Abstract
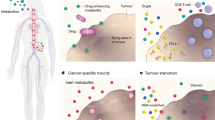
The way cancer cells utilize nutrients to support their growth and proliferation is determined by cancer cell-intrinsic and cancer cell-extrinsic factors, including interactions with the environment. These interactions can define therapeutic vulnerabilities and impact the effectiveness of cancer therapy. Diet-mediated changes in whole-body metabolism and systemic nutrient availability can affect the environment that cancer cells are exposed to within tumours, and a better understanding of how diet modulates nutrient availability and utilization by cancer cells is needed. How diet impacts cancer outcomes is also of great interest to patients, yet clear evidence for how diet interacts with therapy and impacts tumour growth is lacking. Here we propose an experimental framework to probe the connections between diet and cancer metabolism. We examine how dietary factors may affect tumour growth by altering the access to and utilization of nutrients by cancer cells. Our growing understanding of how certain cancer types respond to various diets, how diet impacts cancer cell metabolism to mediate these responses and whether dietary interventions may constitute new therapeutic opportunities will begin to provide guidance on how best to use diet and nutrition to manage cancer in patients.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$29.99 / 30 days
cancel any time
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
References
Vander Heiden, M. G. & DeBerardinis, R. J. Understanding the intersections between metabolism and cancer biology. Cell 168, 657–669 (2017).
Luengo, A., Gui, D. Y. & Vander Heiden, M. G. Targeting metabolism for cancer therapy. Cell Chem. Biol. 24, 1161–1180 (2017).
Davidson, S. M. et al. Environment impacts the metabolic dependencies of Ras-driven non-small cell lung cancer. Cell Metab. 23, 517–528 (2016).
Gui, D. Y. et al. Environment dictates dependence on mitochondrial complex I for NAD+ and aspartate production and determines cancer cell sensitivity to metformin. Cell Metab. 24, 716–727 (2016).
Mayers, J. R. et al. Tissue of origin dictates branched-chain amino acid metabolism in mutant Kras-driven cancers. Science 353, 1161–1165 (2016).
Muir, A. et al. Environmental cystine drives glutamine anaplerosis and sensitizes cancer cells to glutaminase inhibition. Elife 6, e27713 (2017).
Cantor, J. R. et al. Physiologic medium rewires cellular metabolism and reveals uric acid as an endogenous inhibitor of ump synthase. Cell 169, 258–272.e17 (2017).
Vande Voorde, J. et al. Improving the metabolic fidelity of cancer models with a physiological cell culture medium. Sci. Adv. 5, eaau7314 (2019).
Muir, A., Danai, L. V. & Vander Heiden, M. G. Microenvironmental regulation of cancer Cell Metab.olism: implications for experimental design and translational studies. Dis Model. Mech 11, (2018).
Maddocks, O. D. K. et al. Modulating the therapeutic response of tumours to dietary serine and glycine starvation. Nature 544, 372–376 (2017).
Sullivan, M. R. et al. Quantification of microenvironmental metabolites in murine cancers reveals determinants of tumor nutrient availability. Elife 8, e44235 (2019).
Mayne, S. T., Playdon, M. C. & Rock, C. L. Diet, nutrition, and cancer: past, present and future. Nat. Rev. Clin. Oncol. 13, 504–515 (2016).
Khandekar, M. J., Cohen, P. & Spiegelman, B. M. Molecular mechanisms of cancer development in obesity. Nat. Rev. Cancer 11, 886–895 (2011).
Kitahara, C. M. et al. Prospective investigation of body mass index, colorectal adenoma, and colorectal cancer in the prostate, lung, colorectal, and ovarian cancer screening trial. J. Clin. Oncol. 31, 2450–2459 (2013).
Meynet, O. & Ricci, J.-E. Caloric restriction and cancer: molecular mechanisms and clinical implications. Trends Mol. Med. 20, 419–427 (2014).
Michels, K. B. & Ekbom, A. Caloric restriction and incidence of breast cancer. JAMA 291, 1226–1230 (2004).
World Cancer Research Fund/American Institute for Cancer Research. Food, nutrition, physical activity, and the prevention of cancer: a global perspective. American Institute for Cancer Research http://www.aicr.org/assets/docs/pdf/reports/Second_Expert_Report.pdf (2007).
Kushi, L. H. et al. American cancer society guidelines on nutrition and physical activity for cancer prevention: reducing the risk of cancer with healthy food choices and physical activity. CA Cancer J. Clin. 62, 30–67 (2012).
