Abstract
The incidence of acute pancreatitis continues to increase worldwide, and it is one of the most common gastrointestinal causes for hospital admission in the USA. In the past decade, substantial advancements have been made in our understanding of the pathophysiological mechanisms of acute pancreatitis. Studies have elucidated mechanisms of calcium-mediated acinar cell injury and death and the importance of store-operated calcium entry channels and mitochondrial permeability transition pores. The cytoprotective role of the unfolded protein response and autophagy in preventing sustained endoplasmic reticulum stress, apoptosis and necrosis has also been characterized, as has the central role of unsaturated fatty acids in causing pancreatic organ failure. Characterization of these pathways has led to the identification of potential molecular targets for future therapeutic trials. At the patient level, two classification systems have been developed to classify the severity of acute pancreatitis into prognostically meaningful groups, and several landmark clinical trials have informed management strategies in areas of nutritional support and interventions for infected pancreatic necrosis that have resulted in important changes to acute pancreatitis management paradigms. In this Review, we provide a summary of recent advances in acute pancreatitis with a special emphasis on pathophysiological mechanisms and clinical management of the disorder.
Key points
-
The incidence of acute pancreatitis is 34 per 100,000 people in the general population, and it is rising worldwide.
-
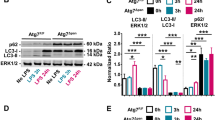
In addition to premature trypsinogen activation, dysfunctional calcium signalling, impaired autophagy, endoplasmic reticulum stress, the unfolded protein response and mitochondrial dysfunction are key cellular processes in the pathogenesis of acute pancreatitis.
-
Well-designed, adequately powered trials are needed to define and examine the efficacy of aggressive fluid resuscitation.
-
Infected walled-off pancreatic necrosis should be managed with an endoscopic step-up strategy.
-
Diabetes and exocrine pancreatic insufficiency are common complications after an episode of acute pancreatitis, occurring in up to one in five patients following acute pancreatitis.
-
Acute pancreatitis impairs long-term quality of life, and many patients experience repeated hospitalizations.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$29.99 / 30 days
cancel any time
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout





Similar content being viewed by others
References
Lugea, A. et al. Human pancreatic acinar cells: proteomic characterization, physiologic responses, and organellar disorders in ex vivo pancreatitis. Am. J. Pathol. 187, 2726–2743 (2017).
Gukovskaya, A. S., Pandol, S. J. & Gukovsky, I. New insights into the pathways initiating and driving pancreatitis. Curr. Opin. Gastroenterol. 32, 429–435 (2016).
Banks, P. A. et al. Classification of acute pancreatitis —2012: revision of the Atlanta classification and definitions by international consensus. Gut 62, 102–111 (2013).
Petrov, M. S. & Yadav, D. Global epidemiology and holistic prevention of pancreatitis. Nat. Rev. Gastroenterol. Hepatol. 16, 175–184 (2018).
Peery, A. F. et al. Burden of gastrointestinal, liver, and pancreatic diseases in the United States. Gastroenterology 149, 1731–1741 (2015).
Munigala, S. et al. Predictors for early readmission in acute pancreatitis (AP) in the United States (US) — a nationwide population based study. Pancreatology 17, 534–542 (2017).
Wadhwa, V. et al. Health care utilization and costs associated with acute pancreatitis. Pancreas 46, 410–415 (2017).
NCD Risk Factor Collaboration (NCD-RisC). Worldwide trends in body-mass index, underweight, overweight, and obesity from 1975 to 2016: a pooled analysis of 2416 population-based measurement studies in 128.9 million children, adolescents, and adults. Lancet 390, 2627–2642 (2017).
Khatua, B., El-Kurdi, B. & Singh, V. P. Obesity and pancreatitis. Curr. Opin. Gastroenterol. 33, 374–382 (2017).
Camilleri, M., Malhi, H. & Acosta, A. Gastrointestinal complications of obesity. Gastroenterology 152, 1656–1670 (2017).
Krishna, S. G., Kamboj, A. K., Hart, P. A., Hinton, A. & Conwell, D. L. The changing epidemiology of acute pancreatitis hospitalizations: a decade of trends and the impact of chronic pancreatitis. Pancreas 46, 482–488 (2017).
Umapathy, C. et al. Natural history after acute necrotizing pancreatitis: a large US tertiary care experience. J. Gastrointest. Surg. 20, 1844–1853 (2016).
Yadav, D., O’Connell, M. & Papachristou, G. I. Natural history following the first attack of acute pancreatitis. Am. J. Gastroenterol. 107, 1096–1103 (2012).
Machicado, J. D. et al. Acute pancreatitis has a long-term deleterious effect on physical health related quality of life. Clin. Gastroenterol. Hepatol. 15, 1435–1443 (2017).
Das, S. L. et al. Newly diagnosed diabetes mellitus after acute pancreatitis: a systematic review and meta-analysis. Gut 63, 818–831 (2014).
Hollemans, R. A. et al. Pancreatic exocrine insufficiency following acute pancreatitis: systematic review and study level meta-analysis. Pancreatology 18, 253–262 (2018).
Vipperla, K. et al. Risk of and factors associated with readmission after a sentinel attack of acute pancreatitis. Clin. Gastroenterol. Hepatol. 12, 1911–1919 (2014).
Ali, U. A. et al. Risk of recurrent pancreatitis and progression to chronic pancreatitis after a first episode of acute pancreatitis. Clin. Gastroenterol. Hepatol. 14, 738–746 (2016).
Javed, M. A. et al. TRO40303 ameliorates alcohol-induced pancreatitis through reduction of fatty acid ethyl ester-induced mitochondrial injury and necrotic cell death. Pancreas 47, 18–24 (2018).
Wen, L. et al. Inhibitors of ORAI1 prevent cytosolic calcium-associated injury of human pancreatic acinar cells and acute pancreatitis in 3 mouse models. Gastroenterology 149, 481–492 (2015).
Criddle, D. N., McLaughlin, E., Murphy, J. A., Petersen, O. H. & Sutton, R. The pancreas misled: signals to pancreatitis. Pancreatology 7, 436–446 (2007).
Marta, K. et al. High versus low energy administration in the early phase of acute pancreatitis (GOULASH trial): protocol of a multicentre randomised double-blind clinical trial. BMJ Open 7, e015874 (2017).
Noel, P. et al. Peripancreatic fat necrosis worsens acute pancreatitis independent of pancreatic necrosis via unsaturated fatty acids increased in human pancreatic necrosis collections. Gut 65, 100–111 (2016).
Bradbury, K. E. et al. Lipolysis of visceral adipocyte triglyceride by pancreatic lipases converts mild acute pancreatitis to severe pancreatitis independent of necrosis and inflammation. Gastroenterology 15, 100–111 (2017).
Acharya, C. et al. Fibrosis reduces severity of acute-on-chronic pancreatitis in humans. Gastroenterology 145, 466–475 (2013).
Al-Bahrani, A. Z. & Ammori, B. J. Clinical laboratory assessment of acute pancreatitis. Clin. Chim. Acta 362, 26–48 (2005).
Tenner, S., Baillie, J., DeWitt, J. & Vege, S. S. & of Gastroenterology, A. C. American College of Gastroenterology guideline: management of acute pancreatitis. Am. J. Gastroenterol. 108, 1400–1415 (2013).
Crockett, S. D., Wani, S., Gardner, T. B., Falck-Ytter, Y. & Barkun, A. N. American Gastroenterological Association Institute Guideline on Initial Management of Acute Pancreatitis. Gastroenterology 154, 1096–1101 (2018).
