Abstract
We evaluated a new epilepsy genetic diagnostic and counseling service covering a UK population of 3.5 million. We calculated diagnostic yield, estimated clinical impact, and surveyed referring clinicians and families. We costed alternative investigational pathways for neonatal onset epilepsy. Patients with epilepsy of unknown aetiology onset < 2 years; treatment resistant epilepsy; or familial epilepsy were referred for counseling and testing. We developed NGS panels, performing clinical interpretation with a multidisciplinary team. We held an educational workshop for paediatricians and nurses. We sent questionnaires to referring paediatricians and families. We analysed investigation costs for 16 neonatal epilepsy patients. Of 96 patients, a genetic diagnosis was made in 34% of patients with seizure onset < 2 years, and 4% > 2 years, with turnaround time of 21 days. Pathogenic variants were seen in SCN8A, SCN2A, SCN1A, KCNQ2, HNRNPU, GRIN2A, SYNGAP1, STXBP1, STX1B, CDKL5, CHRNA4, PCDH19 and PIGT. Clinician prediction was poor. Clinicians and families rated the service highly. In neonates, the cost of investigations could be reduced from £9362 to £2838 by performing gene panel earlier and the median diagnostic delay of 3.43 years reduced to 21 days. Panel testing for epilepsy has a high yield among children with onset < 2 years, and an appreciable clinical and financial impact. Parallel gene testing supersedes single gene testing in most early onset cases that do not show a clear genotype-phenotype correlation. Clinical interpretation of laboratory results, and in-depth discussion of implications for patients and their families, necessitate multidisciplinary input and skilled genetic counseling.
Similar content being viewed by others
Introduction
Genetic testing and counseling for epilepsy is now being incorporated into everyday practice in many parts of the industrialised world.1 This advance has been driven by rapid discoveries in the aetiology of rare monogenic epilepsies, and technological developments in next generation resequencing (NGS).2 The integration of NGS testing into practice is accompanied by several challenges including clinician education, results interpretation, and counseling for patients and their families.3
We reflect on our experience of this transformational change from the perspective of a health service provider, specifically assessing: (a) the effectiveness and utility of NGS testing, (b) the necessary inputs and (c) areas where service improvements can be made to facilitate the transition to 'Precision' or 'Personalised Medicine'. We also asked specific questions about single vs parallel gene testing pathways based on clinician predictive ability; the relative diagnostic yield for different age of onset or epilepsy syndrome; what priorities clinicians and families identify; the resources necessary to provide an effective service, and whether NGS can save time and money4,5 using the neonatal epilepsy group as an example. We address these questions in the context of a review of the initial operation of a UK regional epilepsy genetics service to a population of approximately 3.5 million. To our knowledge there is limited published data from other specialist epilepsy genetics services that similarly reviews their own experience,6 therefore this study aims to fill a gap in that respect. However, there are several articles on the utility of genetic testing in epilepsy and published yield.2,7,8,9 Our study aims to add to the current literature and, in addition, fill in the gaps in knowledge about how to set up a tailored epilepsy genetics service, what referring clinicians and patients and families think about such a service, and the cost saving implications of performing genetic testing.
Results
Demographics
Ninety-six unrelated eligible patients (55 male) were referred to the service, either through the specialist outpatient clinic (n = 40) or directly for molecular investigation through their paediatrician or paediatric neurologist. All were consented for gene panel analysis. As this was a new service, many patients were tested years after onset or diagnosis, including one adult patient and two post-mortem. We categorized them broadly into age of onset and syndrome classes (Table 1). Sixty-four percent (49/77) were classified as drug-resistant.10
Identified variants
Seventy-four of our 96 patients had previous array comparative genomic hybridisation (aCGH) performed (77%), of which 16 (22%) had an identified benign chromosomal rearrangement. The remainder had no detected rearrangement and a normal chromosomal complement. Patients with pathological findings on the aCGH do not tend to make their way into our clinic. In fact, only three patients out of forty-four referred for aCGH by one of the three local clinicians we work with were found to have a pathogenic chromosomal rearrangement by the local laboratory (ViaPath) and were not referred on to our service: one showing Angelman’s syndrome; one Klinefelter’s syndrome; and one showing 9q34 deletion. However, the match between the epilepsy phenotype and the chromosomal rearrangement is not conclusive in any of these three cases so none of these can be considered completely 'solved'.
For NGS panel testing, 11 patients were tested on the original Childhood Epilepsy panel containing 45 genes (CHE-45); 11 on the CHE-76 (Childhood Epilepsy panel containing 76 genes); 49 on CHE-85 (Childhood Epilepsy panel containing 85 genes), and 23 on CHE-102 (Childhood Epilepsy panel containing 102 genes); 2 patients were referred to the epilepsy genetics service with existing positive gene panel results from another provider. The gene panel itself was designed by the following co-authors: RSM, DKP and HAD. The criteria for including a gene on the panel were that it should have been reported more than once in patients with monogenic epilepsies. The selection of genes on the panel was regularly evaluated and updated. The panel included of targeted capture of all exons and at least five base pairs of flanking intronic sequence of the selected genes.
The overall target coverage of the genes on the Amplexa CHE-46 panel was 95–97%; hence, 3–5% of the regions were not analyzed, and some variations may have been missed, while the average target coverage for the larger three panels was 98–99.5%. The regions missed were more or less identical across the different samples, i.e., regions difficult to amplify due to high GC content, repeat elements, or regions with homology in other parts of the genome.
