Abstract
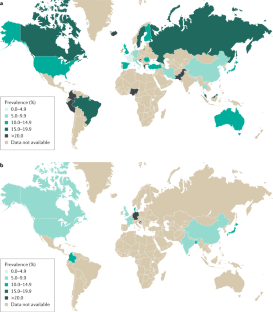
Irritable bowel syndrome (IBS) is one of the most common disorders of gut–brain interaction worldwide, defined according to patterns of gastrointestinal symptoms as described by the Rome diagnostic criteria. However, these criteria, developed with reference to research conducted largely in Western populations, might be limited in their applicability to other countries and cultures. Epidemiological data show a wide variation in the prevalence of IBS globally and more rigorous studies are needed to accurately determine any differences that might exist between countries as well as the potential explanations. The effects of IBS on the individual, in terms of their quality of life, and on health-care delivery and society, in terms of economic costs, are considerable. Although the magnitude of these effects seems to be comparable between nations, their precise nature can vary based on the existence of societal and cultural differences. The pathophysiology of IBS is complex and incompletely understood; genetics, diet and the gut microbiome are all recognized risk factors, but the part they play might be influenced by geography and culture, and hence their relative importance might vary between countries. This Review aims to provide an overview of the burden of IBS in a global context, to discuss future implications for the care of people with IBS worldwide, and to identify key areas for further research.
Key points
-
Irritable bowel syndrome (IBS) is one of the most common disorders of gut–brain interaction, estimated to affect around 1 in 10 people globally.
-
Prevalence rates appear to differ between countries, but the magnitude of the effect of IBS, in terms of cost and quality of life, seems comparable around the world.
-
The pathophysiology of IBS is complex and the role of risk factors such as genetics, diet and the microbiome might operate differently, dependent on geography.
-
As developing countries increasingly adopt a Western diet and lifestyle, we might see a corresponding increase in IBS prevalence rates, a trend that might also reflect increasing awareness of the condition.
-
Even if prevalence rates remain unchanged, projections of global population growth alone indicate that there will be many more people living with IBS worldwide.
-
Well-designed and adequately funded research, which is multi-cultural in design and encourages global collaboration, is needed to further advance our understanding of IBS and promote optimized patient care.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$29.99 / 30 days
cancel any time
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
References
Lovell, R. M. & Ford, A. C. Global prevalence of and risk factors for irritable bowel syndrome: a meta-analysis. Clin. Gastroenterol. Hepatol. 10, 712–721.e4 (2012).
Canavan, C., West, J. & Card, T. Review article: the economic impact of the irritable bowel syndrome. Aliment. Pharmacol. Ther. 40, 1023–1034 (2014).
Gwee, K. A. Irritable bowel syndrome in developing countries – a disorder of civilization or colonization? Neurogastroenterol. Motil. 17, 317–324 (2005).
Danivat, D., Tankeyoon, M. & Sriratanaban, A. Prevalence of irritable bowel syndrome in a non-Western population. Br. Med. J. 296, 1710 (1988).
Gwee, K. A., Wee, S., Wong, M. L. & Png, D. J. The prevalence, symptom characteristics, and impact of irritable bowel syndrome in an asian urban community. Am. J. Gastroenterol. 99, 924–931 (2004).
Xiong, L. S. et al. A population-based epidemiologic study of irritable bowel syndrome in South China: stratified randomized study by cluster sampling. Aliment. Pharmacol. Ther. 19, 1217–1224 (2004).
Corsetti, M., Tack, J., Attara, G. & Sewell, M. IBS global impact report 2018: uncovering the true burden of irritable bowel syndrome (IBS) on people’s lives. GI Society https://badgut.org/wp-content/uploads/IBS-Global-Impact-Report.pdf (2018).
Mearin, F. et al. Bowel disorders. Gastroenterology 150, 1393–1407.e5 (2016).
Sperber, A. D. et al. Conducting multinational, cross-cultural research in the functional gastrointestinal disorders: issues and recommendations. A Rome foundation working team report. Aliment. Pharmacol. Ther. 40, 1094–1102 (2014).
Schmulson, M. et al. A four-country comparison of healthcare systems, implementation of diagnostic criteria, and treatment availability for functional gastrointestinal disorders: a report of the Rome foundation working team on cross-cultural, multinational research. Neurogastroenterol. Motil. 26, 1368–1385 (2014).
Drossman, D. A. Rome IV Functional Gastrointestinal Disorders: Disorders of Gut-Brain Interaction Vol. 1 Ch. 7 (Rome Foundation, 2016).
