Abstract
Vibrio is a genus of ubiquitous bacteria found in a wide variety of aquatic and marine habitats; of the >100 described Vibrio spp., ~12 cause infections in humans. Vibrio cholerae can cause cholera, a severe diarrhoeal disease that can be quickly fatal if untreated and is typically transmitted via contaminated water and person-to-person contact. Non-cholera Vibrio spp. (for example, Vibrio parahaemolyticus, Vibrio alginolyticus and Vibrio vulnificus) cause vibriosis — infections normally acquired through exposure to sea water or through consumption of raw or undercooked contaminated seafood. Non-cholera bacteria can lead to several clinical manifestations, most commonly mild, self-limiting gastroenteritis, with the exception of V. vulnificus, an opportunistic pathogen with a high mortality that causes wound infections that can rapidly lead to septicaemia. Treatment for Vibrio spp. infection largely depends on the causative pathogen: for example, rehydration therapy for V. cholerae infection and debridement of infected tissues for V. vulnificus-associated wound infections, with antibiotic therapy for severe cholera and systemic infections. Although cholera is preventable and effective oral cholera vaccines are available, outbreaks can be triggered by natural or man-made events that contaminate drinking water or compromise access to safe water and sanitation. The incidence of vibriosis is rising, perhaps owing in part to the spread of Vibrio spp. favoured by climate change and rising sea water temperature.
Similar content being viewed by others
Introduction
Vibrio spp. are a group of common, Gram-negative, rod-shaped bacteria that are natural constituents of freshwater, estuarine and marine environments1. Vibrio spp. share several biological and genomic features. Their genomes are divided between two chromosomes, which have been shaped by recombination and horizontal gene transfer (HGT; that is, the acquisition of genetic material by transfer from other organisms). Although these pathogens may be genomically diverse, they all originate from aquatic and marine environments: they prefer warm, brackish (slightly salty) water, and their abundance in the natural environment tends to mirror environmental temperatures. Numerous studies show that sea water is the ecological niche of many microorganisms. Indeed, many bacterial pathogens are frequently encountered in sea water, including Escherichia coli, Salmonella spp., Proteus spp., Pseudomonas aeruginosa, Aeromonas hydrophila and Staphylococcus aureus. These bacteria have been shown to cause an array of clinical manifestations, including otorhinolaryngological, ophthalmological, digestive and dermatological infections2. Vibrio spp. are responsible for the majority of human diseases attributed to the natural microbiota of aquatic environments and seafood3; the most common pathogenic species are Vibrio cholerae, Vibrio parahaemolyticus, Vibrio vulnificus and Vibrio alginolyticus. Cases of Vibrio spp. infections have a marked seasonal distribution, with most cases occurring during warmer months. Vibrio spp. infections are usually initiated from exposure to contaminated water or consumption of raw or undercooked contaminated seafood and cause a variety of symptoms in humans4 (Table 1).
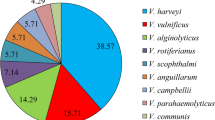
Human diseases caused by pathogenic bacteria of the Vibrio genus can be divided in two major groups: cholera and non-cholera infections. V. cholerae is the aetiological agent of cholera5, a severe diarrhoeal illness usually caused by ingestion of contaminated food or water, although person-to-person transmission is also possible. Of note, V. cholerae can also be found in fresh water. Non-cholera Vibrio spp., such as V. parahaemolyticus and V. vulnificus, cause vibriosis, a group of infections with different clinical manifestations depending on the pathogen species, route of infection and host susceptibility. For example, ingestion of non-cholera bacteria can cause mild gastroenteritis or primary septicaemia (that is, septicaemia following ingestion of raw or undercooked contaminated food), whereas exposure of skin wounds to contaminated water can cause wound infection that can result in secondary septicaemia. Non-cholera Vibrio spp. occupy habitats of moderate or high salinity and can be found in sea water and seafood. These bacteria are the most important environmental human pathogens that originate from aquatic and marine habitats (Fig. 1).
Pathogenic Vibrio spp. share several biological, clinical and environmental characteristics that set them apart as important human pathogens. a | These bacteria share interesting genomic structures, including two chromosomes, which are frequently shaped by recombination and intense horizontal gene transfer events. b | All Vibrio spp. grow in warm (typically ≥15 C°) sea water and brackish water, and Vibrio cholerae can also be found in fresh water. Vibrio spp. can persist in a free living state, colonize fish and marine invertebrates or be associated with plankton, algae and abiotic detritus74. Vibrio spp. can also form biofilms on biotic and abiotic surfaces, an ability that has an essential role in their environmental persistence215. c | However, Vibrio spp. differ in the routes of transmission to humans; non-cholera Vibrio spp., such as Vibrio parahaemolyticus, Vibrio vulnificus and Vibrio alginolyticus, represent an important and growing source of infections through contaminated seafood and direct exposure to water. d | The causative agent of cholera — V. cholerae — is the only Vibrio sp. that has both human and environmental stages in its life cycle74. V. cholerae can be found in fresh water as free living, in clusters of many cells forming biofilms or in association with plankton (a widely recognized environmental reservoir). From contaminated water, V. cholerae can be transmitted directly to the human population216,217. In contrast with other pathogenic non-cholera Vibrio spp., V. cholerae is also transmitted person to person and through the faecal–oral route.
The exact number of Vibrio spp. infections worldwide is uncertain because of limitations in existing surveillance systems, under-reporting or failure to report infections, differences in reporting procedures and the lack of international systems of epidemiology. V. cholerae has played a substantial part in shaping human history. Although cholera is rare in the developed world, it continues to represent a major cause of morbidity and mortality worldwide, especially in developing countries in Asia, Africa and Latin America, where V. cholerae is endemic, population density is high, sanitation is poor and access to safe drinking water is scarce. By contrast, vibriosis outbreaks are becoming increasingly frequent in developed countries, owing in part to a raised ocean temperature that favours the spread of non-cholera Vibrio spp.6. In countries that gather epidemiological data on these pathogens, such as the United States, large numbers of both waterborne7 and foodborne8,9 vibriosis predominate.
This Primer provides an overview of the ecology, epidemiology and public health relevance of Vibrio spp. as well as the mechanisms of disease and provides an outline of the diagnosis, treatment and outlook associated with Vibrio spp. infections. We focus on V. cholerae, V. parahaemolyticus and V. vulnificus as these are the most studied pathogens of greatest epidemiological importance; we highlight recent research work that has redefined our understanding of these pathogens, outline current knowledge gaps and speculate on future research work in this important set of pathogens.
Epidemiology
Vibrio spp. represent a diverse group of human pathogens, and the epidemiology associated with these bacteria is similarly complex. Although national and international agencies such as the Centers for Disease Control and Prevention (CDC) and the WHO gather global epidemiological data on these pathogens, currently no global systematic surveillance framework exists, and few individual countries have dedicated surveillance systems for Vibrio spp. One exception is in the United States, where epidemiological data have been gathered systematically since 1988 through the Cholera and Other Vibrio Information Service (COVIS) CDC programme7. Vibriosis has been notifiable in all 50 states of the United States since 2007. This type of national surveillance system is extremely useful because it provides key insights into routes of exposure, changes in incidence and geographical and epidemiological characteristics associated with Vibrio spp. infections. A 2012 estimate suggests a substantial increase in foodborne-associated Vibrio spp. infections in the United States7. The annual incidence of reported vibriosis increased over threefold from 0.09 cases per 100,000 population in 1996 to 0.29 cases per 100,000 population in 2010 (ref.7).
Vibrio cholerae
An estimated 3–5 million people contract cholera worldwide annually10,11, with ~100,000 deaths12 (Box 1); in endemic countries, about half of the deaths occur in children of <5 years of age13. Cholera has its highest incidence in children of <5 years of age; about half of all cholera cases occur in this age group, although the incidence varies annually14, presumably related to climate and hitherto unknown factors. For centuries, cholera has been endemic in Asia, mainly in the Ganges delta of the Bay of Bengal15, Bangladesh and India16. Asiatic cholera has exploded at several different times, spread rapidly and resulted in waves of global pandemics (Fig. 2). The spread of cholera outside of Asia is largely mediated by human activities17,18. Cholera was likely introduced through infected humans to Africa, Haiti and Latin America, and probably also historically to Europe and the United States19,20. The seventh pandemic continues to be a major public health threat for 175 countries in Asia, Africa and the Americas. Cholera has long been established as a climate-driven disease21,22, and in major endemic settings of Asia, it shows seasonal peak patterns at defined times of the year23.
A key aspect of Vibrio cholerae and Vibrio parahaemolyticus (which sets them apart in the Vibrio spp.) is their ability for pandemic expansion. V. cholerae and V. parahaemolyticus have very similar genomic structures. Although much is known regarding the mechanism of virulence associated with these bacteria, it is not clearly understood why particular strains can gain a foothold in a particular region and cause outbreaks. Certainly, particular strains such as V. cholerae El Tor and V. parahaemolyticus O3:K6 seem to have evolved a competitive advantage, which could explain why they can initiate and maintain substantial outbreaks, leading to pandemic expansion. The current seventh pandemic expansion of V. cholerae (El Tor biotype) started from the Bay of Bengal in the 1960s and spread in at least three independent but overlapping waves. The date ranges on the transcontinental transmission events of the different waves indicate the introduction of the pathogen in the different geographical areas, as inferred by phylogenetic analysis. The cross-continental spread of the first pandemic V. parahaemolyticus serotype, O3:K6, started from the original place of emergence in Southeast Asia in the 1990s, whereas the dispersal of the Pacific Northwest clonal type ST36 is a more-recent phenomenon. The spread of the O3:K6 serotype was restricted to Asia until 1997, when O3:K6 isolates were detected in Peru in June 1997218 and subsequently in Chile at the end of the same year199, initiating the pandemic expansion. From the emergence of infections along the coasts of South America in 1997, this pandemic serogroup disseminated globally, with outbreaks and infections detected in the United States in 1998180, Russia in 199747, France and Spain in 2004 (refs219,220), Mozambique in 2004 (ref.221) and Italy in 2007 (ref.222). Adapted from ref.191, Macmillan Publishers Limited; Data for V. parahaemolyticus from ref.40.
The infection pattern is not well defined for many affected regions, although major factors associated with cholera outbreaks worldwide include sea surface temperature24,25, sea surface height24 (that is, alterations in average sea surface topology), the temperature of fresh water26, plankton blooms27,28, precipitation29 and flooding30. The epidemiological patterns of cholera suggest a strong estuarine link for the disease, as outbreaks tend to start in the coastal regions before cases occur in inland areas31,32. Epidemiological studies have shown that V. cholerae is transmitted mainly in a faecal–oral mode via contaminated drinking water, although the bacterium can also transmit through person-to-person close contact33,34 and through food35. V. cholerae has >200 serogroups that are distinguished on the basis of the chemical composition of the O-antigen of lipopolysaccharide (LPS). O-Antigens are immunodominant and can be used for serological classification of V. cholerae on the basis of the characteristics of the sera generated by immunization with different serogroups. The vast majority of cholera cases are caused by serogroup O1. The O1 serogroup is divided into two main serotypes: Ogawa and Inaba. The serogroup O1 is also divided into biological variants known as biotypes — classical and El Tor — and both of these biotypes can be either Ogawa or Inaba serotypes. The classical and El Tor biotypes differ in a variety of phenotypic traits; the classical biotype was responsible for the first six cholera pandemics (which are considered concluded), whereas the ongoing seventh pandemic is caused by the El Tor biotype, which in 1961 replaced the classical biotype16 (Fig. 2). El Tor was replaced temporarily in 1992 by a non-O1 serogroup strain, which initiated a massive outbreak of cholera-like disease in the coastal villages of India31 and Bangladesh36,37. The rapid spread of this non-O1 serogroup strain, designated O139 Bengal, in most of Asia was thought to herald the beginning of the eighth pandemic, but this organism did not spread out of Asia and accordingly was not classified as a pandemic38. The O139 Bengal strain-associated cholera waned by 1996 but with an upsurge in 2002 (ref.39) and again in 2005 (ref.36); since then, the proposed eighth pandemic pathogen O139 Bengal is not associated with any major outbreak and is only sporadically found. The El Tor biotype continues as the major causative agent of cholera worldwide36.
Non-O1 and non-O139 V. cholerae strains are the causative agents of sporadic, yet severe, gastrointestinal and extraintestinal infections40, and compared with V. cholerae O1 and O139 they are relatively understudied human pathogens. During the Northern Hemisphere summer of 2014, there was a noticeable spike in reported non–O1 and non–O139 V. cholerae infections in the Baltic Sea area, corresponding both temporally and spatially with a substantial heatwave event1,41. Most cases involved self-limiting ear and soft tissue infections associated with swimming or water exposure.
