Abstract
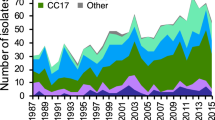
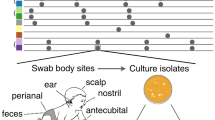
The multidrug-resistant Staphylococcus capitis NRCS-A clone is responsible for sepsis in preterm infants in neonatal intensive care units (NICUs) worldwide. Here, to retrace the spread of this clone and to identify drivers of its specific success, we investigated a representative collection of 250 S. capitis isolates from adults and newborns. Bayesian analyses confirmed the spread of the NRCS-A clone and enabled us to date its emergence in the late 1960s and its expansion during the 1980s, coinciding with the establishment of NICUs and the increasing use of vancomycin in these units, respectively. This dynamic was accompanied by the acquisition of mutations in antimicrobial resistance- and bacteriocin-encoding genes. Furthermore, combined statistical tools and a genome-wide association study convergently point to vancomycin resistance as a major driver of NRCS-A success. We also identified another S. capitis subclade (alpha clade) that emerged independently, showing parallel evolution towards NICU specialization and non-susceptibility to vancomycin, indicating convergent evolution in NICU-associated pathogens. These findings illustrate how the broad use of antibiotics can repeatedly lead initially commensal drug-susceptible bacteria to evolve into multidrug-resistant clones that are able to successfully spread worldwide and become pathogenic for highly vulnerable patients.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$29.99 / 30 days
cancel any time
Subscribe to this journal
Receive 12 digital issues and online access to articles
$119.00 per year
only $9.92 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout





Similar content being viewed by others
Data availability
The datasets supporting the results of this article are available from the Sequence Read Archive under accession no. PRJNA493527. Additional data on the 250 strains are available in Supplementary Table 1.
References
Howson, C. P., Kinney, M. V., McDougall, L. & Lawn, J. E., Born too soon preterm birth action group. Born too soon: preterm birth matters. Reprod. Health 10, S1 (2013).
Liu, L. et al. Global, regional, and national causes of under-5 mortality in 2000-15: an updated systematic analysis with implications for the sustainable development goals. Lancet 388, 3027–3035 (2016).
Boghossian, N. S. et al. Late-onset sepsis in very low birth weight infants from singleton and multiple-gestation births. J. Pediatr. 162, 1120–1124 (2013).
Stoll, B. J. et al. Late-onset sepsis in very low birth weight neonates: the experience of the NICHD neonatal research network. Pediatrics 110, 285–291 (2002).
Cohen-Wolkowiez, M. et al. Early and late onset sepsis in late preterm infants. Pediatr. Infect. Dis. J. 28, 1052–1056 (2009).
Rasigade, J. P. et al. Methicillin-resistant Staphylococcus capitis with reduced vancomycin susceptibility causes late-onset sepsis in intensive care neonates. PLoS ONE 7, e31548 (2012).
Butin, M. et al. Wide geographical dissemination of the multiresistant Staphylococcus capitis NRCS-A clone in neonatal intensive-care units. Clin. Microbiol. Infect. 22, 46–52 (2016).
Butin, M., Martins-Simoes, P., Rasigade, J. P., Picaud, J. C. & Laurent, F. Worldwide endemicity of a multidrug-resistant Staphylococcus capitis clone involved in neonatal sepsis. Emerg. Infect. Dis. 23, 538–539 (2017).
Carter, G. P. et al. Genomic analysis of multi-resistant Staphylococcus capitis associated with neonatal sepsis. Antimicrob. Agents Chemother. 62, e00898–18 (2018).
Ben Said, M. et al. Late-onset sepsis due to Staphylococcus capitis ‘neonatalis’ in low-birthweight infants: a new entity? J. Hosp. Infect. 94, 95–98 (2016).
Lee, J. Y. H. et al. Global spread of three multidrug-resistant lineages of Staphylococcus epidermidis. Nat. Microbiol. 3, 1175–1185 (2018).
Didelot, X. & Wilson, D. J. ClonalFrameML: efficient inference of recombination in whole bacterial genomes. PLoS Comput. Biol. 11, e1004041 (2015).
Stegger, M. et al. Origin and evolution of European community-acquired methicillin-resistant Staphylococcus aureus. mBio 5, e01044–14 (2014).
Nubel, U. et al. A timescale for evolution, population expansion, and spatial spread of an emerging clone of methicillin-resistant Staphylococcus aureus. PLoS Pathog. 6, e1000855 (2010).