Palsson, O., Heymen, S. & Whitehead, W. Abdominal pain versus abdominal discomfort: implications for diagnostic assessment of irritable bowel syndrome (IBS) [abstract P0405]. United European Gastroenterol. J. 2, A243 (2014).
Ghoshal, U. C. et al. Epidemiological and clinical profile of irritable bowel syndrome in India: report of the Indian Society of Gastroenterology Task Force. Indian J. Gastroenterol. 27, 22–28 (2008).
Francisconi, C. F. et al. Multicultural aspects in functional gastrointestinal disorders (FGIDs). Gastroenterology 150, 1344–1354.e2 (2016).
Gwee, K. A., Lu, C. L. & Ghoshal, U. C. Epidemiology of irritable bowel syndrome in Asia: something old, something new, something borrowed. J. Gastroenterol. Hepatol. 24, 1601–1607 (2009).
Holtmann, G. J. & Talley, N. J. Inconsistent symptom clusters for functional gastrointestinal disorders in Asia: is Rome burning? Gut 67, 1911–1915 (2018).
Longstreth, G. F. et al. Functional bowel disorders. Gastroenterology 130, 1480–1491 (2006).
Black, C. J., Yiannakou, Y., Houghton, L. A. & Ford, A. C. Epidemiological, clinical, and psychological characteristics of individuals with self-reported irritable bowel syndrome based on the Rome IV vs Rome III criteria. Clin. Gastroenterol. Hepatol. 18, 392–398.e2 (2020).
Sperber, A. D. et al. The global prevalence of IBS in adults remains elusive due to the heterogeneity of studies: a Rome Foundation working team literature review. Gut 66, 1075–1082 (2017).
Sperber, A. et al. Global study of the epidemiology of functional gastrointestinal disorders. ResearchGate https://www.researchgate.net/project/Global-study-of-the-epidemiology-of-the-functional-gastrointestinal-disorders (2019).
Makharia, G. K. et al. Prevalence of irritable bowel syndrome: a community based study from northern India. J. Neurogastroenterol. Motil. 17, 82–87 (2011).
Chang, F. Y. et al. Prevalence of functional gastrointestinal disorders in Taiwan: questionnaire-based survey for adults based on the Rome III criteria. Asia Pac. J. Clin. Nutr. 21, 594–600 (2012).
Krogsgaard, L. R., Engsbro, A. L. & Bytzer, P. The epidemiology of irritable bowel syndrome in Denmark. A population-based survey in adults ≤50 years of age. Scand. J. Gastroenterol. 48, 523–529 (2013).
Matsumoto, S. et al. Relationship between overactive bladder and irritable bowel syndrome: a large-scale internet survey in Japan using the overactive bladder symptom score and Rome III criteria. BJU Int. 111, 647–652 (2013).
Perveen, I., Rahman, M. M., Saha, M., Rahman, M. M. & Hasan, M. Q. Prevalence of irritable bowel syndrome and functional dyspepsia, overlapping symptoms, and associated factors in a general population of Bangladesh. Indian J. Gastroenterol. 33, 265–273 (2014).
Cai, S. T. et al. Overlap of gastroesophageal reflux disease and functional bowel disorders in the general Chinese rural population. J. Dig. Dis. 16, 395–399 (2015).
Le Pluart, D. et al. Functional gastrointestinal disorders in 35,447 adults and their association with body mass index. Aliment. Pharmacol. Ther. 41, 758–767 (2015).
Rasmussen, S. et al. Overlap of symptoms of gastroesophageal reflux disease, dyspepsia and irritable bowel syndrome in the general population. Scand. J. Gastroenterol. 50, 162–169 (2015).
Kanazawa, M. et al. Abdominal bloating is the most bothersome symptom in irritable bowel syndrome with constipation (IBS-C): a large population-based Internet survey in Japan. Biopsychosoc. Med. 10, 19 (2016).
Althaus, A. et al. Determinants and frequency of irritable bowel syndrome in a German sample. Z. Gastroenterol. 54, 217–225 (2016).
Siah, K. T., Wong, R. K., Chan, Y. H., Ho, K. Y. & Gwee, K. A. Prevalence of irritable bowel syndrome in Singapore and its association with dietary, lifestyle, and environmental factors. J. Neurogastroenterol. Motil. 22, 670–676 (2016).
Long, Y. et al. Prevalence and risk factors for functional bowel disorders in South China: a population based study using the Rome III criteria. Neurogastroenterol. Motil. 29, e12897 (2017).
Ghoshal, U. C. & Singh, R. Frequency and risk factors of functional gastro-intestinal disorders in a rural Indian population. J. Gastroenterol. Hepatol. 32, 378–387 (2017).