Vibrio parahaemolyticus
V. parahaemolyticus is a ubiquitous inhabitant of temperate and tropical coastal areas around the world. The epidemiology of V. parahaemolyticus is characterized by sporadic cases of infection along coastal areas, mostly associated with the consumption of raw or undercooked contaminated seafood over the warmer months1, although wound exposure to contaminated water can also cause infection. V. parahaemolyticus does not spread via person-to-person transmission or the faecal–oral route42. Until the late 1960s, cases of V. parahaemolyticus infections were geographically restricted to Japan, but starting in 1969 V. parahaemolyticus infections were reported in geographically diverse locations, including the Atlantic, Pacific and Gulf States and Hawaii in the United States43, where according to 2011 estimates there are ~30,000 infections each year8. The first well-documented outbreak of V. parahaemolyticus in the United States was detected in Maryland in 1971, associated with crab ingestion44. Strains isolated from patients and from the suspected foods in the United States showed different serotypes from those isolated in Japan45. A comprehensive analysis of the sources of outbreaks in the United States led to the conclusion that the ingestion of raw or improperly cooked contaminated food was the most probable source of the V. parahaemolyticus infections, although cross contamination of cooked food (for example, with contaminated water) might have been a secondary vehicle43. Following the detection of V. parahaemolyticus in clinical cases in the United States, reported infections caused by this organism rapidly increased throughout the 1970s, with sporadic cases and outbreaks reported in Europe, Africa, New Zealand and most of the Asian countries46, thereby turning V. parahaemolyticus into a major seafood-borne pathogen and a global public health concern. Infections were associated with heterogeneous groups of diverse strains, although some groups prevailed in each geographical area. The epidemiology of V. parahaemolyticus experienced a radical change in 1996, when a sudden increment of gastroenteritis cases was detected in Calcutta, India. In contrast to most of the previous outbreaks, all the isolates from these cases clustered in a single homogeneous group, a variant of the serotype O3:K6 containing the same virulence traits: the thermostable direct haemolysin (Tdh), encoded by tdh, but not the Tdh-related haemolysin (Trh), encoded by trh 47. Using molecular typing techniques, these isolates were clearly differentiated from other O3:K6 strains recovered prior to the epidemic onset in Calcutta48. The emergence of this new O3:K6 strain began a prolific expansion of V. parahaemolyticus illnesses throughout most Southeast Asian countries in only 1 year47,48. This strain has continued its pandemic expansion over recent years: infections associated with this strain have been detected in almost all continents, and the O3:K6 strain has become endemic in many areas where it was introduced (Fig. 2). Although there are no definitive data, possible factors contributing to V. parahaemolyticus spread include ballast water discharge and shellfish transport. Climate warming, such as spells of anomalously warm weather, can have a role in initiating outbreaks49.
V. parahaemolyticus was the leading cause of bacterial infectious diarrhoea in the southern China region during 2007–2012, with serotype O3:K6 strains being the most prevalent isolates50. The pandemic strain (that is, the Calcutta O3:K6 strain) was the first example of cross-continental spreading of this pathogen until 2012, when strains belonging to the highly pathogenic ST36 (multilocus sequence type 36) clonal type were detected outside of their normal endemic region in the US Pacific Northwest, causing infections along the northeast coast of the United States and northwest Spain51,52 (Fig. 2). The ST36 clonal type is of some concern because of its increased virulence potential compared with other pathogenic V. parahaemolyticus strains49,53; this increased virulence could mean that smaller bacterial loads of this strain can be sufficient to cause infection, although the precise molecular mechanisms underlying the increased virulence remain to be elucidated. V. parahaemolyticus infections are estimated to cause a substantial percentage of the total cases of foodborne infections in the United States9, where foodborne Vibrio spp. infections have been increasing7 (Fig. 3). The WHO–Food and Agricultural Organization (FAO) risk assessments regarding this pathogen in shellfish were published in 2011 and form the basis of international control measures frequently adopted to reduce risk from seafood54.
Relative rates (compared with 2006–2008 rates) of culture-confirmed foodborne infections caused by different pathogens. Of all the major foodborne pathogens monitored in the United States, non-cholera Vibrio spp. represent the only group showing a clear increase in incidence. Although the absolute number of cases of vibriosis is low (for example, 216 in 2014, compared with ≥7,400 of salmonella and ≥400 of Shiga-toxin producing Escherichia coli (STEC) O157 infection), under-reporting of these infections is substantial, owing to misdiagnosis and lack of systematic screening, among other factors. For example, the number of Vibrio parahaemolyticus infections is estimated to be ~140-fold higher — thus, for each laboratory-confirmed infection, a hundred more are estimated to elude identification8. Adapted with permission from ref.223, Centers for Disease Control and Prevention.
Vibrio vulnificus
This pathogen is common in estuarine waters and has been isolated from a range of different environmental sources, including sea water, sediment and seafood produce42,55. Unlike V. cholerae and V. parahaemolyticus, V. vulnificus is an opportunistic pathogen, with virtually all cases occurring in those with an underlying disease. The most common risk factors are liver diseases (such as cirrhosis or hepatitis), diabetes mellitus and malignancies. Previous studies have indicated that individuals with chronic liver disease such as cirrhosis are up to 80–fold more likely than healthy individuals to develop V. vulnificus-associated primary septicaemia56. V. vulnificus infection is typically most prevalent in individuals of 45–60 years of age and in men, who make up 85–90% of patients; 85.6% of V. vulnificus cases reported to the US FDA between 1992 and 2007 were in men55. This age and sex specificity is probably explained by the fact that susceptible patients with cirrhosis are predominantly of middle age57 and men make up the bulk of persons with cirrhosis57. Similar to V. parahaemolyticus, infections associated with V. vulnificus originate from two distinct sources: consumption of contaminated seafood, in particular molluscan shellfish, resulting in gastroenteritis or primary septicaemia, which is often associated with consumption of oysters, where this bacterium can occur in large numbers (≥105 per gram); or exposure of wounds to sea water or seafood products, resulting in wound infections and secondary septicaemia. However, unlike V. parahaemolyticus, V. vulnificus is a highly fatal human pathogen: it is responsible for >95% of seafood-related deaths in the United States55 and has the highest case fatality rate (~50%) of any foodborne pathogen58. Wound infections associated with V. vulnificus are usually contracted during recreational activities such as swimming, fishing and handling seafood2 and have a substantial mortality (~25%)2,55. Three biotypes (a classification approach based on biochemical characteristics) of V. vulnificus have been identified55 Biotype 1 is responsible for both the majority of ingestion cases (primary septicaemias) and most wound infections. Biotype 2 is the causative agent of a rapidly fatal septicaemia in farmed eels and rarely in humans59. Biotype 3 causes human wound infections that, to date, have mostly been reported among tilapia aquaculture workers in Israel60, although an infection was recently reported in Japan61.
Globally, surveillance data regarding V. vulnificus infections are not gathered systematically, making wider geographical and epidemiological comparisons problematical. Where only fragmentary surveillance data exist (for example, published peer reviewed reports of infections), such as studies in Europe42,62, China63, Taiwan64, South America65, Japan66 and Korea67, infections tend to affect middle-aged men with underlying disease. V. vulnificus is a rare cause of infection (~100 cases per year in the United States), but published studies demonstrate an increase in disease in the United States and potentially also in Europe7,62,68. Incidence of infection is related to environmental distribution, and V. vulnificus exhibits quite distinct temperature and salinity tolerances, as it can be found in warm (13–30 °C) and brackish (2–25 parts per thousand NaCl) waters. The WHO risk assessment on V. vulnificus was published in 2004 (ref.69). Other Vibrio spp. that can infect humans are described in Box 2.
Mechanisms/pathophysiology
Vibrio cholerae
Of all the studied pathogenic Vibrio spp., V. cholerae is the most well understood. V. cholerae is the paradigmatic non-invasive mucosal pathogen: following ingestion of contaminated water or food by the host, the pathogen proliferates to high density along the mucosal surface of the small intestine but does not disrupt the integrity of the epithelial barrier or cause substantial damage to epithelial cells70 (Fig. 4). Instead, the bacteria prompt an intense secretory response, resulting in profuse watery diarrhoea that, if untreated, frequently results in death due to dehydration within 1–2 days. Studies in a variety of animal models and in human volunteers have demonstrated that choleric diarrhoea is primarily a response to a pathogen-secreted factor, cholera toxin (CT)71. Deletion of ctxA and ctxB (encoding cholera enterotoxin subunit A and B, respectively) from pathogenic V. cholerae abrogates the bacterial capacity to induce diarrhoea in animal models, and administration of purified CT is sufficient to induce diarrhoea in human volunteers72.
Once in the human host, after reaching the small intestine, Vibrio cholerae begins expressing genes encoding virulence factors, such as toxin-co-regulated pilus (Tcp) and cholera toxin. Cholera toxin is composed of two subunits, CtxA and CtxB, and binds to the ganglioside (a sialylated glycosphingolipid) GM1 on the plasma membrane of enterocytes via the pentameric CtxB subunit. Bound cholera toxin is endocytosed, then undergoes retrograde transport to the endoplasmic reticulum (ER), where the subunits dissociate. Release of the enzymatic CtxA subunit from the ER into the cytosol enables its allosteric activation by ADP ribosylation factor 6 (ARF6). The ARF6-bound, activated CtxA subunit in turn activates adenylyl cyclase by catalysing ADP ribosylation of a G protein-coupled receptor. Increased cellular levels of cAMP lead to protein kinase A (PKA)-dependent phosphorylation (P) of the cystic fibrosis transmembrane receptor (CFTR), which induces the efflux of ions and water into the lumen of the small intestine that causes diarrhoea.
Additional bacterial factors that contribute to cholera pathogenesis have also been identified through studies in animal models of disease, and some of these have been confirmed in studies in human volunteers73. Several studies demonstrate that clinically apparent V. cholerae infection induces protective immunity against subsequent infection in humans74. A key virulence factor in infant mice is the toxin-co-regulated pilus (Tcp), a type IV pilus (a filamentous surface appendage). Tcp produced by adjacent V. cholerae bacteria can bind to each other, tethering bacteria together and facilitating microcolony formation within the intestines of infected animals, and can also facilitate adhesion to enterocytes75. Human volunteer studies have demonstrated that Tcp is also essential for V. cholerae colonization of the human intestine76, suggesting that findings from infant mouse model hosts are relevant for understanding V. cholerae colonization of the human intestine. In addition to Tcp, many other cell structures and processes, including the LPS O-antigen, cell curvature77, motility and metabolic processes, have been implicated in V. cholerae intestinal colonization73.
Regulation of gene expression
Once the bacteria reach the host intestine, a complex network of regulatory inputs governs expression of V. cholerae virulence factors, many of which are not typically expressed in vitro. Transposon insertion sequencing (a high-throughput technique that combines transposon insertional mutagenesis with next-generation sequencing to identify the genes involved in a specific function) has aided in comprehensive, genome-wide identification of genes that facilitate intestinal colonization78. Environmental factors present in the intestine, including bile, bicarbonate, reduced oxygen tension and unsaturated fatty acids, contribute to the co-expression of genes for the biogenesis of Tcp and CT and other genes associated with colonization79. Transduction of these environmental stimuli is mediated by membrane-localized transcription factors, including CT transcriptional activator (encoded by toxR) and Tcp biosynthesis protein P and H (encoded by tcpP and tcpH, respectively), which induce expression of Tcp virulence regulatory protein (encoded by toxT, also known as tcpN), an activator of virulence gene expression79. Expression of the toxT regulon (a group of genes controlled by a common regulator) is also modulated by metabolic signals and quorum sensing. In contrast to several other pathogens, the expression of V. cholerae virulence genes is typically repressed at high cell densities80. In vivo gene expression studies have suggested that there is a temporal pattern of V. cholerae gene expression within the intestine. Genes expressed early in infection enable colonization, whereas genes expressed late in infection are thought to prepare the pathogen for growth in the environment outside of the host intestine as well as to promote the transmission of the pathogen to new hosts; in fact, for several hours after the pathogen has been excreted, it is thought to be in a hyperinfectious state that facilitates its transmission between hosts73,74,81,82. Genes encoding CT and Tcp are not present in all V. cholerae O1 isolates. ctxA and ctxB are embedded in the genome of CTXϕ, a lysogenic (that is, integrating its viral genome into the host’s) filamentous bacteriophage that has been independently acquired by a subset of V. cholerae lineages83. Similarly, genes encoding Tcp are present in only a subset of V. cholerae isolates — generally those of the O1 serogroup73, which are thought to account for all known cholera pandemics. Notably, only strains that produce Tcp can be infected by CTXϕ, as Tcp serves as the primary bacteriophage receptor. Consequently, the evolution of pathogenic V. cholerae is presumed to have involved sequential acquisition of the Tcp-encoding pathogenicity island (a pathogenicity island is a set of contiguous genes involved in virulence that are acquired by HGT) and then CTXϕ. The O139 pathogenic isolates that temporarily became prevalent in 1992 are thought to have arisen as a result of serogroup conversion of a toxigenic O1 progenitor84.
Vibrio parahaemolyticus
Despite the prevalence of V. parahaemolyticus-induced gastroenteritis, there is limited understanding of how this pathogen causes disease in the intestine. Almost all clinical isolates of V. parahaemolyticus show β-haemolysis activity when cultured on specialized blood agar (Wagatsuma agar), whereas almost all isolates from other sources are non-haemolytic; this difference is known as the Kanagawa phenomenon. Virulent V. parahaemolyticus strains produce a variety of recognized virulence factors during pathogenesis. Of these, Tdh85,86, which is responsible for the Kanagawa phenomenon, and Trh87 are currently the most predictive overall indicators of potential virulence. Most infections are associated with strains that possess tdh and trh, although there are notable published exceptions88. Both Tdh and Trh share several biological properties, including haemolytic activity, enterotoxicity and cytotoxicity89. Whole-genome sequencing efforts have identified that pathogenic isolates of V. parahaemolyticus also encode two type III secretion systems (T3SS): T3SS1 and T3SS2 (refs90,91). Secretion systems are multiprotein structures that mediate the translocation of bacterial effector proteins directly into eukaryotic cells90,92. T3SS1 and T3SS2 also ensure V. parahaemolyticus survival in the environment20. toxR, an ancestral locus in Vibrio spp., is required for V. parahaemolyticus fitness in vivo and for induction of expression of the T3SS2-related genes associated with gastroenteritis93. During infection, V. parahaemolyticus uses adhesion factors to bind to fibronectin and phosphatidic acid on the host cell, and it uses T3SS1 and T3SS2 to transport different effectors and toxins into the cytoplasm, causing cytotoxicity and serious diseases94.