Kalaany, N. Y. & Sabatini, D. M. Tumours with PI3K activation are resistant to dietary restriction. Nature 458, 725–731 (2009).
Hopkins, B. D. et al. Suppression of insulin feedback enhances the efficacy of PI3K inhibitors. Nature 560, 499–503 (2018).
Nogueira, L. M. et al. Dose-dependent effects of calorie restriction on gene expression, metabolism, and tumor progression are partially mediated by insulin-like growth factor-1. Cancer Med. 1, 275–288 (2012).
Lu, Z. et al. Fasting selectively blocks development of acute lymphoblastic leukemia via leptin-receptor upregulation. Nat. Med. 23, 79–90 (2017).
Beyaz, S. et al. High-fat diet enhances stemness and tumorigenicity of intestinal progenitors. Nature 531, 53–58 (2016).
Hursting, S. D., Dunlap, S. M., Ford, N. A., Hursting, M. J. & Lashinger, L. M. Calorie restriction and cancer prevention: a mechanistic perspective. Cancer Metab. 1, 10 (2013).
Lee, C. & Longo, V. D. Fasting vs dietary restriction in cellular protection and cancer treatment: from model organisms to patients. Oncogene 30, 3305–3316 (2011).
Lv, M., Zhu, X., Wang, H., Wang, F. & Guan, W. Roles of caloric restriction, ketogenic diet and intermittent fasting during initiation, progression and metastasis of cancer in animal models: a systematic review and meta-analysis. PLOS ONE 9, e115147 (2014).
De Lorenzo, M. S. et al. Caloric restriction reduces growth of mammary tumors and metastases. Carcinogenesis 32, 1381–1387 (2011).
Nogueira, L. M., Dunlap, S. M., Ford, N. A. & Hursting, S. D. Calorie restriction and rapamycin inhibit MMTV-Wnt-1 mammary tumor growth in a mouse model of postmenopausal obesity. Endocr. Relat. Cancer 19, 57–68 (2012).
Curry, N. L. et al. Pten-null tumors cohabiting the same lung display differential AKT activation and sensitivity to dietary restriction. Cancer Discov. 3, 908–921 (2013).
Lanza-Jacoby, S. et al. Calorie restriction delays the progression of lesions to pancreatic cancer in the LSL-KrasG12D; Pdx-1/Cre mouse model of pancreatic cancer. Exp. Biol. Med. (Maywood) 238, 787–797 (2013).
Mukherjee, P., Abate, L. E. & Seyfried, T. N. Antiangiogenic and proapoptotic effects of dietary restriction on experimental mouse and human brain tumors. Clin. Cancer Res. 10, 5622–5629 (2004).
Shelton, L. M., Huysentruyt, L. C., Mukherjee, P. & Seyfried, T. N. Calorie restriction as an anti-invasive therapy for malignant brain cancer in the VM mouse. ASN Neuro. 2, e00038 (2010).
Danai, L. V. et al. Altered exocrine function can drive adipose wasting in early pancreatic cancer. Nature 558, 600–604 (2018).
Algire, C., Amrein, L., Zakikhani, M., Panasci, L. & Pollak, M. Metformin blocks the stimulative effect of a high-energy diet on colon carcinoma growth in vivo and is associated with reduced expression of fatty acid synthase. Endocr. Relat. Cancer 17, 351–360 (2010).
O’Neill, A. M. et al. High-fat Western diet-induced obesity contributes to increased tumor growth in mouse models of human colon cancer. Nutr. Res. 36, 1325–1334 (2016).
Schulz, M. D. et al. High-fat-diet-mediated dysbiosis promotes intestinal carcinogenesis independently of obesity. Nature 514, 508–512 (2014).
Chang, H. H. et al. Incidence of pancreatic cancer is dramatically increased by a high fat, high calorie diet in KrasG12D mice. PLOS ONE 12, e0184455 (2017).
Nadella, S. et al. Dietary fat stimulates pancreatic cancer growth and promotes fibrosis of the tumor microenvironment through the cholecystokinin receptor. Am. J. Physiol. Gastrointest Liver Physiol. 315, G699–G712 (2018).
Okumura, T. et al. Extra-pancreatic invasion induces lipolytic and fibrotic changes in the adipose microenvironment, with released fatty acids enhancing the invasiveness of pancreatic cancer cells. Oncotarget 8, 18280–18295 (2017).