Saha, M. et al. Irritable bowel syndrome: prevalence and dietary factors in the sylhet district of Bangladesh. Mymensingh Med. J. 27, 82–88 (2018).
Torres, M. J. et al. Food consumption and dietary intakes in 36,448 adults and their association with irritable bowel syndrome: Nutrinet-Sante study. Therap. Adv. Gastroenterol. 11, 1756283x17746625 (2018).
Schauer, B. et al. Irritable bowel syndrome, mental health, and quality of life: data from a population-based survey in Germany (SHIP-Trend-0). Neurogastroenterol. Motil. 31, e13511 (2019).
Iri, R. et al. Epidemiological study of irritable bowel syndrome and its related factors in Sanandaj from 2013 to 2014: a population-based study. Sci. J. Kurd. Univ. Med. Sci. 22, 61–71 (2017).
Keshteli, A. H., Dehestani, B., Daghaghzadeh, H. & Adibi, P. Epidemiological features of irritable bowel syndrome and its subtypes among Iranian adults. Ann. Gastroenterol. 28, 253–258 (2015).
Liu, C. et al. Prevalence of and risk factors for irritable bowel syndrome in community residents in Nanning. World Chin. J. Digestol. 22, 5365–5370 (2014).
Miwa, H. Life style in persons with functional gastrointestinal disorders-large-scale internet survey of lifestyle in Japan. Neurogastroenterol. Motil. 24, 464–471, e217 (2012).
Gomez Alvarez, D. F. et al. Prevalence of irritable bowel syndrome and associated factors according to the Rome III diagnostic criteria in a general population in Colombia [Spanish]. Gastroenterol. Hepatol. 32, 395–400 (2009).
Khoshkrood-Mansoori, B. et al. Irritable bowel syndrome: a population based study. J. Gastrointestin. Liver Dis. 18, 413–418 (2009).
Lee, S. et al. Irritable bowel syndrome is strongly associated with generalized anxiety disorder: a community study. Aliment. Pharmacol. Ther. 30, 643–651 (2009).
Grubic, P. et al. Irritable bowel syndrome in Croatia. Coll. Antropol. 38, 565–570 (2014).
Sperber, A. D., Shvartzman, P., Friger, M. & Fich, A. A comparative reappraisal of the Rome II and Rome III diagnostic criteria: are we getting closer to the ‘true’ prevalence of irritable bowel syndrome? Eur. J. Gastroenterol. Hepatol. 19, 441–447 (2007).
Palsson, O. S., Whitehead, W., Tornblom, H., Sperber, A. D. & Simren, M. Prevalence of Rome IV functional bowel disorders among adults in the United States, Canada, and the United Kingdom. Gastroenterology 158, 1262–1273.e3 (2020).
Lovell, R. M. & Ford, A. C. Effect of gender on prevalence of irritable bowel syndrome in the community: systematic review and meta-analysis. Am. J. Gastroenterol. 107, 991–1000 (2012).
Gwee, K. A., Ghoshal, U. C. & Chen, M. Irritable bowel syndrome in Asia: pathogenesis, natural history, epidemiology, and management. J. Gastroenterol. Hepatol. 33, 99–110 (2018).
Wigington, W. C., Johnson, W. D. & Minocha, A. Epidemiology of irritable bowel syndrome among African Americans as compared with whites: a population-based study. Clin. Gastroenterol. Hepatol. 3, 647–653 (2005).
Kang, J. Y. Systematic review: the influence of geography and ethnicity in irritable bowel syndrome. Aliment. Pharmacol. Ther. 21, 663–676 (2005).
Ho, K. Y., Kang, J. Y. & Seow, A. Prevalence of gastrointestinal symptoms in a multiracial Asian population, with particular reference to reflux-type symptoms. Am. J. Gastroenterol. 93, 1816–1822 (1998).
Rajendra, S. & Alahuddin, S. Prevalence of irritable bowel syndrome in a multi-ethnic Asian population. Aliment. Pharmacol. Ther. 19, 704–706 (2004).
Qumseya, B. J. et al. Irritable bowel syndrome in middle-aged and elderly Palestinians: its prevalence and effect of location of residence. Am. J. Gastroenterol. 109, 723–739 (2014).
Sperber, A. D. et al. Rates of functional bowel disorders among Israeli Bedouins in rural areas compared with those who moved to permanent towns. Clin. Gastroenterol. Hepatol. 3, 342–348 (2005).
Klooker, T. K. et al. Exposure to severe wartime conditions in early life is associated with an increased risk of irritable bowel syndrome: a population-based cohort study. Am. J. Gastroenterol. 104, 2250–2256 (2009).