In part, the paucity of knowledge of pathogenicity and virulence in V. parahaemolyticus results from the absence of an oral-infection-based animal model to replicate human disease; however, progress in this regard has enabled us to infer the crucial steps in how these infections develop91. Strain-to-strain variability in the infectious doses required to initiate V. parahaemolyticus gastroenteritis have been noted, with Pacific Northwest strains (for example, ST36 clonal type) demonstrating a substantially increased attack rate (a biostatistical measure of frequency of morbidity (or speed of spread of a specific pathogen) in an at-risk population) of 30%, corresponding to an infectious dose of 103–104 cells49. This infectious dose is significantly lower than the previous risk assessment analysis on pathogenic strains of V. parahaemolyticus 95.
Vibrio vulnificus
Unlike V. cholerae and V. parahaemolyticus, V. vulnificus is an opportunistic pathogen. Most patients with V. vulnificus infection (≥80%) also have liver disease55, which leads to elevated serum iron, which the bacterium requires for successful tissue growth and invasion. Indeed, most cases of V. vulnificus infection occur in men with underlying conditions resulting in elevated serum iron levels, primarily alcohol-associated liver cirrhosis. V. vulnificus produces both catechol and hydroxamate siderophores96 (high-affinity iron-chelating systems), but the fact that the organism requires high serum iron levels to produce a successful infection suggests that these siderophores are not able to scavenge iron from transferrin or other iron-binding proteins in human serum97 and, therefore, require an iron-saturated transferrin to obtain this key element. Because the liver is the largest source of iron in the human body, conditions associated with liver dysfunction and release of iron into the serum clearly increase the risk of V. vulnificus infection55. The crucial roles that iron has in all aspects of Vibrio spp. life, including pathogenesis, have been superbly summarized98, and, in V. vulnificus, the role of iron in the viable but non-culturable state (a state of suppressed metabolic activity in which the bacteria do not divide; bacteria in this state cannot be grown in culture but remain viable and potentially able to regrow under the appropriate environmental cues), chemotaxis, motility and survival in a host was also described99.
Virulence factors
Numerous studies have been published on the putative virulence factors of V. vulnificus; however, unlike in V. cholerae, there is much yet to be learned as to which gene products are crucial to the ability of this pathogen to cause such rapidly fatal infections. Thus far, the only virulence factor that has been demonstrated to be essential for successful infection is the bacterial capsule, as non-encapsulated bacteria are readily phagocytosed by macrophages55. The capsular LPS of the bacterium is an endotoxin; bacterial endotoxins stimulate inflammation and cytokine production by activated macrophages and B cells, leading to vasodilation, increased capillary permeability and activation of the complement and coagulation pathways. V. vulnificus endotoxin is probably responsible for causing substantial hypotension and generalized organ failure that can be fatal100. Of note, oestrogen has been reported to protect women against the endotoxin produced by this pathogen101. Also important for successful infections is a multifunctional-autoprocessing repeats-in-toxin (MARTX)102, essential for bacterial dissemination from the intestine103; the massive tissue destruction that characterizes both gastrointestinal and wound infections probably results from powerful collagenases, metalloproteinases and lipases and/or phospholipases that the bacterium produces55,104. Other virulence factors include the tonB systems, which are involved in tissue invasiveness and flagellum expression105, vvpE, which mediates intestinal colonization, a mucin-binding protein encoded by gbpA, which is essential for pathogenesis106,107, and the two-component signal transduction system gacS–gacA, which regulates biofilm formation and virulence108.
Biotypes
Complicating our understanding of pathogenesis is the fact that there are three biotypes of V. vulnificus 55. In addition, cells of biotype 1 strains are composed of two genotypes: a clinical (C) genotype, which is responsible for virtually all cases of primary septicaemia, and an environmental (E) genotype, which is associated with almost all of the wound infections109. These genotypes have substantial differences in DNA sequences and correlate well not only with human virulence but also with different isolation sources. Whereas 90% of human clinical isolates are the C-genotype, 85–90% of bacteria from environmental sources (shellfish, water, etc.) are the E-genotype55. Although whole-genome sequencing has been carried out on strains of the two genotypes110,111, to date such studies have not definitively elucidated which genes are essential for human virulence or why E-genotype cells enjoy a substantial environmental survival advantage over cells of the C-genotype in estuarine environments. Why wound infections are of the E-genotype, which typically does not cause septicaemias, is not yet known, although whole-genome sequencing of additional strains will probably identify gene variations that will help to answer these questions. The virulence factors required to cause these life-threatening wound infections probably include very efficient tissue-degrading enzymes, which lead to the characteristic necrotizing fasciitis (rapid and widespread necrosis of the subcutaneous tissue and the fascia) of these infections. As patients with wound infection exhibit a sex difference similar to that seen in patients with septicaemia, the E-genotype bacteria causing wound infections likely have virulence factors similar to those produced by C-genotype bacteria.
Importance of gene transfer
A key characteristic shared between all pathogenic Vibrio spp. is the ubiquity of pathogenicity markers acquired via HGT. Certainly, the best-known example of HGT contributing to the emergence of virulent Vibrio spp. is the presence of CTXϕ in toxigenic strains of V. cholerae 112. The major virulence genes in V. cholerae, which are clustered in several chromosomal regions, seem to have been recently acquired from bacteriophages or through undefined HGT events113, outlining the key role that this process has had on influencing virulence in this pathogen. Of note, environmental factors can influence the efficiency of HGT. In V. cholerae, high concentrations of chitin (a fibrous polysaccharide that is a major component of the exoskeleton of arthropods, such as crustaceans, and the scales of fish) — found naturally in the marine environment — induce an increase in competence and the ability to uptake DNA114. Similarly, in V. vulnificus, chitin has been shown to provide a substratum for Vibrio spp. to attach and exchange genetic information, leading to considerable HGT115. Finally, molecular analysis and comparative genomic analysis of pre-pandemic and pandemic strains revealed that the emergence of V. parahaemolyticus pandemic strains could be associated with recombination and HGT116,117.
Diagnosis, screening and prevention
Diagnosis of cholera
Cholera is a severe form of diarrhoea characterized by rice-water-like stool, which comes out forcibly (purging) at about 1 litre per hour, causing rapid fluid loss (dehydration). This severe diarrhoea is often associated with nausea and vomiting. About 75% of V. cholerae infections are asymptomatic118; among symptomatic infections, ~5% of cases are mild, 35% are considered moderate and ~60% of infections are considered severe119,120. The incubation period of V. cholerae is typically 5 days, although it can range from a few hours to several days121. An individual may be contagious (that is, expels viable bacteria in the faeces) for up to 14 days122. Upon presentation in clinical settings, clinical stool samples and blood samples are typically taken for standard microbiological identification (see below).
From a public health perspective, because of the potential of V. cholerae for spreading and the devastating consequences of epidemics, the management of cholera outbreaks requires immediate identification of cases123. Recent advances in rapid diagnostic tests (RDTs) have shown promise, particularly in settings where availability of microbiological and diagnostic facilities (for example, for PCR or serotyping analysis) are limited. Most RDT methods are based on the detection of V. cholerae O1 and O139 antigens in human stool samples124,125,126. These RDTs could be particularly useful in settings where they can be used alongside established and accredited testing methods and where rapid surveillance of cholera in a population can be used for management and preventive action. A WHO overview and guidance note of RDTs has been recently published123.
Diagnosis of vibriosis
A clinician could suspect vibriosis if a patient has watery diarrhoea and has recently eaten raw or undercooked seafood, especially oysters, or when a wound infection occurs after exposure to sea water127. For V. parahaemolyticus, the vast majority of infections are mild and self-limiting1. Following ingestion, the incubation period usually lasts 12–24 hours; the typical clinical characteristics of V. parahaemolyticus infections include abdominal cramps, diarrhoea, nausea, headaches, fever and chills42. Certainly, for more-serious cases of gastrointestinal vibriosis (for example V. vulnificus infection, with ~90% of cases requiring hospitalization) it is vital to obtain exposure history if the patient has underlying conditions, such as diabetes mellitus or liver diseases. V. vulnificus infections are characterized by an average 48-hour incubation period between the ingestion and onset of symptoms and an average 16-hour incubation period in the case of wound exposure55, highlighting the need for rapid diagnosis. V. vulnificus wound infections can be severe and result in necrotizing fasciitis (Fig. 5). The appropriate clinical samples (stool, blood or wound or ear secretions) are collected for microbiological confirmation of diagnosis.
a | Frequently, fatal Vibrio vulnificus infections can be initiated via minute entry sites. In this patient, the infection progressed to secondary septicaemia and led to a fatal outcome in ≤48 hours after exposure. b | V. vulnificus wound infections are also life altering, with tissue necrosis that necessitates tissue debridement and frequently finger and limb amputation. Images courtesy of J. D. Oliver, University of North Carolina, NC, USA.
Microbiological diagnosis
Vibrio spp. are typically easy to culture from clinical samples. Thiosulfate citrate bile-salts sucrose (TCBS) agar is the standard medium used commonly for the selective isolation and further subculturing of Vibrio spp. Strains that are able to metabolize sucrose, such as V. cholerae and V. alginolyticus, will form yellow colonies on TCBS agar media, whereas other pathogenic species such as V. parahaemolyticus, V. mimicus and V. vulnificus produce green colonies. Other media types, such as blood agar and CHROMagar to isolate V. parahaemolyticus and cellobiose-polymyxin B-colistin (CPC) media for isolation of V. vulnificus 128, can be used to culture colonies that appear green on TCBS agar. In the United States, blood agar is frequently used for initial isolation of Vibrio spp. from clinical samples. Samples that yield positive culture results can be sent to specialized laboratories (national reference laboratories in Europe and state clinical laboratories in the United States) for downstream confirmatory testing typically using species-specific PCR methods. Well-established and robust tests are available for all major Vibrio spp. pathogens, with associated conventional PCR129,130,131 and real-time PCR assays132,133,134,135 for species-level confirmation. More-in-depth molecular characterization, such as PCR of the virulence genes (for example, ctx (including ctxA and ctxB) PCR testing of V. cholerae 136 (to identify toxigenic strains), tdh and trh analysis of V. parahaemolyticus 130 and a variety of virulence-associated PCR tests for V. vulnificus 137,138), is frequently carried out during further clinical investigations. V. parahaemolyticus strains of major clinical significance can be further subtyped using specific PCR methods to identify pandemic strains such as those originating from pandemic groups139 and ST36 clonal types140. Biochemical tests such as appropriate serological testing to further subtype strains, particularly those originating from groups commonly associated with human infections, are frequently used for Vibrio spp. identification purposes; however, these methods have some limitations. For example, these methods are slow, tedious, require staff with a good knowledge for interpretation of results, have subjective interpretation and are expensive141,142.
Cholera prevention
Improvements in water supply, sanitation and food safety, coupled with community awareness, represent the most effective means of preventing cholera and other diarrhoeal diseases. Water, sanitation and hygiene (WASH) improvements in cholera-endemic countries have contributed to mitigate cholera outbreaks. Studies in Bangladesh have demonstrated that household members of patients with cholera are at a much higher risk of developing cholera than the general population; a hospital-based hygiene and water treatment intervention (Cholera-Hospital-Based-Intervention-for-7-Days (CHoBI7)) has shown great promises in reducing cholera infection among the household members of patients with cholera143.
Cholera vaccines have been very effective in controlling cholera; nevertheless, mass vaccination at the country level is not always easy for several reasons, including political or cultural hesitancy in vaccine acceptance, costs (as a booster dose of vaccine is also recommended) and lack of adequate supportive infrastructure for the storage and delivery of vaccines.
Cholera vaccines
The first cholera vaccines developed required parenteral administration; however, this administration route had limited efficacy and short duration of protection. As the oral route elicited increased mucosal antibody responses against cholera, a shift from parenteral vaccines to oral vaccine development occurred in the 1980s. Both live-attenuated and inactivated oral cholera vaccines (OCVs) have been developed and tested144,145,146. At present, three killed whole-cell OCVs have been WHO prequalified (Table 2). Dukoral has a protective efficacy of >60% and has indirect herd protection, bringing the overall level of protection to >90%147. Dukoral is licensed in >80 countries and has been used for vaccine campaigns and as a travellers’ vaccine to protect against cholera as well as diarrhoea caused by enterotoxigenic E. coli. However, this vaccine has not been routinely adopted for public health use, owing to its high cost and logistic issues with vaccine administration, as it needs bicarbonate buffer for reconstitution before intake. Affordable OCVs that do not require buffer for administration have been developed, including ORC-Vax and modified ORC-Vax (mORC-Vax), which include killed whole-cell V. cholerae O139. mORC-Vax has been used in Vietnam since 1997 in the national immunization programme148. The International Vaccine Institute (IVI) in South Korea has supported the technology transfer of the WHO prequalified OCV Shanchol to Incepta Pharmaceuticals in Bangladesh to produce a vaccine, Cholvax, that is undergoing clinical trials in Bangladesh (NCT02742558) before going through licensure. In addition, another OCV, OraVacs, is similar to Dukoral and is licensed for use in China and the Philippines149. The single-dose, live OCV CVD 103-HgR (Vaxchora) is at present approved by the FDA for use in travellers in some countries150. New-generation cholera vaccines are in phase I/II clinical trials (NCT02823899) as well as in preclinical studies151. All these efforts are expected to increase the current global OCV production and meet the needs of cholera-endemic and epidemic settings152.
