Abstract
In Parkinson’s disease (PD), concurrent declines in cognitive and motor domain function can severely limit an individual’s ability to conduct daily tasks. Current diagnostic methods, however, lack precision in differentiating domain-specific contributions of cognitive or motor impairments based on a patients’ clinical manifestation. Fear of falling (FOF) is a common clinical manifestation among the elderly, in which both cognitive and motor impairments can lead to significant barriers to a patients’ physical and social activities. The present study evaluated whether a set of analytical and machine-learning approaches could be used to help delineate boundary conditions and separate cognitive and motor contributions to a patient’s own perception of self-efficacy and FOF. Cognitive and motor clinical scores, in conjunction with FOF, were collected from 57 Parkinson’s patients during a multi-center rehabilitation intervention trial. Statistical methodology was used to extract a subset of uncorrelated cognitive and motor components associated with cognitive and motor predictors, which were then used to independently identify and visualize cognitive and motor dimensions associated with FOF. We found that a central cognitive process, extracted from tests of executive, attentional, and visuoperceptive function, was a unique and significant independent cognitive predictor of FOF in PD. In addition, we provide evidence that the approaches described here may be used to computationally discern specific types of FOF based on separable cognitive or motor models. Our results are consistent with a contemporary model that the deterioration of a central cognitive mechanism that modulates self-efficacy also plays a critical role in FOF in PD.
Similar content being viewed by others
Introduction
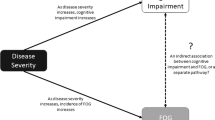
A common feature of progressive neurodegenerative diseases, such as Parkinson’s disease (PD), is that clinical manifestations often involve degenerative pathology in multi-systems in which motor and cognitive dysfunction can co-exist and interact to complicate efforts in symptom diagnosis and intervention.1,2,3 In PD, which carries one of the highest fall risk among neurological illnesses,4 both cognitive and motor-function decline can affect an individual’s ability to conduct daily tasks.1,5,6 For example, fear of falling (FOF), a function of one’s perceived risk of falling and cognitive functioning, is a common concern among the elderly and poses a significant barrier to physical and social activities, which can lead to a downward spiral in general health.1 FOF is significantly associated with actual falls, which together, may lead to a self-induced restriction of activity, reductions in muscle strength, and general physical de-conditioning that may serve to further increase fall risk.1,7,8 Importantly, FOF in and of itself is a significant determinant of health-related quality of life even more so than balance impairments or actual falling.9,10,11 However, although motor impairment and poor gait function are associated with FOF,9,12,13,14,15 individuals with PD can have obvious motor impairment and experience falls, but lack FOF.16 It would therefore be highly desirable to develop precision medicine methods that would be able to differentiate domain-specific contributions of cognitive or motor impairments with respect to FOF.
Previous research has used the Falls Efficacy Scale-International (FES-I) as a composite measure for fall concern and a state of FOF.15,17 Since the FES-I-defined state of FOF incorporates measures related to balance, previous falls, and depressive symptoms,17 the association between motor impairments and FOF is hardly surprising. Indeed, it has been frequently proposed that the therapeutic management of FOF should focus on targeting lower-level mobility problems.1,9,12,13,14 In addition to motor impairment, it is also well established that individuals with PD can have cognitive dysfunction early in the course of the disease that can occur independent of motor system pathology.18,19 FOF in PD therefore, may not necessarily emerge because of underlying motor system pathology, but rather because of poor cognitive functioning. In this context, deteriorating higher-level cognitive functioning may result in an inaccurate appraisal and underestimation of ones’ actual motor capabilities,20 thus resulting in increased uncertainty around fall-related self-efficacy and higher FES-I scores and FOF. Moreover, unlike a motor model of FOF, a cognitive dysfunction model of FOF would also predict that certain individuals with PD may actually overestimate their own physical efficacy.21 This is clinically important as it may lead to a lower level of caution and a greater likelihood of engaging in high fall-risk behaviors in these individuals.
