Abstract
Clinical testing of BRCA1 and BRCA2 began over 20 years ago. With the expiration and overturning of the BRCA patents, limitations on which laboratories could offer commercial testing were lifted. These legal changes occurred approximately the same time as the widespread adoption of massively parallel sequencing (MPS) technologies. Little is known about how these changes impacted laboratory practices for detecting genetic alterations in hereditary breast and ovarian cancer genes. Therefore, we sought to examine current laboratory genetic testing practices for BRCA1/BRCA2. We employed an online survey of 65 questions covering four areas: laboratory characteristics, details on technological methods, variant classification, and client-support information. Eight United States (US) laboratories and 78 non-US laboratories completed the survey. Most laboratories (93%; 80/86) used MPS platforms to identify variants. Laboratories differed widely on: (1) technologies used for large rearrangement detection; (2) criteria for minimum read depths; (3) non-coding regions sequenced; (4) variant classification criteria and approaches; (5) testing volume ranging from 2 to 2.5 × 105 tests annually; and (6) deposition of variants into public databases. These data may be useful for national and international agencies to set recommendations for quality standards for BRCA1/BRCA2 clinical testing. These standards could also be applied to testing of other disease genes.
Similar content being viewed by others
Introduction
Clinical genetic testing of BRCA1 and BRCA2 began in the mid-1990s, but was mainly limited to one laboratory in the United States (US) and a small number of laboratories in Australia and Europe. Twenty-five years later the number and types of patients being offered BRCA1/BRCA2 testing has changed dramatically due in part to changes in patent laws and increased recognition of potential benefits of testing. Additionally, advances in high-throughput sequencing technology have enabled laboratories to offer tests that cover more genes. The testing panels are less expensive than older tests and feature shorter turn-around times (TAT). These changes in access and technology have led to a similarly intense increase over the last 10 years in the number of laboratories offering clinical genetic testing of BRCA1/BRCA2 specifically, multi-gene cancer gene panels for germline and somatic variant analysis, as well as companies that offer whole-exome and whole-genome studies that capture mutation information on these genes. This has led to a diverse array of options from which cancer genetics care providers can choose.
In 2013, a survey of 13 US laboratories offering BRCA1/BRCA2 sequence analysis revealed a large number of differences in technology, gene coverage, analytic sensitivities, ability to detect large rearrangements, cost, single-site analyses, and frequency of reporting variant of uncertain significance (VUS).1 Since 2013, many additional laboratories now offer BRCA1/BRCA2 testing, including laboratories that perform somatic mutation analyses. Given the expanded testing and challenges faced by clinicians and patients interested in comparing test offerings, the Breast Cancer Information Core (BIC) Steering Committee developed and administered a survey aimed to address the question of variation in clinical laboratory practices for BRCA1/BRCA2 testing around the world. The BIC is an open access, online database, which began in 1995, to catalog sequence variants in BRCA1/BRCA2.2 The goal of this study was to obtain a snapshot of current genetic testing laboratory practices for BRCA1/BRCA2 worldwide. We believe this study highlights similarities and differences between laboratories including technologies utilized, regions of the genes commonly assessed, as well as other quality control metrics employed. These findings help us to understand international differences in testing protocols and standards.
Results
Laboratory locations
Survey links were sent to BRCA1/BRCA2 genetic testing laboratories around the world. Every continent, except Antarctica, was represented by at least one testing laboratory (Fig. 1a). The bulk of testing laboratories responding to the survey were from Europe which reflects the demographics of the laboratories which were sent the survey invitation (Fig. 1b). Eight US laboratories completed the survey (Fig. 1c).