The WHO recommends the use of OCVs for control of both endemic and epidemic cholera by pre-emptive vaccination and reactive vaccination (that is, vaccination in response to an existing epidemic), respectively122. With affordable OCVs commercially available in many countries and through the WHO OCV stockpile (established in 2013) for countries that request it, >17 million doses of OCVs have been used in 40 mass administration campaigns for control of outbreaks, endemic cholera and humanitarian crisis situations globally153. The WHO prequalified vaccines are recommended for use in anyone of ≥1 year of age (Euvichol and Shanchol) or ≥2 years of age (Dukoral). No vaccine is registered for use in pregnant women; however, the WHO recommends that pregnant women are included in OCV campaigns. Analysis of large OCV trials has shown that Shanchol is safe in pregnancy with no adverse events in newborn babies154,155. The two-dose Shanchol regimen has around 60% protective efficacy, lasting ≥5 years156. The longevity of protection is better in those of ≥5 years of age, and vaccines provide indirect herd protection, which can lead to ≥90% protective efficacy. A single-dose Shanchol regimen gave ≥6 months of protection from severe cholera requiring hospitalization in those of ≥5 years of age in Bangladesh157. Although vaccines can be used to combat cholera in disadvantaged areas, the efficacy of each cholera vaccine with regard to long-term prevention of cholera remains hotly debated. Amid these debates, different research groups are currently pursuing a new generation of cholera vaccines that would potentially have long shelf life, be easy to transport and store at room temperature and be administered as appropriate with long protective immunity. However, at present, the affordable OCVs are being used to control epidemic and endemic cholera globally. There remains a shortage of OCVs since demand has increased after the establishment of the stockpile.
Prevention of vibriosis
A range of preventive approaches have been successfully applied to prevent non-cholera Vibrio spp. infections, particularly from seafood sources. Common regulatory control measures include monitoring harvest waters and high-risk food items (such as oysters) by microbiological analysis9. Control measures developed in the United States, where vibriosis originating from seafood produce is increasing, include state-level risk assessments and appropriate cold-chain processing of shellfish based on tightly controlled risk appraisals. Postharvest processing methods, such as high-pressure treatment, irradiation, quick-freezing and pasteurization, are available to make seafood produce safe9. These approaches are effective158. In April 2003, California implemented a regulation restricting the sale of raw oysters harvested from the Gulf of Mexico from 1 April to 31 October unless they were processed to reduce V. vulnificus to nondetectable levels using appropriate postharvesting processing methods. This regulation led to a considerable drop in the number of reported V. vulnificus infections and deaths in California associated with raw oysters158. However, in other US states, V. vulnificus infections remain a public health issue. In addition, educational efforts to reduce the risk of infection have been initiated to raise awareness in consumers, restaurant proprietors and physicians about the hazards of eating raw shellfish159. However, there remains little evidence to suggest that these efforts have been successful, as seafood-associated infections have been increasing7.
There have been advances in the use of remote sensing methods, such as those that can directly measure sea surface temperature, as an approach to reduce risks associated with Vibrio spp. and as a forecasting method to identify at-risk areas. The European Centre for Disease Prevention and Control has established a global Vibrio spp. suitability mapping tool that enables 24-hour updated data160. These remote-sensing-enabled methods are increasingly being applied to study outbreaks retrospectively and determine risk factors for outbreaks, and they could offer advance warnings, such as rapid warming in temperate areas, that indicate an increased risk of the presence of Vibrio spp.41. Decreasing the incidence of wound infections is challenging as these mostly occur in individuals engaged in recreational activities in coastal waters. However, the CDC recommends limiting exposure to water and shellfish in individuals who have underlying risk conditions that could increase the probability or the severity of Vibrio spp. infections127. This recommendation is particularly relevant for V. vulnificus and where exposure-associated infections are easily preventable in at-risk groups.
Management
Treatment of Vibrio spp. infections varies depending on the pathogen responsible, route of transmission and observed clinical manifestations (Table 3). Many Vibrio spp. infections are self-limiting and do not require medical intervention beyond supportive care (such as drinking plenty of liquids to replace fluids lost through diarrhoea)127. However, important medical interventions are required where more-serious infections or clinical presentations are evident.
Cholera
Only about one in five individuals that aquire toxigenic V. cholerae exhibits symptomatic cholera, and the severity of the disease depends on both the pathogenic factors of V. cholerae and the host factors, such as age and nutritional and immune system status. Cholera can still be a fatal disease, and mortality in persons with severe cholera can exceed 70% if prompt clinical diagnosis and appropriate management are not available162. Therapy includes rehydration (orally or intravenously), antibiotics and nutritional supplements in malnourished individuals.
Rehydration therapy and maintenance of hydration
Patients with cholera should be treated with oral rehydration solution (ORS), promoting replacement of water and electrolytes lost by patients through frequent passage of voluminous rice-watery stool (Table 3). The WHO guidelines should be followed to evaluate the dehydration status of the patients163; the assessment is based on the clinical evaluation and examination of the patient’s level of consciousness, eyes, tongue, thirst, skin turgor and rate of radial pulse. For mild-to-moderate cases, ORS is used both for rehydration (the initial therapy to restore fluid and electrolytes until the deficit has been replaced) and maintenance of hydration while diarrhoea persists. In addition to glucose-based ORS, rice ORS (ORS in which rice powder replaces glucose) is useful in reducing stool output during both rehydration and maintenance therapy163,164. The patient should be kept under observation and dehydration status should be assessed periodically. Patients with severe dehydration, and many with moderate dehydration (frequent vomiting ≥3 times in an hour), require emergency administration of intravenous fluid164. Ringer’s lactate is a commonly used rehydration fluid; normal saline or cholera saline can also be used. For both adults and children, initial bolus therapy (the first part of the infusion) should be repeated if danger signs (that is, hypovolemic shock) are present after the initial bolus or if the radial pulse remains weak or undetectable. Intravenous fluid should be delivered in continuous infusion until the fluid deficit has been replaced; ORS can then be initiated to keep up with ongoing fluid losses from persistent purging of watery diarrhoea. Each stool that occurs during maintenance therapy should be replaced with a volume of ORS similar to that given during maintenance therapy. Ideally, maintenance therapy should be with ORS but can be performed with intravenous fluid in addition to that prescribed initially. Children with severe acute malnutrition should be managed carefully to prevent acute fluid overload and heart failure; in these patients, the intavenous rehydration process is spaced over 10–12 hours165.
Antibiotic therapy
Antibiotic treatment is initiated following resolution of the initial fluid deficit and cessation of vomiting. This therapy reduces the total volume of stool passed and shortens the period of faecal excretion of V. cholerae 166. The choice of antibiotic can be dictated by local antimicrobial susceptibility profiles. At present, azithromycin and ciprofloxacin are commonly used122,167. However, the pattern of resistance of pathogens can fluctuate in accordance with withdrawal of use of a specific antibiotic in the community. Because of widespread resistance to antibiotics, surveillance is needed to detect changing sensitivity patterns for determining the drug of choice for treating cholera. Molecular analyses are also conducted to determine the mechanism of resistance and its global spread168. When the local V. cholerae isolates are sensitive to azithromycin, children are given 20 mg per kg and adults are given 1 g, each as a single-dose regimen169. Ciprofloxacin is given to children in a dose of 15 mg per kg twice daily for 3 days. On the basis of the antibiotic resistance pattern, a single dose of 300 mg doxycycline in adults may be prescribed. Prophylactic administration of antibiotics during outbreaks or for travellers is not advised.
Zinc supplementation
Zinc therapy in children reduces the morbidity and mortality associated with cholera and other diarrhoeal diseases, as zinc can decrease the duration and severity of diarrhoea170. Zinc is given daily to children (6 months to 5 years of age) with diarrhoea, including those with cholera, as an adjunct therapy, starting as soon as the vomiting subsides, for 10 days171. For children with severe malnutrition and diarrhoea, zinc treatment is recommended for 14 days172. The dehydration status is determined on the basis of clinical signs and symptoms164,173. If there are no signs of dehydration, the preferred treatment is with ORS to prevent dehydration and continued oral feeding is advised for quick recovery.
Complex emergencies
Cholera is increasingly being reported among populations that have never previously witnessed this disease (as in Haiti174 and Yemen175) and in cholera-endemic settings that experience natural or man-made disasters (as in, for example, some African countries, Iraq and Pakistan). In addition to traditional interventions (such as improvements and access to safe water, sanitation and hygiene), prevention and mitigation of cholera in these complex settings also require a portfolio of unconventional strategies, including social, political and educational awareness with implementation of existing treatment and prevention strategies and new scientific-based tools. In these complex scenarios, first responders (such as Doctors without Borders, the United Nations, the WHO and different non-governmental organizations) need to engage local partners (including Ministry of Health and community leaders) and potentially volunteer groups with empathy and emphasize the disastrous consequences of the outbreak if it is not counteracted fast and effectively. The involvement of local organizations in the affected areas could help first responders to mitigate disease transmission through practising optimal sanitation, hygiene, clean food and water intake and avoiding contact with the belongings of patients with cholera. Moreover, locals can ensure that any person showing symptoms of cholera must seek immediate attention at their nearby hospitals and/or clinics to receive adequate treatment. Finally, scientists are also investigating whether a cocktail of vibriophages (bacteriophages that specifically infect V. cholerae) can be used as an alternative therapy for cholera treatment176.
Vibriosis
V. alginolyticus is often associated with ear and soft tissue infections, which can be readily treated using appropriate antibiotics such as doxycycline177. Gastroenteritis associated with V. parahaemolyticus infection is typically self-limiting and resolves within 72 hours42. Very rarely, medical intervention is required, although antibiotic therapy is sometimes used if infections do not resolve or progress to systemic infections. However, given the extremely rapid development of V. vulnificus infections, rapid diagnosis of both septicaemia and localized wound infections is absolutely essential. Often crucial to this end is obtaining good patient histories that indicate raw seafood (particularly oyster) consumption and/or water exposure. Along with rapid diagnosis, prompt and appropriate antibiotic treatment is also needed, as a treatment delay of ≥72 hours after symptom development can raise the case fatality rate to 100%178. Hospitalized patients with V. vulnificus infection frequently require tissue debridement (removal of necrotic tissue) and/or amputation of the affected limbs to limit spread of the infection. Antibiotic treatment recommendations for Vibrio spp. infections include tetracyclines (for example, doxycycline and tetracycline), fluoroquinolones (ciprofloxacin and levofloxacin), third-generation cephalosporins (cefotaxime, ceftazidime and ceftriaxone), aminoglycosides (amikacin, apramycin, gentamicin and streptomycin) and folate pathway inhibitors (trimethoprim–sulfamethoxazole)179,180. The CDC recommends a treatment course of doxycycline (oral or intravenous twice a day for 7–14 days) and a third-generation cephalosporin (intravenous or intramuscular every 8 hours for 7–14 days). However, a review of antibiotic usage data suggests that for V. vulnificus, treatment that includes either quinolone or tetracycline is associated with lower mortality than treatment with cephalosporin alone181. Some resistance to antibiotics has been observed in non-cholera Vibrio spp. such as V. parahaemolyticus and V. vulnificus from environmental sources179,182,183. There is increasing interest in the generation of new therapeutic approaches for specific Vibrio spp. pathogens. New monoclonal antibodies against the carboxyl terminus of V. vulnificus putative MARTX, RtxA1, effectively provided protective immunity in a mouse model of V. vulnificus infection161. Such approaches could be useful in particular for at-risk groups (for example, people handling shellfish produce).
Quality of life
In areas of the world where sanitation and access to clean drinking water are lacking, cholera continues to represent an important cause of morbidity and mortality. Advances in rehydration therapy have made cholera a treatable disease with a low case fatality rate147. However, individuals who survive cholera can have both short-term and long-term health consequences. The immediate consequences include loss of body weight and physical vigour, resulting in restrictions on an individual’s day-to-day quality of life. The purging of watery stool results in expulsion of healthy gut commensal microbiota, and the 3-day course of antibiotic therapy could enable drug-resistant pathogenic Enterobacteriaceae bacteria to be selectively enriched in the gut184. Colonization of the gut by drug-resistant pathogenic genera is causally related to frequent diarrhoea in children of ≤5 years of age185, with long-term consequences such as persistent microbiota immaturity (as the prevalence of drug-resistant species affects the normal commensal gut microbiota)186, which could contribute to malnutrition and lead to irreparable growth stunting and impaired cognitive function. Although the WHO prequalified OCVs have been successfully used in vaccination programmes to prevent cholera in many countries, for a vast number of people the access to vaccines when there is an outbreak still remains challenging owing to the underlying financial and logistic issues globally. Many studies have estimated the cost-effectiveness of vaccine use following WHO criteria and found it both considerable and incremental. The incremental cost-effectiveness ratios for cholera in Zanzibar, Africa, were estimated to be US$750,000 per death averted, US$6,000 per case averted and US$30,000 per disability-adjusted life-year averted, regardless of the differences in the health-care providers and the societal perspectives on the effect of cholera on individuals and on the use of vaccines187.
