/or infection in the field, under non-optimal conditions.
- Immunodominance
-
Describes a phenomenon in which an antigen or epitope is preferentially targeted by the immune system compared with other antigens or epitopes.
- Haemagglutination inhibition assay
-
An assay that measures the ability of serum to block haemagglutination, which is the aggregation (agglutination) of red blood cells caused by influenza virus. The resulting haemagglutination inhibition titre is a correlate of protection for influenza virus that is accepted by many regulatory agencies.
- Seroconversion
-
A measurable increase (typically fourfold) in the titre of specific antibodies that is induced by vaccination or infection.
- Enzyme-linked immunosorbent assay
-
(ELISA). An assay that is used to detect the binding of antibody to antigens.
- Microneutralization assay
-
An assay that measures the ability of serum or antibodies to neutralize influenza virus.
- Imprinting
-
Describes a phenomenon in which the first exposure to influenza virus during childhood leaves an immunological ‘imprint’, whereby subsequent exposures to antigenically different influenza virus strains boost responses to those epitopes that are shared between the two virus strains.
- Group 1 HA proteins
-
A phylogenetic cluster of influenza A virus haemagglutinin (HA) subtypes that includes H1, H2, H5, H6, H8, H9, H11, H12, H13, H16, H17 and H18.
- Glycan shielding
-
Shielding of epitopes from B cell receptors or antibodies by N-linked glycans.
- Group 2 HA proteins
-
A phylogenetic cluster of influenza A virus haemagglutinin (HA) subtypes that includes H3, H4, H7, H10, H14 and H15.
- Neuraminidase inhibition assays
-
Assays that measure the ability of antiserum to block the sialidase activity of neuraminidase (NA).
- Group 1 NA proteins
-
A phylogenetic cluster of influenza A virus neuraminidase (NA) subtypes that includes N1, N4, N5 and N8.
- Group 2 NA proteins
-
A phylogenetic cluster of influenza A virus neuraminidase (NA) subtypes that includes N2, N3, N6, N7 and N9.
- Fc receptor
-
(FcR). A receptor expressed on immune cells to which antibodies can bind via their crystallizable fragment (Fc) region. These receptors are important for antibody-dependent cell-mediated cytotoxicity and antibody-dependent cellular phagocytosis.
- Vaccine efficacy
-
The ability of a vaccine to reduce disease and/or infection in an ideal setting.
- Antibody-dependent cell-mediated cytotoxicity
-
(ADCC). The killing of infected cells by effector cells (for example, natural killer cells) via bound antibody.
- Antibody-dependent cellular phagocytosis
-
(ADCP). The phagocytosis of infected cells or virus by effector cells (for example, macrophages) via bound antibody.
- Complement-dependent lysis
-
The lysis of cells or viruses by complement via bound antibody.
Rights and permissions
About this article
Cite this article
Krammer, F. The human antibody response to influenza A virus infection and vaccination. Nat Rev Immunol 19, 383–397 (2019). https://doi.org/10.1038/s41577-019-0143-6
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41577-019-0143-6
This article is cited by
-
Antigenic drift and immunity gap explain reduction in protective responses against influenza A(H1N1)pdm09 and A(H3N2) viruses during the COVID-19 pandemic: a cross-sectional study of human sera collected in 2019, 2021, 2022, and 2023
Virology Journal (2024)
-
Flipping hemagglutinin on its head
Nature Chemical Biology (2024)
-
Multivalent next generation influenza virus vaccines protect against seasonal and pre-pandemic viruses
Scientific Reports (2024)
-
Effect of Tezepelumab on the Humoral Immune Response to Seasonal Quadrivalent Influenza Vaccination in Patients with Moderate to Severe Asthma: The Phase 3b VECTOR Study
Pulmonary Therapy (2024)
-
Therapeutic mitigation of measles-like immune amnesia and exacerbated disease after prior respiratory virus infections in ferrets
Nature Communications (2024)