Gralnek, I. M., Hays, R. D., Kilbourne, A., Naliboff, B. & Mayer, E. A. The impact of irritable bowel syndrome on health-related quality of life. Gastroenterology 119, 654–660 (2000).
Frank, L. et al. Health-related quality of life associated with irritable bowel syndrome: comparison with other chronic diseases. Clin. Ther. 24, 675–689 (2002).
Singh, P. et al. Patients with irritable bowel syndrome-diarrhea have lower disease-specific quality of life than irritable bowel syndrome-constipation. World J. Gastroenterol. 21, 8103–8109 (2015).
Buono, J. L., Carson, R. T. & Flores, N. M. Health-related quality of life, work productivity, and indirect costs among patients with irritable bowel syndrome with diarrhea. Health Qual. Life Outcomes 15, 35 (2017).
Ballou, S. et al. Effects of irritable bowel syndrome on daily activities vary among subtypes based on results from the IBS in America survey. Clin. Gastroenterol. Hepatol. 17, 2471–2478.e36 (2019).
Bushnell, D. M., Martin, M. L., Ricci, J. F. & Bracco, A. Performance of the EQ-5D in patients with irritable bowel syndrome. Value Health 9, 90–97 (2006).
Drossman, D. A. et al. A focus group assessment of patient perspectives on irritable bowel syndrome and illness severity. Dig. Dis. Sci. 54, 1532–1541 (2009).
Lacy, B. E. et al. IBS patients’ willingness to take risks with medications. Am. J. Gastroenterol. 107, 804–809 (2012).
Drossman, D. A. et al. International survey of patients with IBS: symptom features and their severity, health status, treatments, and risk taking to achieve clinical benefit. J. Clin. Gastroenterol. 43, 541–550 (2009).
Canavan, C., West, J. & Card, T. Change in quality of life for patients with irritable bowel syndrome following referral to a gastroenterologist: a cohort study. PLoS One 10, e0139389 (2015).
Weerts, Z. Z. R. M. et al. Reduction in IBS symptom severity is not paralleled by improvement in quality of life in patients with irritable bowel syndrome. Neurogastroenterol. Motil. 31, e13629 (2019).
Spiegel, B. M. et al. Clinical determinants of health-related quality of life in patients with irritable bowel syndrome. Arch. Intern. Med. 164, 1773–1780 (2004).
World Health Organization. WHOQOL: measuring quality of life (WHO, 2019).
Kanazawa, M. et al. Patients and nonconsulters with irritable bowel syndrome reporting a parental history of bowel problems have more impaired psychological distress. Dig. Dis. Sci. 49, 1046–1053 (2004).
Kanazawa, M. et al. Translation and validation of a Japanese version of the irritable bowel syndrome-quality of life measure (IBS-QOL-J). Biopsychosoc. Med. 1, 6 (2007).
Park, J. M. et al. Cross-cultural validation of irritable bowel syndrome quality of life in Korea. Dig. Dis. Sci. 51, 1478–1484 (2006).
Schmulson, M. et al. Further validation of the IBS-QOL: female Mexican IBS patients have poorer quality of life than females from North Carolina. Dig. Dis. Sci. 52, 2950–2955 (2007).
Zhang, F., Xiang, W., Li, C. Y. & Li, S. C. Economic burden of irritable bowel syndrome in China. World J. Gastroenterol. 22, 10450–10460 (2016).
Muller-Lissner, S. A. & Pirk, O. Irritable bowel syndrome in Germany. A cost of illness study. Eur. J. Gastroenterol. Hepatol. 14, 1325–1329 (2002).
Nellesen, D., Yee, K., Chawla, A., Lewis, B. E. & Carson, R. T. A systematic review of the economic and humanistic burden of illness in irritable bowel syndrome and chronic constipation. J. Manag. Care Pharm. 19, 755–764 (2013).
Flacco, M. E. et al. Costs of irritable bowel syndrome in European countries with universal healthcare coverage: a meta-analysis. Eur. Rev. Med. Pharmacol. Sci. 23, 2986–3000 (2019).
Tack, J. et al. Economic burden of moderate to severe irritable bowel syndrome with constipation in six European countries. BMC Gastroenterol. 19, 69 (2019).
Akehurst, R. L. et al. Health-related quality of life and cost impact of irritable bowel syndrome in a UK primary care setting. Pharmacoeconomics 20, 455–462 (2002).
Hungin, A. P., Whorwell, P. J., Tack, J. & Mearin, F. The prevalence, patterns and impact of irritable bowel syndrome: an international survey of 40,000 subjects. Aliment. Pharmacol. Ther. 17, 643–650 (2003).