Cases of vibriosis are typically self-limiting (for example, V. parahaemolyticus-associated gastroenteritis), with few notable long-term quality-of-life issues associated with these infections. However, V. vulnificus-associated wound infections can frequently result in life-altering clinical interventions such as limb or finger amputation and substantial tissue debridement (Fig. 5). V. vulnificus infections are also the most expensive marine-acquired infections188, underlying the substantial and long-term189 medical interventions often required. A key feature of vibriosis (in particular wound infections) is the need for stringent education programmes for at-risk groups, such as individuals with underlying risk conditions (for example, liver disease, a compromised immune system and diabetes mellitus).
Outlook
Vibrio spp. infections have remained a scourge to humankind for over a millennium190, and V. cholerae and V. parahaemolyticus have caused numerous pandemic outbreaks47,191. Many advances have been made in our knowledge of the mechanism of persistence of pathogenic Vibrio spp. in aquatic reservoirs, the transmission of bacteria from reservoirs to humans causing infections and the pathobiology of disease, and progress has been made in rapid diagnosis and effective intervention strategies. Nevertheless, Vibrio spp. infections are expected to rise in the future. Such a rise could be attributed to global warming, continued population growth (particularly in developing countries where poverty is common), protracted wars and dwindling access to safe drinking water and optimal sanitation. Given that Vibrio spp. infections — particularly cholera — disproportionately affect individuals living in resource-poor countries, the mobilization of resources and timely distribution and storage of supplies, including ORS, vaccines, antibiotics and water purification tablets, are central to mitigate these threats. In addition, risk awareness campaigns and information on management of Vibrio spp. infections through mass media, including social media, would be beneficial. Of note, the majority of Vibrio spp. infections are seasonal and primarily driven by increased temperature, rainfall events and contamination of aquatic reservoirs with Vibrio spp. pathogens. The transient bloom of Vibrio spp. in aquatic reservoirs during warm months is thought to ‘spill over’ to susceptible human populations. Basic and translational research in different areas will contribute to reduce the burden of Vibrio spp. infections (Box 3).
Cholera
Cholera is a preventable disease, yet it remains a persistent source of morbidity and mortality, particularly in resource-limited countries with insufficient access to clean water and appropriate sanitation, and can emerge rapidly in areas where basic environmental infrastructures are disrupted (Box 4). The most effective means to tackle cholera outbreaks are coordinated and multidisciplinary approaches and the availability of appropriate vaccines. Studies have shown that knowledge of the local understanding of cholera can be used to help to manage outbreaks192, and attention to local social and cultural features of cholera can help to increase vaccine coverage193. Thus, sociocultural sciences can contribute to understanding and mitigating cholera outbreaks. Recent investigations have demonstrated the effective killing of V. cholerae by vibriophages194. Manipulating the environmental vibriophage populations could be a future approach to ameliorate cholera outbreaks, promptly shorten cholera epidemics at the community level and limit V. cholerae spread from environmental blooms.
However, many questions remain unanswered. For example, how can toxigenic V. cholerae persist in aquatic reservoirs during interepidemic periods and erupt sporadically in some regions, whereas it completely disappears in other regions? Why do only 20–25% of individuals with V. cholerae infection exhibit symptomatic cholera, whereas most individuals are asymptomatic carriers? With the advent of modern molecular techniques, including metagenomics analysis, real-time PCR and single-cell sorting with automated genetic characterization, V. cholerae from both aquatic reservoirs (including biofilm bacteria) and stool and/or rectal swab samples of household members of patients with cholera should be examined to address these questions. Knowledge gained from these suggested investigations can potentially help to identify risk factors for Vibrio spp. infections and design appropriate and effective intervention strategies to mitigate Vibrio spp. infections.
Changing epidemiology
A notable data gap in the field of Vibrio spp. research is the availability of surveillance data regarding Vibrio spp. infections globally. For instance, in Europe, vibriosis is not a notifiable infection42,62; as a result, there is a paucity of epidemiological and surveillance data regarding these pathogens. Good-quality national surveillance systems do exist, such as COVIS and FoodNet in the United States7, and the data gathered from such systems are invaluable in building up a clear picture of the routes of exposure and changes in incidence and regional effects that these pathogens can have (Fig. 3). We advocate developing a centralized depository of epidemiological data that can be used by researchers in the field of Vibrio spp. microbiology.
Climate warming, in particular rapid warming of coastal regions caused by climate change195, is likely to greatly expand the geographical extent and effects of pathogenic Vibrio spp.1,6,21,49,196 (Fig. 6). Striking evidence of this process has emerged since 2000, including key studies assessing the link between the changing abundance of these bacteria in the environment and environmental warming196,197, the increasing number of reported wound infections observed in temperate areas161 and shellfish-associated outbreaks at high latitudes198,199. These studies, coupled with the preference of these pathogens for growing in warm, brackish water, suggest that these bacteria are likely to continue causing infections under a warming climate scenario (Fig. 6).
Average change in the sea surface temperature around the world between 1901 and 2015. Measurements are based on a combination of direct measurements and satellite measurements. Data show that in most parts of the world the oceans have become warmer, although regionally a decrease in the temperature has occurred (for example, in the North Atlantic). Overall, rising sea surface temperatures favour the spread of Vibrio spp. and increase the population at risk of infection. Based on Figure 2.21 from Hartmann, D.L., et al, in Climate Change 2013: The Physical Science Basis. Contribution of Working Group I to the Fifth Assessment Report of the Intergovernmental Panel on Climate Change (eds Stocker, T.F. et al). (Cambridge University Press, Cambridge and New York, 2013).
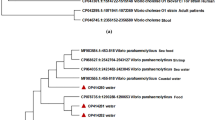
Methods such as whole-genome sequencing have provided incredible insights into the genomic structure, evolution19,20 and virulence capabilities of key members of the Vibrio genus. Whole-genome sequencing has enabled the determination of the source of outbreaks18 and the establishment of the evolutionary history of causative strains191. However, there remain many questions that advances in strain genotyping methods will help to resolve, such as why the Bay of Bengal region has been the source of many pandemic waves of V. cholerae 191 and pandemic O3:K6 V. parahaemolyticus 47 (Fig. 2), or how the rapid geographical expansion of infections following the establishment of strains with pandemic potential was possible. Certainly, with cholera, human travel has been an effective long-distance mechanism of transmission200. However, V. parahaemolyticus has a very different lifestyle and disease transmission route. The rapid expansion of V. parahaemolyticus during pandemic spreading, such as the O3:K6 strain in the 1990s and early 2000s47 and the 2012 long-distance expansion of the Pacific Northwest ST36 clonal type51,201, suggests that mechanisms such as the transfer of shellfish or ballast water movement202,203,204 are involved. Novel sequencing and bioinformatic approaches to infer the evolutionary timelines coupled to these physical transmission routes may help to shed light on epidemic spreading.
A key area of current work is determining the environmental features that drive Vibrio spp. outbreaks. Retrospective studies that have analysed key environmental features before, during and after Vibrio spp. outbreaks are identifying key factors involved in pathogen proliferation, such as anomalous temperature-driven events in non-cholera Vibrio spp.41,49,62, and the role of temperature, sea surface height, plankton blooms, precipitation and flooding in V. cholerae emergence24,26,27,29,30. The methods that frequently use remote-sensing-based approaches are now providing key insights into what specific environmental conditions help to drive outbreaks22. Linking these approaches alongside epidemiological and climatic models such as regional climate change models (for example, with different emission scenarios) may help to identify where outbreaks are likely to emerge in the future205. This information is particularly relevant given predictions regarding warming in many coastal regions driven by climate change.
References
Baker-Austin, C., Trinanes, J., Gonzalez-Escalona, N. & Martinez-Urtaza, J. Non-Cholera vibrios: the microbial barometer of climate change. Trends Microbiol. 25, 76–84 (2017).
Oliver, J. D. Wound infections caused by Vibrio vulnificus and other marine bacteria. Epidemiol. Infect. 133, 383–391 (2005).
Shah Faruque, M. & Epidemiology, G. B. N. in The Biology of Vibrios (Thompson, F. L. et al.) 394 (ASM Press, 2006).
Altekruse, S. F. et al. Vibrio gastroenteritis in the US Gulf of Mexico region: the role of raw oysters. Epidemiol. Infect. 124, 489–495 (2000).
Howard-Jones, N. Robert Koch and the cholera vibrio: a centenary. Br. Med. J. Clin. Res. Ed 288, 379–381 (1984).
Vezzulli, L., Colwell, R. R. & Pruzzo, C. Ocean warming and spread of pathogenic vibrios in the aquatic environment. Microb. Ecol. 65, 817–825 (2013).
Newton, A., Kendall, M., Vugia, D. J., Henao, O. L. & Mahon, B. E. Increasing rates of vibriosis in the United States, 1996-2010: Review of surveillance data from 2 systems. Clin. Infect. Dis. 54, 391–395 (2012). This paper provides an epidemiological overview outlining the increasing risks associated with Vibrio spp. in the United States.
Scallan, E. et al. Foodborne illness acquired in the United States — Major pathogens. Emerg. Infect. Dis. 17, 7–15 (2011).
Iwamoto, M., Ayers, T., Mahon, B. E. & Swerdlow, D. L. Epidemiology of seafood-associated infections in the United States. Clin. Microbiol. Rev. 23, 399–411 (2010).
World Health Organization. Weekly epidemiological record. Weekly epidemiological record 21, 421–428 (2016).
Zuckerman, J. N., Rombo, L. & Fisch, A. The true burden and risk of cholera: implications for prevention and control. Lancet Infect. Dis. 7, 521–530 (2017).
World Health Organization. Cholera. WHO http://www.who.int/mediacentre/factsheets/fs107/en/ (2017).
Ali, M. et al. Le fardeau mondial du choléra. Bull. World Health Organ. 90, 209–218 (2012).
Sack, D. A., Sack, R. B., Nair, G. B. & Siddique, A. K. Cholera. Lancet (Lond., Engl.) 363, 223–233 (2004).
Pollitzer, R., Swaroop, S., Burrows, W. & WHO. Cholera / R. Pollitzer; with a chapter on world incidence, written in collaboration with S. Swaroop, and a chapter on problems in immunology and an annex, written in collaboration with W. Burrows. (WHO, 1959).
Barua, D. in Cholera 1–5 (eds Barua, D. & Greenough, W. B. 3rd) 1–36 (Plenum Medical Book, 1992).
Poirier, M. J., Izurieta, R., Malavade, S. S. & McDonald, M. D. Re-emergence of Cholera in the Americas: risks, susceptibility, and ecology. J. Glob. Infect. Dis. 4, 162–171 (2012).
Orata, F. D., Keim, P. S. & Boucher, Y. The 2010 Cholera outbreak in Haiti: how science solved a controversy. PLOS Pathog. 10, e1003967 (2014).
Weill, F.-X. et al. Genomic history of the seventh pandemic of cholera in Africa. Science 358, 785–789 (2017).
Domman, D. et al. Integrated view of Vibrio cholerae in the Americas. Science 358, 789–793 (2017).
Colwell, R. R. Global climate and infectious disease: the cholera paradigm. Science 274, 2025–2031 (1996). This article provides a comprehensive overview on the effect of climate on cholera epidemics.
Lipp, E. K., Huq, A. & Colwell, R. R. Effects of global climate on infectious disease: the cholera model. Clin. Microbiol. Rev. 15, 757–770 (2002).
Sack, R. B. et al. A 4-Year Study of the Epidemiology of Vibrio cholerae in Four Rural Areas of Bangladesh. J. Infect. Dis. 187, 96–101 (2003).
Lobitz, B. et al. Climate and infectious disease: use of remote sensing for detection of Vibrio cholerae by indirect measurement. Proc. Natl Acad. Sci. USA 97, 1438–1443 (2000).
Pascual, M., Rodo, X., Ellner, S. P., Colwell, R. & Bouma, M. J. Cholera dynamics and El Nino-Southern Oscillation. Science 289, 1766–1769 (2000).
Huq, A. et al. Critical factors influencing the occurrence of Vibrio cholerae in the environment of Bangladesh. Appl. Environ. Microbiol. 71, 4645–4654 (2005).
Huq, A. et al. Environmental factors influencing epidemic Cholera. Am. J. Trop. Med. Hyg. 89, 597–607 (2013).
Worden, A. Z. et al. Trophic regulation of Vibrio cholerae in coastal marine waters. Environ. Microbiol. 8, 21–29 (2006).
Hashizume, M. et al. The effect of rainfall on the incidence of cholera in Bangladesh. Epidemiology 19, 103–110 (2008).
Koelle, K. The impact of climate on the disease dynamics of cholera. Clin. Microbiol. Infect. 15, 29–31 (2009).
Ramamurthy, T. & Sharma, N. C. Cholera outbreaks in India. Curr. Top. Microbiol. Immunol. 379, 49–85 (2014).
Ries, A. A. et al. Cholera in Piura, Peru: a modern urban epidemic. J. Infect. Dis. 166, 1429–1433 (1992).
Goh, K. T., Teo, S. H., Lam, S. & Ling, M. K. Person-to-person transmission of cholera in a psychiatric hospital. J. Infect. 20, 193–200 (2017).