Amplexa Genetics reporting follows the ACMG guidelines. However, there is an argument that these guidelines are not very suitable for conditions with variable penetrance (which many types of epilepsy have been shown to have). As our knowledge and understanding of epilepsy genetics is still limited, they do also report Class II (benign) variants, and this allows us to monitor them in case our understanding changes in the future. When we receive a report from Amplexa, we then compare that with our understanding of the phenotype to check whether this fits with the clinical picture. This often leads us to re-grade classifications of variants reported. If, however, we are still uncertain, we will request assistance from experienced colleagues in the field. Parental segregation may also lead to re-classification of variant class if the results fit with the phenotype or family history, e.g., 95% of SCN1A variants causing SMEI will be de novo. Parental segregation was deemed necessary when a class IV variant (defined as per the ACMG 2015 Guidelines11) or above was identified in the child, or a Class III variant was identified and it was in a gene that seemed to match with the child’s phenotype and/or family history, or in genes where de novo variants are usually pathogenic.
61% of patients (n = 59) had one or more variants (single nucleotide variants only) reported: 31 had only benign variants; 9 had variants of unknown significance (VUS), and 19 had variants judged to be of pathogenic significance. The average number of any variant, not just pathogenic, increased in line with the expansion in size of the gene panel (CHE-46: 1.3; CHE-102: 1.8) indicating the additional burden of clinical interpretation.12 We were constrained in our ability to retest panel negative cases because the testing was done under clinical auspices and therefore no patient with initial negative results were retested on a larger panel in this study. This means that the stated diagnostic yields probably underestimate what could have been achieved if everyone had been tested on the most up to date panel. The average turnaround time for results was 21 working days, less when no variants were seen (18 days) because Sanger validation was not necessary, and slightly more when parental segregation and new sample collection were necessary.
The pipeline used by Amplexa Genetics to establish pathogenicity of variants does indeed resemble other genetic testing NGS models.11,12,13 The panels used were designed to cover all coding exons and exon-intron boundaries of the included genes, including an additional 10 bp of the introns. Sequences were aligned to hg19 using the Torrent Suite (ThermoFisher) and SNPs with a read depth ≥ 20 and variant allele frequency of ≥0.25 were called using the Strand NGS software. Rare or low frequency variants were evaluated in an internally developed pipeline. Included in this evaluation were literature and database searches like Human Gene Mutation Database (HGMD), Exome Aggregation Consortium (ExAC) database, the Genome Aggregation Database (gnomAD). Synonymous variants and variants in autosomal dominant genes which had been observed more than three times or in homo-/hemizygous state in the ExAC/gnomAD database were excluded in severe epileptic encephalopathy (EE) cases. All variants were submitted to prediction tools—predictions on protein level were obtained from dbNSFP Functional Predictions and Cores 3.0 database while the variants were submitted to bioinfomatic software tools, e.g., NNSplice and ESEfinder for predictions on transcriptional level. The ACMG guidelines were applied to the resulting variants.11 Pathogenic variants are listed in Table 2: SCN8A (n = 4) and SCN2A (n = 3) were the two most commonly implicated genes. Two pathogenic variants were observed in SCN1A but not in typical SCN1A-associated generalised epilepsy with febrile seizures or Dravet syndrome cases. Variants of unknown significance were detected in GABRA5, SCN8A, CHRNB2, RYR3, HNRNPU, CACNA1A, SPTAN1, PIGA, KCNQ3, SLC2A1, NPRL3 and CHRNA4 (Table 3).
Variant yield
The yield varied according to age of seizure onset—Table 4 shows results by patient and, if a patient has several different variants they are classified by their most 'serious' ranked variant (pathogenic > VUS > benign). The 59 patients with at least one variant (benign, VUS and pathogenic included) had a total of 54 benign variants amongst them (17 patients had more than one benign variant and 6 had one or more benign variants plus a VUS or pathogenic variant as well); 9 variants of unknown significance; and 20 pathogenic variants (one patient had two variants in two different genes). 12 of the variants were Class 4 and 7 were class 5, as per the ACMG guidelines.11 The diagnostic yield, defined as the percentage of cases “solved” by NGS panel testing was highest in the neonatal onset epilepsies (63%), intermediate in the remaining first 2 years of life (21%), and lowest when onset was later (4%). The diagnostic yield was 23% among drug resistant cases. Clinicians attempted gene prediction (by informed guesses) in 33 cases, and were correct in five (15%): SCN1A, PCDH19, GRIN2A, CDKL5, SCN2A.9
Impact
In 63% of cases with pathogenic variants, the results had an immediate implication for treatment. Most involved ion channel subunit genes such as SCN1A, SCN2A, SCN8A, KCNQ2, leading to recommendations about Na + blocking antiepileptic drugs in 10 cases. Two cases with acetyl-choline receptor subunit variants that were suspected phenotype modifiers (CHRNA4, CHRNB2) were offered experimental nicotine therapy.14 It should be noted that the patient with the CHRNB2 VUS did not have his treatment altered because of this VUS. However, as we suspected it to be a phenotype modifier, he was offered the chance to try experimental nicotine therapy as an adjunctive treatment, to see if that had any impact on his seizures. One-quarter of cases were entered into a registry or research study. The families with pathogenic variants were offered expert genetic counseling: in six cases (31%) an additional affected relative was diagnosed.
Workshop and surveys
19 paediatricians and epilepsy nurses attended the workshop and all offered feedback. 100% agreed that the workshop was excellent and they were likely to change their practice going forward. We received 10 survey responses from families (25% response), and six from clinicians (40%). Both the outpatient and molecular diagnostic components of the service were rated as good or excellent (100%) by clinicians. Families also rated our services highly and 100% would recommend to friends and family (Table 5).
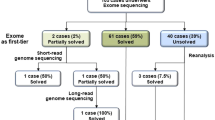
Investigational cost
We retrieved complete records for 16 neonatal epilepsy patients. Total investigation costs ranged from £5094 to £15,622, average £9362, with more than 75% of the costs allocated to neuroimaging and videoEEG-telemetry. In multiple linear regression, we found statistically significant and independent correlation only between diagnostic delay and cost of previous genetic tests (p = 0.011).