Prior studies on the relationship of FOF and cognitive functioning in PD have yielded contradicting results, with some studies suggesting that there is a relationship between cognitive functioning and FOF, and others reporting that there is not.13,16,22,23,24 A notable feature of these studies is that predictor variable correlations and regressions are often conducted on similar domains or aspects of the same domain that are embedded within multiple clinical evaluations (different measures of gait, clinical scores, etc.). When interrelated predictor variables are correlated in regression models they can reflect a common or shared underlying dimension (i.e., variable),13,25,26 which can sometimes lead to difficulty in determining the contributions of individual predictors among a group of interrelated predictors. One approach to overcome this issue is to first separate clinical data into uncorrelated dimensions before predictive statistical analysis. In this study, we therefore used an approach that allowed us to extract uncorrelated measures of cognitive and motor function, which were then used to independently identify and visualize cognitive and motor dimensions associated with FOF.
Results
Extraction of cognitive and motor dimensions
Demographic and clinical data indicated that our patient cohort tended to be male, educated, and moderately impaired (Table 1). To reduce noise in the data and extract underlying features that are most sensitive to FOF, a dimensionality reduction was performed through principal component analysis (PCA). The collected test scores were first adjusted for age, sex, disease duration, and education, and then subjected to PCA to extract uncorrelated components that share underlying variance.25 We found that unlike unadjusted test scores which resulted in partial or mixed-domain components, adjusted scores yielded two separable domain-specific components related to motor and cognitive function. Hoehn & Yahr, UPDRS-III, and gait speed all loaded together onto one component (motor domain), while visuospatial, attention, and memory retrieval test scores all loaded together onto another component (cognition domain) (Table 2 and Supplementary Fig. S1). These domain-specific components represent the largest components, which together, account for over half of the total variance of the six variables used in the dimensionality reduction analysis (Table 2).
Association of cognitive and motor dimensions with FOF
Next, each individual’s component scores were computed and evaluated. Extracted component scores were used to construct logistic regression models to evaluate the relationship between FOF and the extracted domains. As can be seen in Supplementary Fig. S2, a single predictor model including the motor domain illustrates that decreasing motor component scores are associated with an increasing probability of FOF. The cognitive component demonstrated a similar pattern to that of the motor domain with respect to FOF in a single predictor model (Supplementary Fig. S2). However, the individual regression models do not allow us to evaluate the independent contribution of the cognitive domain. For this, we next entered the motor and cognitive component scores into a single logistic regression model. This analysis revealed that while decreases in both motor and cognitive domain functioning are associated with increased probability of FOF, the extracted cognitive component was a significant and independent predictor of FOF (Table 3). The odds ratios and 95% confidence intervals (CI) from the final logistic regression model are shown in Table 3.
Identifying FOF boundaries extending along cognitive and motor dimensions
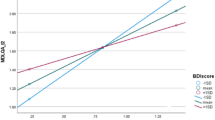
As it is difficult for a single assessment tool, such as the FES-I to capture the underlying contributing factors of FOF, we wanted to examine if it was possible to identify FOF margins along cognitive and motor dimensions. This is important as it may help to uncover the dimensions that may be contributing to an individual’s FOF. For this we used the machine-learning algorithm support vector machines (SVM), which is an effective tool for classifying and defining variable boundaries along dimensions as the algorithm is designed to use a subset of the observed data to identify boundary conditions (i.e., the support vectors) for model building.27,28 Indeed, SVM not only revealed that there are boundaries and regions between FOF and non-FOF based on extracted cognitive and motor dimension scores (Fig. 1; purple vs. blue), but it also delineated boundaries that exist between FOF areas. The statistically distinct models resulting from SVM analysis included a cognitive model representing poor cognitive functioning with relatively mild motor impairment, and a motor model characterized by poor motor functioning with or without poor cognitive functioning (see Discussion and Fig. 1 for additional details).