Sugimoto, J. D. et al. Household transmission of Vibrio cholerae in Bangladesh. PLoS Negl. Trop. Dis. 8, e3314 (2014).
Rabbani, G. H. & Greenough, W. B. 3rd. Food as a vehicle of transmission of cholera. J. Diarrhoeal Dis. Res. 17, 1–9 (1999).
Alam, M. et al. Seasonal cholera caused by Vibrio cholerae serogroups O1 and O139 in the coastal aquatic environment of Bangladesh. Appl. Environ. Microbiol. 72, 4096–4104 (2006).
Nair, G. B. et al. New variants of Vibrio cholerae O1 biotype El Tor with attributes of the classical biotype from hospitalized patients with acute diarrhea in Bangladesh. J. Clin. Microbiol. 40, 3296–3299 (2002).
Reina, J. The 8th cholera pandemic: Vibrio cholerae serogroup 0139 (Bengala strain). Enferm. Infecc. Microbiol. Clin. 13, 246–251 (1995).
Chowdhury, F. et al. Vibrio cholerae serogroup O139: isolation from Cholera patients and asymptomatic household family members in Bangladesh between 2013 and 2014. PLoS Negl. Trop. Dis. 9, e0004183 (2015).
Deshayes, S. et al. Non-O1, non-O139 Vibrio cholerae bacteraemia: case report and literature review. Springerplus 4, 1–9 (2015).
Baker-Austin, C. et al. Heat wave-associated vibriosis, Sweden and Finland, 2014. Emerg. Infect. Dis. 22 (2016).
Baker-Austin, C., Stockley, L., Rangdale, R. & Martinez-Urtaza, J. Environmental occurrence and clinical impact of Vibrio vulnificus and Vibrio parahaemolyticus: A European perspective. Environ. Microbiol. Rep. 2, 7–18 (2010).
Barker, W. H. J. in International Symposium on Vibrio parahaemolyticus (eds Fujino, T., Sakaguchi, G., Sakazaki, R. & Takeda, Y.) 47–52 (Saikon Publishing Co., Ltd., 1974).
Dadisman, T. A. J., Nelson, R., Molenda, J. R. & Garber, H. J. Vibrio parahaemolyticus gastroenteritis in Maryland. I. Clinical and epidemiologic aspects. Am. J. Epidemiol. 96, 414–426 (1972).
Fishbein, M., Wentz, B. & Landry, W. L. in International Symposium on Vibrio parahaemolyticus (eds Fujino, T., Sakaguchi, G., Sakazaki, R. & Takeda, Y.) 53–58 (Saikon Publishing Co., Ltd., 1974).
Joseph, S. W., Colwell, R. R. & Kaper, J. B. Vibrio parahaemolyticus and related halophilic Vibrios. Crit. Rev. Microbiol. 10, 77–124 (1982).
Nair, G. B. et al. Global dissemination of Vibrio parahaemolyticus serotype O3:K6 and its serovariants. Clin. Microbiol. Rev. 20, 39–48 (2007). This paper presents a succinct and historical overview of the pandemic spread of V. parahaemolyticus.
Okuda, J. et al. Emergence of a unique O3:K6 clone of Vibrio parahaemolyticus in Calcutta, India, and isolation of strains from the same clonal group from Southeast Asian travelers arriving in Japan. J. Clin. Microbiol. 35, 3150–3155 (1997).
Martinez-Urtaza, J., Bowers, J. C., Trinanes, J. & DePaola, A. Climate anomalies and the increasing risk of Vibrio parahaemolyticus and Vibrio vulnificus illnesses. Food Res. Int. 43, 1780–1790 (2010).
Li, Y. et al. Vibrio parahaemolyticus, Southern Coastal region of China 2007–2012. Emerg. Infect. Dis. 20, 2012–2015 (2014).
Martinez-Urtaza, J. et al. Spread of Pacific Northwest Vibrio parahaemolyticus strain. N. Engl. J. Med. 369, 1573–1574 (2013). This study is the first to show the pandemic spread of ST36 clonal type V. parahaemolyticus.
Martinez-Urtaza, J. et al. Epidemiological investigation of a foodborne outbreak in Spain associated with U. S. West Coast genotypes of Vibrio parahaemolyticus. SpringerPlus 5, 87 (2016).
Wagley, S. et al. Galleria mellonella as an infection model to investigate virulence of Vibrio parahaemolyticus. Virulence 9, 197–207 (2017).
Food and Agriculture Organization of the United Nations. Risk Assessment of Vibrio parahaemolyticus in Seafood. FAO (2011).
Jones, M. K. & Oliver, J. D. Vibrio vulnificus: Disease and pathogenesis. Infect. Immun. 77, 1723–1733 (2009). This article presents one of the most cited reviews on the virulence of V. vulnificus.
Centers for Disease Control. Vibrio vulnificus infections associated with raw oyster consumption. Morb. Mortal. Wkly. Rep. 42, 405–407 (1993).
Scaglione, S. et al. The epidemiology of cirrhosis in the United States: a population-based study. J. Clin. Gastroenterol. 49, 690–696 (2015).
Rippey, S. R. Infectious diseases associated with molluscan shellfish consumption. Clin. Microbiol. Rev. 7, 419–425 (1994).
Fouz, B., Roig, F. J. & Amaro, C. Phenotypic and genotypic characterization of a new fish-virulent Vibrio vulnificus serovar that lacks potential to infect humans. Microbiology 153, 1926–1934 (2007).
Bisharat, N. et al. Clinical, epidemiological, and microbiological features of Vibrio vulnificus biogroup 3 causing outbreaks of wound infection and bacteraemia in Israel. Israel Vibrio Study Group. Lancet 354, 1421–1424 (1999). This paper provides the first description of V. vulnificus biotype 3.
Hori, M. et al. A case of Vibrio vulnificus infection complicated with fulminant purpura: gene and biotype analysis of the pathogen. JMM Case Reports 4, e005096 (2017).
Baker-Austin, C. et al. Emerging Vibrio risk at high latitudes in response to ocean warming. Nat. Clim. Chang. 3, 73–77 (2012). This article presents the first study to show the spread of pathogenic Vibrio spp. into temperate regions and the role of climate on mediating risk.
Zhao, H. et al. Correlations between clinical features and mortality in patients with Vibrio vulnificus infection. PLoS One 10, e0136019 (2015).
Chuang, Y. C., Yuan, C. Y., Liu, C. Y., Lan, C. K. & Huang, A. H. Vibrio vulnificus infection in Taiwan: report of 28 cases and review of clinical manifestations and treatment. Clin. Infect. Dis. 15, 271–276 (1992).
Raszl, S. M., Froelich, B. A., Vieira, C. R. W., Blackwood, A. D. & Noble, R. T. Vibrio parahaemolyticus and Vibrio vulnificus in South America: water, seafood and human infections. J. Appl. Microbiol. 121, 1201–1222 (2016).
Osaka, K., Komatsuzaki, M., Takahashi, H., Sakano, S. & Okabe, N. Vibrio vulnificus septicaemia in Japan: an estimated number of infections and physicians’ knowledge of the syndrome. Epidemiol. Infect. 132, 993–996 (2004).
Park, S. D., Shon, H. S. & Joh, N. J. Vibrio vulnificus septicemia in Korea: clinical and epidemiologic findings in seventy patients. J. Am. Acad. Dermatol. 24, 397–403 (1991).
Weis, K. E., Hammond, R. M., Hutchinson, R. & Blackmore, C. G. M. Vibrio illness in Florida, 1998–2007. Epidemiol. Infect. 139, 591–598 (2011).
World Health Organization & Food and Agriculture Organization of the United Nations. Microbiological Risk Assessment Series (WHO & FAO, 2004).
Gangarosa, E. F., Beisel, W. R., Benyajati, C., Sprinz, H. & Piyaratn, P. The nature of the gastrointestinal lesion in asiatic cholera and its relation to pathogenesis: a biopsy study. Am. J. Trop. Med. Hyg. 9, 125–135 (1960).
D. E., S. N. Enterotoxicity of bacteria-free culture-filtrate of Vibrio cholerae. Nature 183, 1533–1534 (1959).
Levine, M. M., Kaper, J. B., Black, R. E. & Clements, M. L. New knowledge on pathogenesis of bacterial enteric infections as applied to vaccine development. Microbiol. Rev. 47, 510–550 (1983).
Ritchie, J. M. & Waldor, M. K. Vibrio cholerae interactions with the gastrointestinal tract: lessons from animal studies. Curr. Top. Microbiol. Immunol. 337, 37–59 (2009).
Nelson, J., Eric & Harris, Jason & Glenn Morris, J. & Calderwood, B. Stephen & Camilli, A. Cholera transmission: The host, pathogen and bacteriophage dynamic. Nat. Rev. Microbiol. 7, 693–702 (2009).
Kirn, T. J., Lafferty, M. J. & Sandoe, C. M., T. R. Delineation of pilin domains required for bacterial association into microcolonies and intestinal colonization by Vibrio cholerae. Mol. Microbiol. 35, 896–910 (2000).
Herrington, D. A. et al. Toxin, toxin-coregulated pili, and the toxR regulon are essential for Vibrio cholerae pathogenesis in humans. J. Exp. Med. 168, 1487–1492 (1988).
Bartlett, T. M. et al. A periplasmic polymer curves Vibrio cholerae and promotes pathogenesis. Cell 168, 172–185.e15 (2017).
Chao, M. C., Abel, S., Davis, B. M. & Waldor, M. K. The design and analysis of transposon insertion sequencing experiments. Nat. Rev. Microbiol. 14, 119–128 (2016).
Weber, G. G. & Klose, K. E., K. The complexity of ToxT-dependent transcription in Vibrio cholerae. Indian J. Med. Res. 133, 201–206 (2011).
Rutherford, S. T. & Bassler, B. L. Bacterial quorum sensing: its role in virulence and possibilities for its control. Cold Spring Harb. Perspect. Med. 2, 1–25 (2012).
Chao, M. C. et al. A cytosine methyltransferase modulates the cell envelope stress response in the Cholera pathogen. PLoS Genet. 11, e1005666 (2015).
Millet, Y. A. et al. Insights into Vibrio cholerae intestinal colonization from monitoring fluorescently labeled bacteria. PLoS Pathog. 10, e1004405 (2014).
Davis, B. M., Moyer, K. E., Boyd, E. F. & Waldor, M. K. CTX prophages in classical biotype Vibrio cholerae: functional phage genes but dysfunctional phage genomes. J. Bacteriol. 182, 6992–6998 (2000).
Faruque, S. M. et al. Emergence and evolution of Vibrio cholerae O139. Proc. Natl Acad. Sci. USA 100, 1304–1309 (2003).
Nishibuchi, M. & Kaper, J. B. Thermostable direct hemolysin gene of Vibrio parahaemolyticus: a virulence gene acquired by a marine bacterium. Infect. Immun. 63, 2093–2099 (1995). This study analyses tdh , which is used as a genetic marker for virulence in the diagnosis of pathogenic V. parahaemolyticus.
Letchumanan, V., Chan, K. G. & Lee, L. H. Vibrio parahaemolyticus: A review on the pathogenesis, prevalence, and advance molecular identification techniques. Front. Microbiol. 5, 1–13 (2014).
Honda, T., Ni, Y. & Miwatani, T. Purification and characterization of a hemolysin produced by a clinical isolate of kanagawa phenomenon-negative Vibrio parahaemolyticus and related to the thermostable direct hemolysin. 56, 961–965 (1988).
Ottaviani, D. et al. Nontoxigenic Vibrio parahaemolyticus strains causing acute gastroenteritis. J. Clin. Microbiol. 50, 4141–4143 (2012).
Park, K.-S. et al. Functional characterization of two type III secretion systems of Vibrio parahaemolyticus. Infect. Immun. 72, 6659–6665 (2004).
Makino, K. et al. Genome sequence of Vibrio parahaemolyticus: a pathogenic mechanism distinct from that of V. cholerae. Lancet 361, 743–749 (2003). This first report of the whole genome of V. parahaemolyticus has been used as a reference in any further studies with the identification of the major pathogenic islands associated with virulence.
Ritchie, J. M. et al. Inflammation and disintegration of intestinal villi in an experimental model for Vibrio parahaemolyticus-induced diarrhea. PLoS Pathog. 8, e1002593 (2012).
Portaliou, A. G., Tsolis, K. C., Loos, M. S., Zorzini, V. & Economou, A. Type III Secretion: Building and Operating a Remarkable Nanomachine. Trends Biochem. Sci. 41, 175–189 (2016).
Hubbard, T. P. et al. Genetic analysis of Vibrio parahaemolyticus intestinal colonization. Proc. Natl Acad. Sci. USA 113, 6283–6288 (2016).
Wang, R. et al. The pathogenesis, detection, and prevention of Vibrio parahaemolyticus. Front. Microbiol. 6, 144 (2015).
US Food and Drug Administration. Quantitative Risk Assessment on the Public Health Impact of Pathogenic Vibrio parahaemolyticus in Raw Oysters. FDA (2005).
Simpson, L. M. & Oliver, J. D. Ability of Vibrio vulnificus to obtain iron from transferrin and other iron-binding proteins. Curr. Microbiol. 15, 155–157 (1987).
Arezes, J. et al. Hepcidin-induced hypoferremia is a critical host defense mechanism against the siderophilic bacterium Vibrio vulnificus. Cell Host Microbe 17, 47–57 (2015).