Geographical location of participating BRCA1/BRCA2 testing laboratories. The geographical location of participating laboratories is shown as pins on the world map for non-US laboratories (a), European laboratories (b), and US laboratories (c). Only laboratories that completed at least half of the survey questions are shown. Two of the US laboratories have overlapping pins as they are located in the San Francisco Bay Area. OpenStreetMap and ZeeMaps hold the copyright for the maps
Technologies used
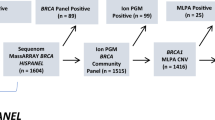
Massively parallel sequencing (MPS) was the most common method utilized by non-US laboratories to identify BRCA1/BRCA2 variants with the most common platforms being Illumina MiSeq (59%; 46 of 78 laboratories) and Ion Torrent (22%, 17 of 78 laboratories) (Fig. 2a). Of the 78 non-US laboratories responding, six reported Sanger sequencing as their only method of sequencing (8%) and 27 additional laboratories (35%) used Sanger as at least one modality, mostly to confirm variants identified by other methods. Twenty-six of 33 (79%) non-US laboratories reporting on both technology used and use of gene-panels include ten or more genes on their panel; seven laboratories reported using MPS for BRCA1/2 only. Many laboratories (31/78; 40%) reported using multiple technologies sequentially for initial discovery. There was less variability in the approach for large rearrangement analysis with 86% of non-US laboratories (66 of 77) utilizing multiplex ligation-dependent probe amplification (MLPA); however, 31% (24 of 77) also used data from a MPS platform, some noting that they used MLPA analyses to confirm rearrangements identified by MPS (Fig. 2b). Five of 77 laboratories (6%) did no duplication/deletion analyses, and one reported sending DNA to an external laboratory if no variants were detected by MPS. All eight US-laboratories used MPS technologies as one modality for sequence variant detection, and six reported using more than one technology (Fig. 2c). All US-laboratories responding offer gene panels and have panels available that include more than ten genes. Five of the eight US-laboratories also reported using Sanger sequencing, mostly for confirmation of variants found through other methods. Only half of the US laboratories used MLPA which differs from the non-US laboratories (66 of 77; 86%) (Fig. 2d). Seven of the US laboratories reported using more than one platform to identify large sequence variants; six used chromosomal microarray analysis or array comparative genomic hybridization (aCGH) (75%) in combination with MPS (five of eight; 63%). One US laboratory reported solely using MPS for detection of large sequence events.
Methods used for BRCA1/BRCA2 variant identification. The number and percentage of non-US (a/b) and US laboratories (c/d) reporting use of each method for identification of BRCA1/BRCA2 sequence variants (a/c) and large rearrangements (b/c) are noted. The percentage of laboratories reporting the use of more than one technology for variant detection was a 40%, b 38%, c 75%, and d 75%. Multiplex ligation-dependent probe amplification (MPLA); massively parallel sequencing (MPS); array comparative genomic hybridization (array CGH)
The survey did not specifically ask testing laboratories whether they only performed panel analyses, only if they performed single gene analyses or did both types of tests. However, laboratories indirectly answered this question when addressing TAT. All eight US laboratories responding to the survey offered panel-testing of multiple cancer susceptibility genes. Of the eight, only one does not offer single gene analysis. For the 47 non-US laboratories, 40 (85%) noted that they perform multi-gene panels; two did not respond to the BRCA1/BRCA2 only TAT question. Forty-five laboratories reported TAT for BRCA1/BRCA2 testing of which eight do not perform panel testing (18%).
Regions of BRCA1/BRCA2 sequenced
For BRCA1/BRCA2 analyses, coding exons were covered in full by all laboratories but only six of 70 non-US laboratories total (9%) and no US laboratories reported doing full intronic sequencing. Of the 54 non-US laboratories reporting the length of intronic sequence included in their tests, 30 (56%) sequenced 11–20 bp of intronic sequence, 12 (22%) sequenced 6–10 bp of intronic sequence and two laboratories sequenced up to 5 bp at intron/exon junctions (Fig. 3a). Twelve non-US laboratories responded with other answers including four laboratories that performed complete intronic sequencing. Twenty-three of 54 non-US laboratories (43%) sequenced non-intronic non-coding regions of BRCA1/BRCA2 including promoters, enhancers, 3′untranslated regions (UTRs), and 5′UTRs (Fig. 3b). US laboratories sequenced similar intronic regions as non-US laboratories with three sequencing 11–20 bp (43%), one sequencing 6–10 bp (14%), one sequencing 20 bp proximal to the 5′ end of an exon and 10 bp distal to the 3′ end of an exon (14%), one sequencing up to 5 bp of introns plus all previously established intronic variants (14%) and one sequencing all previously established intronic variants. Six of seven US laboratories reported sequencing additional non-intronic, regulatory regions of BRCA1/BRCA2. One laboratory noted that they reported variants in established clinically relevant non-coding regions. We did not ask specifically whether the laboratories reported sequence variants from these regions.