Philip, B. et al. A high-fat diet activates oncogenic Kras and COX2 to induce development of pancreatic ductal adenocarcinoma in mice. Gastroenterology 145, 1449–1458 (2013).
Huang, M. et al. Diet-induced alteration of fatty acid synthase in prostate cancer progression. Oncogenesis 5, e195 (2016).
Kim, S. et al. Myristoylation of Src kinase mediates Src-induced and high-fat diet-accelerated prostate tumor progression in mice. J. Biol. Chem. 292, 18422–18433 (2017).
Sundaram, S. & Yan, L. High-fat diet enhances mammary tumorigenesis and pulmonary metastasis and alters inflammatory and angiogenic profiles in MMTV-PyMT Mice. AntiCancer Res. 36, 6279–6287 (2016).
Ip, B. C., Liu, C., Smith, D. E., Ausman, L. M. & Wang, X. D. High-refined-carbohydrate and high-fat diets induce comparable hepatic tumorigenesis in male mice. J. Nutr. 144, 647–653 (2014).
Maddocks, O. D. et al. Serine starvation induces stress and p53-dependent metabolic remodelling in cancer cells. Nature 493, 542–546 (2013).
Sullivan, M. R. et al. Increased serine synthesis provides an advantage for tumors arising in tissues where serine levels are limiting. Cell Metab. 29, 1410–1421 (2019).
Breillout, F., Hadida, F., Echinard-Garin, P., Lascaux, V. & Poupon, M. F. Decreased rat rhabdomyosarcoma pulmonary metastases in response to a low methionine diet. AntiCancer Res. 7, 861–867 (1987).
Guo, H. et al. Therapeutic tumor-specific cell cycle block induced by methionine starvation in vivo. Cancer Res. 53, 5676–5679 (1993).
Hoshiya, Y. et al. Human tumors are methionine dependent in vivo. AntiCancer Res. 15, 717–718 (1995).
Komninou, D., Leutzinger, Y., Reddy, B. S. & Richie, J. P. J. Methionine restriction inhibits colon carcinogenesis. Nutr. Cancer 54, 202–208 (2006).
Gao, X. et al. Dietary methionine influences therapy in mouse cancer models and alters human metabolism. Nature https://doi.org/10.1038/s41586-019-1437-3 (2019).
Stafford, P. et al. The ketogenic diet reverses gene expression patterns and reduces reactive oxygen species levels when used as an adjuvant therapy for glioma. Nutr. Metab. (Lond) 7, 74 (2010).
Abdelwahab, M. G. et al. The ketogenic diet is an effective adjuvant to radiation therapy for the treatment of malignant glioma. PLOS ONE 7, e36197 (2012).
Poff, A. M., Ari, C., Seyfried, T. N. & D’Agostino, D. P. The ketogenic diet and hyperbaric oxygen therapy prolong survival in mice with systemic metastatic cancer. PLOS ONE 8, e65522 (2013).
Freedland, S. J. et al. Carbohydrate restriction, prostate cancer growth, and the insulin-like growth factor axis. Prostate 68, 11–19 (2008).
Mavropoulos, J. C. et al. The effects of varying dietary carbohydrate and fat content on survival in a murine LNCaP prostate cancer xenograft model. Cancer Prev. Res. (Phila) 2, 557–565 (2009).
Otto, C. et al. Growth of human gastric cancer cells in nude mice is delayed by a ketogenic diet supplemented with omega-3 fatty acids and medium-chain triglycerides. BMC Cancer 8, 122 (2008).
Liśkiewicz, A. D. et al. Long-term high fat ketogenic diet promotes renal tumor growth in a rat model of tuberous sclerosis. Sci. Rep. 6, 21807 (2016).
Xia, S. et al. Prevention of dietary-fat-fueled ketogenesis attenuates BRAF V600E tumor growth. Cell Metab. 25, 358–373 (2017).
Kang, H. B. et al. Metabolic rewiring by oncogenic BRAF V600E links ketogenesis pathway to BRAF-MEK1 signaling. Mol. Cell 59, 345–358 (2015).
Morscher, R. J. et al. Inhibition of neuroblastoma tumor growth by ketogenic diet and/or calorie restriction in a CD1-nu mouse model. PLOS ONE 10, e0129802 (2015).