SVM classification plot based on cognitive and motor dimension scores. Purple and blue areas represent SVM defined FOF and non-FOF classification regions based on combined cognitive and motor dimension scores, respectively. “X” and “O” represent data from individuals, while the “X” denotes support vector data for model building. Red and black “X” and “O” coloring denotes FOF and non-FOF, respectively. Here, overall classification accuracy was greater than 92%. Note the model also identified boundaries between FOF; a region corresponding to poor cognitive functioning with relatively mild motor impairment (labeled as “Cognitive Model”), and a region represented by poor motor functioning (labeled as “Motor Model”) that also extends down along the cognitive dimension
Discussion
In the current study we performed a new set of statistical procedures with the aim to more precisely identify the underlying features that are most sensitive to FOF. We found through dimensionality reduction that a cognitive domain component can serve as an independent predictor of FOF in PD. This unique cognitive domain, defined by visuospatial, attention, and memory functioning, may reflect a central cognitive mechanism (see below). The significant association between cognitive dysfunction and FOF persisted even after adjusting for impairments in the motor dimension, indicating that both motor and cognitive models of FOF may play an important, yet different, role in FOF.
Previous bivariate and multivariate analysis related to the topic of cognitive functioning and FOF in PD have yielded conflicting results.13,16,22,23,24 In particular, executive-related functioning has not been explicitly identified in these studies as an independent predictor of FOF in PD. In addition to confirming previous research identifying a motor model of FOF, unique to this study, we used statistical methodology and dimensionality reduction and identified a cognitive domain-specific component associated with FOF in PD based on standardized clinical test scores. This makes comparisons between domains immediately interpretable despite the different methods and scales used to assess them. The approaches described here can be used to computationally discern cognitive and motor models of FOF in PD. Given that our study sample represents individuals with fairly mild to moderate PD, the analytical and machine-learning approaches described here may help in the initial therapeutic management of FOF and the development of individualized treatment plans to facilitate precision medicine in PD.
The PCA method used here also produced an additional interesting result, the finding that visuospatial/executive skills (alternating trail making; visuoconstructional-cube; visuoconstructional-clock) and attention (serial subtract 7) both loaded highly onto the same component (Table 2 and Supplementary Fig. S1). This supports previous work suggesting that the frontal-mediated attention/working memory task of serial subtract 7 may also have internal visuospatial scratchpad and spatial components.29 In fact, previous work has suggested that “storage-plus-processing” tasks are linked to executive function by a shared underlying cognitive ability, which has been referred to in the literature as executive attention or central executive.26,30 This underlying dimension, defined as the higher-level neural component required to coordinate complex cognition, involves directing attention, maintaining task goals, decision making, and memory retrieval,26,30 all of which are required for the cognitive tasks used in the current study. This suggests that despite a lack of significant motor impairment, FOF may indeed emerge in the cognitive model from dysfunction of a more complex cognitive mechanism and that the independent contribution of this higher-level cognitive component, rather than the more specific cognitive domains of attention, visuospatial, and memory retrieval per se, may represent aberrant coordinated regulation of executive systems.
Clinically, dysfunction of complex cognitive control may take the form of disrupted ‘cognitive’ estimates of probability and cost, and an underestimate of functional abilities as a result of a dissociation between heightened subjective feelings of threat (i.e., fall-related self-efficacy), and objectively accurate cognitive threat calculations.20,21,31 However, as the cognitive neuropathological load increases, awareness of more severe motor deficits can decline which can lead to the opposite effect, an overestimate of functional abilities.32,33 This may also help explain the downward left-protruding non-FOF region in Fig. 1, and represent individuals that may be at a higher risk of falling (i.e., individuals with greater motor impairment, but fail to recognize/appreciate this). This interpretation is consistent with that of Mak et al. (2014), who reported that greater disease severity and cognitive impairment is not necessarily associated with increased FOF, despite increased fall risk.24
In the SVM analysis, we also identified an interesting non-FOF region directly above the motor model (Fig. 1). This suggests, albeit indirectly, that under the condition of intact cognitive functioning, FOF may not become a dominant clinical manifestation. This may be due to one’s continued ability for increased attentional focus and awareness of self-efficacy, and the conscious use of protective measures, such as cautious gait to provide a sufficient level of fall-related self-efficacy.34,35 This also raises the possibility that cognitive training may be an effective therapeutic approach to reduce FOF.