Non-coding regions assessed. Of 54 non-US laboratories reporting, the number that sequenced intronic regions (a) or non-coding non-intronic regions (b) are shown for different categories. Most of the intronic sequence refers to sequence near intron/exon boundaries. *Only sequencing previously established clinical relevant intronic variants. Other for introns includes multiple categories of size of introns and other for non-intronic regions includes “non-specified”, partial or only intronic non-coding regions. Twenty-seven laboratories answered the non-intronic regulatory regions of BRCA1/BRCA2 question
Variant confirmation
If a sequence variant was identified, over half of non-US (56%; 29 of 52) and US laboratories (71%, five of seven) confirmed all variants of uncertain significance (VUS), pathogenic and likely-pathogenic sequence variants by another method. Twenty-seven percent of non-US laboratories and 29% of US laboratories confirmed only pathogenic or likely pathogenic variants. Sanger sequencing was the most common method to validate variants (98%; 50 of 51 non-US laboratories and 86%, six of seven US laboratories), although 43% of US laboratories (three of seven) began confirmation by repeating analysis with the original technology. MLPA was used to confirm duplication or deletion variants in 61% of non-US laboratories (31/51) and 57% of US laboratories (3/7). Other methods used to confirm large rearrangements by US laboratories included aCGH, quantitative PCR (qPCR), and the PacBio system.
Coverage of Sequencing
There was a large range in both average read depth and minimum read depth required to meet quality assurances for MPS (Table 1). Of the 37 non-US laboratories reporting read-depths, the median read depth across all genes on their cancer gene platforms was 476 with an average read depth of 759. These values were lower for BRCA1/BRCA2 with a median read depth of 100 and an average read depth of 484. US laboratories reported a median read depth across all MPS platforms of 738 with a median of 425 and a higher read-depth for BRCA1/BRCA2 (average = 820, median = 500). Forty-two non-US laboratories reported a minimum read depth required for BRCA1/BRCA2 analysis; these ranged from 20 to 500 reads for BRCA1/BRCA2. When an exon failed to meet the minimum quality standards for that laboratory, most non-US laboratories used Sanger sequencing for the failed region (67%, 31 of 46) or a combination of repeating the entire or part of the assay and/or Sanger sequencing the affected region (22% 10 of 46). A small number of non-US laboratories repeated the entire assay (4%; 2 of 46) or repeated the assay around the affected region (2.1%, 1 of 46) without any Sanger sequencing. In contrast, four of the US laboratories (50%) repeated the entire assay and/or performed Sanger sequencing of the affected region.
Analytics-sensitivity/specificity
Forty-six non-US laboratories answered questions related to the analytical sensitivity of their BRCA1/BRCA2 testing. Of these, 16 (30%) had not calculated an analytic sensitivity for identification of known BRCA variants. Twenty-six non-US laboratories (52%) provided a value with an average analytical sensitivity of 98.3 and a median of 99. All eight US laboratories answered questions related to sensitivity and provided an estimated analytical sensitivity for detection of sequence variants with an average of 99.6% and a range of 98–100%. Seven of eight US laboratories reported the number of samples used to calculate the sensitivity with an average of 598, a median of 500, and a range of 20–1864.
