Abstract
Coeliac disease is an immune-mediated enteropathy against dietary gluten present in wheat, rye and barley and is one of the most common lifelong food-related disorders worldwide. Coeliac disease is also considered to be a systemic disorder characterized by a variable combination of gluten-related signs and symptoms and disease-specific antibodies in addition to enteropathy. The ingestion of gluten leads to the generation of harmful gluten peptides, which, in predisposed individuals, can induce adaptive and innate immune responses. The clinical presentation is extremely variable; patients may have severe gastrointestinal symptoms and malabsorption, extraintestinal symptoms or have no symptoms at all. Owing to the multifaceted clinical presentation, diagnosis remains a challenge and coeliac disease is heavily underdiagnosed. The diagnosis of coeliac disease is achieved by combining coeliac disease serology and small intestinal mucosal histology during a gluten-containing diet. Currently, the only effective treatment for coeliac disease is a lifelong strict gluten-free diet; however, the diet is restrictive and gluten is difficult to avoid. Optimizing diagnosis and care in coeliac disease requires continuous research and education of both patients and health-care professionals.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$29.99 / 30 days
cancel any time
Subscribe to this journal
Receive 1 digital issues and online access to articles
$99.00 per year
only $99.00 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout







Similar content being viewed by others
References
Abadie, V., Sollid, L. M., Barreiro, L. B. & Jabri, B. Integration of genetic and immunological insights into a model of celiac disease pathogenesis. Ann. Rev. Immunol. 29, 493–525 (2011).
Karell, K. et al. HLA types in celiac disease patients not carrying the DQA1*05-DQB1*02 (DQ2) heterodimer: results from the European Genetics Cluster on celiac disease. Hum. Immunol. 64, 469–477 (2003).
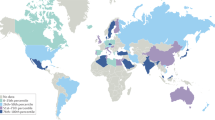
Singh, P. et al. Global prevalence of celiac disease: systematic review and meta-analysis. Clin. Gastroenterol. Hepatol. 16, 823–836 (2018). This paper presents a recent meta-analysis of the worldwide prevalence of coeliac disease.
Volta, U., Caio, G., Stanghellini, V. & De Giorgio, R. The changing clinical profile of celiac disease: a 15-year experience (1998–2012) in an Italian referral center. BMC Gastroenterol. 14, 194 (2014).
Kivelä, L. et al. Presentation of celiac disease in Finnish children is no longer changing: a 50-year perspective. J. Pediatr. 167, 1109–1115 (2015).
Fuchs, V. et al. Delayed celiac disease diagnosis predisposes to reduced quality of life and incremental use of health care services and medicines: a prospective nationwide study. United Eur. Gastroenterol. J. 6, 567–575 (2018).
Tio, M., Cox, M. R. & Eslick, G. D. Meta-analysis: coeliac disease and the risk of all-cause mortality, any malignancy and lymphoid malignancy. Aliment. Pharmacol. Ther. 35, 540–551 (2012).
Han, Y., Chen, W., Li, P. & Ye, J. Association between coeliac disease and risk of any malignancy and gastrointestinal malignancy: a meta-analysis. Medicine (Baltimore) 94, e1612 (2015).
Tuire, I. et al. Persistent duodenal intraepithelial lymphocytosis despite a long-term strict gluten-free diet in celiac disease. Am. J. Gastroenterol. 107, 1563–1569 (2012).
Vilppula, A. et al. Clinical benefit of gluten-free diet in screen-detected older celiac disease patients. BMC Gastroenterol. 11, 136 (2011).
Catassi, C. et al. Coeliac disease in the year 2000: exploring the iceberg. Lancet 343, 200–203 (1994).
Mäki, M. et al. Prevalence of celiac disease among children in Finland. N. Engl. J. Med. 348, 2517–2524 (2003). This article presents a milestone study applying coeliac-specific serology to uncover the true prevalence of coeliac disease in the general population.
McMillan, S. A. et al. Factors associated with serum antibodies to reticulin, endomysium, and gliadin in an adult population. Gut 39, 43–47 (1996).
Mustalahti, K. et al. The prevalence of celiac disease in Europe: results of a centralized, international mass screening project. Ann. Med. 42, 587–595 (2010).
West, J. et al. Seroprevalence, correlates, and characteristics of undetected coeliac disease in England. Gut 52, 960–965 (2003).
Korponay-Szabó, I. R. et al. Population screening for coeliac disease in primary care by district nurses using a rapid antibody test: diagnostic accuracy and feasibility study. BMJ 335, 1244–1247 (2007).
Rubio-Tapia, A., Ludvigsson, J. F., Brantner, T. L., Murray, J. A. & Everhart, J. E. The prevalence of celiac disease in the United States. Am. J. Gastroenterol. 107, 1538–1544 (2012).
Parra-Medina, R. et al. Prevalence of celiac disease in Latin America: a systematic review and meta-regression. PLOS ONE 10, e0124040 (2015).
Hovell, C. J. et al. High prevalence of coeliac disease in a population-based study from Western Australia: a case for screening? Med. J. Aust. 175, 247–250 (2001).
Ramakrishna, B. S. et al. Prevalence of adult celiac disease in India: regional variations and associations. Am. J. Gastroenterol. 111, 115–123 (2016).
Shamir, R. et al. The use of a single serological marker underestimates the prevalence of celiac disease in Israel: a study of blood donors. Am. J. Gastroenterol. 97, 2589–2594 (2002).
Yuan, J. et al. Prevalence of celiac disease autoimmunity among adolescents and young adults in China. Clin. Gastroenterol. Hepatol. 15, 1572–1579 (2017).
Makharia, G. K. et al. World Gastroenterology Organization-Asia Pacific Association of Gastroenterology Working Party on Celiac Disease. Issues associated with the emergence of coeliac disease in the Asia–Pacific region: a working party report of the World Gastroenterology Organization and the Asian Pacific Association of Gastroenterology. J. Gastroenterol. Hepatol. 29, 666–677 (2014).
Lohi, S. et al. Increasing prevalence of coeliac disease over time. Aliment. Pharmacol. Ther. 26, 1217–1225 (2007).