Isaji, S. et al. Revised Japanese guidelines for the management of acute pancreatitis 2015: revised concepts and updated points. J. Hepatobiliary Pancreat. Sci. 22, 433–445 (2015).
Working Group IAP/APA Acute Pancreatitis Guidelines. IAP/APA evidence-based guidelines for the management of acute pancreatitis. Pancreatology 13, e1–e15 (2013).
Gerasimenko, J. V. et al. Ca2+ release-activated Ca2+ channel blockade as a potential tool in antipancreatitis therapy. Proc. Natl Acad. Sci. USA 110, 13186–13191 (2013).
Murphy, J. A. et al. Direct activation of cytosolic Ca2+ signaling and enzyme secretion by cholecystokinin in human pancreatic acinar cells. Gastroenterology 135, 632–641 (2008).
Biczo, G. et al. Mitochondrial dysfunction, through impaired autophagy, leads to endoplasmic reticulum stress, deregulated lipid metabolism, and pancreatitis in animal models. Gastroenterology 154, 689–703 (2018).
Mukherjee, R. et al. Mechanism of mitochondrial permeability transition pore induction and damage in the pancreas: inhibition prevents acute pancreatitis by protecting production of ATP. Gut 65, 1333–1346 (2016).
Aghdassi, A. A. et al. Cathepsin D regulates cathepsin B activation and disease severity predominantly in inflammatory cells during experimental pancreatitis. J. Biol. Chem. 293, 1018–1029 (2018).
Talukdar, R. et al. Release of cathepsin B in cytosol causes cell death in acute pancreatitis. Gastroenterology 151, 747–758 (2016).
Dawra, R. et al. Intra-acinar trypsinogen activation mediates early stages of pancreatic injury but not inflammation in mice with acute pancreatitis. Gastroenterology 141, 2210–2217 (2011).
Wartmann, T. et al. Cathepsin L inactivates human trypsinogen, whereas cathepsin L-deletion reduces the severity of pancreatitis in mice. Gastroenterology 138, 726–737 (2010).
Gukovskaya, A. S. et al. Neutrophils and NADPH oxidase mediate intrapancreatic trypsin activation in murine experimental acute pancreatitis. Gastroenterology 122, 974–984 (2002).
Halangk, W. et al. Role of cathepsin B in intracellular trypsinogen activation and the onset of acute pancreatitis. J. Clin. Invest. 106, 773–781 (2000).
Sendler, M. et al. Cathepsin B-mediated activation of trypsinogen in endocytosing macrophages increases severity of pancreatitis in mice. Gastroenterology 154, 704–718 (2018).
Zeng, Y., Wang, X., Zhang, W., Wu, K. & Ma, J. Hypertriglyceridemia aggravates ER stress and pathogenesis of acute pancreatitis. Hepatogastroenterology 59, 2318–2326 (2012).
Wu, J. S., Li, W. M., Chen, Y. N., Zhao, Q. & Chen, Q. F. Endoplasmic reticulum stress is activated in acute pancreatitis. J. Dig. Dis. 17, 295–303 (2016).
Lugea, A. et al. Adaptive unfolded protein response attenuates alcohol-induced pancreatic damage. Gastroenterology 140, 987–997 (2011).
Antonucci, L. et al. Basal autophagy maintains pancreatic acinar cell homeostasis and protein synthesis and prevents ER stress. Proc. Natl Acad. Sci. USA 112, 6166 (2015).
Sendler, M. et al. Tumour necrosis factor alpha secretion induces protease activation and acinar cell necrosis in acute experimental pancreatitis in mice. Gut 62, 430–439 (2013).
Merza, M. et al. Neutrophil extracellular traps induce trypsin activation, inflammation, and tissue damage in mice with severe acute pancreatitis. Gastroenterology 149, 1931 (2015).
Jakkampudi, A. et al. NF-kappaB in acute pancreatitis: Mechanisms and therapeutic potential. Pancreatology 16, 477–488 (2016).
Shanbhag, S. T. et al. Acute pancreatitis conditioned mesenteric lymph causes cardiac dysfunction in rats independent of hypotension. Surgery 163, 1097–1105 (2018).
Mole, D. J. et al. Tryptophan catabolites in mesenteric lymph may contribute to pancreatitis-associated organ failure. Br. J. Surg. 95, 855–867 (2008).
Mittal, A. et al. The proteome of mesenteric lymph during acute pancreatitis and implications for treatment. JOP 10, 130–142 (2009).
Flint, R. S. et al. Acute pancreatitis severity is exacerbated by intestinal ischemia-reperfusion conditioned mesenteric lymph. Surgery 143, 404–413 (2008).
Gorelick, F. S. & Lerch, M. M. Do animal models of acute pancreatitis reproduce human disease? Cell. Mol. Gastroenterol. Hepatol. 4, 251–262 (2017).
Gukovskaya, A. S., Gukovsky, I., Algul, H. & Habtezion, A. Autophagy, inflammation, and immune dysfunction in the pathogenesis of pancreatitis. Gastroenterology 153, 1212–1226 (2017).
Lampel, M. & Kern, H. F. Acute interstitial pancreatitis in the rat induced by excessive doses of a pancreatic secretagogue. Virchows Arch. A 373, 97–117 (1977).
Pandol, S. J., Gukovsky, I., Satoh, A., Lugea, A. & Gukovskaya, A. S. Animal and in vitro models of alcoholic pancreatitis: role of cholecystokinin. Pancreas 27, 297–300 (2003).
Criddle, D. N. The role of fat and alcohol in acute pancreatitis: a dangerous liaison. Pancreatology 15, S6–S12 (2015).
Huang, W. et al. Fatty acid ethyl ester synthase inhibition ameliorates ethanol-induced Ca2+-dependent mitochondrial dysfunction and acute pancreatitis. Gut 63, 1313–1324 (2014).
Hegyi, P., Pandol, S., Venglovecz, V. & Rakonczay, Z. J. The acinar-ductal tango in the pathogenesis of acute pancreatitis. Gut 60, 544–552 (2011).
Noble, M. D., Romac, J., Vigna, S. R. & Liddle, R. A. A. pH-sensitive, neurogenic pathway mediates disease severity in a model of post-ERCP pancreatitis. Gut 57, 1566–1571 (2008).
Lerch, M. M. et al. Acute necrotizing pancreatitis in the opossum: earliest morphological changes involve acinar cells. Gastroenterology 103, 205–213 (1992).
Senninger, N., Moody, F. G., Coelho, J. C. & Van Buren, D. H. The role of biliary obstruction in the pathogenesis of acute pancreatitis in the opossum. Surgery 99, 688–693 (1986).
Runkel, N. S., Rodriguez, L. F., Moody, F. G., LaRocco, M. T. & Blasdel, T. Salmonella infection of the biliary and intestinal tract of wild opossums. Lab. Anim. Sci. 41, 54–56 (1991).
Senninger, N. & Runkel, N. in Essentials of Experimental Surgery: Gastroenterology Ch. 23 (eds Gregerson, H. et al.) (Gordon and Breach Publishing Group, 1995).
Dolai, S. et al. Pancreatitis-induced depletion of syntaxin 2 promotes autophagy and increases basolateral exocytosis. Gastroenterology 154, 1805–1821 (2018).
Kruger, B., Albrecht, E. & Lerch, M. M. The role of intracellular calcium signaling in premature protease activation and the onset of pancreatitis. Am. J. Pathol. 157, 43–50 (2000).
Maleth, J. & Hegyi, P. Ca2+ toxicity and mitochondrial damage in acute pancreatitis: translational overview. Phil. Trans. R. Soc. B 371, 20150425 (2016).