Prior work has demonstrated a relationship between self-efficacy and behavioral measures of cognitive performance, and that self-efficacy can be enhanced by the provision of efficacy information that reflects mastery.36,37,38 Therefore, self-efficacy, and thus FOF, is a modifiable psychological construct.39 This is important as it suggests that the therapeutic management of FOF may be better served by focussing efforts on appropriate targets; lower-order mobility issues with the motor model, and cognitive functioning targets for the cognitive model. With easily amenable App-based approaches for cognitive training,40 and the capacity for smartphone Apps to facilitate behavior change, recent advancements in mobile device technology41,42,43 make integration of smartphone technology into behavioral healthcare quite feasible even in the cognitive dimension.44,45,46
We do acknowledge the limitations of this study. The primary limitation of this study is its cross-sectional design. Our study sample therefore represents a static picture of individuals with fairly mild to moderate PD, many without FOF. A long-term longitudinal study would allow for a better predictive model to capture changes in cognitive and motor domains and the time-dependent transition to FOF within the same study sample. A second limitation is that we do not have fall history data. This is related to the fact that the individuals anticipated to report a fall history would also have greater cognitive dysfunction,47,48 and thus clearly limits the reliability of retrospective data like that typically collected for fall history.49 Future studies should therefore consider a prospective account of fall events to identify fall risk. Third, while an advantage of SVM is that it only considers instances that are close to the boundary; meaning that SVM is unaffected by instances far away from the boundary despite the fact that they may be greater in number,27,28 there is still a need for future work to verify these proof-of-concept findings in a larger and more heterogeneous PD population (i.e., mild to severe PD). This would allow for both, more robust boundary definitions as there would be a greater proportion of individuals with and without FOF at the boundary that could be used to define the boundary (i.e., support vectors), as well as further validating the localization of individuals to particular FOF models. Fourth, another limitation of the current study is that individuals were not evaluated on measures of depression and/or anxiety. This may be particularly relevant as cognitive dysfunction associated with FOF may also be driving certain neuropsychiatric aspects of PD such as increased anxiety.50 Finally, it is also worth mentioning that extracted cognitive and motor domain scores were not adjusted for l-Dopa equivalent daily dose. However, similar to previous work,25 extracted scores were instead adjusted for disease duration, which is significantly associated with l-Dopa equivalent daily dose even after controlling for other demographic and disease-specific measures.51,52 Strengths of this study on the other hand are that it incorporated data from multiple centers, and that it used the FES-I to conceptualize FOF. Despite the fact that the individuals in the current study did not undergo comprehensive neuropsychiatric testing, and with the limitations of our cross-sectional design, our use of FES-I-defined FOF has the added advantage of using a FOF conceptualization, which incorporates measures of balance and neuropsychiatric symptoms through which the convergent and predictive validity has been explored extensively in a longitudinal design.17
To conclude, as the nature of FOF is multi-factorial, it is difficult for a single assessment tool, such as the FES-I to capture the underlying contributing factors to FOF. Simply identifying FOF in PD may not be sufficient. The approach presented here, on the other hand, may not only be able to identify PD individuals with FOF, but may also help identify the underlying model contributing to FOF. This form of precision medicine may ultimately have a transformative effect on the therapeutic management of FOF in PD.
Methods
Participants
This is a cross-sectional observational study that included a convenience sample of 57 (n = 57) individuals with PD from an ongoing registered intervention trial (ISRCTN06023392). Ethics approval from the University Ethics Board for Human Research (REB13-0009) and informed written consent were obtained. Our sample size was guided by a recommendation of having approximately 10 times as many participants as dimensionality reduction variables,53 which was to be subsequently verified by the Kaiser–Meyer–Olkin measure of sampling adequacy. All PD participants were initially recruited via clinician referral by a neurologist at the University of Calgary, University of Alberta, and University of British Columbia, and through Parkinson Alberta Society support groups. These patients had a confirmed diagnosis of PD, were on a steady medication routine, and were tested in the “on” state.