Catassi, C. et al. Natural history of celiac disease autoimmunity in a USA cohort followed since 1974. Ann. Med. 42, 530–538 (2010).
Rubio-Tapia, A. et al. Increased prevalence and mortality in undiagnosed celiac disease. Gastroenterology 137, 88–93 (2009). This comprehensive paper shows an increase in the true prevalence of coeliac disease over time and suggests increased mortality in individuals with unrecognized coeliac disease.
Ilus, T. et al. Refractory coeliac disease in a country with a high prevalence of clinically-diagnosed coeliac disease. Aliment. Pharmacol. Ther. 39, 418–425 (2014).
Vilppula, A. et al. Increasing prevalence and high incidence of celiac disease in elderly people: a population-based study. BMC Gastroenterol. 9, 49 (2009).
Kondrashova, A. et al. Lower economic status and inferior hygienic environment may protect against celiac disease. Ann. Med. 40, 223–231 (2008).
Kemppainen, K. et al. Factors that increase risk of celiac disease autoimmunity after a gastrointestinal infection in early life. Clin. Gastroenterol. Hepatol. 15, 694–702 (2017).
Andrén Aronsson, C. et al. Effects of gluten intake on risk of celiac disease: a case–control study on a Swedish birth cohort. Clin. Gastroenterol. Hepatol. 14, 403–409 (2016).
Mariné, M. et al. The prevalence of coeliac disease is significantly higher in children compared with adults. Aliment. Pharmacol. Ther. 33, 477–486 (2011).
Singh, P., Arora, S., Lal, S., Strand, T. A. & Makharia, G. K. Risk of celiac disease in the first- and second-degree relatives of patients with celiac disease: a systematic review and meta-analysis. Am. J. Gastroenterol. 110, 1539–1548 (2015).
Husby, S. et al. European Society for Pediatric Gastroenterology, Hepatology, and Nutrition guidelines for the diagnosis of coeliac disease. J. Pediatr. Gastroenterol. Nutr. 54, 136–160 (2012).
Shewry, P. R., Halford, N. G., Belton, P. S. & Tatham, A. S. The structure and properties of gluten: an elastic protein from wheat grain. Phil. Trans. R. Soc. 357, 133–142 (2002).
Kasarda, D. D. in Celiac Disease — Proceedings of the Seventh International Symposiumon Coeliac Disease (eds Mäki, M., Collin, P. & Visakorpi, J. K.) 195–212 (Coeliac Disease Study Group, 1996).
Shan, L. et al. Structural basis for gluten intolerance in celiac sprue. Science 297, 2275–2279 (2002). This excellent study demonstrates the proteolytic resistance of gliadin and is the first to suggest a new treatment modality based on proteolytic breakdown of gluten peptides.
Sollid, L. M. Coeliac disease: dissecting a complex inflammatory disorder. Nat. Rev. Immunol. 2, 647–655 (2002).
Caminero, A. et al. Duodenal bacteria from patients with celiac disease and healthy subjects distinctly affect gluten breakdown and immunogenicity. Gastroenterology 151, 670–683 (2016).
Pinto-Sánchez, M. I. et al. Safety of adding oats to a gluten-free diet for patients with celiac disease: systematic review and meta-analysis of clinical and observational studies. Gastroenterology 153, 395–409 (2017).
van Heel, D. A. et al. A genome-wide association study for celiac disease identifies risk variants in the region harboring IL2 and IL21. Nat. Genet. 39, 827–829 (2007).
Trynka, G. et al. Dense genotyping identifies and localizes multiple common and rare variant association signals in celiac disease. Nat. Genet. 43, 1193–1201 (2011).
Gutierrez-Achury, J. et al. Fine mapping in the MHC region accounts for 18% additional genetic risk for celiac disease. Nat. Genet. 47, 577–578 (2015).
Sollid, L. M. The roles of MHC class II genes and post-translational modification in celiac disease. Immunogenetics 69, 605–616 (2017).
Pietzak, M. M., Schofield, T. C., McGinniss, M. J. & Nakamura, R. M. Stratifying risk for celiac disease in a large at-risk United States population by using HLA alleles. Clin. Gastroenterol. Hepatol. 7, 966–971 (2009).
Hunt, K. A. et al. Newly identified genetic risk variants for celiac disease related to the immune response. Nat. Genet. 40, 395–402 (2008).
Dubois, P. C. et al. Multiple common variants for celiac disease influencing immune gene expression. Nat. Genet. 42, 295–302 (2010).
Lundin, K. E. et al. Gliadin-specific, HLA-DQ(alpha 1*0501, beta 1*0201) restricted T cells isolated from the small intestinal mucosa of celiac disease patients. J. Exp. Med. 178, 187–196 (1993).
van de Wal, Y. et al. Small intestinal T cells of celiac disease patients recognize a natural pepsin fragment of gliadin. Proc. Natl Acad. Sci. USA 95, 10050–10054 (1998).
Dieterich, W. et al. Identification of tissue transglutaminase as the autoantigen of celiac disease. Nat. Med. 3, 797–801 (1997). This landmark study identifies TG2 as the target of coeliac-disease-specific autoantibodies and is the first study to suggest that gliadin is a preferred substrate for this enzyme.
Molberg, O. et al. Tissue transglutaminase selectively modifies gliadin peptides that are recognized by gut-derived T cells in celiac disease. Nat. Med. 4, 713–717 (1998). This outstanding article shows that TG2-mediated deamidation of gliadin peptides creates epitopes that bind efficiently to coeliac-type HLA-DQ2, which are capable of inducing strong T cell activation, which is a hallmark of adaptive immune response in coeliac disease.
Tollefsen, S. et al. HLA-DQ2 and -DQ8 signatures of gluten T cell epitopes in celiac disease. J. Clin. Invest. 116, 2226–2236 (2006).
Rossjohn, J. & Koning, F. A biased view toward celiac disease. Mucosal Immunol. 9, 583–586 (2016).
Bodd, M. et al. HLA-DQ2-restricted gluten-reactive T cells produce IL-21 but not IL-17 or IL-22. Mucosal Immunol. 3, 594–601 (2010).