Frandemark, A., Tornblom, H., Jakobsson, S. & Simren, M. Work productivity and activity impairment in irritable bowel syndrome (IBS): a multifaceted problem. Am. J. Gastroenterol. 113, 1540–1549 (2018).
Cash, B., Sullivan, S. & Barghout, V. Total costs of IBS: employer and managed care perspective. Am. J. Manag. Care 11 (Suppl. 1), S7–S16 (2005).
Leong, S. A. et al. The economic consequences of irritable bowel syndrome: a US employer perspective. Arch. Intern. Med. 163, 929–935 (2003).
Poulsen, C. H. et al. Irritable bowel symptoms, use of healthcare, costs, sickness and disability pension benefits: a long-term population-based study. Scand. J. Public. Health 47, 867–875 (2019).
Wong, R. K. et al. Partner burden in irritable bowel syndrome. Clin. Gastroenterol. Hepatol. 11, 151–155 (2013).
Saito, Y. A. et al. Familial aggregation of irritable bowel syndrome: a family case-control study. Am. J. Gastroenterol. 105, 833–841 (2010).
Waehrens, R., Ohlsson, H., Sundquist, J., Sundquist, K. & Zoller, B. Risk of irritable bowel syndrome in first-degree, second-degree and third-degree relatives of affected individuals: a nationwide family study in Sweden. Gut 64, 215–221 (2015).
Levy, R. L. et al. Irritable bowel syndrome in twins: heredity and social learning both contribute to etiology. Gastroenterology 121, 799–804 (2001).
Bengtson, M. B., Ronning, T., Vatn, M. H. & Harris, J. R. Irritable bowel syndrome in twins: genes and environment. Gut 55, 1754–1759 (2006).
Mohammed, I., Cherkas, L. F., Riley, S. A., Spector, T. D. & Trudgill, N. J. Genetic influences in irritable bowel syndrome: a twin study. Am. J. Gastroenterol. 100, 1340–1344 (2005).
Jin, D. C. et al. Regulation of the serotonin transporter in the pathogenesis of irritable bowel syndrome. World J. Gastroenterol. 22, 8137–8148 (2016).
Zhu, Y., Zheng, G. & Hu, Z. Association between SERT insertion/deletion polymorphism and the risk of irritable bowel syndrome: a meta-analysis based on 7039 subjects. Gene 679, 133–137 (2018).
Garcia-Etxebarria, K. et al. Increased prevalence of rare sucrase-isomaltase pathogenic variants in irritable bowel syndrome patients. Clin. Gastroenterol. Hepatol. 16, 1673–1676 (2018).
Verstraelen, T. E., Ter Bekke, R. M., Volders, P. G., Masclee, A. A. & Kruimel, J. W. The role of the SCN5A-encoded channelopathy in irritable bowel syndrome and other gastrointestinal disorders. Neurogastroenterol. Motil. 27, 906–913 (2015).
Bonfiglio, F. et al. A GWAS meta-analysis from 5 population-based cohorts implicates ion channel genes in the pathogenesis of irritable bowel syndrome. Neurogastroenterol. Motil. 30, e13358 (2018).
Bonfiglio, F. et al. Female-specific association between variants on chromosome 9 and self-reported diagnosis of irritable bowel syndrome. Gastroenterology 155, 168–179 (2018).
Norcliffe-Kaufmann, L., Slaugenhaupt, S. A. & Kaufmann, H. Familial dysautonomia: History, genotype, phenotype and translational research. Prog. Neurobiol. 152, 131–148 (2017).
Komuro, H. et al. Corticotropin-releasing hormone receptor 2 gene variants in irritable bowel syndrome. PLoS One 11, e0147817 (2016).
Sato, N. et al. Corticotropin-releasing hormone receptor 1 gene variants in irritable bowel syndrome. PLoS One 7, e42450 (2012).
Monsbakken, K. W., Vandvik, P. O. & Farup, P. G. Perceived food intolerance in subjects with irritable bowel syndrome–etiology, prevalence and consequences. Eur. J. Clin. Nutr. 60, 667–672 (2006).
Buscail, C. et al. Western dietary pattern is associated with irritable bowel syndrome in the french nutrinet cohort. Nutrients 9, 986 (2017).
Eswaran, S. Low FODMAP in 2017: lessons learned from clinical trials and mechanistic studies. Neurogastroenterol. Motil. 29, e13055 (2017).
Hill, P., Muir, J. G. & Gibson, P. R. Controversies and recent developments of the low-FODMAP diet. Gastroenterol. Hepatol. 13, 36–45 (2017).