Payne, S. M., Mey, A. R. & Wyckoff, E. E. Vibrio iron transport: evolutionary adaptation to life in multiple environments. Microbiol. Mol. Biol. Rev. 80, 69–90 (2016).
Pajuelo, D. et al. Iron and Fur in the life cycle of the zoonotic pathogen Vibrio vulnificus. Environ. Microbiol. 18, 4005–4022 (2016).
Bahrani, K. J. D. O. Studies on the lipopolysaccharide of a virulent and an avirulent strain of Vibrio vulnificus. Biochem. Cell Biol. 68, 547–551 (1990).
Merkel, S. M., Alexander, S., Zufall, E., Oliver, J. D. & Huet-Hudson, Y. M. Essential role for estrogen in protection against Vibrio vulnificus-induced endotoxic shock. Infect. Immun. 69, 6119–6122 (2001).
Roig, F. J., González-Candelas, F. & Amaro, C. Domain organization and evolution of multifunctional autoprocessing repeats-in-toxin (MARTX) toxin in vibrio vulnificus. Appl. Environ. Microbiol. 77, 657–668 (2011).
Gavin, H. E., Beubier, N. T. & Satchell, K. J. F. The effector domain region of the Vibrio vulnificus MARTX toxin confers biphasic epithelial barrier disruption and is essential for systemic spread from the intestine. PLoS Pathog. 13, e1006119 (2017).
Jang, K. K. et al. Identification and characterization of Vibrio vulnificus plpA encoding a phospholipase A2 essential for pathogenesis. J. Biol. Chem. 292, 17129–17143 (2017).
Duong-Nu, T.-M. et al. All three TonB systems are required for Vibrio vulnificus CMCP6 tissue invasiveness by controlling flagellum expression. Infect. Immun. 84, 254–265 (2015).
Lee, S.-J. et al. VvpE mediates the intestinal colonization of Vibrio vulnificus by the disruption of tight junctions. Int. J. Med. Microbiol. 306, 10–19 (2016).
Jang, K. K., Gil, S. Y., Lim, J. G. & Choi, S. H. Regulatory characteristics of Vibrio vulnificus gbpA gene encoding a mucin-binding protein essential for pathogenesis. J. Biol. Chem. 291, 5774–5787 (2016).
Gauthier, J. D. et al. Role of GacA in virulence of Vibrio vulnificus. Microbiology 156, 3722–3733 (2010).
Rosche, T. M., Yano, Y. & Oliver, J. D. A rapid and simple PCR analysis indicates there are two subgroups of Vibrio vulnificus which correlate with clinical or environmental isolation. Microbiol. Immunol. 49, 381–389 (2005). This article describes a PCR method to rapidly differentiate the two genotypes of V. vulnificus and their correlation to isolation source.
Morrison, S. S. et al. Pyrosequencing-based comparative genome analysis of Vibrio vulnificus environmental isolates. PLoS One 7, e37553 (2012).
Gulig, P. A. et al. SOLiD sequencing of four Vibrio vulnificus genomes enables comparative genomic analysis and identification of candidate clade-specific virulence genes. BMC Genomics 11, 512 (2010).
Waldor, M. K. & Mekalanos, J. J. Lysogenic conversion by a filamentous phage encoding cholera toxin. Science 272, 1910–1914 (1996). This paper presents the first description of the structural genes for CT encoded by a filamentous bacteriophage.
Faruque, S. M. & Mekalanos, J. J. Pathogenicity islands and phages in Vibrio cholerae evolution. Trends Microbiol. 11, 505–510 (2003).
Meibom, K. L., Blokesch, M., Dolganov, N. A., Wu, C.-Y. & Schoolnik, G. K. Chitin induces natural competence in Vibrio cholerae. Science 310, 1824–1827 (2005). This study shows the crucial role of chitin in the acquisition of new genetic material via natural transformation; the role of chitin is crucial to understand the role of zooplankton in the evolution and life cycle of Vibrio spp.
Neiman, J., Guo, Y. & Rowe-Magnus, D. A. Chitin-induced carbotype conversion in Vibrio vulnificus. Infect. Immun. 79, 3195–3203 (2011).
Boyd, E. F. et al. Molecular analysis of the emergence of pandemic Vibrio parahaemolyticus. BMC Microbiol. 8, 110 (2008).
Liu, M. & Chen, S. A novel adhesive factor contributing to the virulence of Vibrio parahaemolyticus. Sci. Rep. 5, 14449 (2015).
World Health Organization. 10 facts on cholera. World Health Organization http://www.who.int/features/factfiles/cholera/en/ (2016).
Harris, J. B. et al. Susceptibility to Vibrio cholerae infection in a cohort of household contacts of patients with cholera in Bangladesh. PLoS Negl. Trop. Dis. 2, e221 (2008).
Qadri, F., Svennerholm, A.-M., Faruque, A. S. G. & Sack, R. B. Enterotoxigenic Escherichia coli in Developing Countries: Epidemiology, Microbiology, Clinical Features, Treatment, and Prevention. Clin. Microbiol. Rev. 18, 465–483 (2005).
Andrew Azman, S., Kara Rudolph, E. & Derek Cummings, A. T. J. L. The incubation period of cholera: A systematic review. J. Infect. 66, 432–438 (2013).
World Health Organization. Prevention and control of cholera outbreaks: WHO policy and recommendations. WHO http://www.who.int/cholera/prevention_control/recommendations/en/index5.html (2017).
World Health Organization. The Use of Cholera Rapid Diagnostic Tests — Interim Report. WHO (2016).
Mukherjee, P. et al. Evaluation of a rapid immunochromatographic dipstick kit for diagnosis of cholera emphasizes its outbreak utility. Jpn J. Infect. Dis. 63, 234–238 (2010).
Wang, X.-Y. et al. Field evaluation of a rapid immunochromatographic dipstick test for the diagnosis of cholera in a high-risk population. BMC Infect. Dis. 6, 17 (2006).
Dick, M. H., Guillerm, M., Moussy, F. & Chaignat, C. L. Review of two decades of Cholera diagnostics — how far have we really come? PLoS Negl. Trop. Dis. 6, e1845 (2012).
Centers for Disease Control. Vibrio species causing Vibriosis CDC (2017).
Høi, L., Dalsgaard, I. & Dalsgaard, A. Improved isolation of Vibrio vulnificus from seawater and sediment with cellobiose-colistin agar. 64, 1721–1724 (1998).
Hill, W. E. et al. Polymerase chain reaction identification of Vibrio vulnificus in artificially contaminated oysters. Appl. Environ. Microbiol. 57, 707–711 (1991).
Bej, A. K. et al. Detection of total and hemolysin producing Vibrio parahaemolyticus in shellfish using multiplex PCR amplification of tl, tdh, and trh. J. Microbiol. Methods 36, 215–225 (1999).
Chun, J., Huq, A. & Colwell, R. R. Analysis of 16S-23S rRNA intergenic spacer regions of Vibrio cholerae and Vibrio mimicus. Appl. Environ. Microbiol. 65, 2202–2208 (1999).
Nordstrom, J. L., Vickery, M. C. L., Blackstone, G. M., Murray, S. L. & DePaola, A. Development of a multiplex real-time PCR assay with an internal amplification control for the detection of total and pathogenic Vibrio parahaemolyticus bacteria in oysters. Appl. Environ. Microbiol. 73, 5840–5847 (2007).
Taiwo, M. et al. Comparison of toxR and tlh based PCR assays for Vibrio parahaemolyticus. Food Control 77, 116–120 (2017).
Campbell, M. S. & Wright, A. C. Real-time PCR analysis of Vibrio vulnificus from oysters. Appl. Environ. Microbiol. 69, 7137–7144 (2003).
Lyon, W. J. TaqMan, P. C. R. for detection of Vibrio cholerae O1, O139, non-O1, and non-O139 in pure cultures, raw oysters, and synthetic seawater. Appl. Environ. Microbiol. 67, 4685–4693 (2001).
Shirail, H. et al. Polymerase chain reaction for detection of the Cholera enterotoxin operon of Vibrio cholerae. J. Clin. Microbiol. 29, 2517–2521 (1991).
Roig, F. J., Sanjuan, E., Llorens, A. & Amaro, C. pilF Polymorphism-based PCR to distinguish Vibrio vulnificus strains potentially dangerous to public health. Appl. Environ. Microbiol. 76, 1328–1333 (2010).
Han, F. & Ge, B. Multiplex PCR assays for simultaneous detection and characterization of Vibrio vulnificus strains. Lett. Appl. Microbiol. 51, 234–240 (2010).
Myers, M. L., Panicker, G. & Bej, A. K. PCR detection of a newly emerged pandemic Vibrio parahaemolyticus O3: K6 pathogen in pure cultures and seeded waters from the Gulf of Mexico. Appl. Environ. Microbiol. 69, 2194–2200 (2003).
Whistler, C. A. et al. Use of whole-genome phylogeny and comparisons for development of a multiplex PCR assay to identify sequence type 36 Vibrio parahaemolyticus. J. Clin. Microbiol. 53, 1864–1872 (2015).
Martinez-Urtaza, J., Lozano-Leon, A., Viña-Feas, A., de Novoa, J. & Garcia-Martin, O. Differences in the API 20E biochemical patterns of clinical and environmental Vibrio parahaemolyticus isolates. FEMS Microbiol. Lett. 255, 75–81 (2006).
Croci, L. et al. Comparison of different biochemical and molecular methods for the identification of Vibrio parahaemolyticus. J. Appl. Microbiol. 102, 229–237 (2007).
George, C. M. et al. Randomized controlled trial of hospital-based hygiene and water treatment intervention (CHoBI7) to reduce Cholera. Emerg. Infect. Dis. 22, 233–241 (2016).
Sinclair, D., Abba, K., Zaman, K., Qadri, F. & Graves, P. M. Oral vaccines for preventing cholera. Cochrane Database Syst. Rev. 3, CD008603 (2011).
US Food and Drug Administration. VAXCHORA. FDA https://www.fda.gov/BiologicsBloodVaccines/Vaccines/ApprovedProducts/ucm505866.htm (2018).
Hsiao, A., Desai, S. N., Mogasale, V., Excler, J.-L. & Digilio, L. Lessons learnt from 12 oral cholera vaccine campaigns in resource-poor settings. Bull. World Health Organ. 95, 303–312 (2017).
Longini, I. M. et al. Controlling endemic cholera with oral vaccines. PLoS Med. 4, e336 (2007).
Anh, D. et al. Safety and immunogenicity of a reformulated Vietnamese bivalent killed, whole-cell, oral cholera vaccine in adults. Vaccines 25, 1149–1155 (2007).
Frew, S. E., Liu, V. Y. & Singer, P. A. A business plan to help the ‘global South’ in its fight against neglected diseases. Health Aff. (Millwood). 28, 1760–1773 (2009).
Levine, M. M. et al. PaxVax CVD 103-HgR single-dose live oral cholera vaccine. Expert Rev. Vaccines 16, 197–213 (2017).
Karlsson, S. L. et al. Development of stable Vibrio cholerae O1 Hikojima type vaccine strains co–expressing the Inaba and Ogawa lipopolysaccharide antigens. PLoS One 9, e108521 (2014).
World Health Organization. Immunisation standards: inactivated oral single dose vial. WHO http://www.who.int/immunization_standards/vaccine_quality/pq_298_euvichol_1dose_eubiologics/en/ (2017).
World Health Organization. Weekly epidemiological record. Weekly epidemiological record 92, 437–452 (2017).
World Health Organization. Weekly epidemiological record. Weekly epidemiological record 92, 301–320 (2017).
Khan, A. I. et al. Safety of the oral cholera vaccine in pregnancy: Retrospective findings from a subgroup following mass vaccination campaign in Dhaka. Bangladesh. Vaccine 35, 1538–1543 (2017).
Bhattacharya, S. K. et al. 5 year efficacy of a bivalent killed whole-cell oral cholera vaccine in Kolkata, India: a cluster-randomised, double-blind, placebo-controlled trial. Lancet Infect. Dis. 13, 1050–1056 (2013).
Qadri, F. et al. Efficacy of a single-dose, inactivated oral Cholera vaccine in Bangladesh. N. Engl. J. Med. 374, 1723–1732 (2016).
Vugia, D. J., Tabnak, F., Newton, A. E., Hernandez, M. & Griffin, P. M. Impact of 2003 State Regulation on Raw Oyster – associated Vibrio vulnificus Illnesses and Deaths, California, USA. Emerg. Infect. Dis. 19, 1276–1280 (2013).
Potasman, I., Paz, A. & Odeh, M. Infectious outbreaks associated with bivalve shellfish consumption: a worldwide perspective. Clin. Infect. Dis. 35, 921–928 (2002).
European Centre for Disease Prevention and Control. Vibrio Risk Portal. E3 Geoportal https://e3geoportal.ecdc.europa.eu/SitePages/Vibrio%20Map%20Viewer.aspx (2018).
Lee, T. H., Cha, S. S., Lee, C. S., Rhee, J. H. & Chung, K. M. Monoclonal antibodies against Vibrio vulnificus RtxA1 elicit protective immunity through distinct mechanisms. Infect. Immun. 82, 4813–4823 (2014).
Harris, J. B., LaRocque, R. C., Qadri, F., Ryan, E. T. & Calderwood, S. B. Cholera. Lancet 379, 2466–2476 (2012).