Prior single gene testing among this sample included Fragile-X (FMR1), Ataxia-Telengectasia (ATM), Niemann-Pick C (NPC1, NPC2), spinal muscular atrophy (SMN1, SMN2), Prader-Willi syndrome (15q11.2-q13), myotonic dystrophy (DMPK), ARX, atypical Rett syndrome (CDKL5), and Glutaric aciduria Type 1 (GAT1). Because both MRI and EEG can be performed for disease monitoring as well as diagnosis, we excluded these and focused on the remaining laboratory analyses performed on blood, urine and cerebrospinal fluid (CSF) samples. We found that two-thirds of these costs (total average per patient: £2004) were made up of array CGH and single gene tests, as well as metabolic investigations and invasive lumbar puncture. The delay between epilepsy onset and diagnosis ranged from 83 days to 17 years (median 3.4 years). Consequently, we calculated that if all neonatal epilepsy patients underwent NGS panel testing as part of their first line investigations, their theoretical total investigational costs would have averaged £2838, which is £6524 less (70%) than the actual average cost.
Discussion
NGS panel testing in epilepsy is largely effective and useful, and has particular strengths for early onset epilepsies. The high diagnostic yield in the neonatal (63%) and infant (21%) onset groups is unprecedented. We do not think there is any one answer as to why the yield was so high, however only selecting the most appropriate patients for testing and having a good panel design are of course very important factors.
There is a significant impact on treatment and risk counselling for the majority of genetically diagnosed cases.2 Families put a high value on exploring the implications of the results for their child and family; and referring clinicians appreciated the quality of clinical interpretation and rapid turnaround time.
The inputs required are substantial and complex: in our context, they were based on an existing integrated tertiary and secondary level regional epilepsy service, and relied on an educated referral base to select appropriate cases, an expert multidisciplinary team for interpreting variants with clinical features, and the skills of a specialized genetic counselor to translate findings into tangible benefits for families.
There is also a potential for huge reduction in investigation burden, cost and delay, taking into account the priorities of users and referrers.
Utility and effectiveness
Diagnostic yield and clinical impact
Yields of 10–48.5% have been reported from diagnostic NGS panels consisting of 36–265 target epilepsy genes,7,9,15,16,17,18,19,20 with a higher diagnostic yield in children under 2 years at seizure onset. We found patients with pathogenic variants in the most common epilepsy genes SCN8A (n = 4), SCN2A (n = 3), SCN1A (n = 2), KCNQ2 (n = 2) and STXBP1, GRIN2A, CHRNA4 (n = 1 each), accounting for 70% of all presumed disease-causing variants (Table 2). In all living cases involving Na or K channel mutations, recommendations or changes were made to antiepileptic medications. 9% of cases were entered into a clinical trial; 26% of cases were entered into a phenotype registry or study awaiting future trials, and families were introduced to online patient groups. Additionally, one quarter of patients had another relative diagnosed following their diagnosis. The rapid turnaround time of 21 working days (14 days for urgent cases) means interventions could be started in sufficient time to theoretically modify disease course or prevent complications, although the evidence base for such therapies is yet to be established.21 In addition, we found presumed pathogenic variants in epilepsy genes that have not been well characterized including HNRNPU, and the recessive PIGT (homozygous). 8 of the 20 pathogenic variants have previously been published7,8,15,22,23,24,25,26,27,28,29,30,31,32 a further 3 are listed in ClinVar (Table 2); while 9 are novel.
Single vs parallel gene testing
The philosophy of parallel testing or 'gene-first', in patients where a genetic cause is suspected but there is extensive genetic heterogeneity, is vindicated by clinicians’ limited ability to predict results, and by some remarkable surprises. Clinician prediction was not often attempted and we suspect this is because of the extreme genetic heterogeneity, pleiotropy, reduced penetrance and variable expression in infantile onset epilepsies, these factors providing the rationale for parallel gene testing.33,34 The cases in which prediction was attempted reflect examples where there is better known genotype-phenotype correlation. There are for example, some more specific clinical features that are characteristic of one, or a handful, of genes: clustering of febrile seizures (PCDH19); temperature sensitivity (SCN1A); etc. We discuss two case examples involving patients with pathogenic mutation in these genes in the discussion section.
Still there were many surprises as evidenced by the poor prediction rate. The full phenotypic spectra of many epilepsy genes are currently being reported in the literature; as part of our continuing clinician education for referring clinicians, we aim to disseminate this new knowledge to ensure that patients are accurately selected for genetic testing. The following three cases deserve discussion because they demonstrate the strong clinical foundation necessary for genetic testing in epilepsy.
The first was a 7-year-old child with early-onset (3 years) drug-resistant absence seizures preceded by multiple febrile seizures; her mother noted the absences were sensitive to high temperature. Her father had drug-responsive juvenile onset absence epilepsy. aCGH showed a paternally inherited 15q13.3 deletion, which explained the familial susceptibility to absence seizures, but not the daughter’s early age of onset, drug resistance, febrile seizures or heat sensitivity. Gene panel testing then revealed a de novo mutation in SCN1A, p.Arg1648His (Table 2).
The second had an onset of Lennox-Gastaut like symptoms in the first year of life, with severe learning difficulties including developmental regression of language and motor function at the age of 3. He had a pattern of nocturnal motor seizures clustering over several days, repeating three times per month, and was drug-resistant. NGS panel results showed pathogenic variants in HNRNPU (de novo) and CHRNA4 (inherited); the former explaining his overall phenotype, the second explaining his clustering nocturnal motor seizures. A trial of transdermal nicotine significantly reduced his nocturnal motor seizures and improved his daytime communication and functioning.14 Both this case and the SCN1A case exemplify how 'second hits' can modify a seizure phenotype and also act as a focus for therapeutic modulation.