The laboratories were also asked questions about the sensitivity, false discovery rate (FDR), and positive predictive value (PPV) of their method for identifying insertion/deletions (indels). Of the 24 non-US laboratories responding, 21% (5/24) did not know this information. Of the 16 laboratories that reported sensitivity as a value, the average was 97% and the median was 99.5% with a range of 85.2 to 100%. Four US laboratories reported a FDR with an average of 2.25%, a median of 2.5% and a range of 0–4. Multiple laboratories noted that FDR and PPV rates were difficult to determine. Of the 20 non-US laboratories responding with values, the average reliably detected indel size was 31 bp with a median of 21 bp and a range of 1–104 bp. One non-US laboratory, using Sanger sequencing, noted that they could reliably detect indels of less than 100 bp. For the five US laboratories responding, one noted that sensitivity, FDR, and PPV for indels were not calculated. For the other four laboratories, three noted a sensitivity of 100% with 95% confidence intervals of above 99.9% and a specificity of 100% and/or a FDR of 0%. Six US laboratories reported the size of reliably detected indels. Reliable detection varied between deletions and duplications; deletions of an average size of 33 bp with a median of 30 bp and a range of 20–40 bp and duplications of an average length of 23 bp, a median of 25 bp and a range of 10 to 40 bp were considered optimal for detection.
Variant classification
A number of variant interpretation guidelines were used. All reporting laboratories responded that variant interpretation was performed by in-house staff. For non-US laboratories, the majority had a board certified medical geneticist or molecular geneticist on their interpretation team (74%, 35/47). The remaining laboratories had genetic counselors, individuals with clinical genetics expertise related to the specific gene or an expert panel performed variant classification. Almost half of non-US laboratories (47%, 22 of 47) and 38% of US laboratories (3/8) reported using American College of Medical Genetics and Genomics (ACMG) guidelines for variant interpretation.3 The remaining laboratories reported using in-house guidelines (non-US laboratories 28% 13 of 47; US laboratories 63%) or country or organization-specific guidelines (non-US laboratories 21%). However, in the text descriptions, many of the laboratories using “in house” guidelines relied at least in part on guidelines from expert agencies. Guidelines or reference databases used to aid in classification included Evidence-based Network for the Interpretation of Germline Mutant Alleles (ENIGMA) (enigmaconsortium.org/library/general-documents), Vereniging Klinisch Genetische Laboratoriumdiagnostiek (www.vkgl.nl/nl), Association for Clinical Genomic Science (www.acgs.uk.com), and others.4 Laboratories described a mixture of different resources and databases used to help in classification including ClinVar, literature searches, Alamut Visual (www.interactive-biosoftware.com/alamut-visual), Sorting Intolerant From Tolerant (SIFT)(sift.jcvi.org), Polyphen2 (genetics.bwh.harvard.edu/pph2), dbSNP (www.ncbi.nlm.nih.gov/projects/SNP), Breast Information Core Database (BIC)(research.nhgri.nih.gov/bic), Leiden Open Variation Database (LOVD)(www.lovd.nl/3.0/home), Universal Mutation Database (UMD)(www.umd.be/BRCA1), and BRCA Exchange (brcaexchange.org).5,6,7,8,9
Interpretation of VUS is an important clinical issue. Interestingly, more than half (52%, 24 of 46) of the responding non-US laboratories had not specifically calculated their BRCA1/BRCA2 VUS rates. Of those that determined their rate of BRCA1/BRCA2 VUS, these varied widely from 3–50% with an average and median VUS rate for BRCA1 of 14 and 13% and for BRCA2 of 16 and 13%. Some caution should be taken for interpretation of these figures as the definition of VUS (e.g., all VUS versus VUS per individual) and thresholds for calling vary between laboratories; also some laboratories may have reported all sequence variants and not just VUS (Supplemental Table 1). For the five US laboratories that calculated BRCA1/BRCA2 VUS frequencies, the percentage of individuals/tests with a VUS ranged from less than 2 to 6%. Segregation analyses can be helpful for classifying variants. Seventy percent (33 of 47) of non-US laboratories offered variant-specific testing for family members when a VUS was identified and another 15% of laboratories (7 of 47) offered VUS testing depending on the circumstance. All US laboratories offered VUS-family studies, but testing was limited to defined circumstances (Supplementary Table 2).