Catassi, C. et al. The overlapping area of non-celiac gluten sensitivity (NCGS) and wheat-sensitive irritable bowel syndrome (IBS): an update. Nutrients 9, 1268 (2017).
Dionne, J. et al. A systematic review and meta-analysis evaluating the efficacy of a gluten-free diet and a low FODMAPs diet in treating symptoms of irritable bowel syndrome. Am. J. Gastroenterol. 113, 1290–1300 (2018).
Zhou, Q. et al. Randomised placebo-controlled trial of dietary glutamine supplements for postinfectious irritable bowel syndrome. Gut 68, 996–1002 (2019).
Parker, T. J. et al. Irritable bowel syndrome: is the search for lactose intolerance justified? Eur. J. Gastroenterol. Hepatol. 13, 219–225 (2001).
Varju, P. et al. Lactose intolerance but not lactose maldigestion is more frequent in patients with irritable bowel syndrome than in healthy controls: a meta-analysis. Neurogastroenterol. Motil. 31, e13527, https://doi.org/10.1111/nmo.13527 (2018).
Fritscher-Ravens, A. et al. Many patients with irritable bowel syndrome have atypical food allergies not associated with immunoglobulin E. Gastroenterology 157, 109–118.e5 (2019).
Chong, P. P. et al. The microbiome and irritable bowel syndrome-a review on the pathophysiology, current research and future therapy. Front. Microbiol. 10, 1136 (2019).
Kassinen, A. et al. The fecal microbiota of irritable bowel syndrome patients differs significantly from that of healthy subjects. Gastroenterology 133, 24–33 (2007).
Parthasarathy, G. et al. Relationship between microbiota of the colonic mucosa vs feces and symptoms, colonic transit, and methane production in female patients with chronic constipation. Gastroenterology 150, 367–379.e1 (2016).
Tap, J. et al. Identification of an Intestinal microbiota signature associated with severity of irritable bowel syndrome. Gastroenterology 152, 111–123.e8 (2017).
Enck, P. et al. Irritable bowel syndrome. Nat. Rev. Dis. Primers 2, 16014 (2016).
Quigley, E. M. M. Gut microbiome as a clinical tool in gastrointestinal disease management: are we there yet? Nat. Rev. Gastroenterol. Hepatol. 14, 315–320 (2017).
Halmos, E. P. et al. Diets that differ in their FODMAP content alter the colonic luminal microenvironment. Gut 64, 93–100 (2015).
Pimentel, M. et al. Antibiotic treatment of constipation-predominant irritable bowel syndrome. Dig. Dis. Sci. 59, 1278–1285 (2014).
Ianiro, G. et al. Systematic review with meta-analysis: efficacy of faecal microbiota transplantation for the treatment of irritable bowel syndrome. Aliment. Pharmacol. Ther. 50, 240–248 (2019).
El-Salhy, M., Hatlebakk, J. G., Gilja, O. H., Brathen Kristoffersen, A. & Hausken, T. Efficacy of faecal microbiota transplantation for patients with irritable bowel syndrome in a randomised, double-blind, placebo-controlled study. Gut https://doi.org/10.1136/gutjnl-2019-319630 (2019).
Ford, A. C. et al. Efficacy of prebiotics, probiotics, and synbiotics in irritable bowel syndrome and chronic idiopathic constipation: systematic review and meta-analysis. Am. J. Gastroenterol. 109, 1547–1561 (2014).
Ford, A. C., Harris, L. A., Lacy, B. E., Quigley, E. M. M. & Moayyedi, P. Systematic review with meta-analysis: the efficacy of prebiotics, probiotics, synbiotics and antibiotics in irritable bowel syndrome. Aliment. Pharmacol. Ther. 48, 1044–1060 (2018).
Deschasaux, M. et al. Depicting the composition of gut microbiota in a population with varied ethnic origins but shared geography. Nat. Med. 24, 1526–1531 (2018).
Yatsunenko, T. et al. Human gut microbiome viewed across age and geography. Nature 486, 222–227 (2012).
Mueller, S. et al. Differences in fecal microbiota in different European study populations in relation to age, gender, and country: a cross-sectional study. Appl. Environ. Microbiol. 72, 1027–1033 (2006).
Vangay, P. et al. US immigration westernizes the human gut microbiome. Cell 175, 962–972.e10 (2018).
Spiller, R. & Garsed, K. Postinfectious irritable bowel syndrome. Gastroenterology 136, 1979–1988 (2009).
Card, T. et al. Post-infectious IBS: defining its clinical features and prognosis using an internet-based survey. United European Gastroenterol. J. 6, 1245–1253 (2018).