Zhang, S. L. et al. STIM1 is a Ca2+ sensor that activates CRAC channels and migrates from the Ca2+ store to the plasma membrane. Nature 437, 902–905 (2005).
Lur, G. et al. InsP(3)receptors and Orai channels in pancreatic acinar cells: co-localization and its consequences. Biochem. J. 436, 231–239 (2011).
Romac, J. M.-J., Shahid, R. A., Swain, S. M., Vigna, S. R. & Liddle, R. A. Piezo1 is a mechanically activated ion channel and mediates pressure induced pancreatitis. Nat. Commun. 9, 1715 (2018).
Elmunzer, B. J. et al. Rectal indomethacin alone versus indomethacin and prophylactic pancreatic stent placement for preventing pancreatitis after ERCP: study protocol for a randomized controlled trial. Trials 17, 2 (2016).
Atar, D. et al. Effect of intravenous TRO40303 as an adjunct to primary percutaneous coronary intervention for acute ST-elevation myocardial infarction: MITOCARE study results. Eur. Heart J. 36, 112–119 (2015).
Le Lamer, S. et al. Translation of TRO40303 from myocardial infarction models to demonstration of safety and tolerance in a randomized phase I trial. J. Transl Med. 12, 38 (2014).
Saluja, A. K. et al. Secretagogue-induced digestive enzyme activation and cell injury in rat pancreatic acini. Am. J. Physiol. 276, G835–G842 (1999).
Wilson, J. S. et al. Both ethanol consumption and protein deficiency increase the fragility of pancreatic lysosomes. J. Lab. Clin. Med. 115, 749–755 (1990).
Haber, P. S., Wilson, J. S., Apte, M. V., Korsten, M. A. & Pirola, R. C. Chronic ethanol consumption increases the fragility of rat pancreatic zymogen granules. Gut 35, 1474–1478 (1994).
Louhimo, J., Steer, M. L. & Perides, G. Necroptosis is an important severity determinant and potential therapeutic target in experimental severe pancreatitis. Cell. Mol. Gastroenterol. Hepatol. 2, 519–535 (2016).
Han, J., Zhong, C.-Q. & Zhang, D.-W. Programmed necrosis: backup to and competitor with apoptosis in the immune system. Nat. Immunol. 12, 1143–1149 (2011).
He, S. et al. Receptor interacting protein kinase-3 determines cellular necrotic response to TNF-alpha. Cell 137, 1100–1111 (2009).
Wang, G., Qu, F.-Z., Li, L., Lv, J.-C. & Sun, B. Necroptosis: a potential, promising target and switch in acute pancreatitis. Apoptosis 21, 121–129 (2016).
Diakopoulos, K. N. et al. Impaired autophagy induces chronic atrophic pancreatitis in mice via sex- and nutrition-dependent processes. Gastroenterology 148, 626–638 (2015).
Mareninova, O. A. et al. Impaired autophagic flux mediates acinar cell vacuole formation and trypsinogen activation in rodent models of acute pancreatitis. J. Clin. Invest. 119, 3340–3355 (2009).
Lugea, A. et al. The combination of alcohol and cigarette smoke induces endoplasmic reticulum stress and cell death in pancreatic acinar cells. Gastroenterology 153, 1674–1686 (2017).
Zelic, M. et al. RIP kinase 1-dependent endothelial necroptosis underlies systemic inflammatory response syndrome. J. Clin. Invest. 128, 2064–2075 (2018).
Lee, H.-J., Yoon, Y.-S. & Lee, S.-J. Mechanism of neuroprotection by trehalose: controversy surrounding autophagy induction. Cell Death Dis. 9, 712 (2018).
Ron, D. & Walter, P. Signal integration in the endoplasmic reticulum unfolded protein response. Nat. Rev. Mol. Cell. Biol. 8, 519–529 (2007).
Kim, I., Xu, W. & Reed, J. C. Cell death and endoplasmic reticulum stress: disease relevance and therapeutic opportunities. Nat. Rev. Drug Discov. 7, 1013–1030 (2008).
Seyhun, E. et al. Tauroursodeoxycholic acid reduces endoplasmic reticulum stress, acinar cell damage, and systemic inflammation in acute pancreatitis. Am. J. Physiol. Liver Physiol. 301, 773 (2011).
Pandol, S. J., Gorelick, F. S. & Lugea, A. Environmental and genetic stressors and the unfolded protein response in exocrine pancreatic function — a hypothesis. Front. Physiol. 2, 8 (2011).
Richardson, C. E., Kooistra, T. & Kim, D. H. An essential role for XBP-1 in host protection against immune activation in C. elegans. Nature 463, 1092–1095 (2010).
Xu, C., Bailly-Maitre, B. & Reed, J. C. Endoplasmic reticulum stress: cell life and death decisions. J. Clin. Invest. 115, 2656–2664 (2005).
Chen, J. C., Wu, M. L., Huang, K. C. & Lin, W. W. HMG-CoA reductase inhibitors activate the unfolded protein response and induce cytoprotective GRP78 expression. Cardiovasc. Res. 80, 138–150 (2008).
Morck, C. et al. Statins inhibit protein lipidation and induce the unfolded protein response in the non-sterol producing nematode. Caenorhabditis elegans. Proc. Natl Acad. Sci. USA 106, 18285–18290 (2009).
Wu, B. U., Pandol, S. J. & Liu, I. L. Simvastatin is associated with reduced risk of acute pancreatitis: findings from a regional integrated healthcare system. Gut 64, 133–138 (2015).
Gornik, I., Gasparovic, V., Vrdoljak, N. G., Haxiu, A. & Vucelic, B. Prior statin therapy is associated with milder course and better outcome in acute pancreatitis—a cohort study. Pancreatology 13, 196–200 (2013).
Lee, P. J. et al. Association of statins with decreased acute pancreatitis severity: a propensity score analysis. J. Clin. Gastroenterol. 52, 742–746 (2017).
US National Library of Medicine. ClinicalTrials.gov https://clinicaltrials.gov/ct2/show/NCT02743364 (2019).
Venglovecz, V. et al. The importance of aquaporin 1 in pancreatitis and its relation to the CFTR Cl(-) channel. Front. Physiol. 9, 854 (2018).
Pallagi, P., Hegyi, P. & Rakonczay, Z. J. The physiology and pathophysiology of pancreatic ductal secretion: the background for clinicians. Pancreas 44, 1211–1233 (2015).
Hegyi, P. et al. CFTR: a new horizon in the pathomechanism and treatment of pancreatitis. Rev. Physiol. Biochem. Pharmacol. 170, 37–66 (2016).
Hegyi, P. & Petersen, O. H. The exocrine pancreas: the acinar-ductal tango in physiology and pathophysiology. Rev. Physiol. Biochem. Pharmacol. 165, 1–30 (2013).
Maleth, J. et al. Alcohol disrupts levels and function of the cystic fibrosis transmembrane conductance regulator to promote development of pancreatitis. Gastroenterology 148, 427–439 (2015).
Venglovecz, V. et al. Effects of bile acids on pancreatic ductal bicarbonate secretion in guinea pig. Gut 57, 1102–1112 (2008).
Vigna, S. R., Shahid, R. A., Nathan, J. D., McVey, D. C. & Liddle, R. A. Leukotriene B4 mediates inflammation via TRPV1 in duct obstruction-induced pancreatitis in rats. Pancreas 40, 708–714 (2011).
Wen, L. et al. Transient high pressure in pancreatic ducts promotes inflammation and alters tight junctions via calcineurin signaling in mice. Gastroenterology 155, 1250–1263 (2018).