Woolf, E. C., Syed, N. & Scheck, A. C. Tumor metabolism, the ketogenic diet and β-hydroxybutyrate: novel approaches to adjuvant brain tumor therapy. Front. Mol. Neurosci. 9, 122 (2016).
Zhou, W. et al. The calorically restricted ketogenic diet, an effective alternative therapy for malignant brain cancer. Nutr. Metab. (Lond) 4, 5 (2007).
Seyfried, T. N., Sanderson, T. M., El-Abbadi, M. M., McGowan, R. & Mukherjee, P. Role of glucose and ketone bodies in the metabolic control of experimental brain cancer. Br. J. Cancer. 89, 1375–1382 (2003).
Maurer, G. D. et al. Differential utilization of ketone bodies by neurons and glioma cell lines: a rationale for ketogenic diet as experimental glioma therapy. BMC Cancer 11, 315 (2011).
Shukla, S. K. et al. Metabolic reprogramming induced by ketone bodies diminishes pancreatic cancer cachexia. Cancer Metab. 2, 18 (2014).
Wheatley, K. E. et al. Low-carbohydrate diet versus caloric restriction: effects on weight loss, hormones, and colon tumor growth in obese mice. Nutr. Cancer 60, 61–68 (2008).
Allen, B. G. et al. Ketogenic diets enhance oxidative stress and radio-chemo-therapy responses in lung cancer xenografts. Clin. Cancer Res. 19, 3905–3913 (2013).
Pascual, G. et al. Targeting metastasis-initiating cells through the fatty acid receptor CD36. Nature 541, 41–45 (2017).
Chen, M. et al. An aberrant SREBP-dependent lipogenic program promotes metastatic prostate cancer. Nat. Genet. 50, 206–218 (2018).
Knott, S. R. V. et al. Asparagine bioavailability governs metastasis in a model of breast cancer. Nature 554, 378–381 (2018).
Patti, G. J., Yanes, O. & Siuzdak, G. Innovation: metabolomics: the apogee of the omics trilogy. Nat. Rev. Mol. Cell Biol. 13, 263–269 (2012).
Collet, T. H. et al. A metabolomic signature of acute caloric restriction. J. Clin. Endocrinol. Metab. 102, 4486–4495 (2017).
Margolis, L. M. et al. Calorie restricted high protein diets downregulate lipogenesis and lower intrahepatic triglyceride concentrations in male rats. Nutrients 8, E571 (2016).
Miller, K. N. et al. Aging and caloric restriction impact adipose tissue, adiponectin, and circulating lipids. Aging Cell 16, 497–507 (2017).
Selman, C. et al. Coordinated multitissue transcriptional and plasma metabonomic profiles following acute caloric restriction in mice. Physiol. Genomics 27, 187–200 (2006).
Raeini-Sarjaz, M., Vanstone, C. A., Papamandjaris, A. A., Wykes, L. J. & Jones, P. J. Comparison of the effect of dietary fat restriction with that of energy restriction on human lipid metabolism. Am. J. Clin. Nutr. 73, 262–267 (2001).
Appel, L. J. et al. Effects of protein, monounsaturated fat, and carbohydrate intake on blood pressure and serum lipids: results of the OmniHeart randomized trial. JAMA 294, 2455–2464 (2005).
Ma, Y. et al. Association between carbohydrate intake and serum lipids. J. Am. Coll. Nutr. 25, 155–163 (2006).
Kennedy, A. R. et al. A high-fat, ketogenic diet induces a unique metabolic state in mice. Am. J. Physiol. Endocrinol. Metab. 292, E1724–E1739 (2007).
Douris, N. et al. Adaptive changes in amino acid metabolism permit normal longevity in mice consuming a low-carbohydrate ketogenic diet. Biochim. Biophys. Acta. 1852, 2056–2065 (2015).
Heischmann, S. et al. Regulation of kynurenine metabolism by a ketogenic diet. J. Lipid Res. 59, 958–966 (2018).
Fujisaka, S. et al. Diet, genetics, and the gut microbiome drive dynamic changes in plasma metabolites. Cell Rep. 22, 3072–3086 (2018).
Wang, W. et al. Effects of high-fat diet on plasma profiles of eicosanoid metabolites in mice. Prostaglandins Other Lipid Mediat. 127, 9–13 (2016).
Sansbury, B. E., Bhatnagar, A. & Hill, B. G. Impact of nutrient excess and endothelial nitric oxide synthase on the plasma metabolite profile in mice. Front. Physiol. 5, 453 (2014).