The third case had severe clusters of infantile convulsions continuing for 48–72 h and recurring every few months with intercurrent febrile illness; at age 11 years he became seizure free on levetiracetam and now attends college. His clinical features resembled the seizure phenotype described in Epilepsy with Mental Retardation Limited to Females.35 NGS panel testing surprisingly revealed a mosaic heterozygous mutation in PCDH19. There are very few reported cases in males, and the genetic mechanism remains obscure.36
In the older age group (seizure onset > 2 years), the diagnostic yield was relatively low (4%). One reason is that far fewer genes have been discovered in later onset epilepsies, and this should prompt us towards more concerted efforts in collaborative gene discovery, especially in the focal epilepsies. However, it is likely that many of these later-onset epilepsies have a more complex aetiology and so even when we discover some of the associated genes, their impact on disease development will probably be modest and show wide variability of penetrance and expression amongst affected individuals.
Genes for autosomal dominant sleep-related hypermotor epilepsy, although among the first discovered (CHRNA4, CHRNB2, CHRNA2, KCNT1, DEPDC5, CRH, PRIMA1) still only explain approximately 10% of cases.37 Unfortunately, none of our five tested patients carried a causative mutation, suggesting that genetic testing is not cost-effective in differentiating nocturnal motor phenomena in adolescents. Only recently, new genes for familial focal epilepsy (FFE) have been reported from the GATOR1 pathway (DEPDC5, NPRL2, NPRL3) and these were missing from earlier versions of the gene panel CHE-46, CHE-76, CHE-85). While we speculate that some of our FFE patients might have tested positive, we note the low (0.8–12%) current yield in sporadic and FFE cases.38
We also noted the low yield for children with infantile or epileptic spasms. Infantile spasms are aetiologically heterogeneous: tuberous sclerosis is the most common single cause, followed by hypoxic-ischaemic injury, stroke and brain malformations, and 70% of cases have abnormal MR imaging.39 In a recent study of 44 unsolved infantile seizures cases, 7% had a de novo chromosomal rearrangement, and pathogenic mutations were revealed by trio exome sequencing in 28% of the remainder, suggesting that the diagnostic yield can be significant in fully investigated unsolved cases.40 Among our nine unsolved cases, a complete imaging, cytogenetic and metabolic screen had only been completed in one, suggesting room for better workup of these cases prior to NGS panel testing.
Necessary inputs
Clinical interpretation
Variant interpretation is not always straightforward, and requires close cooperation between molecular geneticist, bioinformatician, neurologist and genetic counsellor. We dealt with a large volume of benign (n = 54) or VUS (n = 11), which represents a substantial burden for clinical interpretation as well as a source of uncertainty for families. VUS arise for a number of reasons, e.g., inadequate bioinformatic prediction, lack of functional data, missing segregation, or incomplete knowledge of genotype-phenotype correlation. In this scenario, segregation information on a novel variant only contributes to diagnostic certainty when there is confidence about the bioinformatic prediction and the associated epilepsy phenotype. If the evidence is scant, then proving that the change is de novo, or segregates with disease in an affected parent will, in reality, make very little difference to the patient or family until further evidence establishes the VUS as likely pathogenic, or benign. Without expert interpretation, clinicians may be vulnerable to pitfalls such as over-interpreting variants as mutations or vice-versa,41 and wrongly assigning pathogenicity to heterozygous variants in recessive conditions.
Clinician education and health structure
Clinicians who understand the benefits and limitations of the service are able to offer it most effectively to the right patients. Our educational workshop was very useful in this regard, and most referrals that we received from workshop participants were appropriate and properly worked up beforehand. Without this hierarchical structure, there is the possibility of bypassing guidelines on investigation and wasting resources. However, clinical education is an ongoing process and continuing feedback on outcomes and beneficial impacts are probably necessary to sustain and grow referrals and appropriate NGS requests.
Genetic counseling
Despite universal access to the internet, many families have limited understanding of the principles of human genetics and require clear and relevant information, relayed in the context of their own situation before they can make an informed decision about genetic testing. Genetic counseling is the process of helping people understand and adapt to the medical, psychological, and familial implications of genetic contributions to disease.42 The genetic counselor is therefore ideally placed to discuss with the family: facilitating adaptation to their child’s condition, discussing the process and implications of genetic testing, as well as promoting informed choices, for now and in the future (e.g., family planning). A large proportion of genetic epilepsies are as a result of de novo mutations, and so cascade testing for the wider family is often not necessary. However, as germline mosaicism is now thought to be more common than it was originally,43 the possibility of prenatal testing in any future pregnancies is always discussed.
Re-engineering services for precision medicine
Clinician and family feedback
Clinicians valued the new specialist service, perceiving it helpful for diagnosis, management and counseling, and 50% believed it had saved additional investigations. Referrals increased over the course of the study, indicating an unmet need in the population. Families also found the experience of genetic counseling and testing helpful, regardless of whether their child’s case was solved or not. This feedback points to the need for informed and unhurried discussion around genetic testing, something that cannot be currently achieved in the current constraints of a general neurology clinic.
Cost saving
Clinician perceptions of cost-saving are supported by the analysis of neonatal epilepsy data, showing that investigation costs could be reduced by two-thirds by ordering an NGS panel earlier in the pathway, which has been noted before.2,4,5 This might also reduce the median diagnostic delay from 3.43 years to 21 days and feasibly allow the early use of disease-modifying drugs. However, true cost-savings are likely to be less than the theoretical and would need to be calculated using a prospective study design, preferably with a non-NGS tested concurrent control group. Such calculations may need to be repeated as technology evolves. Nevertheless, guideline revision requires consensus and commitment from multiple organizational stakeholders.
Limitations
While a prospective design has many advantages in terms of selection bias, there are a couple of limitations of this study. First, because our clinical pathway separates children with primary epilepsy from all children with early-onset seizures, and requires a routine workup to exclude lesional and some metabolic causes as well as excluding single gene testing for SCN1A and SLC2A1, the results may not be generalizable to other health care contexts. Second, our diagnostic yield concealed some variability because of the evolution of the gene panel over the period of study, reflecting the fast pace of gene discovery—this might have led to some under-diagnosis of patients using earlier panels.