Orabi, A. I. et al. Targeted inhibition of pancreatic acinar cell calcineurin is a novel strategy to prevent post-ERCP pancreatitis. Cell. Mol. Gastroenterol. Hepatol. 3, 119–128 (2017).
Maleth, J. et al. Non-conjugated chenodeoxycholate induces severe mitochondrial damage and inhibits bicarbonate transport in pancreatic duct cells. Gut 60, 136–138 (2011).
Perides, G., Laukkarinen, J. M., Vassileva, G. & Steer, M. L. Biliary acute pancreatitis in mice is mediated by the G-protein-coupled cell surface bile acid receptor Gpbar1. Gastroenterology 138, 715–725 (2010).
Elliot, D. W., Williams, R. D. & Zollinger, R. M. Alterations in the pancreatic resistance to bile in the pathogenesis of acute pancreatitis. Ann. Surg. 146, 662–669 (1957).
Lerch, M. M. & Aghdassi, A. A. The role of bile acids in gallstone-induced pancreatitis. Gastroenterology 138, 429–433 (2010).
Rakonczay, Z. J., Hegyi, P., Takacs, T., McCarroll, J. & Saluja, A. K. The role of NF-kappaB activation in the pathogenesis of acute pancreatitis. Gut 57, 259–267 (2008).
Watanabe, T., Kudo, M. & Strober, W. Immunopathogenesis of pancreatitis. Mucosal Immunol. 10, 283–298 (2017).
Griffith, J. W., Sokol, C. L. & Luster, A. D. Chemokines and chemokine receptors: positioning cells for host defense and immunity. Annu. Rev. Immunol. 32, 659–702 (2014).
Zhou, G.-X. et al. Protective effects of MCP-1 inhibitor on a rat model of severe acute pancreatitis. Hepatobiliary Pancreat. Dis. Int. 9, 201–207 (2010).
Bhatia, M. et al. Treatment with neutralising antibody against cytokine induced neutrophil chemoattractant (CINC) protects rats against acute pancreatitis associated lung injury. Gut 47, 838–844 (2000).
Malla, S. R. et al. Effect of oral administration of AZD8309, a CXCR2 antagonist, on the severity of experimental pancreatitis. Pancreatology 16, 761–769 (2016).
Saeki, K. et al. CCL2-induced migration and SOCS3-mediated activation of macrophages are involved in cerulein-induced pancreatitis in mice. Gastroenterology 142, 1010–1020 (2012).
Bhatia, M. & Hegde, A. Treatment with antileukinate, a CXCR2 chemokine receptor antagonist, protects mice against acute pancreatitis and associated lung injury. Regul. Pept. 138, 40–48 (2007).
Pastor, C. M. et al. Role of macrophage inflammatory peptide-2 in cerulein-induced acute pancreatitis and pancreatitis-associated lung injury. Lab. Invest. 83, 471–478 (2003).
Frossard, J. L. et al. Role of CCL-2, CCR-2 and CCR-4 in cerulein-induced acute pancreatitis and pancreatitis-associated lung injury. J. Clin. Pathol. 64, 387–393 (2011).
Gerard, C. et al. Targeted disruption of the beta-chemokine receptor CCR1 protects against pancreatitis-associated lung injury. J. Clin. Invest. 100, 2022–2027 (1997).
He, M., Horuk, R. & Bhatia, M. Treatment with BX471, a nonpeptide CCR1 antagonist, protects mice against acute pancreatitis-associated lung injury by modulating neutrophil recruitment. Pancreas 34, 233–241 (2007).
Papachristou, G. I. Prediction of severe acute pancreatitis: current knowledge and novel insights. World J. Gastroenterol. 14, 6273–6275 (2008).
Jakkampudi, A. et al. Acinar injury and early cytokine response in human acute biliary pancreatitis. Sci. Rep. 7, 2 (2017).
Gu, H. et al. Necro-inflammatory response of pancreatic acinar cells in the pathogenesis of acute alcoholic pancreatitis. Cell Death Dis. 4, e816 (2013).
Ushio-Fukai, M. Compartmentalization of redox signaling through NADPH oxidase-derived ROS. Antioxid. Redox Signal. 11, 1289–1299 (2009).
Eppensteiner, J., Davis, R. P., Barbas, A. S., Kwun, J. & Lee, J. Immunothrombotic activity of damage-associated molecular patterns and extracellular vesicles in secondary organ failure induced by trauma and sterile insults. Front. Immunol. 9, 190 (2018).
Yasuda, T. et al. Significant increase of serum high-mobility group box chromosomal protein 1 levels in patients with severe acute pancreatitis. Pancreas 33, 359–363 (2006).
Sharif, R. et al. Impact of toll-like receptor 4 on the severity of acute pancreatitis and pancreatitis-associated lung injury in mice. Gut 58, 813–819 (2009).
Hoque, R. et al. TLR9 and the NLRP3 inflammasome link acinar cell death with inflammation in acute pancreatitis. Gastroenterology 141, 358–369 (2011).
Lee, B., Zhao, Q. & Habtezion, A. Immunology of pancreatitis and environmental factors. Curr. Opin. Gastroenterol. 33, 383–389 (2017).
Hoque, R. Update on innate immunity and perspectives on metabolite regulation in acute pancreatitis. Curr. Opin. Gastroenterol. 32, 507–512 (2016).
Hoque, R., Farooq, A., Ghani, A., Gorelick, F. & Mehal, W. Z. Lactate reduces liver and pancreatic injury in Toll-like receptor- and inflammasome-mediated inflammation via GPR81-mediated suppression of innate immunity. Gastroenterology 146, 1763–1774 (2014).
Primiano, M. J. et al. Efficacy and pharmacology of the NLRP3 inflammasome inhibitor CP-456,773 (CRID3) in murine models of dermal and pulmonary inflammation. J. Immunol. 197, 2421–2433 (2016).
Mridha, A. R. et al. NLRP3 inflammasome blockade reduces liver inflammation and fibrosis in experimental NASH in mice. J. Hepatol. 66, 1037–1046 (2017).
Gao, L. et al. NLRP3 inflammasome: a promising target in ischemic stroke. Inflamm. Res. 66, 17–24 (2017).
Li, G. et al. TLR4-mediated NF-kappaB signaling pathway mediates HMGB1-induced pancreatic injury in mice with severe acute pancreatitis. Int. J. Mol. Med. 37, 99–107 (2016).
Wu, B. U. et al. Lactated Ringer’s solution reduces systemic inflammation compared with saline in patients with acute pancreatitis. Clin. Gastroenterol. Hepatol. 9, 717 (2011).
Choi, J. H., Kim, H. J., Lee, B. U., Kim, T. H. & Song, I. H. Vigorous periprocedural hydration with lactated Ringer’s solution reduces the risk of pancreatitis after retrograde cholangiopancreatography in hospitalized patients. Clin. Gastroenterol. Hepatol. 15, 92 (2017).
Aoun, E. et al. Diagnostic accuracy of interleukin-6 and interleukin-8 in predicting severe acute pancreatitis: a meta-analysis. Pancreatology 9, 777–785 (2009).
Zhang, H. et al. IL-6 trans-signaling promotes pancreatitis-associated lung injury and lethality. J. Clin. Invest. 123, 1019–1031 (2013).
Sathyanarayan, G., Garg, P. K., Prasad, H. & Tandon, R. K. Elevated level of interleukin-6 predicts organ failure and severe disease in patients with acute pancreatitis. J. Gastroenterol. Hepatol. 22, 550–554 (2007).