Simoes, P. M. et al. Single-molecule sequencing (PacBio) of the Staphylococcus capitis NRCS-A clone reveals the basis of multidrug resistance and adaptation to the neonatal intensive care unit environment. Front. Microbiol. 7, 1991 (2016).
Martins Simoes, P. et al. Characterization of a novel composite staphylococcal cassette chromosome mec (SCCmec-SCCcad/ars/cop) in the neonatal sepsis-associated Staphylococcus capitis pulsotype NRCS-A. Antimicrob. Agents Chemother. 57, 6354–6357 (2013).
Duforet-Frebourg, N., Bazin, E. & Blum, M. G. B. Genome scans for detecting footprints of local adaptation using a Bayesian factor model. Mol. Biol. Evol. 31, 1–13 (2014).
Merker, M. et al. Evolutionary history and global spread of the Mycobacterium tuberculosis Beijing lineage. Nat. Genet. 47, 242–249 (2015).
Beabout, K. et al. The ribosomal S10 protein is a general target for decreased tigecycline susceptibility. Antimicrob. Agents Chemother. 59, 5561–5566 (2015).
Kuroda, M., Kuwahara-Arai, K. & Hiramatsu, K. Identification of the up- and down-regulated genes in vancomycin-resistant Staphylococcus aureus strains Mu3 and Mu50 by cDNA differential hybridization method. Biochem. Biophys. Res. Commun. 269, 485–490 (2000).
Grayczyk, J. P., Harvey, C. J., Laczkovich, I. & Alonzo, F. 3rd A lipoylated metabolic protein released by Staphylococcus aureus suppresses macrophage activation. Cell Host Microbe 22, 678–687 (2017).
Zorzoli, A., Grayczyk, J. P. & Alonzo, F. III. Staphylococcus aureus tissue infection during sepsis is supported by differential use of bacterial or host-derived lipoic acid. PLoS Pathog. 12, e1005933 (2016).
Hu, Q., Peng, H. & Rao, X. Molecular events for promotion of vancomycin resistance in vancomycin intermediate Staphylococcus aureus. Front. Microbiol. 7, 1601 (2016).
Krzyzaniak, N., Pawlowska, I. & Bajorek, B. Review of drug utilization patterns in NICUs worldwide. J. Clin. Pharm. Ther. 41, 612–620 (2016).
Rasigade, J.-P. et al. Strain-specific estimation of epidemic success provides insights into the transmission dynamics of tuberculosis. Sci. Rep. 7, 45326 (2017).
Lamichhane-Khadka, R. et al. sarA inactivation reduces vancomycin-intermediate and ciprofloxacin resistance expression by Staphylococcus aureus. Int. J. Antimicrob. Agents 34, 136–141 (2009).
Schaaff, F., Reipert, A. & Bierbaum, G. An elevated mutation frequency favors development of vancomycin resistance in Staphylococcus aureus. Antimicrob. Agents Chemother. 46, 3540–3548 (2002).
Jacqz-Aigrain, E., Zhao, W., Sharland, M. & van den Anker, J. N. Use of antibacterial agents in the neonate: 50 years of experience with vancomycin administration. Semin. Fetal Neonatal Med. 18, 28–34 (2013).
Levine, D. P. Vancomycin: a history. Clin. Infect. Dis. 42, S5–S12 (2006).
Mukhopadhyay, S., Sengupta, S. & Puopolo, K. M. Challenges and opportunities for antibiotic stewardship among preterm infants. Arch. Dis. Child Fetal Neonatal Ed. 104, F327–F332 (2019).
Cailes, B. et al. Antimicrobial resistance in UK neonatal units: neonIN infection surveillance network. Arch. Dis. Child Fetal Neonatal Ed. 103, F474–F478 (2018).
Butin, M. et al. Adaptation to vancomycin pressure of multiresistant Staphylococcus capitis NRCS-A involved in neonatal sepsis. J. Antimicrob. Chemother. 70, 3027–3031 (2015).
Williamson, D. A. et al. High usage of topical fusidic acid and rapid clonal expansion of fusidic acid-resistant Staphylococcus aureus: a cautionary tale. Clin. Infect. Dis. 59, 1451–1454 (2014).
Millette, M. et al. Capacity of human nisin- and pediocin-producing lactic acid bacteria to reduce intestinal colonization by vancomycin-resistant enterococci. Appl. Environ. Microbiol. 74, 1997–2003 (2008).