Conclusion
NGS-based genetic testing has high clinical utility in children with epilepsy onset before 2 years or in drug-resistant or familial cases. The impacts are numerous and range from treatment change to risk counseling, and potential recruitment to clinical trials as new experimental therapies become available. A successful service requires strong engagement from secondary health care providers, an existing framework for specialist referral and investigation, substantial collaboration between clinicians and scientists for variant interpretation, as well as expertise in genetic counseling and flexibility in communicating with and meeting the evolving needs of families. To make the best of any innovation in medicine, health care organizations need to be open to change and reconfiguration of resources to benefit patients and their families.
Methods
Ethics
(a) Methods were performed in accordance with relevant regulations and guidelines and (b) methods were approved by The Great Ormond Street Hospital/Institute of Child Health Research Ethics Committee (reference number: 09/H0713/76).
Population
We collected prospective data related to genetic testing on 96 patients referred to the King’s Health Partners epilepsy genetics service for molecular diagnostic testing, between November 2014 and September 2016. The service is provided to the southeast region of England, a population of approximately 3.5 million including the south-east of London. The region includes two teaching hospitals with tertiary paediatric neurology departments (King’s College Hospital NHS Trust and Evelina London Children’s Hospital) and eleven district general hospitals in which there is a general paediatrician with a special interest in epilepsy. Medical services are state-run and organized through a regional clinical network with common management guidelines for epilepsy.44 Patients are seen first at their district general hospital before being referred, if appropriate, for a tertiary specialist opinion either at one of the two tertiary centres or in a regional specialist epilepsy clinic.
The epilepsy genetics service comprises two components: a specialist clinic run by a paediatric epileptologist with a research interest in genetics (DKP), a genetic counselor (SO) and clinical fellow (ST, RR); and a molecular genetic diagnostic service using an NGS epilepsy panel (LHGL, QH, HAD), with clinical interpretation by the whole team.
Pathway
In the absence of consensus guidelines, we considered patients suitable for genetic testing with either early-onset (<2 years) epilepsy, treatment resistant epilepsy of unknown cause, or familial epilepsy where the genetic cause was unknown. Two of our patients sadly died during the testing process. As a rule, we only considered patients with epilepsy as their primary diagnosis, rather than patients with intellectual disability (ID) or autism (ASD) who had seizures as part of their phenotype. This is because our service is part of the epilepsy service, whereas patients with primary ID or ASD who also have seizures do not usually use our pathway, unless they have a relevant family history. Patients followed one of three pathways for genetic testing: either being seen (i) in the specialist epilepsy genetic clinic, as above (n = 40); (ii) by a paediatric neurologist (n = 7) or paediatric epileptologist (n = 37) at one of the two tertiary centres; or (iii) seen by a general paediatrician (n = 12) with a special interest in epilepsy at a district general hospital, with referrals made in discussion with their linked paediatric epileptologist. Patients were recommended to have completed routine aetiological investigations as per regional guidelines (EEG, MRI, metabolic as necessary), and the clinician was asked to complete a proforma summarizing the electroclinical phenotype, epilepsy syndrome, age at seizure onset, drug response, results of previous investigations, and clinical prediction of candidate gene. We collected aCGH data in cases where it had been performed. Children with suspected typical Dravet Syndrome (OMIM 607208) or Glut-1 Deficiency syndromes (OMIM 606777) undergo single gene testing and were not included here; patients with brain malformations are tested on a separate gene panel and also not discussed here.
At the outpatient visit, we spent approximately 1 h with each new patient. The paediatric epileptologist and genetic counsellor took a detailed clinical and genetic history and performed a neurological examination on the affected child. Patients were operationally categorized into broad epilepsy syndromes (Table 1) because many did not fit into the International League Against Epilepsy classification of epilepsy syndromes.45 The genetic counselor then discussed the possibility of NGS panel testing, and if the family were interested, proceeded to explain: the process; benefits and limitations; potential outcomes and what they might mean; discussed any issues of concern that might arise around results, obtained written informed consent (using the appended consent form) prior to the start of this study, and planned for follow-up.
Education
We held a half-day educational workshop aimed at regional paediatricians and epilepsy nurses, to discuss which patients were suitable for testing, which test to choose and how to obtain informed consent. We designed the educational workshops along evidence-based lines for effective learning, using case-based simulations in small groups.46,47,48 After the workshop, attendees gave anonymous feedback indicating that 100% of them were 'likely' or 'very likely' to change their practice. We circulated proposed guidelines for genetic testing to the group which were agreed in consensus. Following this, in actual practice we have seen the number of referrals increase and that most referrals meet our published guidelines. Furthermore, the number of new referrers has increased and as we provide email feedback to every referrer, appropriateness is also improving amongst new referrers. Additionally, we posted separate information for clinicians and families on our website www.childhood-epilepsy.org.