Dianliang, Z., Jieshou, L., Zhiwei, J. & Baojun, Y. Association of plasma levels of tumor necrosis factor (TNF)-alpha and its soluble receptors, two polymorphisms of the TNF gene, with acute severe pancreatitis and early septic shock due to it. Pancreas 26, 339–343 (2003).
Vege, S. S. et al. Pentoxifylline treatment in severe acute pancreatitis: a pilot, double-blind, placebo-controlled, randomized trial. Gastroenterology 149, 318–320 (2015).
Stone, J. H. et al. Trial of tocilizumab in giant-cell arteritis. N. Engl. J. Med. 377, 317–328 (2017).
Schirmer, M., Muratore, F. & Salvarani, C. Tocilizumab for the treatment of giant cell arteritis. Expert Rev. Clin. Immunol. 14, 339–349 (2018).
Chen, K.-L. et al. Effects of tocilizumab on experimental severe acute pancreatitis and associated acute lung injury. Crit. Care Med. 44, e664–e677 (2016).
Yucebay, F. et al. Tocilizumab as first-line therapy for steroid-refractory acute graft-versus-host-disease: analysis of a single-center experience. Leuk. Lymphoma 15, 1–7 (2019).
Pablos, J. L. et al. Efficacy of tocilizumab monotherapy after response to combined tocilizumab and methotrexate in patients with rheumatoid arthritis: the randomised JUST-ACT study. Clin. Exp. Rheumatol. (in the press).
Friess, H. et al. Enhanced expression of TGF-betas and their receptors in human acute pancreatitis. Ann. Surg. 227, 95–104 (1998).
Deviere, J. et al. Interleukin 10 reduces the incidence of pancreatitis after therapeutic endoscopic retrograde cholangiopancreatography. Gastroenterology 120, 498–505 (2001).
Hutchins, A. P., Diez, D. & Miranda-Saavedra, D. The IL-10/STAT3-mediated anti-inflammatory response: recent developments and future challenges. Brief. Funct. Genomics 12, 489–498 (2013).
Lin, R. et al. Interleukin-10 attenuates impairment of the blood-brain barrier in a severe acute pancreatitis rat model. J. Inflamm. 15, 4 (2018).
Warzecha, Z. et al. IGF-1 stimulates production of interleukin-10 and inhibits development of caerulein-induced pancreatitis. J. Physiol. Pharmacol. 54, 575–590 (2003).
Sharma, D. et al. Association of systemic inflammatory and anti-inflammatory responses with adverse outcomes in acute pancreatitis: preliminary results of an ongoing study. Dig. Dis. Sci. 62, 3468–3478 (2017).
Hasan, A., Moscoso, D. I. & Kastrinos, F. The role of genetics in pancreatitis. Gastrointest. Endosc. Clin. N. Am. 28, 587–603 (2018).
Zator, Z. & Whitcomb, D. C. Insights into the genetic risk factors for the development of pancreatic disease. Therap. Adv. Gastroenterol. 10, 323–336 (2017).
Krishna, S. G. et al. Morbid obesity is associated with adverse clinical outcomes in acute pancreatitis: a propensity-matched study. Am. J. Gastroenterol. 110, 1608–1619 (2015).
Navina, S. et al. Lipotoxicity causes multisystem organ failure and exacerbates acute pancreatitis in obesity. Sci. Transl Med. 3, 107ra110 (2011).
Fallon, M. B. et al. Effect of cerulein hyperstimulation on the paracellular barrier of rat exocrine pancreas. Gastroenterology 108, 1863–1872 (1995).
Gaisano, H. Y. et al. Supramaximal cholecystokinin displaces Munc18c from the pancreatic acinar basal surface, redirecting apical exocytosis to the basal membrane. J. Clin. Invest. 108, 1597–1611 (2001).
Durgampudi, C. et al. Acute lipotoxicity regulates severity of biliary acute pancreatitis without affecting its initiation. Am. J. Pathol. 184, 1773–1784 (2014).
Umpaichitra, V., Banerji, M. A. & Castells, S. Postprandial hyperlipidemia after a fat loading test in minority adolescents with type 2 diabetes mellitus and obesity. J. Pediatr. Endocrinol. Metab. 17, 853–864 (2004).
Natu, A. et al. Visceral adiposity predicts severity of acute pancreatitis. Pancreas 46, 776–781 (2017).
Halleux, C. M. et al. Secretion of adiponectin and regulation of apM1 gene expression in human visceral adipose tissue. Biochem. Biophys. Res. Commun. 288, 1102–1107 (2001).
Nawaz, H. et al. Elevated serum triglycerides are independently associated with persistent organ failure in acute pancreatitis. Am. J. Gastroenterol. 110, 1497–1503 (2015).
Patel, K. et al. Lipolysis of visceral adipocyte triglyceride by pancreatic lipases converts mild acute pancreatitis to severe pancreatitis independent of necrosis and inflammation. Am. J. Pathol. 185, 808–819 (2015).
Ammori, B. J. et al. Early increase in intestinal permeability in patients with severe acute pancreatitis: correlation with endotoxemia, organ failure, and mortality. J. Gastrointest. Surg. 3, 252–262 (1999).
Blenkiron, C. et al. MicroRNAs in mesenteric lymph and plasma during acute pancreatitis. Ann. Surg. 260, 341–347 (2014).
Landahl, P., Ansari, D. & Andersson, R. Severe acute pancreatitis: gut barrier failure, systemic inflammatory response, acute lung injury, and the role of the mesenteric lymph. Surg. Infect. 16, 651–656 (2015).
Peng, H. et al. Blocking abdominal lymphatic flow attenuates acute hemorrhagic necrotizing pancreatitis -associated lung injury in rats. J. Inflamm. 10, 9 (2013).
Zhang, D., Tsui, N., Li, Y. & Wang, F. Thoracic duct ligation in the rat attenuates lung injuries in acute pancreatitis. Lymphology 46, 144–149 (2013).
Toliyat, M. et al. Interventional radiology in the management of thoracic duct injuries: anatomy, techniques and results. Clin. Imaging 42, 183–192 (2017).
Girotra, M., Horwhat, J. D., Settle, T. L. & Parasher, V. K. Endoscopic ultrasound-guided transesophageal thoracic duct puncture in a Swine model: a survival study. J. Laparoendosc. Adv. Surg. Tech. A 23, 588–591 (2013).
Parasher, V. K. et al. Lymph sampling and lymphangiography via EUS-guided transesophageal thoracic duct puncture in a swine model. Gastrointest. Endosc. 59, 564–567 (2004).
Choi, J.-H. et al. Revised Atlanta classification and determinant-based classification: Which one better at stratifying outcomes of patients with acute pancreatitis? Pancreatology 17, 194–200 (2017).
Zubia-Olaskoaga, F. et al. Comparison between revised Atlanta classification and determinant-based classification for acute pancreatitis in intensive care medicine. Why do not use a modified determinant-based classification? Crit. Care Med. 44, 910–917 (2016).
Talukdar, R., Clemens, M. & Vege, S. S. Moderately severe acute pancreatitis: prospective validation of this new subgroup of acute pancreatitis. Pancreas 41, 306–309 (2012).
Vege, S. S. et al. Low mortality and high morbidity in severe acute pancreatitis without organ failure: a case for revising the Atlanta classification to include ‘moderately severe acute pancreatitis’. Am. J. Gastroenterol. 104, 710–715 (2009).
Schepers, N. J. et al. Impact of characteristics of organ failure and infected necrosis on mortality in necrotising pancreatitis. Gut. https://doi.org/10.1136/gutjnl-2017-314657 (2018).