Butin, M. et al. Vancomycin treatment is a risk factor for vancomycin-nonsusceptible Staphylococcus capitis sepsis in preterm neonates. Clin. Microbiol. Infect. 23, 839–844 (2017).
Brown, S., Santa Maria, J. P. Jr & Walker, S. Wall teichoic acids of gram-positive bacteria. Annu. Rev. Microbiol. 67, 313–336 (2013).
Nasser, R. M. et al. Outbreak of Burkholderia cepacia bacteremia traced to contaminated hospital water used for dilution of an alcohol skin antiseptic. Infect. Control Hosp. Epidemiol. 25, 231–239 (2004).
Ory, J. et al. Successful implementation of infection control measure in a neonatal intensive care unit to combat the spread of pathogenic multidrug resistant Staphylococcus capitis. Antimicrob. Resist. Infect. Control 8, 57 (2019).
Wood, D. E. & Salzberg, S. L. Kraken: ultrafast metagenomic sequence classification using exact alignments. Genome Biol. 15, R46 (2014).
Wick, R. R., Judd, L. M., Gorrie, C. L. & Holt, K. E. Unicycler: resolving bacterial genome assemblies from short and long sequencing reads. PLoS Comput. Biol. 13, e1005595 (2017).
Gurevich, A., Saveliev, V., Vyahhi, N. & Tesler, G. QUAST: quality assessment tool for genome assemblies. Bioinformatics 29, 1072–1075 (2013).
Inouye, M. et al. SRST2: Rapid genomic surveillance for public health and hospital microbiology labs. Genome Med. 6, 90 (2014).
Kaya, H. et al. SCCmecFinder, a web-based tool for typing of staphylococcal cassette chromosome mec in Staphylococcus aureus using whole-genome sequence data. mSphere 3, e00612–17 (2018).
Langmead, B. & Salzberg, S. L. Fast gapped-read alignment with Bowtie 2. Nat. Methods 9, 357–359 (2012).
Couvin, D. et al. CRISPRCasFinder, an update of CRISRFinder, includes a portable version, enhanced performance and integrates search for Cas proteins. Nucleic Acids Res. 46, W246–W251 (2018).
Schmidt, H. A., Strimmer, K., Vingron, M. & von Haeseler, A. TREE-PUZZLE: maximum likelihood phylogenetic analysis using quartets and parallel computing. Bioinformatics 18, 502–504 (2002).
Guindon, S. et al. New algorithms and mehtods to estimate maximum-likelihood phylogenies: asessing the performance of PhyML 2.0. Syst. Biol. 59, 307–321 (2010).
Letunic, I. & Bork, P. Interactive tree of life (iTOL) v3: an online tool for the display and annotation of phylogenetic and other trees. Nuc. Acids Res. 44, W242–W245 (2016).
Rambaut, A., Lam, T. T., Max Carvalho, L. & Pybus, O. G. Exploring the temporal structure of heterochronous sequences using TempEst (formerly Path-O-Gen). Virus Evol. 2, vew007 (2016).
Anderson, M. J. & Robinson, J. Permutation tests for linear models. Aust. NZ J. Stat. 43, 75–88 (2001).
Bouckaert, R. et al. BEAST 2: a software platform for Bayesian evolutionary analysis. PLoS Comput. Biol. 10, e1003537 (2014).
Huson, D. H. & Bryant, D. Application of phylogenetic networks in evolutionary studies. Mol. Biol. Evol. 23, 254–267 (2006).
Didelot, X., Lawson, D., Darling, A. & Falush, D. Inference of homologous recombination in bacteria using whole genome sequences. Genetics 186, 1435–1449 (2010).
Joseph, S. J., Didelot, X., Gandhi, K., Dean, D. & Read, T. D. Interplay of recombination and selection in the genomes of Chlamydia trachomatis. Biol. Direct 6, 28 (2011).
Kelley, L. A., Mezulis, S., Yates, C. M., Wass, M. N. & Sternberg, M. J. The Phyre2 web portal for protein modeling, prediction and analysis. Nat. Protoc. 10, 845–858 (2015).
Pettersen, E. F. et al. UCSF Chimera—a visualization system for exploratory research and analysis. J. Comput. Chem. 25, 1605–1612 (2004).
Andrews, J. M. Determination of minimum inhibitory concentrations. J. Antimicrob. Chemother. 48, 5–16 (2001).
Satola, S. W., Farley, M. M., Anderson, K. F. & Patel, J. B. Comparison of detection methods for heteroresistant vancomycin-intermediate Staphylococcus aureus, with the population analysis profile method as the reference method. J. Clin. Microbiol. 49, 177–183 (2011).