As VUS can be reclassified as additional data become available, we asked how often laboratories reclassified VUS. Most non-US laboratories (57%, 27 of 47) specified that reclassification was done on an ad hoc basis, 9% (4 of 47) re-assessed VUS at least annually, and 23% of laboratories (11 of 47) re-assessed VUS every 1–3 years. Three non-US laboratories did not reassess variants (6%). This is in contrast to US laboratories in which 57% (four of seven) reassessed variants less than once a year, 29% (two of seven) reclassified variants on an ad hoc basis and one laboratory reassessed VUS every 1–3 years. One US laboratory reported that VUS were assessed daily due to automated reclassification tools used in real time. When a VUS was reclassified, regardless of classification, all eight US laboratories and 39% (18/46) of non-US laboratories recontacted the ordering provider. Thirty-three percent (15/46) of non-US laboratories recontacted the ordering provider only when the VUS had been reclassified as pathogenic or likely pathogenic. The remaining non-US laboratories did not automatically contact the ordering physician (11%, 5 of 46) or only did so when asked by the ordering provider (13%, 6 of 46).
To aid in classifying missense and other non-truncating variants as pathogenic or not, it is useful to know how frequently a variant has been observed in populations being tested. One third of non-US laboratories (36%, 16 of 45) did not report any variants to any databases, one third (33%, 15 of 45) shared BRCA1/BRCA2 data with multiple open-access databases, and the remainder of labs reported to only one database (22%, 10 of 45) or to private or member-only databases (9%, 4/45). Of laboratories that reported variants the most common databases were LOVD (40%, 18 of 45), BIC (36%, 16 of 44) and ClinVar (27%, 12 of 45). US laboratories were more likely to submit sequence data to public databases. Seven of eight US laboratories (88%) reported sequence variants to ClinVar; one laboratory did not report to public or private databases.
Testing volume
Variant interpretation, TAT, and some quality measures may be impacted by the testing volume. There was significant variation among laboratories responding to this survey question. Forty-three non-US laboratories described the number of BRCA1/BRCA2 tests performed between October 2015 and September 2016; the number of tests ranged from 2 to 2025 with an average number per year of 568 and a median of 300. Twelve laboratories performed fewer than 100 tests per year. Only three US laboratories answered the question on the number of tests performed in the year from October 2015 to September 2016. The range was ~45,000 to 252,223 which surpassed all non-US laboratories by an order of magnitude (maximum of 2025); this may be influenced by population size of country, the length of time that testing has been available to clinicians, country-specific guidelines for testing, and differences in marketing practices.
Client-related concerns
When there is a choice of laboratory and the patient and primary care provider are using BRCA1/BRCA2 testing results to aid in surgical decision making, TAT is an important consideration. Of 38 non-US laboratories reporting, there was an average TAT for gene-panel testing of 6.5 weeks with a median of 5.6 weeks and a range of 11 days to 6 months. For BRCA1/BRCA2 single-gene or small panel analysis specifically, there was an average TAT of 4.9 weeks (median = 4.0 weeks, range 0.5–4 months) for the 45 laboratories responding. This contrasts with US laboratories that had a much shorter average TAT of 2.4 weeks for gene-panels of over ten genes with a median of 2.6 weeks and a range of 1.1 to 3.5 weeks. For single gene analysis or small panels (six US laboratories reporting), there was an average TAT of 1.7 weeks with a median of 1.5 weeks and a range of 6.5 days to 2 weeks. One US laboratory noted that there were additional options to expedite test results if requested. To determine if TAT was influenced by the number of tests performed per year, we plotted the TAT for BRCA1/BRCA2 tests in days by number of tests performed per year for the three US laboratories and 38 non-US laboratories for which both values were present (Fig. 4). There was no correlation between TAT and testing volume (Pearson’s correlation all labs combined = −0.28; non-US labs only was 0.02). There was also no correlation between dedicated staff and TAT (Pearson’s correlation for all labs = −0.14; non-US labs = 0.009). There was a negative correlation for US laboratories with decreased TAT associated with increased numbers of staff and increased testing volume, but these were based on only three US laboratories (Pearson’s correlation US labs = −0.72 and −0.76, respectively).