Neal, K. R., Hebden, J. & Spiller, R. Prevalence of gastrointestinal symptoms six months after bacterial gastroenteritis and risk factors for development of the irritable bowel syndrome: postal survey of patients. BMJ 314, 779–782 (1997).
Thabane, M., Kottachchi, D. T. & Marshall, J. K. Systematic review and meta-analysis: the incidence and prognosis of post-infectious irritable bowel syndrome. Aliment. Pharmacol. Ther. 26, 535–544 (2007).
Wadhwa, A. et al. High risk of post-infectious irritable bowel syndrome in patients with Clostridium difficile infection. Aliment. Pharmacol. Ther. 44, 576–582 (2016).
Ghoshal, U. C. & Rahman, M. M. Post-infection irritable bowel syndrome in the tropical and subtropical regions: Vibrio cholerae is a new cause of this well-known condition. Indian J. Gastroenterol. 38, 87–94 (2019).
Neal, K. R., Barker, L. & Spiller, R. C. Prognosis in post-infective irritable bowel syndrome: a six year follow up study. Gut 51, 410–413 (2002).
Schwille-Kiuntke, J. et al. Postinfectious irritable bowel syndrome: follow-up of a patient cohort of confirmed cases of bacterial infection with Salmonella or Campylobacter. Neurogastroenterol. Motil. 23, e479–e488 (2011).
Rodriguez, L. A. & Ruigomez, A. Increased risk of irritable bowel syndrome after bacterial gastroenteritis: cohort study. BMJ 318, 565–566 (1999).
Zanini, B. et al. Incidence of post-infectious irritable bowel syndrome and functional intestinal disorders following a water-borne viral gastroenteritis outbreak. Am. J. Gastroenterol. 107, 891–899 (2012).
Marshall, J. K., Thabane, M., Borgaonkar, M. R. & James, C. Postinfectious irritable bowel syndrome after a food-borne outbreak of acute gastroenteritis attributed to a viral pathogen. Clin. Gastroenterol. Hepatol. 5, 457–460 (2007).
Hanevik, K. et al. Irritable bowel syndrome and chronic fatigue 6 years after giardia infection: a controlled prospective cohort study. Clin. Infect. Dis. 59, 1394–1400 (2014).
Wensaas, K. A. et al. Irritable bowel syndrome and chronic fatigue 3 years after acute giardiasis: historic cohort study. Gut 61, 214–219 (2012).
Svendsen, A. T., Bytzer, P. & Engsbro, A. L. Systematic review with meta-analyses: does the pathogen matter in post-infectious irritable bowel syndrome? Scand. J. Gastroenterol. 54, 546–562 (2019).
Klem, F. et al. Prevalence, risk factors, and outcomes of irritable bowel syndrome after infectious enteritis: a systematic review and meta-analysis. Gastroenterology 152, 1042–1054.e1 (2017).
Rahman, M. M. et al. Long-term gastrointestinal consequences are frequent following sporadic acute infectious diarrhea in a tropical country: a prospective cohort study. Am. J. Gastroenterol. 113, 1363–1375 (2018).
Parida, P. K. et al. A prospective study on incidence, risk factors, and validation of a risk score for post-infection irritable bowel syndrome in coastal eastern India. Indian J. Gastroenterol. 38, 134–142 (2019).
Youn, Y. H. et al. Long-term clinical course of post-infectious irritable bowel syndrome after shigellosis: a 10-year follow-up study. J. Neurogastroenterol. Motil. 22, 490–496 (2016).
Center for Disease Control and Prevention. Foodborne illness and germs (CDC, 2019).
GBD Diarrhoeal Diseases Collaborators. Estimates of global, regional, and national morbidity, mortality, and aetiologies of diarrhoeal diseases: a systematic analysis for the Global Burden of Disease Study 2015. Lancet Infect. Dis. 17, 909–948 (2017).
Zamani, M., Alizadeh-Tabari, S. & Zamani, V. Systematic review with meta-analysis: the prevalence of anxiety and depression in patients with irritable bowel syndrome. Aliment. Pharmacol. Ther. 50, 132–143 (2019).
Van Oudenhove, L. et al. Biopsychosocial aspects of functional gastrointestinal disorders: how central and environmental processes contribute to the development and expression of functional gastrointestinal disorders. Gastroenterology 150, 1355–1367.e2 (2016).
Koloski, N. A. et al. The brain-gut pathway in functional gastrointestinal disorders is bidirectional: a 12-year prospective population-based study. Gut 61, 1284–1290 (2012).
Quigley, E. M. M. The gut-brain axis and the microbiome: clues to pathophysiology and opportunities for novel management strategies in irritable bowel syndrome (IBS). J. Clin. Med. 7, 6 (2018).