Barbier, M. et al. Changing patterns of human migrations shaped the global population structure of Mycobacterium tuberculosis in France. Sci. Rep. 8, 5855 (2018).
Jaillard, M. et al. A fast and agnostic method for bacterial genome-wide association studies: Bridging the gap between k-mers and genetic events. PLoS Genet. 14, e1007758 (2018).
Vallenet, D. et al. MaGe: a microbial genome annotation system supported by synteny results. Nuc. Acids Res. 34, 53–65 (2006).
Maali, Y. et al. Understanding the virulence of Staphylococcus pseudintermedius: a major role of pore-forming toxins. Front. Cell Infect. Microbiol. 8, 221 (2018).
Loftus, R. W., Dexter, F., Robinson, A. D. M. & Horswill, A. R. Desiccation tolerance is associated with Staphylococcus aureus hypertransmissibility, resistance and infection development in the operating room. J. Hosp. Infect. 100, 299–308 (2018).
Karauzum, H. et al. Comparison of adhesion and virulence of two predominant hospital-acquired methicillin-resistant Staphylococcus aureus clones and clonal methicillin-susceptible S. aureus isolates. Infect. Immun. 76, 5133–5138 (2008).
Streker, K., Freiberg, C., Labischinski, H., Hacker, J. & Ohlsen, K. Staphylococcus aureus NfrA (SA0367) is a flavin mononucleotide-dependent NADPH oxidase involved in oxidative stress response. J. Bacteriol. 187, 2249–2256 (2005).
Loo, C., Mitrakul, K., Voss, I., Hughes, C. & Ganeshkumar, N. Involvement of an inducible fructose phosphotransferase operon in Streptococcus gordonii biofilm formation. J. Bacteriol. 185, 6241–6254 (2003).
Valour, F. et al. Staphylococcus epidermidis in orthopedic device infections: the role of bacterial internalization in human osteoblasts and biofilm formation. PLoS ONE 8, e67240 (2013).
Tissieres, P. et al. Innate immune deficiency of extremely premature neonates can be reversed by interferon-γ. PLoS ONE 7, e32863 (2012).
Acknowledgements
We thank M. Stegger and his team for insightful exchanges during the manuscript drafting and C. Allix-Béguec, C. Gaudin, M. Mairey and S. Duthoy for their help in genome sequencing. This project was supported by the European Society of Clinical Microbiology and Infectious Diseases study group (Project P307-14), the Fondation pour la Recherche Médicale (project ING20160435683) and the European Union Patho-Ngen-Trace (project FP7-278864).
Author information
Authors and Affiliations
Consortia
Contributions
M.Butin, T.W., J.-C.P. and F.L. conceived the project. M.Butin and F.L. established and analysed clinical and reference isolate datasets. B.P., A.K. and R.P. performed DNA extractions. P.S. performed DNA sequencing. B.P., A.K. and R.P. performed antimicrobial susceptibility testing. P.T. performed phagocytosis assays. M.Butin performed all additional phenotypic assays. T.W., M.Barbier, P.M.-S. and M.Bergot analysed genomic data. J.-P.R. participated in genomic analyses and performed THD analysis. M.Bergot and L.J. performed GWAS analysis. T.W., M.Butin, P.S. and F.L. drafted the manuscript. All authors reviewed and contributed to the final manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Extended data
Extended Data Fig. 1 CLONALFRAMEML analysis of recombination in S. capitis.
Analysis was based on 55 genomes: all non-NRCS-A strains were included, however the clone NRCS-A was undersampled to avoid a statistical bias in favor of mutational changes. Dark blue horizontal bars indicate recombination events detected by the analysis.
Extended Data Fig. 2 NRCS-A host types and genetic structure.
a, NRCS-A isolates within an MSTREE based on the whole genome sequencing data. Each strain is represented by a circle or a fraction of a circle, colors correspond to different host types. Numbers indicate the mutational steps between the strains. b, Same data as above but represented in an MDS plot. c, Within NRCS-A diversity as assessed by mean pairwise SNP distances (N=197). d, Graphical chart representing the fraction of strains obtained from newborns in the basal, Proto-outbreak 1 and 2 and Outbreak strains.