Stamnaes, J. & Sollid, L. M. Celiac disease: autoimmunity in response to food antigen. Semin. Immunol. 27, 343–352 (2015).
Korponay-Szabó, I. R. et al. In vivo targeting of intestinal and extraintestinal transglutaminase 2 by coeliac autoantibodies. Gut 53, 641–648 (2004).
Di Niro, R. et al. Responsive population dynamics and wide seeding into the duodenal lamina propria of transglutaminase-2-specific plasma cells in celiac disease. Mucosal Immunol. 9, 254–264 (2016).
Iversen, R. et al. Strong clonal relatedness between serum and gut IgA despite different plasma cell origins. Cell Rep. 20, 2357–2367 (2017).
Rauhavirta, T., Hietikko, M., Salmi, T. & Lindfors, K. Transglutaminase 2 and transglutaminase 2 autoantibodies in celiac disease: a review. Clin. Rev. Allergy Immunol. https://doi.org/10.1007/s12016-016-8557-4 (2016).
Sarra, M. et al. IL-15 positively regulates IL-21 production in celiac disease mucosa. Mucosal Immunol. 6, 244–255 (2013).
Malamut, G. et al. IL-15 triggers an antiapoptotic pathway in human intraepithelial lymphocytes that is a potential new target in celiac disease-associated inflammation and lymphomagenesis. J. Clin. Invest. 120, 2131–2143 (2010).
Salvati, V. M. et al. Interleukin 18 and associated markers of T helper cell type 1 activity in coeliac disease. Gut 50, 186–190 (2002).
Mention, J. J. et al. Interleukin 15: a key to disrupted intraepithelial lymphocyte homeostasis and lymphomagenesis in celiac disease. Gastroenterology 125, 730–745 (2003).
Kutlu, T. et al. Numbers of T cell receptor (TCR) alpha beta+ but not of TcR gamma delta+ intraepithelial lymphocytes correlate with the grade of villous atrophy in coeliac patients on a long term normal diet. Gut 34, 208–214 (1993).
Maiuri, L. et al. FAS engagement drives apoptosis of enterocytes of coeliac patients. Gut 48, 418–424 (2001).
Oberhuber, G. et al. Evidence that intestinal intraepithelial lymphocytes are activated cytotoxic T cells in celiac disease but not in giardiasis. Am. J. Pathol. 148, 1351–1357 (1996).
Meresse, B. et al. Coordinated induction by IL15 of a TCR-independent NKG2D signaling pathway converts CTL into lymphokine-activated killer cells in celiac disease. Immunity 21, 357–366 (2004).
Hüe, S. et al. A direct role for NKG2D/MICA interaction in villous atrophy during celiac disease. Immunity 21, 367–377 (2004).
Luciani, A. et al. Lysosomal accumulation of gliadin p31-43 peptide induces oxidative stress and tissue transglutaminase-mediated PPARgamma downregulation in intestinal epithelial cells and coeliac mucosa. Gut 59, 311–319 (2010).
Araya, R. E. et al. Mechanisms of innate immune activation by gluten peptide p31-43 in mice. Am. J. Physiol. Gastrointest. Liver Physiol. 311, G40–G49 (2016).
Riddle, M. S., Murray, J. A., Cash, B. D., Pimentel, M. & Porter, C. K. Pathogen-specific risk of celiac disease following bacterial causes of foodborne illness: a retrospective cohort study. Dig. Dis. Sci. 58, 3242–3245 (2013).
Setty, M. et al. Distinct and synergistic contributions of epithelial stress and adaptive immunity to functions of intraepithelial killer cells and active celiac disease. Gastroenterology 149, 681–691 (2015).
Bouziat, R. et al. Reovirus infection triggers inflammatory responses to dietary antigens and development of celiac disease. Science 356, 44–50 (2017).
Zevallos, V. F. et al. Nutritional wheat amylase-trypsin inhibitors promote intestinal inflammation via activation of myeloid cells. Gastroenterology 152, 1100–1113 (2017).
Forsberg, G. et al. Presence of bacteria and innate immunity of intestinal epithelium in childhood celiac disease. Am. J. Gastroenterol. 99, 894–904 (2004).
Ou, G. et al. Proximal small intestinal microbiota and identification of rod-shaped bacteria associated with childhood celiac disease. Am. J. Gastroenterol. 104, 3058–3067 (2009).
Wacklin, P. et al. Altered duodenal microbiota composition in celiac disease patients suffering from persistent symptoms on a long-term gluten-free diet. Am. J. Gastroenterol. 109, 1933–1941 (2014).
Sánchez, E., Donat, E., Ribes-Koninckx, C., Fernández-Murga, M. L. & Sanz, Y. Duodenal-mucosal bacteria associated with celiac disease in children. Appl. Environ. Microbiol. 79, 5472–5479 (2013).
D’Argenio, V. et al. Metagenomics reveals dysbiosis and a potentially pathogenic N. flavescens strain in duodenum of adult celiac patients. Am. J. Gastroenterol. 111, 879–890 (2016).
Verdu, E. & Caminero, A. How infection can incite sensitivity to food. Science 556, 29–30 (2017).
Lerner, A., Arleevskaya, M., Schmiedl, A. & Mathiass, T. Microbes and viruses are bugging the gut in celiac disease. Are they friends or foes? Front. Microbiol. 8, 1392 (2017).
Vriezinga, S. L. et al. Randomized feeding intervention in infants at high risk for celiac disease. N. Engl. J. Med. 371, 1304–1315 (2014). This multicentre, randomized, double-blind, placebo-controlled dietary intervention study in at-risk children addresses whether the early introduction of gluten is able to prevent the onset of coeliac disease.
Decker, E. et al. Cesarean delivery is associated with celiac disease but not inflammatory bowel disease in children. Pediatrics 125, e1433–e1440 (2010).
Koletzko, S. et al. Cesarean section on the risk of celiac disease in the offspring: the Teddy study. J. Pediatr. Gastroenterol. Nutr. 66, 417–424 (2018).
Mårild, K. et al. Antibiotic exposure and the development of coeliac disease: a nationwide case-control study. BMC Gastroenterol. 13, 109 (2013).