Clinical testing
The participants completed Unified Parkinson’s Disease Rating Scale Part 3 (UPDRS-III) and Hoehn & Yahr staging by a trained practitioner. For cognitive executive function tests, we used standard visuospatial function (alternating trail making; visuoconstructional-cube; visuoconstructional-clock), attention processing (serial subtract 7), and short-term memory retrieval (delayed word recall).54 These cognitive tasks collectively test one’s storage-plus-processing capabilities, which are thought to rely on a common underlying cognitive process.26,30 Fall-related self-efficacy and FOF was assessed by the 16-item FES-I, which scores the level of concern about falls for a range of activities of daily living related to social and physical activities inside and outside the home,55 and has been clinically validated for PD.56 FOF is conceptualized by a “high-degree of fall concern” defined by a cut-off value determined by the state variables of balance, previous falls, and depressive symptoms.17 The state of FOF, therefore, is defined by a total FES-I score of ≥28.15,17
Walking test
Self-selected walking speed, or gait velocity provides a quantifiable index of ambulatory ability and gait functioning.57 To obtain an objective and quantitative assessment of walking speed, patients wore a wearable sensor (Ambulosono Sensor System58,59) and were instructed to walk in a defined area on-site at a self-selected pace. The walking time was controlled by Ambulosono, which runs off the iOS GaitReminder App that can issue auditory instructions while continuously recording step size via iOS gyro and accelerometers (after corrections for limb length, angular excursion, signal filtering, and drift).60 Step parameters obtained via GaitReminder have an average of <10% difference when tested against direct video measurements, and a similar error rate was also found when the App was used for treadmill walking or over-ground ambulation where actual values can be obtained from direct machine reading or physical measurement (e.g., markings on the floor).58,61 Similar results have also been obtained in a subsequent cohort (not shown).
Data and statistical analysis
All clinical and demographic data from our sample were included in our analysis. Descriptive statistics were calculated for demographic, clinical, and cognitive test scores (Table 1). Hoehn & Yahr and UPDRS-III were transformed into the same direction (i.e., assessment possible maximum score minus actual score). This means subjects that score lower (i.e., less motor impairment/disease severity) will have a higher transformed score. To avoid redundancy and account for underlying correlation patterns, a dimensionality reduction was performed through PCA. Linear regression was used to adjust raw test scores for age, disease duration, years of education, and sex, and the standardized residuals for each of the six predictor variables were included in the PCA. PCA components were extracted with an eigenvalue threshold of 1 or greater, and the components were rotated using a varimax rotation.25 The Kaiser–Meyer–Olkin measure verified sampling adequacy (KMO > 0.5). Component scores were then used in logistic regression models. SVM modeling27,28 was used to visualize FOF boundaries along extracted cognitive and motor dimensions. For our model hyperparameters we used a soft-margin constant C = 10 for the decision boundary and gamma = 0.5 to prevent over-fitting (verified with cross-validation). A radial basis function kernel was used. All analyses were conducted using IBM SPSS Statistics and R. Tests of significance were computed via the Wald statistic, and α was set at 0.05.
Data availability
The data that support the findings of this study are available from the corresponding authors upon reasonable request.
Code availability
R (R Core Team (2017). R: A language and environment for statistical computing. R Foundation for Statistical Computing, Vienna, Austria) and package e1071 are freely available (https://www.R-project.org/).
References
Speelman, A. D. et al. How might physical activity benefit patients with Parkinson disease? Nat. Rev. Neurol. 7, 528–534 (2011).
Titova, N., Padmakumar, C., Lewis, S. J. G. & Chaudhuri, K. R. Parkinson’s: a syndrome rather than a disease? J. Neural Transm. (Vienna) 124, 907–914 (2017).
Caligiore, D. et al. Parkinson’s disease as a system-level disorder.NPJ Parkinsons Dis. https://doi.org/10.1038/npjparkd.2016.25 (2016).
Homann, B. et al. The impact of neurological disorders on the risk for falls in the community dwelling elderly: a case-controlled study. BMJ Open https://doi.org/10.1136/bmjopen-2013-003367 (2013).
Domingos, J. M. et al. Cognitive impairment in fall-related studies in Parkinson disease. J Parkinsons Dis. 5, 453–469 (2015).
Allan, L. M., Ballard, C. G., Rowan, E. N. & Kenny, R. A. Incidence and prediction of falls in dementia: a prospective study in older people. PLoS One https://doi.org/10.1371/journal.pone.0005521 (2009).