Gene panel
We used the Amplexa Genetics epilepsy gene panel CHE-46 (46 epilepsy genes) at the start of the service,7 which was updated to CHE-76, CHE-85 and CHE-102 during the study period in light of new gene discoveries (by DKP, RM, HAD), (Table 6). To identify putative disease-causing variants, we performed targeted NGS of 46–102 epilepsy genes in four successive panels (January 2014—January 2016). The criteria for including a gene on the panel were that it should have been reported more than once in patients with monogenic epilepsies. The genes included on the CHE-46 panel were: ALDH7A1, ALG13, ARHGEF9, CACNA1A, CDKL5, CHD2, CPA6, DEPDC5, DNM1, GABRA1, GABBR1, GABBR2, GABRB3, GABRD, GABRG2, GNAO1, GRIN1, GRIN2A, GRIN2B, HCN1, HDAC4, HNRNPU, IQSEQ2, KCNA2, KCNQ2, KCNQ3, KCNT1, KCTD7, LGI1, MBD5, PCDH19, PLCB1, PNPO, PRRT2, SCN1A, SCN1B, SCN2A, SCN8A, SLC25A22, SLC2A1, SLC35A3, SPTAN1, STX1B, STXBP1, SYNGAP1, and TBC1D24; additionally for CHE-76: ADSL, ATP1A2, ATP1A3, ATRX, CHRNA2, CHRNA4, CHRNB2, GABRA5, GAMT, GATM, MECP2, MEF2C, MTOR, PIGA, PIK3AP1, PNKP, POLG, PURA, RYR3, SLC25A2, SLC6A1, SLC6A8, SLC9A6, SMARCA2, TCF4, UBE3A; and additionally for CHE-85: CLCN2, CNKRS2, FASN, FOXG1, HDAC4, HNRNPU, HUWE1, KCNH5, KCTD7, MBD5, PIGO, PIGT, RELN, SIK1, SLC13A5, SLC35A2, SLC35A3, SLC6A8, SLC9A6, ZDHHC9; and for CHE-102: CACNB4, CUX2, EEF1A2, GRIN2D, KANK1, KCNB1, KCNMA1, KIAA2022, NPRL2, NPRL3, PIK3R2, ST3GAL3, SZT2, WWOX. aCGH, where performed, was conducted using an oligonucleotide array with ~60,000 probes across the genome. Paternity testing was not performed.
Sample preparation
Genomic DNA was extracted from blood using standard methods. For the CHE-45, panel libraries were prepared from 15 ng of template DNA using the Ion AmpliSeq library 2.0 kit and custom primers following the manufacturer’s instructions (ThermoFisher Scientific).7 The CHE-76, CHE-85 and CHE-102 panel libraries were prepared from 1000 ng template DNA, Agilent SureSelect target enrichment (Agilent technologies) and KAPA library preparation kit (KAPA Biosystems) following manufacturer’s instructions. The library DNA was clonally amplified onto the Ion Spheres Particles (ISPs) by emulsion PCR using an Ion OneTouch 2 system and the Ion PGM Template OT2 200 kit (ThermoFisher Scientific). ISPs were sequenced on an Ion PGM sequencer using an Ion 314, Ion 316 or Ion 318 chip and the Ion PGM 200 Sequencing kit as per the manufacturer’s instructions (ThermoFisher Scientific).
Bioinformatics
Sequences were mapped to hg19 in the Torrent suite software (ThermoFisher Scientific) and variant calling was achieved in the Strand NGS software (Avadis) with a minimum of 20-fold read depth. Common SNPs with an allele frequency ≥ 2% and SNPs observed in more than 2 samples for each analyzed sample batch were filtered out. Genetic nonsynonymous/splice site variants were evaluated through database searches: dbSNP, Exome Variant Server, the Exome Aggregation Consortium database (ExAC), the Genome Aggregation Database (gnomAD) and HGMD Professional. Missense variants were also submitted to prediction softwares such as SIFT and PolyPhen-2, while splice site variants were evaluated by NNSPlice and Splicesite finder. Variants analyzed under a dominant inheritance model that were observed more than 10 times in ExAC were considered too common as monogenic causes. Potentially pathogenic variants were validated through conventional Sanger sequencing, and, if possible, parents were included for segregation analysis when indicated.
Criteria for assessing pathogenicity of rare variants
We share the brief clinical summary of the patient with the laboratory to aid genotype-phenotype correlation; subsequently we interpret the gene panel report in detailed clinical context at a monthly multidisciplinary meeting including epileptologists (EH, REW, KL, DKP), a clinical neurophysiologist (SG) and genetic counselor (SO). We also consulted bioinformatics databases, patient registries, expert colleagues and published literature. Laboratory reported variants categorized by the ACMG system11 were then (re-)classified by us as either benign variants, VUS, or pathogenic variants for the purposes of genetic counselling. For predicted possibly damaging variants where segregation analysis could be performed, we required the variant to meet one of the following criteria to constitute a likely pathogenic variant: de novo in early-onset severe epilepsy syndromes, segregation with the disorder, inheritance from an unaffected parent but previously reported in other families with the same phenotype and incomplete penetrance, or adherence to a recessive X-linked or parent-of-origin mode of inheritance.
Result feedback
We offered either a telephone or face-to-face consultation to the family, followed up with a written summary of the discussions in a letter.
Opinion survey
We solicited the views of all 40 families through an anonymous 16-item questionnaire available as paper copy or web version (www.surveymonkey.com). The questionnaire covered three main topics of quality, impact and perceived value, and was formulated with the assistance of the Head of Patient Experience at one of the tertiary centres. We also sent an email link to a 10-item anonymous (www.surveymonkey.com) questionnaire to all 15 clinicians who had referred patients to the epilepsy genetics service (questions were adapted from a longer survey used in the evaluation of SCN1A testing6).
Investigational cost
We searched electronic patient records to generate a list and timing of all investigations ordered in the neonatal epilepsy group; then matched these against 2017 hospital tariffs, separating them into categories of neuroimaging; EEG; routine blood tests; metabolic investigations of blood, urine and CSF; tissue biopsy; array CGH and karyotype; single gene tests; and NGS panel. We assessed the independent association of imaging, EEG, metabolic and genetic tests with diagnostic delay in days using multiple linear regression.
Data availability
All supporting data can be found as presented in this paper.
References
Pal, D. K., Pong, A. W. & Chung, W. K. Genetic evaluation and counseling for epilepsy. Nat. Rev. Neurol. 6, 445–453 (2010).
Berg, A. T. et al. Early-life epilepsies and the emerging role of genetic testing. JAMA Pediatr. 171, 863–871 (2017).
Poduri, A., Sheidley, B. R., Shostak, S. & Ottman, R. Genetic testing in the epilepsies-developments and dilemmas. Nat. Rev. Neurol. 10, 293–299 (2014).