Kemppainen, K. et al. Association between early-life antibiotic use and the risk of islet or celiac disease autoimmunity. JAMA Pediatr. 171, 1217–1225 (2017).
Lebwohl, B., Spechler, S. J., Wang, T. C., Green, P. H. & Ludvigsson, J. F. Use of proton pump inhibitors and subsequent risk of celiac disease. Dig. Liver Dis. 46, 36–40 (2014).
Ivarsson, A. et al. Epidemic of coeliac disease in Swedish children. Acta Paediatr. 89, 165–171 (2000).
Szajewska, H. et al. Systematic review with meta-analysis: early infant feeding and coeliac disease — update 2015. Aliment. Pharmacol. Ther. 41, 1038–1054 (2015).
Lionetti, E. et al. Introduction of gluten, HLA status, and the risk of celiac disease in children. N. Engl. J. Med. 371, 1295–1303 (2014).
Crespo-Escobar, P. et al. The role of gluten consumption at an early age in celiac disease development: a further analysis of the prospective PreventCD cohort study. Am. J. Clin. Nutr. 105, 890–896 (2017).
Snook, J. A. et al. Adult coeliac disease and cigarette smoking. Gut 39, 60–62 (1996).
Steens, R. F. et al. A national prospective study on childhood celiac disease in the Netherlands 1993–2000: an increasing recognition and a changing clinical picture. J. Pediatr. 147, 239–243 (2005).
Collin, P., Salmi, T. T., Hervonen, K., Kaukinen, K. & Reunala, T. Dermatitis herpetiformis: a cutaneous manifestation of coeliac disease. Ann. Med. 49, 23–31 (2017).
Jericho, H., Sansotta, N. & Guandalini, S. Extraintestinal manifestations of celiac disease: effectiveness of the gluten-free diet. J. Pediatr. Gastroenterol. Nutr. 65, 75–79 (2017).
Rampertab, S. D., Pooran, N., Brar, P., Singh, P. & Green, P. H. Trends in the presentation of celiac disease. Am. J. Med. 119, 355 (2006).
Giersiepen, K. et al. Accuracy of diagnostic antibody tests for coeliac disease in children: summary of an evidence report. J. Pediatr. Gastroenterol. Nutr. 54, 229–241 (2012).
Lewis, N. R. & Scott, B. B. Systemic review: the use of serology to exclude or diagnose coeliac disease (a comparison of the endomysial and tissue transglutaminase antibody tests). Aliment. Pharmacol. Ther. 24, 47–54 (2006).
Chou, R. et al. Screening for celiac disease. Evidence report and systemic review for the US preventive services task force. JAMA 217, 1258–1268 (2017).
Ferrara, F. et al. Anti-transglutaminase antibodies in non-coeliac children suffering from infectious diseases. Clin. Exp. Immunol. 159, 217–223 (2010).
Lewis, N. R. & Scott, B. B. Meta-analysis: deamidated gliadin peptide antibody and tissue transglutaminase antibody compared as screening tests for coeliac disease. Aliment. Pharmacol. Ther. 31, 73–81 (2010).
Hoerter, N. A. et al. Diagnostic yield of isolated deamidated gliadin peptide antibody elevation for celiac disease. Dig. Dis. Sci. 62, 1272–1276 (2017).
Korponay-Szabó, I. R. et al. Elevation of IgG antibodies against tissue transglutaminase as a diagnostic tool for coeliac disease in selective IgA deficiency. Gut 52, 1567–1571 (2003).
Aziz, I. et al. The clinical and phenotypical assessment of seronegative villous atrophy; a prospective UK centre experience evaluating 200 adult cases over a 15-year period (2000–2015). Gut 66, 1563–1572 (2017).
Singh, P. et al. Diagnostic accuracy of point of care tests for diagnosing celiac disease: a systematic review and meta-analysis. J. Clin. Gastroenterol. https://doi.org/10.1097/MCG.0000000000001081 (2018).
Kurppa, K. et al. Diagnosing mild enteropathy celiac disease: a randomized, controlled clinical study. Gastroenterology 136, 816–823 (2009).
Zanini, B. et al. Celiac disease with mild enteropathy is not mild disease. Clin. Gastroenterol. Hepatol. 11, 253–258 (2013).
Taavela, J. et al. A prospective study on the usefulness of duodenal bulb biopsies in celiac disease diagnosis in children: urging caution. Am. J. Gastroenterol. 111, 124–133 (2016).
Taavela, J. et al. Validation of morphometric analyses of small-intestinal biopsy readouts in celiac disease. PLOS ONE 8, e76163 (2013).
Villanacci, V. et al. Histopathological evaluation of duodenal biopsy in the PreventCD project. An observational interobserver agreement study. APMIS 126, 208–214 (2018).
Kaukinen, K., Partanen, J., Mäki, M. & Collin, P. HLA-DQ typing in the diagnosis of celiac disease. Am. J. Gastroenterol. 97, 695–699 (2002).
Salmi, T. T., Collin, P., Reunala, T., Mäki, M. & Kaukinen, K. Diagnostic methods beyond conventional histology in coeliac disease diagnosis. Dig. Liver Dis. 42, 28–32 (2010).
Anderson, R. P., Degano, P., Godkin, A. J., Jewell, D. P. & Hill, A. V. In vivo antigen challenge in celiac disease identifies a single transglutaminase-modified peptide as the dominant A-gliadin T cell epitope. Nat. Med. 6, 337–342 (2000).
Raki, M. et al. Tetramer visualization of gut-homing gluten-specific T cells in the peripheral blood of celiac disease patients. Proc. Natl Acad. Sci. USA 104, 2831–2836 (2007).
Sarna, V. K. et al. HLA-DQ-gluten tetramer blood test accurately identifies patients with and without celiac disease in absence of gluten consumption. Gastroenterology 54, 886–896 (2018).
Biesiekierski, J. R. et al. Gluten causes gastrointestinal symptoms in subjects without celiac disease: a double-blind randomized placebo-controlled trial. Am. J. Gastroenterol. 106, 508–514 (2011).