Petrov, M. S., Shanbhag, S., Chakraborty, M., Phillips, A. R. J. & Windsor, J. A. Organ failure and infection of pancreatic necrosis as determinants of mortality in patients with acute pancreatitis. Gastroenterology 139, 813–820 (2010).
Wu, B. U. et al. Blood urea nitrogen in the early assessment of acute pancreatitis: an international validation study. Arch. Intern. Med. 171, 669–676 (2011).
Brown, A., Orav, J. & Banks, P. A. Hemoconcentration is an early marker for organ failure and necrotizing pancreatitis. Pancreas 20, 367–372 (2000).
Koutroumpakis, E. et al. Admission hematocrit and rise in blood urea nitrogen at 24h outperform other laboratory markers in predicting persistent organ failure and pancreatic necrosis in acute pancreatitis: a post hoc analysis of three large prospective databases. Am. J. Gastroenterol. 110, 1707–1716 (2015).
Karpavicius, A., Dambrauskas, Z., Sileikis, A., Vitkus, D. & Strupas, K. Value of adipokines in predicting the severity of acute pancreatitis: comprehensive review. World J. Gastroenterol. 18, 6620–6627 (2012).
Deng, L. H. et al. Plasma cytokines can help to identify the development of severe acute pancreatitis on admission. Medicine 96, e7312 (2017).
Mentula, P. et al. Early prediction of organ failure by combined markers in patients with acute pancreatitis. Br. J. Surg. 92, 68–75 (2005).
Zhang, Y.-P. et al. Early prediction of persistent organ failure by serum angiopoietin-2 in patients with acute pancreatitis. Dig. Dis. Sci. 61, 3584–3591 (2016).
Di, M.-Y. et al. Prediction models of mortality in acute pancreatitis in adults: a systematic review. Ann. Intern. Med. 165, 482–490 (2016).
Mounzer, R. et al. Comparison of existing clinical scoring systems to predict persistent organ failure in patients with acute pancreatitis. Gastroenterology 142, 1476 (2012).
Forsmark, C. E. & Yadav, D. Predicting the prognosis of acute pancreatitis. Ann. Intern. Med. 165, 523–524 (2016).
Mofidi, R. et al. Association between early systemic inflammatory response, severity of multiorgan dysfunction and death in acute pancreatitis. Br. J. Surg. 93, 738–744 (2006).
Lankisch, P. G. et al. Hemoconcentration: an early marker of severe and/or necrotizing pancreatitis? A critical appraisal. Am. J. Gastroenterol. 96, 2081–2085 (2001).
Singh, V. K. et al. Early systemic inflammatory response syndrome is associated with severe acute pancreatitis. Clin. Gastroenterol. Hepatol. 7, 1247–1251 (2009).
Buxbaum, J. L. et al. Early aggressive hydration hastens clinical improvement in mild acute pancreatitis. Am. J. Gastroenterol. 112, 797–803 (2017).
Mao, E. Q. et al. Rapid hemodilution is associated with increased sepsis and mortality among patients with severe acute pancreatitis. Chin. Med. J. 123, 1639–1644 (2010).
Wall, I. et al. Decreased mortality in acute pancreatitis related to early aggressive hydration. Pancreas 40, 547–550 (2011).
Singh, V. K. et al. An international multicenter study of early intravenous fluid administration and outcome in acute pancreatitis. United European Gastroenterol. J. 5, 491–498 (2017).
Yamashita, T. et al. Large volume fluid resuscitation for severe acute pancreatitis is associated with reduced mortality: a multicenter retrospective study. J. Clin. Gastroenterol. 53, 385–391 (2018).
Haydock, M. D. et al. Fluid therapy in acute pancreatitis: anybody’s guess. Ann. Surg. 257, 182–188 (2013).
de-Madaria, E. et al. Fluid resuscitation with lactated Ringer’s solution versus normal saline in acute pancreatitis: a triple-blind, randomized, controlled trial. United European Gastroenterol. J. 6, 63–72 (2018).
van Brunschot, S. et al. Abdominal compartment syndrome in acute pancreatitis: a systematic review. Pancreas 43, 665–674 (2014).
Larino-Noia, J. et al. Early and/or immediately full caloric diet versus standard refeeding in mild acute pancreatitis: a randomized open-label trial. Pancreatology 14, 167–173 (2014).
Zhao, X. L. et al. Early oral refeeding based on hunger in moderate and severe acute pancreatitis: a prospective controlled, randomized clinical trial. Nutrition 31, 171–175 (2015).
Vaughn, V. M. et al. Early versus delayed feeding in patients with acute pancreatitis: a systematic review. Ann. Intern. Med. 166, 883–892 (2017).
Machicado, J. D. et al. Practice patterns and utilization of tube feedings in acute pancreatitis patients at a large US referral center. Pancreas 47, 1150–1155 (2018).
Eatock, F. C. et al. A randomized study of early nasogastric versus nasojejunal feeding in severe acute pancreatitis. Am. J. Gastroenterol. 100, 432–439 (2005).
Petrov, M. S., Correia, M. I. T. D. & Windsor, J. A. Nasogastric tube feeding in predicted severe acute pancreatitis. A systematic review of the literature to determine safety and tolerance. JOP 9, 440–448 (2008).
Bakker, O. J. et al. Early versus on-demand nasoenteric tube feeding in acute pancreatitis. N. Engl. J. Med. 371, 1983–1993 (2014).
Al-Omran, M., Albalawi, Z. H., Tashkandi, M. F. & Al-Ansary, L. A. Enteral versus parenteral nutrition for acute pancreatitis. Cochrane Database Syst. Rev. 1, CD002837 (2010).
Yao, H., He, C., Deng, L. & Liao, G. Enteral versus parenteral nutrition in critically ill patients with severe pancreatitis: a meta-analysis. Eur. J. Clin. Nutr. 72, 66–68 (2018).
Basurto Ona, X., Rigau Comas, D. & Urrutia, G. Opioids for acute pancreatitis pain. Cochrane Database Syst. Rev. 7, CD009179 (2013).
Barlass, U. et al. Morphine worsens the severity and prevents pancreatic regeneration in mouse models of acute pancreatitis. Gut 67, 600–602 (2018).
Jabaudon, M. et al. Thoracic epidural analgesia and mortality in acute pancreatitis: a multicenter propensity analysis. Crit. Care Med. 46, e198–e205 (2018).
Bachmann, K. A. et al. Effects of thoracic epidural anesthesia on survival and microcirculation in severe acute pancreatitis: a randomized experimental trial. Crit. Care 17, R281 (2013).
Richards, E. R., Kabir, S. I., McNaught, C.-E. & MacFie, J. Effect of thoracic epidural anaesthesia on splanchnic blood flow. Br. J. Surg. 100, 316–321 (2013).
Bulyez, S. et al. Epidural analgesia in critically ill patients with acute pancreatitis: the multicentre randomised controlled EPIPAN study protocol. BMJ Open 7, e015280 (2017).
da Costa, D. W. et al. Same-admission versus interval cholecystectomy for mild gallstone pancreatitis (PONCHO): a multicentre randomised controlled trial. Lancet 386, 1261–1268 (2015).
da Costa, D. W. et al. Cost-effectiveness of same-admission versus interval cholecystectomy after mild gallstone pancreatitis in the PONCHO trial. Br. J. Surg. 103, 1695–1703 (2016).
Young, S.-H. et al. Cholecystectomy reduces recurrent pancreatitis and improves survival after endoscopic sphincterotomy. J. Gastrointest. Surg. 21, 294–301 (2017).
Noel, R. et al. Index versus delayed cholecystectomy in mild gallstone pancreatitis: results of a randomized controlled trial. HPB 20, 932–938 (2018).