World Health Organization. Treatment Diarrhoea: Manual — A manual for Physicians Other Senior Health Workers. WHO (1990).
Alam, N. H. & Ashraf, H. Treatment of infectious diarrhea in children. Paediatr. Drugs 5, 151–165 (2003).
Ahmed, T. et al. Mortality in severely malnourished children with diarrhoea and use of a standardised management protocol. Lancet 353, 1919–1922 (1999).
Lindenbaum, J., Greenough, W. B. & Islam, M. R. Antibiotic therapy of Cholera in children. Bull. World Health Organ. 37, 529–538 (1967).
Bardhan, P. K. in Conn’s current therapy (eds Rakel, R. E. & Bope, E. T.) 18–24 (Saunders, 2005).
Munita, J. M. & Arias, C. A. Mechanisms of Antibiotic Resistance. Microbiol. Spectr. 4 (2016).
Kaushik, J. S., Gupta, P., Faridi, M. M. & Das, S. Single dose azithromycin versus ciprofloxacin for cholera in children: a randomized controlled trial. Indian Pediatr. 47, 309–315 (2010).
Roy, S. K. et al. Zinc supplementation in children with cholera in Bangladesh: randomised controlled trial. BMJ 336, 266–268 (2008).
World Health Organization WHO/Unicef joint statement: Clin. Management Acute Diarrhoea. WHO (2004).
Larson, C. P., Roy, S. K., Khan, A. I., Rahman, A. S. & Qadri, F. Zinc treatment to under-five children: applications to improve child survival and reduce burden of disease. J. Health. Popul. Nutr. 26, 356–365 (2008).
World Health Organization. Pocket book of hospital care for children. WHO (2013).
Ivers, L. C. Eliminating Cholera transmission in Haiti. N. Engl. J. Med. 376, 101–103 (2017).
World Health Organization. Situation Report — Cholera, Yemen. WHO (2017).
Yen, M., Cairns, L. S. & Camilli, A. A cocktail of three virulent bacteriophages prevents Vibrio cholerae infection in animal models. Nat. Commun. 8, 1–7 (2017).
Reilly, G. D. D., Reilly, C. A. A., Smith, E. G. G. & Baker-Austin, C. Vibrio alginolyticus-associated wound infection acquired in British waters, Guernsey, July 2011. Eurosurveillance 16, 3 (2011).
Klontz, K. C. et al. Syndromes of Vibrio vulnificus infections. Clinical and epidemiologic features in Florida cases, 1981–1987. Ann. Intern. Med. 109, 318–323 (1988).
Shaw, K. S. et al. Antimicrobial susceptibility of Vibrio vulnificus and Vibrio parahaemolyticus recovered from recreational and commercial areas of Chesapeake Bay and Maryland coastal bays. PLoS One 9, e89616 (2014).
Daniels, N. A. et al. Vibrio parahaemolyticus infections in the United States, 1973–1998. J. Infect. Dis. 181, 1661–1666 (2000).
Wong, K. C., Brown, A. M., Luscombe, G. M., Wong, S. J. & Mendis, K. Antibiotic use for Vibrio infections: important insights from surveillance data. BMC Infect. Dis. 15, 226 (2015).
Baker-Austin, C. et al. Antibiotic resistance in the shellfish pathogen Vibrio parahaemolyticus isolated from the coastal water and sediment of Georgia and SC. USA. J. Food Prot. 71, 2552–2558 (2008).
Baker-Austin, C. et al. Multi-site analysis reveals widespread antibiotic resistance in the marine pathogen Vibrio vulnificus. Microb. Ecol. 57, 151–159 (2009).
Monira, S. et al. Metagenomic profile of gut microbiota in children during cholera and recovery. Gut Pathog. 5, 1 (2013).
Monira, S. et al. Multi-drug resistant pathogenic bacteria in the gut of young children in Bangladesh. Gut Pathog. 9, 19 (2017).
Subramanian, S. et al. HHS Publ. Access. 510, 417–421 (2014).
Schaetti, C. et al. Costs of illness due to Cholera, costs of immunization and cost-effectiveness of an oral Cholera mass vaccination campaign in Zanzibar. PLoS Negl. Trop. Dis. 6, e1844 (2012).
Ralston, E. P., Kite-Powell, H. & Beet, A. An estimate of the cost of acute health effects from food- and water-borne marine pathogens and toxins in the USA. J. Water Health 9, 680–694 (2011).
Hendren, N., Sukumar, S. & Glazer, C. S. Vibrio vulnificus septic shock due to a contaminated tattoo. BMJ Case Rep. https://doi.org/10.1136/bcr-2017-220199 (2017).
Fraser, C. M. et al. DNA sequence of both chromosomes of the cholera pathogen Vibrio cholerae. Nature 406, 477–483 (2000). This article presents the first report of the genome sequence of the two chromosomes of V. cholerae, providing key insights to understand the evolution and virulence of this pathogen.
Mutreja, A. et al. Evidence for several waves of global transmission in the seventh cholera pandemic. Nature 477, 462–465 (2011). This study is the first to use whole-genome sequencing to elucidate the epidemiology and global dispersal of the seventh pandemic of V. cholerae.
Schaetti, C. et al. Comparing sociocultural features of cholera in three endemic African settings. BMC Med. 11, 206 (2013).
Sundaram, N. et al. Sociocultural determinants of anticipated oral cholera vaccine acceptance in three African settings: a meta-analytic approach. BMC Publ. Health 16, 1–11 (2016).
Jensen, Ma, Faruque, S. M., Mekalanos, J. J. & Levin, B. R. Modeling the role of bacteriophage in the control of cholera outbreaks. Proc. Natl Acad. Sci. USA 103, 4652–4657 (2006).
Lima, F. P. & Wethey, D. S. Three decades of high-resolution coastal sea surface temperatures reveal more than warming. Nat. Commun. 3, 704 (2012).
Vezzulli, L. et al. Long-term effects of ocean warming on the prokaryotic community: evidence from the vibrios. ISME J. 6, 21–30 (2012). This study shows the role of rapid climate warming on changing the abundance of Vibrio spp. in the marine environment using novel retrospective molecular methods.
Vezzulli, L. et al. Climate influence on Vibrio and associated human diseases during the past half-century in the coastal North Atlantic. Proc. Natl Acad. Sci. USA 113, E5062–E5071 (2016).
McLaughlin, J. B. et al. Outbreak of Vibrio parahaemolyticus gastroenteritis associated with Alaskan oysters. N. Engl. J. Med. 353, 1463–1470 (2005).
González-Escalona, N. et al. Vibrio parahaemolyticus Diarrhea, Chile, 1998 and 2004. Emerg. Infect. Dis. 11, 129–131 (2005).
Tatem, A. J., Rogers, D. J. & Hay, S. I. Global Transport Networks and Infectious Disease Spread. Adv. Parasitol. 52, 293–343 (2006).
Martinez-Urtaza, J. M. et al. Genomic variation and evolution of Vibrio parahaemolyticus ST36 over the course of a transcontinental epidemic expansion. mBio 8, e01425–17 (2017).
Rivera, I. N. G., Souza, K. M. C., Souza, C. P. & Lopes, R. M. Free-living and plankton-associated vibrios: assessment in ballast water, harbor areas, and coastal ecosystems in Brazil. Front. Microbiol. 3, 1–8 (2012).
McCarthy, S. A. & Khambaty, F. M. International dissemination of epidemic Vibrio cholerae by cargo ship ballast and other nonpotable waters. Appl. Environ. Microbiol. 60, 2597–2601 (1994). This study is the first to describe the role of cargo ships in the dispersal of pathogenic Vibrio spp. via discharges of ballast water.
Ruiz, G. M. et al. Global spread of microorganisms by ships. Nature 408, 49–50 (2000).
Jacobs, J., Moore, S. K., Kunkel, K. E. & Sun, L. A framework for examining climate-driven changes to the seasonality and geographical range of coastal pathogens and harmful algae. Clim. Risk Manag. 8, 16–27 (2015).
Schets, F. M., van den Berg, H. H. J. L., Marchese, A., Garbom, S. & de Roda Husman, A. M. Potentially human pathogenic vibrios in marine and fresh bathing waters related to environmental conditions and disease outcome. Int. J. Hyg. Environ. Health 214, 399–406 (2011).
Schets, F. M. et al. Vibrio alginolyticus infections in the Netherlands after swimming in the North Sea. Eurosurveillance 11, E061109.3 (2006).
Ramamurthy, T., Chowdhury, G., Pazhani, G. P. & Shinoda, S. Vibrio fluvialis: an emerging human pathogen. Front. Microbiol. 5, 91 (2014).
Igbinosa, E. O. & Okoh, A. I. Vibrio fluvialis: An unusual enteric pathogen of increasing public health concern. Int. J. Environ. Res. Publ. Health 7, 3628–3643 (2010).
Centers for Disease Control Cholera in Haiti. CDC https://www.cdc.gov/cholera/haiti/index.html#one (2017).
Chin, C.-S. et al. The Origin of the Haitian Cholera Outbreak Strain. N. Engl. J. Med. 364, 33–42 (2011).
Frerichs, R. R., Keim, P. S., Barrais, R. & Piarroux, R. Nepalese origin of cholera epidemic in Haiti. Clin. Microbiol. Infect. 18, E158–E163 (2012).
Alam, M. T. et al. Monitoring water sources for environmental reservoirs of toxigenic Vibrio cholerae O1. Haiti. Emerg. Infect. Dis. 20, 356–363 (2014).
Alam, M. T. et al. Increased isolation frequency of toxigenic Vibrio cholerae O1 from environmental monitoring sites in Haiti. PLoS One 10, e0124098 (2015).
Reen, F. J., Almagro-Moreno, S., Ussery, D. & Boyd, E. F. The genomic code: inferring Vibrionaceae niche specialization. Nat. Rev. Microbiol. 4, 697–704 (2006).
Alam, M. et al. Viable but nonculturable Vibrio cholerae O1 in biofilms in the aquatic environment and their role in cholera transmission. Proc. Natl Acad. Sci. USA 104, 17801–17806 (2007).
Sultana, M. et al. Biofilms Comprise a Component of the Annual Cycle of Vibrio cholerae in the Bay of Bengal Estuary. mBio 9, 1–13 (2018).
Gonzalez-Escalona, N. et al. Determination of molecular phylogenetics of Vibrio parahaemolyticus strains by multilocus sequence typing. J. Bacteriol. 190, 2831–2840 (2008).
Quilici, M.-L., Robert-Pillot, A., Picart, J. & Fournier, J.-M. Pandemic Vibrio parahaemolyticus O3:K6 spread, France. Emerg. Infect. Dis. 11, 1148–1149 (2005).
Martinez-Urtaza, J. et al. Characterization of pathogenic Vibrio parahaemolyticus isolates from clinical sources in Spain and comparison with Asian and North American pandemic isolates. J. Clin. Microbiol. 42, 4672–4678 (2004).
Ansaruzzaman, M. et al. Pandemic serovars (O3:K6 and O4:K68) of Vibrio parahaemolyticus associated with diarrhea in Mozambique: spread of the pandemic into the African continent. J. Clin. Microbiol. 43, 2559–2562 (2005).
Ottaviani, D. et al. First clinical report of pandemic Vibrio parahaemolyticus O3:K6 infection in Italy. J. Clin. Microbiol. 46, 2144–2145 (2008).
Centers for Disease Control and Prevention Preliminary Incidence and Trends of Infections with Pathogens Transmitted Commonly Through Food — Foodborne Diseases Active Surveillance Network, 10 U.S. Sites, 2006–2014. Morbidity and Mortality Weekly Report 64, 495–499 (2015).
Author information
Authors and Affiliations
Contributions
Introduction (C.B.-A.); Epidemiology (A.A., M.A. and J.M.-U.); Mechanisms/pathophysiology (J.D.O. and M.K.W.); Diagnosis, screening and prevention (J.D.O. and F.Q.); Management (J.D.O. and F.Q.); Quality of life (M.A. and C.B.-A.); Outlook (A.A., C.B.-A. and J.M.-U.); Overview of Primer (C.B.-A.).
Corresponding author
Ethics declarations
Competing interests
All authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Related link
WHO Global Health Observatory Map Gallery: http://gamapserver.who.int/mapLibrary/Files/Maps/Global_Cholera(WER)_2016.png
Rights and permissions
About this article
Cite this article
Baker-Austin, C., Oliver, J.D., Alam, M. et al. Vibrio spp. infections. Nat Rev Dis Primers 4, 1–19 (2018). https://doi.org/10.1038/s41572-018-0005-8
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41572-018-0005-8
This article is cited by
-
Whole genome sequence of Vibrio cholerae NB-183 isolated from freshwater in Ontario, Canada harbors a unique gene repertoire
BMC Genomic Data (2024)
-
Recovering high-quality bacterial genomes from cross-contaminated cultures: a case study of marine Vibrio campbellii
BMC Genomics (2024)
-
Evaluation of a novel lysis-based sample processing method to optimize Vibrio vulnificus detecting by loop-mediated isothermal amplification assay
BMC Microbiology (2024)
-
Rapid visual nucleic acid detection of Vibrio alginolyticus by recombinase polymerase amplification combined with CRISPR/Cas13a
World Journal of Microbiology and Biotechnology (2024)
-
Synthesis and Anti-VIBRIO Activity of Gallic Acid Derivatives Containing Thiosemicarbazide
Chemistry of Natural Compounds (2024)