Carroccio, A. et al. Non-celiac wheat sensitivity diagnosed by double-blind placebo-controlled challenge: exploring a new clinical entity. Am. J. Gastroenterol. 107, 1898–1906 (2012).
Carraccio, A. et al. Persistence of nonceliac wheat sensitivity, based on long-term follow-up. Gastroenterology 153, 56–58 (2017).
Uhde, M. et al. Intestinal cell damage and systemic immune activation in individuals reporting sensitivity to wheat in the absence of coeliac disease. Gut 65, 1930–1937 (2016).
Francavilla, R. et al. Randomized double-blind placebo-controlled crossover trial for the diagnosis of non-celiac gluten sensitivity in children. Am. J. Gastroenterol. 113, 421–430 (2018).
Sapone, A. et al. Spectrum of gluten-related disorders: consensus on new nomenclature and classification. BMC Med. 10, 13 (2012).
Skodje, G. I. et al. Fructan, rather than gluten, induces symptoms in patients with self-reported non-celiac gluten sensitivity. Gastroenterology 154, 529–539 (2018).
Biagi, F. & Corazza, G. R. Mortality in celiac disease. Nat. Rev. Gastroenterol. Hepatol. 7, 158–162 (2010).
Van Doorn, R. K. et al. CDDUX: a disease-specific health-related quality-of-life questionnaire for children with celiac disease. J. Pediatr. Gastroenterol. Nutr. 47, 147–152 (2008).
Nachman, F. et al. Quality of life in celiac disease patients: prospective analysis on the importance of clinical severity at diagnosis and the impact of treatment. Dig. Liver Dis. 41, 15–25 (2009).
Shamir, R., Hernell, O. & Leshno, M. Cost-effectiveness analysis of screening for celiac disease in the adult population. Med. Decis. Making 26, 282–293 (2006).
Mearin, M. L. The prevention of coeliac disease. Best Pract. Res. Clin. Gastroenterol. 29, 493–501 (2015).
Ivarsson, A. et al. Prevalence of childhood celiac disease and changes in infant feeding. Pediatrics 131, 687–694 (2013).
Stordal, K., White, R. A. & Eggesbo, M. Early feeding and risk of celiac disease in a prospective birth cohort. Pediatrics 132, 1202–1209 (2013).
Jansen, M. A. et al. Infant feeding and anti-tissue transglutaminase antibody concentrations in the Generation R Study. Am. J. Clin. Nutr. 100, 1095–1101 (2014).
Aronsson, C. A. et al. Age at gluten introduction and risk of celiac disease. Pediatrics 135, 239–245 (2015).
Silano, M., Agostoni, C., Sanz, Y. & Guandalini, S. Infant feeding and risk of developing celiac disease: a systematic review. BMJ Open 6, e009163 (2016).
Mårild, K. et al. Infections and risk of celiac disease in childhood: a prospective nationwide cohort study. Am. J. Gastroenterol. 110, 1475–1484 (2015).
Lionetti, E. et al. Mode of delivery and risk of celiac disease: risk of celiac disease and age at gluten introduction cohort study. J. Pediatr. 184, 81–86 (2017).
Downey, L., Houten, R., Murch, S. & Longson, D. Recognition, assessment, and management of coeliac disease: summary of updated NICE guidance. BMJ 351, h4513 (2015).
Catassi, C. et al. Detection of celiac disease in primary care: a multicentre case-finding study in North America. Am. J. Gastoenterol. 102, 1454–1460 (2007).
Virta, L. J., Kaukinen, K. & Collin, P. Incidence and prevalence of diagnosed coeliac disease in Finland: results of effective case finding in adults. Scand. J. Gastroenterol. 44, 933–938 (2009).
Alessandrini, S., Giacomoni, E. & Muccioli, F. Mass population screening for celiac disease in children: the experience in Republic of San Marino from 1993 to 2009. Ital. J. Pediatr. 39, 67 (2013).
Nordyke, K. et al. How do children experience participating in a coeliac disease screening? A qualitative study based on children’s written narratives. Scand. J. Public Health 38, 351–358 (2010).
Katz, K. D. et al. Screening for celiac disease in a North American population: sequential serology and gastrointestinal symptoms. Am. J. Gastroenterol. 106, 1333–1339 (2011).
Koppen van, E. J. et al. Long-term health and quality-of-life consequences of mass screening for childhood celiac disease: a 10-year follow-up study. Pediatrics 123, 582–588 (2009).
Kiefte-de Jong, J. C. et al. Levels of antibodies against tissue transglutaminase during pregnancy are associated with reduced fetal weight and birth weight. Gastroenterology 144, 726–735 (2013).
Kurppa, K. et al. Benefits of a gluten-free diet for asymptomatic patients with serologic markers of celiac disease. Gastroenterology 147, 610–617 (2014).
Mahadev, S., Gardner, R., Lewis, S. K., Lebwohl, B. & Green, P. H. Quality of life in screen-detected celiac disease patients in the United States. J. Clin. Gastroenterol. 50, 393–397 (2015).
Jansen, M. A. et al. Growth trajectories and bone mineral density in anti-tissue transglutaminase antibody-positive children: the Generation R Study. Clin. Gastroenterol. Hepatol. 13, 913–920 (2015).
US Preventive Services Task Force. Screening for celiac disease: US preventive services task force recommendation statement. JAMA 317, 1252–1257 (2017).
See, J. A., Kaukinen, K., Makharia, G. K., Gibson, P. R. & Murray, J. A. Practical insights into gluten-free diets. Nat. Rev. Gastroenterol. Hepatol. 12, 580–591 (2015).
Šuligoj, T., Gregorini, A., Colomba, M., Ellis, H. J. & Ciclitira, P. J. Evaluation of the safety of ancient strains of wheat in coeliac disease reveals heterogeneous small intestinal T cell responses suggestive of coeliac toxicity. Clin. Nutr. 32, 1043–1049 (2013).
Malalgoda, M., Meinhardt, S. W. & Simsek, S. Detection and quantitation of immunogenic epitopes related to celiac disease in historical and modern hard red spring wheat cultivars. Food Chem. 264, 101–107 (2018).