Nealon, W. H., Bawduniak, J. & Walser, E. M. Appropriate timing of cholecystectomy in patients who present with moderate to severe gallstone-associated acute pancreatitis with peripancreatic fluid collections. Ann. Surg. 239, 741–751 (2004).
van Dijk, S. M. et al. Acute pancreatitis: recent advances through randomised trials. Gut 66, 2024–2032 (2017).
Tang, E., Stain, S. C., Tang, G., Froes, E. & Berne, T. V. Timing of laparoscopic surgery in gallstone pancreatitis. Arch. Surg. 130, 496–500 (1995).
Nikkola, J., Laukkarinen, J., Huhtala, H. & Sand, J. The intensity of brief interventions in patients with acute alcoholic pancreatitis should be increased, especially in young patients with heavy alcohol consumption. Alcohol Alcohol. 52, 453–459 (2017).
Xiang, J.-X. et al. Impact of cigarette smoking on recurrence of hyperlipidemic acute pancreatitis. World J. Gastroenterol. 23, 8387–8394 (2017).
Nordback, I. et al. The recurrence of acute alcohol-associated pancreatitis can be reduced: a randomized controlled trial. Gastroenterology 136, 848–855 (2009).
Pedersen, S. B., Langsted, A. & Nordestgaard, B. G. Nonfasting mild-to-moderate hypertriglyceridemia and risk of acute pancreatitis. JAMA Intern. Med. 176, 1834–1842 (2016).
Munigala, S., Kanwal, F., Xian, H., Scherrer, J. F. & Agarwal, B. Increased risk of pancreatic adenocarcinoma after acute pancreatitis. Clin. Gastroenterol. Hepatol. 12, 1143–1150 (2014).
Schepers, N. J. et al. Early biliary decompression versus conservative treatment in acute biliary pancreatitis (APEC trial): study protocol for a randomized controlled trial. Trials 17, 5 (2016).
Bradley, E. L. 3rd & Dexter, N. D. Management of severe acute pancreatitis: a surgical odyssey. Ann. Surg. 251, 6–17 (2010).
Gosnell, F. E., O’Neill, B. B. & Harris, H. W. Necrotizing pancreatitis during pregnancy: a rare cause and review of the literature. J. Gastrointest. Surg. 5, 371–376 (2001).
Sun, J. et al. Conservative treatment and percutaneous catheter drainage improve outcome of necrotizing pancreatitis. Hepatogastroenterology 62, 195–199 (2015).
Mouli, V. P., Sreenivas, V. & Garg, P. K. Efficacy of conservative treatment, without necrosectomy, for infected pancreatic necrosis: a systematic review and meta-analysis. Gastroenterology 144, 333–340 (2013).
van Santvoort, H. C. et al. A conservative and minimally invasive approach to necrotizing pancreatitis improves outcome. Gastroenterology 141, 1254–1263 (2011).
Mier, J., Leon, E. L., Castillo, A., Robledo, F. & Blanco, R. Early versus late necrosectomy in severe necrotizing pancreatitis. Am. J. Surg. 173, 71–75 (1997).
Arvanitakis, M. et al. Endoscopic management of acute necrotizing pancreatitis: European Society of Gastrointestinal Endoscopy (ESGE) evidence-based multidisciplinary guidelines. Endoscopy 50, 524–546 (2018).
van Santvoort, H. C. et al. A step-up approach or open necrosectomy for necrotizing pancreatitis. N. Engl. J. Med. 362, 1491–1502 (2010).
Bakker, O. J. et al. Endoscopic transgastric versus surgical necrosectomy for infected necrotizing pancreatitis: a randomized trial. JAMA 307, 1053–1061 (2012).
van Brunschot, S. et al. Endoscopic or surgical step-up approach for infected necrotising pancreatitis: a multicentre randomised trial. Lancet 391, 51–58 (2018).
Kumar, N., Conwell, D. L. & Thompson, C. C. Direct endoscopic necrosectomy versus step-up approach for walled-off pancreatic necrosis: comparison of clinical outcome and health care utilization. Pancreas 43, 1334–1339 (2014).
Guo, J. et al. A multi-institutional consensus on how to perform endoscopic ultrasound-guided peri-pancreatic fluid collection drainage and endoscopic necrosectomy. Endosc. Ultrasound 6, 285–291 (2017).
Gurusamy, K. S., Pallari, E., Hawkins, N., Pereira, S. P. & Davidson, B. R. Management strategies for pancreatic pseudocysts. Cochrane Database Syst. Rev. 4, CD011392 (2016).
Hammad, T. et al. Efficacy and safety of lumen-apposing metal stents in management of pancreatic fluid collections: are they better than plastic stents? A systematic review and meta-analysis. Dig. Dis. Sci. 63, 289–301 (2018).
Siddiqui, A. A. et al. Fully covered self-expanding metal stents versus lumen-apposing fully covered self-expanding metal stent versus plastic stents for endoscopic drainage of pancreatic walled-off necrosis: clinical outcomes and success. Gastrointest. Endosc. 85, 758–765 (2017).
Sharaiha, R. Z. et al. Endoscopic therapy with lumen-apposing metal stents is safe and effective for patients with pancreatic walled-off necrosis. Clin. Gastroenterol. Hepatol. 14, 1797–1803 (2016).
Siddiqui, A. A. et al. EUS-guided drainage of peripancreatic fluid collections and necrosis by using a novel lumen-apposing stent: a large retrospective, multicenter U.S. experience (with videos). Gastrointest. Endosc. 83, 699–707 (2016).
Stecher, S. S. et al. Delayed severe bleeding complications after treatment of pancreatic fluid collections with lumen-apposing metal stents. Gut 66, 1871–1872 (2017).
Bang, J. Y., Hasan, M., Navaneethan, U., Hawes, R. & Varadarajulu, S. Lumen-apposing metal stents (LAMS) for pancreatic fluid collection (PFC) drainage: may not be business as usual. Gut 66, 2054–2056 (2017).
Brimhall, B. et al. Increased incidence of pseudoaneurysm bleeding with lumen-apposing metal stents compared to double-pigtail plastic stents in patients with peripancreatic fluid collections. Clin. Gastroenterol. Hepatol. 16, 1521–1528 (2018).
Larsen, M. & Kozarek, R. A. Management of disconnected pancreatic duct syndrome. Curr. Treat. Opt. Gastroenterol. 14, 348–359 (2016).
Rana, S. S. et al. Prevention of recurrence of fluid collections in walled off pancreatic necrosis and disconnected pancreatic duct syndrome: Comparative study of one versus two long term transmural stents. Pancreatology 16, 687–688 (2016).
Bang, J. Y. et al. Impact of disconnected pancreatic duct syndrome on the endoscopic management of pancreatic fluid collections. Ann. Surg. 267, 561–568 (2018).
Tellez-Avina, F. I. et al. Permanent indwelling transmural stents for endoscopic treatment of patients with disconnected pancreatic duct syndrome: long-term results. J. Clin. Gastroenterol. 52, 85–90 (2018).
Rana, S. S., Bhasin, D. K., Rao, C., Sharma, R. & Gupta, R. Consequences of long term indwelling transmural stents in patients with walled off pancreatic necrosis & disconnected pancreatic duct syndrome. Pancreatology 13, 486–490 (2013).
Ahmed, M., Aziz, M. U., Mansoor, M. A. & Anwar, S. Vascular complications in cases of acute pancreatitis — CT scan based study. J. Pak. Med. Assoc. 66, 977–989 (2016).