Lai, Y. S. et al. Mass-spectrometry-based serum metabolomics of a c57bl/6j mouse model of high-fat-diet-induced non-alcoholic fatty liver disease development. J. Agric Food Chem. 63, 7873–7884 (2015).
Stone, K. P. et al. Compromised responses to dietary methionine restriction in adipose tissue but not liver of ob/ob mice. Obesity (Silver Spring) 23, 1836–1844 (2015).
Kokkinakis, D. M., Schold, S. C. J., Hori, H. & Nobori, T. Effect of long-term depletion of plasma methionine on the growth and survival of human brain tumor xenografts in athymic mice. Nutr. Cancer 29, 195–204 (1997).
Lees, E. K. et al. Direct comparison of methionine restriction with leucine restriction on the metabolic health of C57BL/6J mice. Sci. Rep. 7, 9977 (2017).
Elshorbagy, A. K. et al. Cysteine supplementation reverses methionine restriction effects on rat adiposity: significance of stearoyl-coenzyme A desaturase. J. Lipid Res. 52, 104–112 (2011).
Huang, T. H. et al. A methionine-restricted diet and endurance exercise decrease bone mass and extrinsic strength but increase intrinsic strength in growing male rats. J. Nutr. 144, 621–630 (2014).
Fukumura, D., Duda, D. G., Munn, L. L. & Jain, R. K. Tumor microvasculature and microenvironment: novel insights through intravital imaging in pre-clinical models. Microcirculation 17, 206–225 (2010).
Pan, M. et al. Regional glutamine deficiency in tumours promotes dedifferentiation through inhibition of histone demethylation. Nat. Cell Biol. 18, 1090–1101 (2016).
Wiig, H. & Swartz, M. A. Interstitial fluid and lymph formation and transport: physiological regulation and roles in inflammation and cancer. Physiol. Rev. 92, 1005–1060 (2012).
Wiig, H., Aukland, K. & Tenstad, O. Isolation of interstitial fluid from rat mammary tumors by a centrifugation method. Am. J. Physiol. Heart Circ. Physiol. 284, H416–H424 (2003).
Haslene-Hox, H. et al. A new method for isolation of interstitial fluid from human solid tumors applied to proteomic analysis of ovarian carcinoma tissue. PLOS ONE 6, e19217 (2011).
Ho, P. C. et al. Phosphoenolpyruvate is a metabolic checkpoint of anti-tumor T Cell Res.ponses. Cell 162, 1217–1228 (2015).
Burgess, E. A. & Sylven, B. Glucose, lactate, and lactic dehydrogenase activity in normal interstitial fluid and that of solid mouse tumors. Cancer Res. 22, 581–588 (1962).
Gullino, P. M., Clark, S. H. & Grantham, F. H. The interstitial fluid of solid tumors. Cancer Res. 24, 780–794 (1964).
Hensley, C. T. et al. Metabolic heterogeneity in human lung tumors. Cell 164, 681–694 (2016).
Poff, A. M., Ari, C., Arnold, P., Seyfried, T. N. & D’Agostino, D. P. Ketone supplementation decreases tumor cell viability and prolongs survival of mice with metastatic cancer. Int. J. Cancer 135, 1711–1720 (2014).
Birsoy, K. et al. Metabolic determinants of cancer cell sensitivity to glucose limitation and biguanides. Nature 508, 108–112 (2014).
Schwarz, J. M., Linfoot, P., Dare, D. & Aghajanian, K. Hepatic de novo lipogenesis in normoinsulinemic and hyperinsulinemic subjects consuming high-fat, low-carbohydrate and low-fat, high-carbohydrate isoenergetic diets. Am. J. Clin. Nutr. 77, 43–50 (2003).
Ikemoto, S. et al. High-fat diet-induced hyperglycemia and obesity in mice: differential effects of dietary oils. Metabolism 45, 1539–1546 (1996).
Jang, C. et al. The small intestine converts dietary fructose into glucose and organic acids. Cell Metab. 27, 351–361.e3 (2018).
Balakumar, M. et al. High-fructose diet is as detrimental as high-fat diet in the induction of insulin resistance and diabetes mediated by hepatic/pancreatic endoplasmic reticulum (ER) stress. Mol. Cell Biochem. 423, 93–104 (2016).