Wild, D., Robins, G. G., Burley, V. J. & Howdle, P. D. Evidence of high sugar intake, and low fibre and mineral intake, in the gluten-free diet. Aliment. Pharmacol. Ther. 32, 573–581 (2010).
Lebwohl, B. et al. Long term gluten consumption in adults without celiac disease and risk of coronary heart disease: prospective cohort study. BMJ 357, j1892 (2017).
Codex Alimentarius International Food Standards. Standard for foods for special dietary use for persons intolerant to gluten. Codex Stan 118–1979. Codex Alimentarius www.fao.org/input/download/standards/291/CXS_118e_2015.pdf (2008).
Collin, P., Thorell, L., Kaukinen, K. & Mäki, M. The safe threshold for gluten contamination in gluten-free products. Can trace amounts be accepted in the treatment of coeliac disease? Aliment. Pharmacol. Ther. 19, 1277–1283 (2004).
Méndez, E., Vela, C., Immer, U. & Janssen, F. W. Report of a collaborative trial to investigate the performance of the R5 enzyme linked immunoassay to determine gliadin in gluten-free food. Eur. J. Gastroenterol. Hepatol. 17, 1053–1063 (2005).
Akobeng, A. K. & Thomas, A. G. Systematic review: tolerable amount of gluten for people with coeliac disease. Aliment. Pharmacol. Ther. 27, 1044–1052 (2008).
Catassi, C. et al. A prospective, double-blind, placebo-controlled trial to establish a safe gluten threshold for patients with celiac disease. Am. J. Clin. Nutr. 85, 160–166 (2007).
van Overbeek, F. M. et al. The daily gluten intake in relatives of patients with coeliac disease compared with that of the general Dutch population. Eur. J. Gastroenterol. Hepatol. 9, 1097–1099 (1997).
Hall, N. J., Rubin, G. & Charnock, A. Systematic review: adherence to a gluten-free diet in adult patients with coeliac disease. Aliment. Pharmacol. Ther. 30, 315–330 (2009).
Villafuerte-Galvez, J. et al. Factors governing long-term adherence to a gluten-free diet in adult patients with coeliac disease. Aliment. Pharmacol. Ther. 42, 753–760 (2015).
Ukkola, A. et al. Patients’ experiences and perceptions of living with coeliac disease — implications for optimizing care. J. Gastrointestin. Liver Dis. 21, 17–22 (2012).
Halmos, E. P. et al. Food knowledge and psychological state predict adherence to a gluten-free diet in a survey of 5310 Australians and New Zealanders with coeliac disease. Aliment. Pharmacol. Ther. 48, 78–86 (2018).
Aziz, I. et al. Change in awareness of gluten-related disorders among chefs and the general public in the UK: a 10-year follow-up study. Eur. J. Gastroenterol. Hepatol. 26, 1228–1233 (2014).
Branchi, F. et al. Celiac disease and drug-based therapies: inquiry into patients demands. Digestion 93, 160–166 (2016).
Clemens, R. & van Klinken, B. J. The future of oats in the food and health continuum. Br. J. Nutr. 112, S75–S79 (2014).
Peräaho, M. et al. Oats can diversify a gluten-free diet in celiac disease and dermatitis herpetiformis. J. Am. Diet. Assoc. 104, 1148–1150 (2004).
Arentz-Hansen, H. et al. The molecular basis for oat intolerance in patients with celiac disease. PLOS Med. https://doi.org/10.1371/journal.pmed.0010001 (2004).
Peräaho, M. et al. Effect of an oats-containing gluten-free diet on symptoms and quality of life in coeliac disease. A randomized study. Scand. J. Gastroenterol. 39, 27–31 (2004).
Sjöberg, V. et al. Noncontaminated dietary oats may hamper normalization of the intestinal immune status in childhood celiac disease. Clin. Transl Gastroenterol. 5, e58 (2014).
Silano, M. et al. Avenins from different cultivars of oats elicit response by coeliac peripheral lymphocytes. Scand. J. Gastroenterol. 42, 1302–1305 (2007).
Comino, I. et al. Identification and molecular characterization of oat peptides implicated on coeliac immune response. Food Nutr. Res. 60, 30324 (2016).
Ludvigsson, J. F. et al. Diagnosis and management of adult coeliac disease: guidelines from the British Society of Gastroenterology. Gut 63, 1210–1228 (2014).
Herman, M. L. et al. Patients with celiac disease are not followed up adequately. Clin. Gastroenterol. Hepatol. 10, 893–899 (2012).
Haines, M. L., Anderson, R. P. & Gibson, P. R. Systematic review: the evidence base for long-term management of coeliac disease. Aliment. Pharmacol. Ther. 28, 1042–1066 (2008).
Bebb, J. R., Lawson, A., Knight, T. & Long, R. G. Long-term follow-up of coeliac disease — what do coeliac patients want? Aliment. Pharmacol. Ther. 23, 827–831 (2006).
Johansson, K., Malmberg Hård Af Segerstad, E., Mårtensson, H. & Agardh, D. Dietitian visits were a safe and cost-effective form of follow-up care for children with celiac disease. Acta Paediatr. https://doi.org/10.1111/apa.14411 (2018).
Pekki, H. et al. Performing routine follow-up biopsy 1 year after diagnosis does not affect long-term outcomes in coeliac disease. Aliment. Pharmacol. Ther. 45, 1459–1468 (2017).
Wessels, M. M. et al. Complementary serologic investigations in children with celiac disease is unnecessary during follow-up. J. Pediatr. 169, 55–60 (2016).
Newnham, E. D., Shepherd, S. J., Strauss, B. J., Hosking, P. & Gibson, P. R. Adherence to the gluten-free diet can achieve the therapeutic goals in almost all patients with coeliac disease: a 5-year longitudinal study from diagnosis. Gastroenterol. Hepatol. 31, 342–349 (2016).
Hære, P. et al. Long-term mucosal recovery and healing in celiac disease is the rule — not the exception. Scand. J. Gastroenterol. 51, 1439–1446 (2016).