Lindholm, B., Hagell, P., Hansson, O. & Nilsson, M. H. Prediction of falls and/or near falls in people with mild Parkinson’s disease. PLoS One https://doi.org/10.1371/journal.pone.0117018 (2015).
Allen, N. E., Schwarzel, A. K. & Canning, C. G. Recurrent falls in Parkinson’s disease: a systematic review. Parkinsons Dis. https://doi.org/10.1155/2013/906274 (2013).
Rahman, S., Griffin, H. J., Quinn, N. P. & Jahanshahi, M. On the nature of fear of falling in Parkinson’s disease. Behav. Neurol. https://doi.org/10.3233/BEN-2011-0330 (2011).
Thordardottir, B., Nilsson, M. H., Iwarsson, S. & Haak, M. “You plan, but you never know”--participation among people with different levels of severity of Parkinson’s disease. Disabil. Rehabil. 36, 2216–2224 (2014).
Grimbergen, Y. A. et al. Impact of falls and fear of falling on health-related quality of life in patients with Parkinson’s disease. J. Parkinsons Dis. 3, 409–413 (2013).
Cakit, B. D. et al. The effects of incremental speed-dependent treadmill training on postural instability and fear of falling in Parkinson’s disease. Clin. Rehabil. 21, 698–705 (2007).
Jonasson, S. B. et al. Concerns about falling in Parkinson’s disease: associations with disabilities and personal and environmental factors. J. Parkinsons Dis. 5, 341–349 (2015).
Mak, M. K., Pang, M. Y. & Mok, V. Gait difficulty, postural instability, and muscle weakness are associated with fear of falling in people with Parkinson’s disease. Parkinsons Dis. https://doi.org/10.1155/2012/901721 (2012).
Chomiak et al. Concurrent arm swing-stepping (CASS) can reveal gait start hesitation in Parkinson’s patients with low self-efficacy and fear of falling. Aging Clin. Exp. Res. 27, 457–463 (2015).
Thomas, A. A., Rogers, J. M., Amick, M. M. & Friedman, J. H. Falls and the falls efficacy scale in Parkinson’s disease. J. Neurol. 257, 1124–1128 (2010).
Delbaere, K. et al. The Falls Efficacy Scale International (FES-I). A comprehensive longitudinal validation study. Age Ageing 39, 210–216 (2010).
Cooper, J. A. et al. Cognitive impairment in early, untreated Parkinson’s disease and its relationship to motor disability. Brain 114, 2095–2122 (1991).
Kim, I. et al. Early-onset mild cognitive impairment in Parkinson’s disease: Altered corticopetal cholinergic network. Sci. Rep. https://doi.org/10.1038/s41598-017-02420-w (2017).
Hadjistavropoulos, T., Delbaere, K. & Fitzgerald, T. D. Reconceptualizing the role of fear of falling and balance confidence in fall risk. J. Aging Health 23, 3–23 (2010).
Borges Sde, M., Radanovic, M. & Forlenza, O. V. Fear of falling and falls in older adults with mild cognitive impairment and Alzheimer’s disease. Neuropsychol. Dev. Cogn. B 22, 312–321 (2015).
Lindholm, B., Hagell, P., Hansson, O. & Nilsson, M. H. Factors associated with fear of falling in people with Parkinson’s disease. BMC Neurol. https://doi.org/10.1186/1471-2377-14-19 (2014).
Brozova, H., Stochl, J., Roth, J. & Ruzicka, E. Fear of falling has greater influence than other aspects of gait disorders on quality of life in patients with Parkinson’s disease. Neuro Endocrinol. Lett. 30, 453–457 (2009).
Mak, M. K., Wong, A. & Pang, M. Y. Impaired executive function can predict recurrent falls in Parkinson’s disease. Arch. Phys. Med Rehabil. 95, 2390–2395 (2014).
Cholerton, B. A. et al. Evaluation of mild cognitive impairment subtypes in Parkinson’s disease. Mov. Disord. 29, 756–764 (2014).