Koloski, N. A., Jones, M. & Talley, N. J. Evidence that independent gut-to-brain and brain-to-gut pathways operate in the irritable bowel syndrome and functional dyspepsia: a 1-year population-based prospective study. Aliment. Pharmacol. Ther. 44, 592–600 (2016).
World Health Organization. Mental disorders affect one in four people (WHO, 2019).
Baxter, A. J. et al. Challenging the myth of an “epidemic” of common mental disorders: trends in the global prevalence of anxiety and depression between 1990 and 2010. Depress. Anxiety 31, 506–516 (2014).
Steel, Z. et al. The global prevalence of common mental disorders: a systematic review and meta-analysis 1980-2013. Int. J. Epidemiol. 43, 476–493 (2014).
Baxter, A. J., Scott, K. M., Vos, T. & Whiteford, H. A. Global prevalence of anxiety disorders: a systematic review and meta-regression. Psychol. Med. 43, 897–910 (2013).
Khoury, C. K. et al. Increasing homogeneity in global food supplies and the implications for food security. Proc. Natl Acad. Sci. USA 111, 4001–4006 (2014).
GlobalData. EpiCast report: irritable bowel syndrome — Epidemiology forecast to 2026 (GlobalData, 2017).
PopulationPyramid.net. Population of the World in 2020. PopulationPyramid.net https://www.populationpyramid.net/world/2020/ (2019).
PopulationPyramid.net. Population of the World 2040. PopulationPyramid.net https://www.populationpyramid.net/world/2040/ (2019).
Davies, S. C. Annual report of the Chief Medical Officer 2015, on the state of the public’s health, baby boomers: fit for the future (Department of Health and Social Care, 2016).
Blue Cross Blue Shield. The health of millennials. bcbs https://www.bcbs.com/the-health-of-america/reports/the-health-of-millennials (2019).
Anderson, N. B. Stress in America: paying with our health (American Psychological Association, 2015).
Bupa. Stress leaves Generation X old before their time. Bupa https://www.bupa.co.uk/newsroom/ourviews/stress-leaves-generation (2016).
Black, C. J. & Ford, A. C. Rational investigations in irritable bowel syndrome. Frontline Gastroenterol. 11, 140–147 (2019).
Lacy, B. E., Ford, A. C. & Talley, N. J. Quality of care and the irritable bowel syndrome: is now the time to set standards? Am. J. Gastroenterol. 113, 167–169 (2018).
Chang, L. et al. Functional bowel disorders: a roadmap to guide the next generation of research. Gastroenterology 154, 723–735 (2018).
International Confederation of Dietetic Associations. Dieticians around the world: their education and their work (ICDA, 2008).
Choudhry, F. R., Mani, V., Ming, L. C. & Khan, T. M. Beliefs and perception about mental health issues: a meta-synthesis. Neuropsychiatr. Dis. Treat. 12, 2807–2818 (2016).
Beck, A., Nadkarni, A., Calam, R., Naeem, F. & Husain, N. Increasing access to cognitive behaviour therapy in low and middle income countries: a strategic framework. Asian J. Psychiatr. 22, 190–195 (2016).
Author information
Authors and Affiliations
Contributions
All authors contributed equally to all aspects of this manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Peer review information
Nature Reviews Gastroenterology & Hepatology thanks S. Fukudo, W. Whitehead and the other, anonymous, reviewer(s) for their contribution to the peer review of this work.
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Black, C.J., Ford, A.C. Global burden of irritable bowel syndrome: trends, predictions and risk factors. Nat Rev Gastroenterol Hepatol 17, 473–486 (2020). https://doi.org/10.1038/s41575-020-0286-8
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41575-020-0286-8
This article is cited by
-
Gastrointestinal and brain barriers: unlocking gates of communication across the microbiota–gut–brain axis
Nature Reviews Gastroenterology & Hepatology (2024)
-
Factors Underlying the Difference in Response to Fecal Microbiota Transplantation Between IBS Patients with Severe and Moderate Symptoms
Digestive Diseases and Sciences (2024)
-
Hydrogen Sulfide Producers Drive a Diarrhea-Like Phenotype and a Methane Producer Drives a Constipation-Like Phenotype in Animal Models
Digestive Diseases and Sciences (2024)
-
Engagement in GI Behavioral Health Is Associated with Reduced Portal Messages, Phone Calls, and ED Visits
Digestive Diseases and Sciences (2024)
-
Assessing the relationship between gut microbiota and irritable bowel syndrome: a two-sample Mendelian randomization analysis
BMC Gastroenterology (2023)