Joshi, C. et al. Reducing the cost of the diagnostic odyssey in early onset epileptic encephalopathies. Biomed. Res. Int. 2016, 6421039 (2016).
Tan, T. Y. et al. Diagnostic impact and cost-effectiveness of whole-exome sequencing for ambulant children with suspected monogenic conditions. JAMA Pediatr. 171, 855–862 (2017).
Brunklaus, A. et al. The clinical utility of an SCN1A genetic diagnosis in infantile-onset epilepsy. Dev. Med. Child. Neurol. 55, 154–161 (2013).
Møller, R. S. et al. Gene panel testing in epileptic encephalopathies and familial epilepsies. Mol. Syndromol. 7, 210–219 (2016).
Butler, K. M. et al. De novo and inherited SCN8A epilepsy mutations detected by gene panel analysis. Epilepsy Res. 129, 17–25 (2017).
Trump, N. et al. Improving diagnosis and broadening the phenotypes in early-onset seizure and severe developmental delay disorders through gene panel analysis. J. Med. Genet. 53, 310–317 (2016).
Kwan, P. et al. Definition of drug resistant epilepsy: consensus proposal by the ad hoc Task Force of the ILAE Commission on Therapeutic Strategies. Epilepsia 51, 1069–1077 (2010).
Richards, S. et al. Standards and guidelines for the interpretation of sequence variants: a joint consensus recommendation of the American College of Medical Genetics and Genomics and the Association for Molecular Pathology. Genet. Med. 17, 405–424 (2015).
Eilbeck, K., Quinlan, A. & Yandell, M. Settling the score: variant prioritization and Mendelian disease. Nat. Rev. Genet. 18, 599–612 (2017).
Muzzey, D., Evans, E. A. & Lieber, C. Understanding the basics of NGS: from mechanism to variant calling. Curr. Genet. Med. Rep. 3, 158–165 (2015).
Brodtkorb, E. & Picard, F. Tobacco habits modulate autosomal dominant nocturnal frontal lobe epilepsy. Epilepsy Behav. 9, 515–520 (2006).
Lemke, J. R. et al. Targeted next generation sequencing as a diagnostic tool in epileptic disorders. Epilepsia 53, 1387–1398 (2012).
Carvill, G. L. et al. Targeted resequencing in epileptic encephalopathies identifies de novo mutations in CHD2 and SYNGAP1. Nat. Genet. 45, 825–830 (2013).
Kodera, H. et al. Targeted capture and sequencing for detection of mutations causing early onset epileptic encephalopathy. Epilepsia 54, 1262–1269 (2013).
Wang, J., Gotway, G., Pascual, J. M. & Park, J. Y. Diagnostic yield of clinical next-generation sequencing panels for epilepsy. JAMA Neurol. 71, 650–651 (2014).
Della Mina, E. et al. Improving molecular diagnosis in epilepsy by a dedicated high-throughput sequencing platform. Eur. J. Human. Genet. 23, 354–362 (2015).
Mercimek-Mahmutoglu, S. et al. Diagnostic yield of genetic testing in epileptic encephalopathy in childhood. Epilepsia 56, 707–716 (2015).
Chapman, K. E., Specchio, N., Shinnar, S. & Holmes, G. L. Seizing control of epileptic activity can improve outcome. Epilepsia 56, 1482–1485 (2015).
Vaher, U. et al. De novo SCN8A mutation identified by whole-exome sequencing in a boy with neonatal epileptic encephalopathy, multiple congenital anomalies, and movement disorders. J. Child. Neurol. 29, NP202–NP206 (2014).
Singh, R., Jayapal, S., Goyal, S., Jungbluth, H. & Lascelles, K. Early-onset movement disorder and epileptic encephalopathy due to de novo dominant SCN8A mutation. Seizure 26, 69–71 (2015).
Larsen, J. et al. The phenotypic spectrum of SCN8A encephalopathy. Neurology 84, 480–489 (2015).
Anand, G. et al. Autosomal dominant SCN8A mutation with an unusually mild phenotype. Eur. J. Paediatr. Neurol. 20, 761–765 (2016).
Parrini, E. et al. Diagnostic Targeted resequencing in 349 patients with drug-resistant pediatric epilepsies identifies causative mutations in 30 different genes. Hum. Mutat. 38, 216–225 (2017).
Wagnon, J. L. & Meisler, M. H. Recurrent and non-recurrent mutations of SCN8A in epileptic encephalopathy. Front. Neurol. 6, 104 (2015).
Zara, F. et al. Genetic testing in benign familial epilepsies of the first year of life: clinical and diagnostic significance. Epilepsia 54, 425–436 (2013).
Weckhuysen, S. et al. KCNQ2 encephalopathy: emerging phenotype of a neonatal epileptic encephalopathy. Ann. Neurol. 71, 15–25 (2012).
Depienne, C. et al. Genetic and phenotypic dissection of 1q43q44 microdeletion syndrome and neurodevelopmental phenotypes associated with mutations in ZBTB18 and HNRNPU. Hum. Genet. 136, 463–479 (2017).
Lemke, J. R. et al. Mutations in GRIN2A cause idiopathic focal epilepsy with rolandic spikes. Nat. Genet. 45, 1067–1072 (2013).
von Stulpnagel, C. et al. Epilepsy in patients with GRIN2A alterations: genetics, neurodevelopment, epileptic phenotype and response to anticonvulsive drugs. Eur. J. Paediatr. Neurol. 21, 530–541 (2017).
Grayton, H. M., Fernandes, C., Rujescu, D. & Collier, D. A. Copy number variations in neurodevelopmental disorders. Prog. Neurobiol. 99, 81–91 (2012).
Parker, L., Howlett, I. C., Rusan, Z. M. & Tanouye, M. A. Seizure and epilepsy: studies of seizure disorders in Drosophila. Int. Rev. Neurobiol. 99, 1–21 (2011).