Goncalves, M. D. et al. High-fructose corn syrup enhances intestinal tumor growth in mice. Science 363, 1345–1349 (2019).
Hensley, C. T., Wasti, A. T. & DeBerardinis, R. J. Glutamine and cancer: cell biology, physiology, and clinical opportunities. J. Clin. Invest. 123, 3678–3684 (2013).
Sellers, K. et al. Pyruvate carboxylase is critical for non-small-cell lung cancer proliferation. J. Clin. Invest. 125, 687–698 (2015).
Tardito, S. et al. Glutamine synthetase activity fuels nucleotide biosynthesis and supports growth of glutamine-restricted glioblastoma. Nat. Cell Biol. 17, 1556–1568 (2015).
Raffaghello, L. et al. Starvation-dependent differential stress resistance protects normal but not cancer cells against high-dose chemotherapy. Proc. Natl Acad. Sci. USA 105, 8215–8220 (2008).
Schroll, M. M., Liu, X., Herzog, S. K., Skube, S. B. & Hummon, A. B. Nutrient restriction of glucose or serum results in similar proteomic expression changes in 3D colon cancer cell cultures. Nutr. Res. 36, 1068–1080 (2016).
Lashinger, L. M. et al. Starving cancer from the outside and inside: separate and combined effects of calorie restriction and autophagy inhibition on Ras-driven tumors. Cancer Metab. 4, 18 (2016).
Bianchi, G. et al. Fasting induces anti-Warburg effect that increases respiration but reduces atp-synthesis to promote apoptosis in colon cancer models. Oncotarget 6, 11806–11819 (2015).
Zhang, J. et al. Low ketolytic enzyme levels in tumors predict ketogenic diet responses in cancer cell lines in vitro and in vivo. J. Lipid Res. 59, 625–634 (2018).
Huang, D. et al. Hepatocellular carcinoma redirects to ketolysis for progression under nutrition deprivation stress. Cell Res. 26, 1112–1130 (2016).
Buescher, J. M. et al. A roadmap for interpreting 13C metabolite labeling patterns from cells. Curr. Opin. Biotechnol. 34, 189–201 (2015).
Chong, J. et al. MetaboAnalyst 4.0: towards more transparent and integrative metabolomics analysis. Nucleic Acids Res. 46, W486–W494 (2018).
Sergushichev, A. A. et al. GAM: a web-service for integrated transcriptional and metabolic network analysis. Nucleic Acids Res. 44, W194–W200 (2016).
Hui, S. et al. Glucose feeds the TCA cycle via circulating lactate. Nature 551, 115–118 (2017).
Valkenburg, K. C., de Groot, A. E. & Pienta, K. J. Targeting the tumour stroma to improve cancer therapy. Nat. Rev. Clin. Oncol. 15, 366–381 (2018).
Lyssiotis, C. A. & Kimmelman, A. C. Metabolic interactions in the tumor microenvironment. Trends Cell Biol. 27, 863–875 (2017).
Ying, M., Guo, C. & Hu, X. The quantitative relationship between isotopic and net contributions of lactate and glucose to the TCA cycle. J. Biol. Chem. 294, 9615–9630 (2019).
Timmers, S. et al. Calorie restriction-like effects of 30 days of resveratrol supplementation on energy metabolism and metabolic profile in obese humans. Cell Metab. 14, 612–622 (2011).
Pernicova, I. & Korbonits, M. Metformin–mode of action and clinical implications for diabetes and cancer. Nat. Rev. Endocrinol. 10, 143–156 (2014).
Fang, Y. et al. Duration of rapamycin treatment has differential effects on metabolism in mice. Cell Metab. 17, 456–462 (2013).
Ohe, K., Morris, H. P. & Weinhouse, S. Beta-hydroxybutyrate dehydrogenase activity in liver and liver tumors. Cancer Res. 27, 1360–1371 (1967).
Tisdale, M. J. & Brennan, R. A. Loss of acetoacetate coenzyme A transferase activity in tumours of peripheral tissues. Br. J. Cancer. 47, 293–297 (1983).
Patel, M. S., Russell, J. J. & Gershman, H. Ketone-body metabolism in glioma and neuroblastoma cells. Proc. Natl Acad. Sci. USA 78, 7214–7218 (1981).
Magee, B. A., Potezny, N., Rofe, A. M. & Conyers, R. A. The inhibition of malignant cell growth by ketone bodies. Aust. J. Exp. Biol. Med. Sci. 57, 529–539 (1979).