Turn-around time per testing volume. The turn-around time (TAT) in days is plotted as a function of number of BRCA1/BRCA2 tests performed in a one-year time period for the three US laboratories and 38 non-US laboratories who reported values for both questions. US laboratories are indicated by a circle. No correlation was found between TAT and testing volume for all 41 laboratories or the 38 non-US laboratories (Pearson’s correlation = −0.23 and 0.02 respectively)
Laboratories were asked whether there were national or regional guidelines to determine when to order a test and which genes to include on clinical tests for hereditary cancer syndromes (Supplemental Table 1 and 2). For the seven US laboratories that responded, three (43%) depended on the referring physician to determine appropriateness, two (29%) used National Comprehensive Cancer Network and/or payer/insurance guidelines and one (14%) used insurance carrier guidelines. For non-US laboratories, almost half (20 of 41 laboratories) depended on the ordering physician to determine the test being ordered and the other half (21 of 41) used specific guidelines. The specific guidelines for inclusion of a gene on a clinical panel for non-US laboratories varied: 12 of 41 laboratories (29%) had no country-specific guidelines, eight (20%) had defined genes that were covered by insurance, and 20 laboratories (49%) had regional or national level guidelines.
Discussion
To our knowledge, this is the first international survey of laboratories performing clinical testing of BRCA1/BRCA2 since the adaptation of MPS. MPS use for clinical testing has been predicted to introduce challenges in workflow, interpretation, and result reporting.10 By sampling the variety of technological approaches used by testing laboratories and highlighting similarities and differences, our goal is to provide information for testing laboratories and agencies providing guidelines for quality laboratory practices.
Across the world, MPS platforms were the preferred method for detection of non-rearrangement BRCA1/BRCA2 sequence variants. All laboratories interrogated all coding BRCA1/BRCA2 exons with varying lengths of introns sequenced. Although many survey responses were similar between non-US and US laboratories, our survey revealed some key differences. Non-US laboratories were more likely to use MLPA as one modality for large rearrangement detection (86%) compared to US laboratories (50%) who were more likely to use aCGH (75%) and MPS (88%). Most US and non-US laboratories utilized MPS as the prime modality for variant detection, but perhaps due to testing volume, more non-US laboratories used Illumina MiSeq (59%) instead of the higher capacity Illumina HiSeq used by most US laboratories (63%). US laboratories were much more likely to use in-house methods of classifying VUS (63%) compared to non-US laboratories (26%). Non-US laboratories were more likely to use country-specific or expert panel-specific BRCA1/BRCA2 guidelines (21%); although three of eight US laboratories used ACMG or modified ACMG guidelines.3 US laboratories were more likely to share sequence results with public databases (88% reported to ClinVar) than non-US laboratories (55% reported to at least one public database). Importantly, over one third of non-US laboratories did not report variants to any databases or only reported to private/member only sites (9%). From a client point of view, US laboratories have a substantially shorter average TAT for BRCA1/BRCA2 or small gene panels. This difference may be driven by competition between companies in the US, the distribution of commercial versus academic laboratories, and/or differences in insurance coverage versus national health care coverage for testing. Finally, responding US laboratories performed many more BRCA1/BRCA2 tests (lowest reported 45,000) per year relative to non-US laboratories (range 1–2025), although only a small number of US laboratories answered this question. The vast difference in testing volume between US and non-US laboratories may be due in part to differences in the population size of responding countries or in numbers of patients referred for BRCA1/BRCA2 testing. There was a strong correlation for US laboratories between TAT and number of BRCA1/BRCA2 tests performed annually (Pearson’s correlation = −0.76); however there was no correlation for non-US laboratories (Pearson’s correlation = 0.02).