Malamut, G. et al. Presentation and long-term follow-up of refractory celiac disease: comparison of type I with type II. Gastroenterology 136, 81–90 (2009).
Abdulkarim, A. S., Burgart, L. J., See, J. & Murray, J. A. Etiology of nonresponsive celiac disease: results of a systematic approach. Am. J. Gastroenterol. 97, 2016–2021 (2007).
van Wanrooij, R. L. et al. Outcome of referrals for non-responsive celiac disease in a tertiary center: low incidence of refractory celiac disease in the Netherlands. Clin. Transl Gastroenterol. 8, e218 (2017).
Rubio-Tapia, A. et al. Clinical staging and survival in refractory celiac disease: a single center experience. Gastroenterology 136, 99–107 (2009). This paper shows the poor prognosis of RCD.
Biagi, F. et al. PROgnosticating COeliac patieNts SUrvivaL: the PROCONSUL score. PLOS ONE 9, e84163 (2014).
Kaukinen, K. et al. Persistent small bowel mucosal villous atrophy without symptoms in coeliac disease. Aliment. Pharmacol. Ther. 25, 1237–1245 (2007).
Laurikka, P. et al. Gastrointestinal symptoms in celiac disease patients on a long-term gluten-free diet. Nutrients 8, E429 (2016).
Paarlahti, P. et al. Predictors of persistent symptoms and reduced quality of life in treated coeliac disease patients: a large cross-sectional study. BMC Gastroenterol. 13, 75 (2013).
Laurikka, P. et al. Dietary factors and mucosal immune response in celiac disease patients having persistent symptoms despite a gluten-free diet. J. Clin. Gastroenterol. https://doi.org/10.1097/MCG.0000000000001013 (2018).
Ilus, T., Kaukinen, K., Virta, L. J., Pukkala, E. & Collin, P. Incidence of malignancies in diagnosed celiac patients: a population-based estimate. Am. J. Gastroenterol. 109, 1471–1477 (2014).
Lebwohl, B. et al. Mucosal healing and risk for lymphoproliferative malignancy in celiac disease: a population-based cohort study. Ann. Intern. Med. 159, 169–175 (2013).
Ludvigsson, J. F., West, J., Ekbom, A. & Stephansson, O. Reduced risk of breast, endometrial and ovarian cancer in women with celiac disease. Int. J. Cancer. 131, E244–E250 (2012).
Di Sabatino, A. et al. Splenic hypofunction and the spectrum of autoimmune and malignant complications in celiac disease. Clin. Gastroenterol. Hepatol. 4, 179–186 (2006).
Ludvigsson, J. F., Montgomery, S. M., Ekbom, A., Brandt, L. & Granath, F. Small-intestinal histopathology and mortality risk in celiac disease. JAMA 302, 1171–1178 (2009). This large population-based study indicates increased mortality in clinically diagnosed coeliac disease with villous atrophy as well as in patients with mild enteropathy.
Abdul Sultan, A. et al. Causes of death in people with coeliac disease in England compared with the general population: a competing risk analysis. Gut 64, 1220–1226 (2015).
Jordan, N. E. et al. Development and validation of a celiac disease quality of life instrument for North American children. J. Pediatr. Gastroenterol. Nutr. 57, 477–486 (2013).
Häuser, W., Gold, J., Stallmach, A., Caspary, W. F. & Stein, J. Development and validation of the Celiac Disease Questionnaire (CDQ), a disease-specific health-related quality of life measure for adult patients with celiac disease. J. Clin. Gastroenterol. 41, 157–166 (2007).
Dorn, S. et al. The development and validation of a new coeliac disease quality of life survey (CD-QOL). Aliment. Pharmacol. Ther. 31, 666–675 (2010).
Ukkola, A. et al. Diet improves perception of health and well-being in symptomatic, but not asymptomatic, patients with celiac disease. Clin. Gastroenterol. Hepatol. 9, 118–123 (2011).
Midhagen, G. & Hallert, C. High rate of gastrointestinal symptoms in celiac patients living on a gluten-free diet: controlled study. Am. J. Gastroenterol. 98, 2023–2026 (2003). This article reports that patients with coeliac disease may have persistent symptoms despite adherence to a long-term strict gluten-free diet.
Roos, S., Kärner, A. & Hallert, C. Psychological well-being of adult coeliac patients treated for 10 years. Dig. Liver Dis. 38, 177–182 (2006).
Rothbaum, F., Wolfer, J. & Visintainer, M. Coping behavior and locus of control in children1. J. Personal. 47, 118–135 (1979).
Compas, B. E. et al. Coping with chronic illness in childhood and adolescence. Annu. Rev. Clin. Psychol. 8, 455–480 (2012).
Vriezinga, S. et al. E-Healthcare for celiac disease — a multicenter randomized controlled trial. J. Pediatr. 195, 154–160 (2018).
Zarkadas, M. et al. Living with coeliac disease and a gluten-free diet: a Canadian perspective. J. Hum. Nutr. Diet. 26, 10–23 (2013).
Sollid, L. M. & Jabri, B. Triggers and drivers of autoimmunity: lessons from coeliac disease. Nat. Rev. Immunol. 13, 294–302 (2013).
Marietta, E. et al. A new model for dermatitis herpetiformis that uses HLA-DQ8 transgenic NOD mice. J. Clin. Invest. 114, 1090–1097 (2004).
Bethune, M. T. et al. A non-human primate model for gluten sensitivity. PLOS ONE 3, e1614 (2008).
DePaolo, R. W. et al. Co-adjuvant effects of retinoic acid and IL-15 induce inflammatory immunity to dietary antigens. Nature 471, 220–224 (2011).
Werkstetter, K. J. et al. Accuracy in diagnosis of celiac disease without biopsies in clinical practice. Gastroenterology 153, 924–935 (2017). This prospective multicentre study shows that a non-invasive serology-based diagnostic approach is feasible in coeliac disease.
Moreno, M. L. et al. Detection of gluten immunogenic peptides in the urine of patients with coeliac disease reveals transgressions in the gluten-free diet and incomplete mucosal healing. Gut 66, 250–257 (2017).