Rodrigues, L. M. et al. The action of β-hydroxybutyrate on the growth, metabolism and global histone H3 acetylation of spontaneous mouse mammary tumours: evidence of a β-hydroxybutyrate paradox. Cancer Metab. 5, 4 (2017).
Xu, X. et al. Overview of the development of glutaminase inhibitors: achievements and future directions. J. Med. Chem. 62, 1096–1115 (2019).
Lien, E. C., Lyssiotis, C. A. & Cantley, L. C. Metabolic reprogramming by the PI3K-Akt-mTOR pathway in cancer. Recent Results Cancer Res. 207, 39–72 (2016).
Kanarek, N. et al. Histidine catabolism is a major determinant of methotrexate sensitivity. Nature 559, 632–636 (2018).
Huennekens, F. M. The methotrexate story: a paradigm for development of cancer chemotherapeutic agents. Adv. Enzyme Regul. 34, 397–419 (1994).
Nencioni, A., Caffa, I., Cortellino, S. & Longo, V. D. Fasting and cancer: molecular mechanisms and clinical application. Nat. Rev. Cancer 18, 707–719 (2018).
Hoshiya, Y., Kubota, T., Matsuzaki, S. W., Kitajima, M. & Hoffman, R. M. Methionine starvation modulates the efficacy of cisplatin on human breast cancer in nude mice. AntiCancer Res. 16, 3515–3517 (1996).
Poirson-Bichat, F., Gonçalves, R. A., Miccoli, L., Dutrillaux, B. & Poupon, M. F. Methionine depletion enhances the antitumoral efficacy of cytotoxic agents in drug-resistant human tumor xenografts. Clin. Cancer Res. 6, 643–653 (2000).
Lee, C. et al. Fasting cycles retard growth of tumors and sensitize a range of cancer cell types to chemotherapy. Sci. Transl. Med. 4, 124ra27 (2012).
de Groot, S. et al. The effects of short-term fasting on tolerance to (neo) adjuvant chemotherapy in HER2-negative breast cancer patients: a randomized pilot study. BMC Cancer 15, 652 (2015).
Dorff, T. B. et al. Safety and feasibility of fasting in combination with platinum-based chemotherapy. BMC Cancer 16, 360 (2016).
Safdie, F. M. et al. Fasting and cancer treatment in humans: a case series report. Aging (Albany NY) 1, 988–1007 (2009).
Bauersfeld, S. P. et al. The effects of short-term fasting on quality of life and tolerance to chemotherapy in patients with breast and ovarian cancer: a randomized cross-over pilot study. BMC Cancer 18, 476 (2018).
Hoffman, R. M. Clinical studies of methionine-restricted diets for cancer patients. Methods Mol. Biol. 1866, 95–105 (2019).
Thivat, E. et al. Phase II trial of the association of a methionine-free diet with cystemustine therapy in melanoma and glioma. AntiCancer Res. 29, 5235–5240 (2009).
Durando, X. et al. Dietary methionine restriction with FOLFOX regimen as first line therapy of metastatic colorectal cancer: a feasibility study. Oncol. 78, 205–209 (2010).
Di Biase, S. et al. Fasting regulates EGR1 and protects from glucose- and dexamethasone-dependent sensitization to chemotherapy. PLOS Biol. 15, e2001951 (2017).
Obrist, F. et al. Metabolic vulnerability of cisplatin-resistant cancers. EMBO J. 37, e98597 (2018).
Gravel, S. P. et al. Serine deprivation enhances antineoplastic activity of biguanides. Cancer Res. 74, 7521–7533 (2014).
Ricci, M. R. & Ulman, E. A. Laboratory animal diets: a critical part of your in vivo research. Research Diets https://researchdiets.com/system/resources/W1siZiIsIjIwMTgvMDMvMjkvNzF0NjQ5OXcwZl9MYWJvcmF0b3J5X0FuaW1hbF9EaWV0c19fQV9Dcml0aWNhbF9QYXJ0X29mX3lvdXJfSW5fdml2b19SZXNlYXJjaF93ZWIucGRmIl1d/Laboratory_Animal_Diets_%20A_Critical_Part_of_your_In_vivo_Research_web.pdf (2005).
Chen, Y. et al. The influence of dietary lipid composition on liver mitochondria from mice following 1 month of calorie restriction. BioSci. Rep. 33, 83–95 (2012).