McCabe, D. P. et al. The relationship between working memory capacity and executive functioning: evidence for a common executive attention construct. Neuropsychology 24, 222–243 (2010).
Noble, W. S. What is a support vector machine? Nat. Biotechnol. 24, 1565–1567 (2006).
Ben-Hur, A. & Weston, J. A user’s guide to support vector machines. Methods Mol. Biol. 609, 223–239 (2010).
Chochon, F., Cohen, L., van de Moortele, P. F. & Dehaene, S. Differential contributions of the left and right inferior parietal lobules to number processing. J. Cogn. Neurosci. 11, 617–630 (1999).
Miyake, A. et al. How are visuospatial working memory, executive functioning, and spatial abilities related? A latent-variable analysis. J. Exp. Psychol. Gen. 130, 621–640 (2001).
Grupe, D. W. & Nitschke, J. B. Uncertainty and anticipation in anxiety: an integrated neurobiological and psychological perspective. Nat. Rev. Neurosci. 14, 488–501 (2013).
Lin, F. et al. Awareness of memory abilities in community-dwelling older adults with suspected dementia and mild cognitive impairment. Dement. Geriatr. Cogn. Disord. 30, 83–92 (2010).
Tabert, M. H. et al. Functional deficits in patients with mild cognitive impairment: prediction of AD. Neurology 58, 758–764 (2002).
Buetow, S. A., Martinez-Martin, P. & McCormack, B. Falling upward with Parkinson’s disease. NPJ Parkinsons Dis. https://doi.org/10.1038/s41531-017-0031-3 (2017).
Rosenberg-Katz, K. et al. Fall risk is associated with amplified functional connectivity of the central executive network in patients with Parkinson’s disease. J. Neurol. 262, 2448–2456 (2015).
Themanson, J. R. et al. Self-efficacy effects on neuroelectric and behavioral indices of action monitoring in older adults. Neurobiol. Aging 29, 1111–1122 (2008).
Albert, M. S. et al. Predictors of cognitive change in older persons: MacArthur studies of successful aging. Psychol. Aging 10, 578–589 (1995).
Berry, J. M. & West, R. L. Cognitive self-efficacy in relation to personal mastery and goal setting across the life span. Int J. Behav. Dev. 16, 351–379 (1993).
Zijlstra, G. A. et al. Effects of a multicomponent cognitive behavioral group intervention on fear of falling and activity avoidance in community-dwelling older adults: results of a randomized controlled trial. J. Am. Geriatr. Soc. 57, 2020–2028 (2009).
Tippett, W. J. & Rizkalla, M. N. Brain training: rationale, methods, and pilot data for a specific visuomotor/visuospatial activity program to change progressive cognitive decline. Brain Behav. 4, 171–179 (2013).
Chomiak, T. et al. A training approach to improve stepping automaticity while dual-tasking in Parkinson’s disease: a prospective pilot study. Medicine (Baltimore) https://doi.org/10.1097/MD.0000000000005934 (2017).
Lakshminarayana, R. et al. Using a smartphone-based self-management platform to support medication adherence and clinical consultation in Parkinson’s disease. NPJ Parkinsons Dis. https://doi.org/10.1038/s41531-016-0003-z (2017).
McGregor, S. et al. The use of accelerometry as a tool to measure disturbed nocturnal sleep in Parkinson’s disease. NPJ Parkinsons Dis. https://doi.org/10.1038/s41531-017-0038-9 (2018).
Higgins, J. P. Smartphone applications for patients’ health and fitness. Am. J. Med. 129, 11–19 (2016).
Luxton, D. D. et al. mHealth for Mental Health: Integrating Smartphone Technology in Behavioral Healthcare. Prof. Psychol.: Res. Pract. 42, 505–512 (2011).
Lu, M. H., Lin, W. L. & Yueh, H. P. Development and evaluation of a cognitive training game for older people: a design-based approach. Front. Psychol. https://doi.org/10.3389/fpsyg.2017.01837 (2017).
Domingos, J. M. et al. Cognitive impairment in fall-related studies in Parkinson’s disease. J Parkinsons Dis. 5, 453–469 (2015).