Kelly, C. P. et al. Larazotide acetate in patients with coeliac disease undergoing a gluten challenge: a randomised placebo-controlled study. Aliment. Pharmacol. Ther. 37, 252–262 (2013).
Leffler, D. A. et al. Larazotide acetate for persistent symptoms of celiac disease despite a gluten-free diet: a randomized controlled trial. Gastroenterology 148, 1311–1319 (2015). This paper describes the performance of a new therapeutic compound affecting small intestine mucosal barrier function in the treatment of coeliac disease.
Lähdeaho, M.-L. et al. Glutenase ALV003 attenuates gluten-induced mucosal injury in patients with celiac disease. Gastroenterology 146, 1649–1658 (2014). This pioneering paper reports that unfavourable gluten-induced small intestinal mucosal damage can be attenuated with gluten-degrading proteolytic enzyme therapy.
Syage, J. A., Murray, J. A., Green, P. H. R. & Khosla, C. Latiglutenase improves symptoms in seropositive celiac disease patients while on a gluten-free diet. Dig. Dis. Sci. 62, 2428–2432 (2017).
Goel, G. et al. Epitope-specific immunotherapy targeting CD4-positive T cells in coeliac disease: two randomised, double-blind, placebo-controlled phase 1 studies. Lancet Gastroenterol. Hepatol. 2, 479–493 (2017).
Ludvigsson, J. F. et al. Outcome measures in coeliac disease trials: the Tampere recommendations. Gut 67, 1410–1424 (2018).
Adriaanse, M. P. M. et al. Progress towards non-invasive diagnosis and follow-up of celiac disease in children; a prospective multicentre study to the usefulness of plasma I-FABP. Sci. Rep. 7, 8671 (2017).
Choung, R. S., Murray, J. A., Marietta, E. V., Van Dyke, C. T. & Ross, A. B. Serum alkylresorcinols as biomarkers of dietary gluten exposure in coeliac disease. Aliment. Pharmacol. Ther. 45, 643–652 (2017).
Owen, D. R. & Owen, D. A. Celiac disease and other causes of duodenitis. Arch. Pathol. Lab. Med. 142, 35–43 (2018).
DeGaetani, M. et al. Villous atrophy and negative celiac serology: a diagnostic and therapeutic dilemma. Am. J. Gastroenterol. 108, 647–653 (2013).
Adelman, D. C. et al. Measuring change in small intestinal histology in patients with celiac disease. Am. J. Gastroenterol. 113, 339–347 (2018).
Acknowledgements
The authors thank for the Academy of Finland, the Sigrid Juselius Foundation and the Competitive State Research Financing of the Expert Area of Tampere University Hospital (K. Kaukinen, K.L. and K. Kurppa); the European Commission (FP6-FP7); Stichting Coeliakie Onderzoek Nederland; the European Society for Paediatric Gastroenterology, Hepatology and Nutrition (ESPGHAN; M.L.M.); the Indian government and non-government organizations (G.K.M.), the US NIH (J.A.M.); the Canadian Institutes of Health Research and Crohn’s Colitis Canada grants; the Nestle Research Center; and Biocodex (E.F.V.) for support and funding. J.A.M. also acknowledges philanthropic support from the Mayo Foundation.
Reviewer information
Nature Reviews Disease Primers thanks C. Catassi, T. Not and the other anonymous referee(s) for the peer review of this work.
Author information
Authors and Affiliations
Contributions
Introduction (K. Kaukinen and K.L.); Epidemiology (K. Kaukinen, K.L., G.K.M. and J.A.M.); Mechanisms/pathophysiology (K. Kaukinen, K.L. and E.F.V.); Diagnosis, screening and prevention (K. Kaukinen, K.L. and M.L.M.); Management (K. Kaukinen, K.L., K. Kurppa and K.E.A.L.); Quality of life (K. Kaukinen, K.L. and C.C.); Outlook (K. Kaukinen, K.L., C.C., K. Kurppa, K.E.A.L., G.K.M., M.L.M., J.A.M. and E.F.V.); Overview of the Primer (K. Kaukinen).
Corresponding author
Ethics declarations
Competing interests
None of the authors declares any financial competing interests. The authors have the following non-financial competing interests. K. Kaukinen, K.L. and K. Kurppa are members of the Scientific Advisory Board of the Finnish Coeliac Society. K. Kaukinen and K. Kurppa are members of the Finnish Coeliac Disease Current Care Guidelines committee. K. Kaukinen is a vice chairman of the Finnish Society of Internal Medicine. G.K.M. holds the post of Secretary General of the Indian Society of Gastroenterology, is a board member of the International Society for Studies on Coeliac Disease, is Co-Chair of the Research Committee of the World Gastroenterology Organization, serves as Coordinator of the Indian National Taskforce on Inflammatory Bowel Disease and is co-inventor of a device for faecal incontinence. J.A.M. is Section Editor for Mayo Clinic Proceedings. E.F.V. holds a Canada Research Chair and is an advisory board member of Innovate Pharmaceuticals, is President of the Society for the Study of Coeliac Disease, is Treasurer of the Canadian Association of Gastroenterology (CAG) and is an executive board member of CAG and the Canadian Digestive Health Foundation.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Lindfors, K., Ciacci, C., Kurppa, K. et al. Coeliac disease. Nat Rev Dis Primers 5, 3 (2019). https://doi.org/10.1038/s41572-018-0054-z
Published:
DOI: https://doi.org/10.1038/s41572-018-0054-z
This article is cited by
-
Immunomodulatory and Anti-Inflammatory Effects of Vitamin A and Tryptophan on Monocyte-Derived Dendritic Cells Stimulated with Gliadin in Celiac Disease Patients
Inflammation (2024)
-
Total serum IgA levels and HLA-DQB1*02:01 allelic status
Immunologic Research (2024)
-
Redefining serological diagnostics with immunoaffinity proteomics
Clinical Proteomics (2023)
-
Prevalence of vomiting and nausea and associated factors after chronic and acute gluten exposure in celiac disease
BMC Gastroenterology (2023)
-
Cerebellar presence of immune cells in patients with neuro-coeliac disease
Acta Neuropathologica Communications (2023)