Abbott, S. K., Else, P. L., Atkins, T. A. & Hulbert, A. J. Fatty acid composition of membrane bilayers: importance of diet polyunsaturated fat balance. Biochim. Biophys. Acta. 1818, 1309–1317 (2012).
Tosi, F., Sartori, F., Guarini, P., Olivieri, O. & Martinelli, N. Delta-5 and delta-6 desaturases: crucial enzymes in polyunsaturated fatty acid-related pathways with pleiotropic influences in health and disease. Adv. Exp. Med. Biol. 824, 61–81 (2014).
Ackerman, D. et al. triglycerides promote lipid homeostasis during hypoxic stress by balancing fatty acid saturation. Cell Rep. 24, 2596–2605.e5 (2018).
Kamphorst, J. J. et al. Hypoxic and Ras-transformed cells support growth by scavenging unsaturated fatty acids from lysophospholipids. Proc. Natl Acad. Sci. USA 110, 8882–8887 (2013).
Serini, S., Piccioni, E., Merendino, N. & Calviello, G. Dietary polyunsaturated fatty acids as inducers of apoptosis: implications for cancer. Apoptosis 14, 135–152 (2009).
Roongta, U. V. et al. Cancer cell dependence on unsaturated fatty acids implicates stearoyl-CoA desaturase as a target for cancer therapy. Mol. Cancer Res. 9, 1551–1561 (2011).
Peck, B. et al. Inhibition of fatty acid desaturation is detrimental to cancer cell survival in metabolically compromised environments. Cancer Metab. 4, 6 (2016).
Peck, B. & Schulze, A. Lipid desaturation - the next step in targeting lipogenesis in cancer. FEBS J. 283, 2767–2778 (2016).
Reeves, P. G., Nielsen, F. H. & Fahey, G. C. AIN-93 purified diets for laboratory rodents: final report of the American Institute of Nutrition ad hoc writing committee on the reformulation of the AIN-76A rodent diet. J. Nutr. 123, 1939–1951 (1993).
Ellacott, K. L., Morton, G. J., Woods, S. C., Tso, P. & Schwartz, M. W. Assessment of feeding behavior in laboratory mice. Cell Metab. 12, 10–17 (2010).
Pugh, T. D., Klopp, R. G. & Weindruch, R. Controlling caloric consumption: protocols for rodents and rhesus monkeys. Neurobiol. Aging 20, 157–165 (1999).
Acknowledgements
The authors thank members of the Vander Heiden laboratory for thoughtful discussions and comments on the manuscript. E.C.L. is a Damon Runyon Fellow supported by the Damon Runyon Cancer Research Foundation (DRG-2299-17). M.G.V.H. is supported by the Emerald Foundation, the Lustgarten Foundation, SU2C, the Ludwig Center at MIT, the US National Cancer Institute, the MIT Center for Precision Cancer Medicine and a Faculty Scholars award from the Howard Hughes Medical Institute.
Author information
Authors and Affiliations
Contributions
Both authors contributed to the discussion of manuscript content, writing of the manuscript and reviewing or editing of the manuscript before submission.
Corresponding author
Ethics declarations
Competing interests
M.G.V.H. is a consultant for and scientific advisory board member of Agios Pharmaceuticals, Aeglea Biotherapeutics and Auron Therapeutics. E.C.L. reports no competing interests.
Additional information
Peer review information
Nature Reviews Cancer thanks L. Hodson, V. Longo and the other, anonymous, reviewer(s) for their contribution to the peer review of this work.
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Lien, E.C., Vander Heiden, M.G. A framework for examining how diet impacts tumour metabolism. Nat Rev Cancer 19, 651–661 (2019). https://doi.org/10.1038/s41568-019-0198-5
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41568-019-0198-5
This article is cited by
-
Unveiling the methionine cycle: a key metabolic signature and NR4A2 as a methionine-responsive oncogene in esophageal squamous cell carcinoma
Cell Death & Differentiation (2024)
-
Lipids as mediators of cancer progression and metastasis
Nature Cancer (2024)
-
Is metabolism the magic bullet for targeted cancer therapy?
BMC Cancer (2023)
-
Lipid metabolic reprogramming in tumor microenvironment: from mechanisms to therapeutics
Journal of Hematology & Oncology (2023)
-
Fatty acid metabolism reprogramming in ccRCC: mechanisms and potential targets
Nature Reviews Urology (2023)