Although we aimed to do a global survey, a limited number of laboratories from Africa, South America, and Asia were sent direct survey links. As the survey was in English, language differences also may have contributed to a low response rate for laboratories in Asian, African, and South American countries. Additionally, as the survey was lengthy and some questions required additional research, some laboratories may not have participated. The US-response rate was low (8 of 27), but because some of the surveys to the non-US laboratories were sent by others through laboratory networks, we are unable to calculate response rate. This survey was not comprehensive and may be missing information on some key differences in practices, such as method of library preparation for MPS and rationale for choice of technologies utilized. Additionally, this survey was not designed to compare sensitivity and specificity of pathogenic variant detection or VUS calling which is an important consideration for establishing best practices. Finally, we did not collect information on the rationale behind the choice of technologies for each laboratory which could be useful for laboratories updating technologies for BRCA1/2 variant identification.
In conclusion, this study shows that there are key similarities in technology used for BRCA1/BRCA2 sequence and rearrangement analysis around the world. There was variation in laboratory-specific quality criteria for average and minimum numbers of read depths which could impact sensitivity. Laboratories reported VUS at varying rates, but also calculated rates of VUS differently. Based on these results and two recent studies, one showing a 2.6% diagnostic error rate for detection of pathogenic and significant variants using MPS approaches,11 and a second study suggesting that only two of seven MPS workflows could detect all 23 “challenging variants” in a blinded study12, we suggest points for consideration for laboratories performing or contemplating BRCA or panel testing (Fig. 5). These points for consideration (Fig. 5) are complemented by those from other groups, such as the Association for American Pathologist and the College of American Pathologist who have developed standards and guidelines for MPS Bioinformatics pipelines used in clinical tests.13 Of critical note, global data sharing of variants with sufficient data to allow multiple lines of evidence without duplication would facilitate variant reclassification and a central alert system to improve the quality of variant analysis and ensure more consistent management of high risk gene carriers as has been highlighted recently.14,15 Due to the diversity across laboratories, this study highlights the opportunity for international organizations to formulate guidelines for laboratories performing BRCA1/BRCA2 genetic testing.
Materials and methods
Survey
Two online surveys were developed: one for non-US laboratories and one for US laboratories that included questions specific to the US (Supplementary Notes 1 and 2). Each survey had four sections: 1: Testing Laboratory Information, 2: Multigene Hereditary Cancer Panels, 3: Variant Assessment; and 4: Staffing, Billing and Other Client-Support Related Questions. Surveys were developed using Qualtrics Survey Software (Qualtrics, Provo, UT and Seattle, WA).
Distribution of survey
Initial links to surveys were sent on 1 December 2016. Contact names and potential testing laboratories were identified through the BIC Steering Committee contacts, Google searches and mass e-mails sent from coordinators of the European Molecular Genetics Quality Network and United Kingdom National External Quality Assessment Service for Molecular Genetics to all genetics testing laboratories in their networks. Twenty-seven US laboratories were sent the survey. Survey links were distributed over a 4-month period. The international survey closed to new respondents on 29 March 2017 and the US survey closed to new respondents on 9 May 2017. For the non-US laboratories, 78 laboratories answered some questions, and 48 of those fully completed the survey, although some questions were not applicable to all laboratories (Supplementary Table 1). Eight US laboratories responded to the survey (Supplementary Table 2). The number of laboratories answering each question is included for each data point as the denominator varies.
Data analysis
Summary data and frequencies were tallied in Qualtrics. As some questions had “click all that apply” answers, the percentage and number of laboratories responding are both reported. When a range of values was reported (e.g., 500–1000 read depth), the mid-point was used in the calculation (e.g., 750 reads). When a greater than or less than symbol was included (e.g., >100), the numerical value was used in the calculation. Answers related to time were converted to weeks.
Map generation
The geographical locations of the participating laboratories were mapped by plotting the latitude and longitude markers obtained from the IP address of the individual completing the survey using ZeeMaps (https://www.zeemaps.com).
Data availability
The authors declare that all of the data supporting the findings of this study are available within the paper and its supplementary information files.
References
Forman, A. & Daly, M. Comparing commercial genetic testing laboratories (US) offering multigene hereditary cancer panels. Paper presented at Sixth International Symposium on Hereditary Breast and Ovarian Cancer. Montreal, Quebec, Canada, May 10–13, 2016.