Scheffer, I. E. et al. Epilepsy and mental retardation limited to females: an under-recognized disorder. Brain 131, 918–927 (2008).
Terracciano, A. et al. PCDH19-related epilepsy in two mosaic male patients. Epilepsia 57, e51–e55 (2016).
Tinuper, P. et al. Definition and diagnostic criteria of sleep-related hypermotor epilepsy. Neurology 86, 1834–1842 (2016).
Hildebrand, M. S. et al. A targeted resequencing gene panel for focal epilepsy. Neurology 86, 1605–1612 (2016).
Poulat, A. L. et al. A proposed diagnostic approach for infantile spasms based on a spectrum of variable aetiology. Eur. J. Paediatr. Neurol. 18, 176–182 (2014).
Michaud, J. L. et al. The genetic landscape of infantile spasms. Hum. Mol. Genet. 23, 4846–4858 (2014).
McCarthy, J. J. & Mendelsohn, B. A. The Significance of Unknown Significance: A Teachable Moment. Medcape Paediatrics. https://www.medscape.com/viewarticle/865546 (2016).
National Society of Genetic Counselors’ Definition Task, F.. et al. A new definition of Genetic Counseling: National Society of Genetic Counselors’ Task Force report. J. Genet. Couns. 15, 77–83 (2006).
Gajecka, M. Unrevealed mosaicism in the next-generation sequencing era. Mol. Genet. Genom. 291, 513–530 (2016).
National Institute for Health and Care Excellence. The Diagnosis and Management of the Epilepsies in Adults and Children in Primary and Secondary Care/cg137 (National, Institute for Health and Care Excellence, London, UK, 2012).
Berg, A. T. et al. Revised terminology and concepts for organization of seizures and epilepsies: report of the ILAE Commission on Classification and Terminology, 2005–2009. Epilepsia 51, 676–685 (2010).
Raza, A., Coomarasamy, A. & Khan, K. S. Best evidence continuous medical education. Arch. Gynecol. Obstet. 280, 683–687 (2009).
Davis, D. et al. Continuing medical education effect on practice performance: effectiveness of continuing medical education: American College of Chest Physicians Evidence-Based Educational Guidelines. Chest 135, 42S–48S (2009).
Bluestone, J. et al. Effective in-service training design and delivery: evidence from an integrative literature review. Hum. Resour. Health 11, 51 (2013).
Schwarz, J. M., Cooper, D. N., Schuelke, M. & Seelow, D. MutationTaster2: mutation prediction for the deep-sequencing age. Nat. Methods 11, 361–362 (2014).
Acknowledgements
We would like to thank all the children and families that were involved in this study, as well as the members of the South-East Thames Paediatric Epilepsy Group (SETPEG) for their attendance at our Education Day, and their feedback. We would also like to thank the Head of Patient Experience, Sarah Allen, at Guys and St Thomas’s Hospital for her help with our patient satisfaction questionnaire. Finally, we would like to thank all our referring clinicians: Dr. Elaine Hughes, Dr. Ruth Williams, Dr. Karine Lascelles, Dr. Katherine Anderson, Dr. Ming Lim, Prof. Paul Gringras, Dr. Rajesh Gupta, Dr. Nikil Sudarsan, Dr. Vasantha Gowda, Dr. Darshan Das, Dr. Lyvia Dabydeen and Dr. David McCormick. This work was supported by grants from the Canadian Institutes of Health Research (201503MOP-342469, DKP); European Union Programme of the Seventh Framework Programme Development of Strategies for Innovative Research to improve diagnosis, prevention and treatment in children with difficult to treat Epilepsy, 'DESIRE' (602531, DKP); National Institute for Health Research (DKP); Medical Research Council (DKP); Waterloo Foundation (DKP); Charles Sykes Epilepsy Research Trust (DKP); NIHR Specialist Biomedical Research Centre for Mental Health of South London and Maudsley NHS Foundation Trust (DKP).
Author information
Authors and Affiliations
Contributions
S.O.: writer and co-editor of paper; formulated, sent out and collated data from questionnaires. S.T.: phenotyping of patients and co-editor of paper. R.R.: phenotyping of patients and gave comments on the paper. R.L.: economic analysis. E.H.: phenotyping of patients and gave comments on the paper. R.W.: phenotyping of patients and gave comments on the paper. K.L.: phenotyping of patients and gave comments on the paper. L.H.G.L.: DNA extraction, NGS panel testing, Sanger Sequencing, and bioinformatic analysis. Q.H.: DNA extraction, NGS panel testing, Sanger Sequencing, and bioinformatic analysis. H.A.D.: bioinformatic analysis and gave comments on the paper. R.S.M.: clinical interpretation and gave comments on the paper. D.P.: Guarantor, and assisted with writing and editing of the paper.
Corresponding author
Ethics declarations
Competing interests
Stephanie Oates is part funded by Amplexa Genetics. The remaining authors declare no competing interests.
Additional information
Publisher's note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Oates, S., Tang, S., Rosch, R. et al. Incorporating epilepsy genetics into clinical practice: a 360°evaluation. npj Genomic Med 3, 13 (2018). https://doi.org/10.1038/s41525-018-0052-9
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41525-018-0052-9
This article is cited by
-
From precision diagnosis to precision treatment in epilepsy
Nature Reviews Neurology (2023)
-
Liquid biopsies in epilepsy: biomarkers for etiology, diagnosis, prognosis, and therapeutics
Human Cell (2022)
-
Application of Next-Generation Sequencing in Neurodegenerative Diseases: Opportunities and Challenges
NeuroMolecular Medicine (2021)
-
Rare deleterious mutations of HNRNP genes result in shared neurodevelopmental disorders
Genome Medicine (2021)
-
Impact of predictive, preventive and precision medicine strategies in epilepsy
Nature Reviews Neurology (2020)