Extended Data Fig. 3 Genome scan analysis of NRCS-A strains for detecting SNPs involved in local adaptation.
a, Plot of the first 2 principal components (PC). The 197 NRCS-A strains are represented by points and colorized according to their phylogenic origin (Proto-outbreak 1 and 2 in blue, and Outbreak in red). PC 2 is the one separating the basal proto-outbreak 1 and 2 strains from the outbreak strains. b, Manhattan plot representing the 3,658 SNPs and values obtained after performing Mahalanobis distances. The SNPs are colorized according to the PC to which they correlate most (PC1 = black, PC2 = red, PC3 = green and PC4 = blue).
Extended Data Fig. 4 Specific SNPs in Outbreak and Alpha isolates.
Respectively 32 and 17 SNPs were specifically identified in Outbreak strains among NRCS-A strains (n=197) or in clade Alpha strains among Basal strains (n=53). Those SNPs were identified using PCADAPT.
Extended Data Fig. 5 Tertiary protein structures.
a, Positions on the tertiary protein structure of outbreak specific non-synonymous mutations detected via PCADAPT and involved in antibiotic resistance (tigecycline and vancomycin). b, Positions on the tertiary protein structure of alpha-clone specific non-synonymous mutations for a set of two genes involved in cell wall synthesis. Visualization and predictions were executed by PHYRE2 software (http://www.sbg.bio.ic.ac.uk/phyre2).
Extended Data Fig. 6 Phenotypic and genotypic resistance patterns of S. capitis isolates.
Phenotypic data of S. capitis isolates (n=250) were obtained from agar dilution and biomarkers of antibiotic resistance were detected using GENEFINDER. Comparison between groups of isolates was performed using two-sided Fisher exact test.
Extended Data Fig. 7 Phenotypic assays comparing a subset of representative isolates of each of the four subgroups identified by the phylogeographical analysis (Outbreak, Proto-outbreak 1, Proto-outbreak 2 and ‘other isolates’).
In all 6 graphs, center values represent means. a, Culture supernatants cytotoxicity assay using THP1 cells, adjusted on a positive control (Triton) of 12 representative S. capitis isolates (two independent experiments in triplicate for each strains). b, Survival of strains (n=12) after 24 hours of persistence in desiccation conditions (two independent experiments in triplicate for each strains). c, Comparison of the doubling time of bacterial growth during the exponential phase in standard conditions (BHI) of 24 representative S. capitis isolates (three independent experiments in triplicate for each strains) and d, Under oxidative stress (ethanol-supplemented medium to a final concentration of 6.5%) (n=24 strains, three independent experiments in triplicate for each strains). e, Quantification of biofilm production of 24 representative S. capitis isolates using crystal violet method (expressed as optic densitometry at 590nm) (three independent experiments in triplicate for each strains). f, Phagocytosis index of monocytes and granulocytes from cord blood for a subset of 5 representative isolates of “Outbreak” and “Basal” isolates (four independent experiments). Of note, results of phagocytosis of neutrophils and activated neutrophils are not represented here because they were similar to those with granulocytes.
Extended Data Fig. 8 Genes associated with vancomycin MIC and/or THD success index using DBGWAS.
Here are represented genes with a -log10 (HMP) > 7.5 on either axis, and/or > 5 on both axes, thus considered significant.
Supplementary information
Supplementary Information
Results, including three supplementary figures.
Supplementary Table 1
This table includes source data and details about each isolate (identification, origin, phenotypic and genomic characteristics, genes content and THD index).
Rights and permissions
About this article
Cite this article
Wirth, T., Bergot, M., Rasigade, JP. et al. Niche specialization and spread of Staphylococcus capitis involved in neonatal sepsis. Nat Microbiol 5, 735–745 (2020). https://doi.org/10.1038/s41564-020-0676-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41564-020-0676-2
This article is cited by
-
Pathogenic potential of meat-borne coagulase negative staphylococci strains from slaughterhouse to fork
International Microbiology (2024)
-
Transcontinental spread and evolution of Mycobacterium tuberculosis W148 European/Russian clade toward extensively drug resistant tuberculosis
Nature Communications (2022)
-
Development of a novel core genome MLST scheme for tracing multidrug resistant Staphylococcus capitis
Nature Communications (2022)
-
High fluoroquinolone resistance proportions among multidrug-resistant tuberculosis driven by dominant L2 Mycobacterium tuberculosis clones in the Mumbai Metropolitan Region
Genome Medicine (2022)
-
Staphylococcus epidermidis clones express Staphylococcus aureus-type wall teichoic acid to shift from a commensal to pathogen lifestyle
Nature Microbiology (2021)