Harris, S., Nadkarni, N. A., Naina, H. V. & Vege, S. S. Splanchnic vein thrombosis in acute pancreatitis: a single-center experience. Pancreas 42, 1251–1254 (2013).
Gonzelez, H. J., Sahay, S. J., Samadi, B., Davidson, B. R. & Rahman, S. H. Splanchnic vein thrombosis in severe acute pancreatitis: a 2-year, single-institution experience. HPB 13, 860–864 (2011).
Easler, J. et al. Portosplenomesenteric venous thrombosis in patients with acute pancreatitis is associated with pancreatic necrosis and usually has a benign course. Clin. Gastroenterol. Hepatol. 12, 854–862 (2014).
Xu, W., Qi, X., Chen, J., Su, C. & Guo, X. Prevalence of splanchnic vein thrombosis in pancreatitis: a systematic review and meta-analysis of observational studies. Gastroenterol. Res. Pract. 2015, 245460 (2015).
Toque, L. et al. Predictive factors of splanchnic vein thrombosis in acute pancreatitis: a 6-year single-center experience. J. Dig. Dis. 16, 734–740 (2015).
Machicado, J. D. & Yadav, D. Epidemiology of recurrent acute and chronic pancreatitis: similarities and differences. Dig. Dis. Sci. 62, 1683–1691 (2017).
Cote, G. A. et al. Recurrent acute pancreatitis significantly reduces quality of life even in the absence of overt chronic pancreatitis. Am. J. Gastroenterol. 113, 906–912 (2018).
Sankaran, S. J. et al. Frequency of progression from acute to chronic pancreatitis and risk factors: a meta-analysis. Gastroenterology 149, 1490–1500 (2015).
Sliwinska-Mosson, M. et al. The effect of smoking on expression of IL-6 and antioxidants in pancreatic fluids and tissues in patients with chronic pancreatitis. Pancreatology 12, 295–304 (2012).
Kirkegard, J., Cronin-Fenton, D., Heide-Jorgensen, U. & Mortensen, F. V. Acute pancreatitis and pancreatic cancer risk: a nationwide matched-cohort study in Denmark. Gastroenterology 154, 1729–1736 (2018).
Shinzeki, M. et al. Serum immunosuppressive acidic protein levels in patients with severe acute pancreatitis. Pancreas 35, 327–333 (2007).
Chung, S.-D., Chen, K.-Y., Xirasagar, S., Tsai, M.-C. & Lin, H.-C. More than 9-times increased risk for pancreatic cancer among patients with acute pancreatitis in Chinese population. Pancreas 41, 142–146 (2012).
Rijkers, A. P. et al. Risk of pancreatic cancer after a primary episode of acute pancreatitis. Pancreas 46, 1018–1022 (2017).
Nikkola, J. et al. The long-term prospective follow-up of pancreatic function after the first episode of acute alcoholic pancreatitis: recurrence predisposes one to pancreatic dysfunction and pancreatogenic diabetes. J. Clin. Gastroenterol. 51, 183–190 (2017).
Das, S. L. M. et al. Relationship between the exocrine and endocrine pancreas after acute pancreatitis. World J. Gastroenterol. 20, 17196–17205 (2014).
Shimosegawa, T. et al. International consensus diagnostic criteria for autoimmune pancreatitis: guidelines of the International Association of Pancreatology. Pancreas 40, 352–358 (2011).
Badalov, N. et al. Drug-induced acute pancreatitis: an evidence-based review. Clin. Gastroenterol. Hepatol. 5, 648–661 (2007).
US National Library of Medicine. ClinicalTrials.gov https://clinicaltrials.gov/ct2/show/NCT03401190 (2019).
Bae, S.-C. & Lee, Y. H. Comparison of the efficacy and tolerability of tocilizumab, sarilumab, and sirukumab in patients with active rheumatoid arthritis: a Bayesian network meta-analysis of randomized controlled trials. Clin. Rheumatol. 37, 1471–1479 (2018).
Dellinger, E. P. et al. Determinant-based classification of acute pancreatitis severity: an international multidisciplinary consultation. Ann. Surg. 256, 875–880 (2012).
Author information
Authors and Affiliations
Contributions
P.J.L. researched data for the article. Both authors contributed equally to all other aspects of the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Glossary
- Mitochondrial permeability transition pores
-
Proteins located in the inner membrane of the mitochondrion, which when open can cause rapid mitochondrial depolarization and dysfunction.
- Calcium release-activated channels
-
Calcium ion channels that are activated when calcium stores are depleted from the endoplasmic reticulum.
- Local complications
-
A collective term to denote collections that form within and/or around pancreatic parenchyma as a result of acute pancreatitis.
- Unfolded protein response
-
(UPR). A collective term to denote a set of compensatory cellular responses to endoplasmic reticulum stress
- Autophagy
-
An orderly mechanism that processes, degrades and recycles various unwanted cellular components.
- ER stress
-
A state in which the demand of cellular machinery overwhelms the capacity of the endoplasmic reticulum (ER), leading to accumulation of misfolded proteins.
- Cholecystokinin
-
A hormone that causes gallbladder contraction and pancreatic enzyme secretion.
- Nuclear factor-κB
-
(NF-κB). A transcription factor that can cause production of pro-inflammatory cytokines and chemokines.
- Inositol 1,4,5-trisphosphate receptor
-
(Ins(1,4,5,)P3R). A glycoprotein complex located in the endoplasmic reticulum that can operate as a calcium channel.
- Zymogen granules
-
Vesicles that contain various pancreatic enzyme precursors.
- Cathepsin B
-
A lysosomal protease.
- Necroptosis
-
A regulated form of cell death.
- Receptor-interacting protein kinase
-
(RIP). A type of protein kinase that is implicated in regulation of cell death.
- Cystic fibrosis transmembrane regulator
-
(CFTR). A chloride channel located in pancreatic duct cells that enables passage of anions and water.
- Monocyte chemoattractant protein 1
-
(MCP1). A chemokine that is involved in facilitating migration and recruitment of monocytes.
- Damage-associated molecular patterns
-
(DAMPs). A variety of substances released by damaged cells that can activate an immune response.
- Systemic inflammatory response syndrome
-
(SIRS). A host immune response to an inflammatory or infectious insult that is often characterized by fevers, leukocytosis, tachycardia, tachypnea and hypotension.
- Cystenterostomy
-
The creation of a connection between a cyst wall and the wall of the gastrointestinal tract.
Rights and permissions
About this article
Cite this article
Lee, P.J., Papachristou, G.I. New insights into acute pancreatitis. Nat Rev Gastroenterol Hepatol 16, 479–496 (2019). https://doi.org/10.1038/s41575-019-0158-2
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41575-019-0158-2
This article is cited by
-
Network pharmacology and in vitro experimental verification unveil glycyrrhizin from glycyrrhiza glabra alleviates acute pancreatitis via modulation of MAPK and STAT3 signaling pathways
BMC Complementary Medicine and Therapies (2024)
-
The integration of single-cell and bulk RNA-seq atlas reveals ERS-mediated acinar cell damage in acute pancreatitis
Journal of Translational Medicine (2024)
-
Exploring the interplay of gut microbiota, inflammation, and LDL-cholesterol: a multiomics Mendelian randomization analysis of their causal relationship in acute pancreatitis and non-alcoholic fatty liver disease
Journal of Translational Medicine (2024)
-
Critical appraisal of machine learning prognostic models for acute pancreatitis: protocol for a systematic review
Diagnostic and Prognostic Research (2024)
-
Impact of stress hyperglycemia on long-term prognosis in acute pancreatitis without diabetes
Internal and Emergency Medicine (2024)