Camicioli, R. & Majumdar, S. R. Relationship between mild cognitive impairment and falls in older people with and without Parkinson’s disease: 1-Year prospective cohort study. Gait Posture 32, 87–91 (2010).
Hannan, M. T. et al. Optimizing the tracking of falls in studies of older participants: comparison of quarterly telephone recall with monthly falls calendars in the MOBILIZE Boston Study. Am. J. Epidemiol. 171, 1031–1036 (2010).
Reynolds, G. O., Hanna, K. K., Neargarder, S. & Cronin-Golomb, A. The relation of anxiety and cognition in Parkinson’s disease. Neuropsychology 31, 596–604 (2017).
Munhoz, R. P. et al. Long-duration Parkinson’s disease: role of lateralization of motor features. Park. Relat. Disord. 19, 77–80 (2013).
Lee, J. Y. et al. Daily dose of dopaminergic medications in Parkinson disease: clinical correlates and a posteriori equation. Neurology Asia 15, 137–143 (2010).
Everitt, B. S. Multivariate analysis: the need for data, and other problems. Br. J. Psychiatry 126, 237–240 (1975).
Nasreddine, Z. S. et al. The Montreal Cognitive Assessment, MoCA: a brief screening tool for mild cognitive impairment. J. Am. Geriatr. Soc. 53, 695–699 (2005)."
Greenberg S. A. Assessment of Fear of Falling in Older Adults: The Falls Efficiacy Scale-Internation (FES-I). Best Practices in Nursing Care to Older Adults. (The Hartford Institute for Geriatric Nursing, New York University, College of Nursing, New York, 2011).
Jonasson S. B., Nilsson M. H. & Lexell J. Psychometric properties of four fear of falling rating scales in people with Parkinson’s disease. BMC Geriatr. https://doi.org/10.1186/1471-2318-14-66 (2014).
Fritz, S. & Lusardi, M. White paper: “walking speed: the sixth vital sign”. J. Geriatr. Phys. Ther. 32, 46–49 (2009).
Chomiak, T. et al. A new quantitative method for evaluating freezing of gait and dual-attention task deficits in Parkinson’s disease. J. Neural Transm. (Vienna). 122, 1523–1531 (2015).
Hu, B. et al. AmbuloSono: a sensorimotor contingent musical walking program for Parkinson's disease rehabilitation. J. Parkinson Dis. 3, 146 (2013).
Shao, M. et al. Objective assessment of gait and walking ability in an outpatient neurology clinic. Neurology 86, P4.316 (2016).
Cihal, A. et al. Validation of a novel GaitReminder Apple iPod application to measure real-time stride data and control music play in a gait rehabilitation program for people with Parkinson’s disease. Mov. Disord. 28, S164 (2013).
Acknowledgements
We would like to thank the Canadian Institutes of Health Research, Alberta Innovates-Health Solutions, and Parkinson Alberta Society for their support. We would also like to thank Mr. Abhijot Singh Sidhu for his help with sensor measurements. T.C. was previously funded by MITACs, and S.N.T. was partially funded by the International Foundation of Ethical Research (IFER) based in Colorado. M.J.M. was supported through the UBC/PPRI Chair in Parkinson’s research.
Author information
Authors and Affiliations
Contributions
Research project design and execution: B.H., R.C., M.J.M., A.W., J.B., S.N.T., T.C.; Statistical and data analysis: T.C., A.W., B.H.; Manuscript: T.C. drafted the manuscript, and all other authors reviewed it.
Corresponding authors
Ethics declarations
Competing interests
B.H. invented the Ambulosono data system and GaitReminder App which is under investigational use. The remaining authors declare no competing interests.
Additional information
Publisher's note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Chomiak, T., Watts, A., Burt, J. et al. Differentiating cognitive or motor dimensions associated with the perception of fall-related self-efficacy in Parkinson’s disease. npj Parkinson's Disease 4, 26 (2018). https://doi.org/10.1038/s41531-018-0059-z
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41531-018-0059-z
This article is cited by
-
A novel single-sensor-based method for the detection of gait-cycle breakdown and freezing of gait in Parkinson’s disease
Journal of Neural Transmission (2019)