Szabo, C., Masiello, A., Ryan, J. F. & Brody, L. C. The breast information core: database design, structure and scope. Hum. Mutat. 16, 123–131 (2002).
Richards, S. et al. Standards and guidelines for the interpretation of sequence variants: a joint consensus recommendation for the American College of Genetics and Genomics and the Association for Molecular Pathology. Genet. Med. 17, 405–424 (2015).
Wallis, Y. et al. Practice guidelines for the evaluation of pathogenicity and the reporting of sequence variants in clinical molecular genetics. Association for Clinical Genetic Sciences. http://www.acgs.uk.com/media/774853/evaluation_and_reporting_of_sequence_variants_bpgs_june_2013_-_finalpdf.pdf. (2013).
Landrum, M. J. et al. ClinVar: public archive of interpretations of clinically relevant variants. Nucleic Acids Res. 44, D862–D868 (2016).
Kumar, P., Henikoff, S. & Ng, P. C. Predicting the effects of coding non-synonymous variants on protein function using the SIFT algorithm. Nat. Protoc. 4, 1073–1081 (2009).
Adzhubei, I., Jordan, D. M. & Sunyaev, S. R. Predicting functional effect of human missense mutations using PolyPhen-2. Curr. Protoc. Hum. Genet. 76.20.1–7.20.41 (2013).
Fokkema, I. F. et al. LOVD v.2.0: the next generation in gene variant databases. Hum. Mutat. 32, 557–563 (2011).
Caputo, S. et al. Description and analysis of genetic variants in French hereditary breast and ovarian cancer families recorded in the UMD-BRCA1/BRCA2 databases. Nucleic Acids Res. 40, D992–D1002 (2012).
Wallace, A. J. New challenges for BRCA testing: a view from the diagnostic laboratory. Eur. J. Hum. Genet. 24, S10–S18 (2016).
Ellison, G., Wallace, A., Kohlmann, A. & Patton, S. A comparative study of germline BRCA1 and BRCA2 mutation screening methods in use in 20 European clinical diagnostic laboratories. Br. J. Cancer 117, 710–716 (2017).
Lincoln, S. et al. An interlaboratory study of complex variant detection in clinical testing (Abstract/Program 230). Presented at the 67th Annual Meeting of the American Society of Human Genetics, October 20, 2017, Orlando, Florida.
Roy, S. et al. Standards and guidelines for validating next-generation sequencing bioinformatics pipelines: a joint recommendation of the association for molecular pathology and college of American pathologists. J. Mol. Diagn. 20, 4–27 (2017).
Lincoln, S. E. et al. Consistency of BRCA1 and BRCA2 variant classifications among clinical diagnostic laboratories. JCO Precis. Oncol 1: https://doi.org/10.1200/PO.16.00020 (2017).
Lebo, M. S. et al. Data sharing as a national quality improvement program: reporting on BRCA1 and BRCA2 variant-interpretation comparisons through the Canadian Open Genetics Repository (COGR). Genet. Med. https://doi.org/10.1038/gim.2017.80. (2017).
Acknowledgements
We thank the laboratory personnel and directors for taking the time to complete these surveys. Simon Patton and Zandra Deans kindly distributed the survey link for this study to their clinical laboratory networks: EMQN and UK NEQAS for Molecular Genetics. David Kaufman, NHGRI provided advice on the structure of the survey. The BIC steering committee provided thoughtful discussion on survey questions and data presentation and international laboratory contacts. This work was supported in part by the Intramural Research Program of the National Human Genome Research Institute and by the Intramural Research Program, Center for Cancer Research, National Cancer Institute. A.N.M. is funded by the Florida Breast Cancer Foundation. S.L.N. is the Morris and Horowitz Families Endowed Professor. A.B.S. is funded by a National Health and Medical Research (NHMRC) Senior Research Fellowship. W.D.F. is funded by the Canadian Institute for Health Research.
Author information
Authors and Affiliations
Consortia
Contributions
All authors designed the study and the survey. Surveys were distributed by A.F. and A.E.T. A.E.T. analyzed and curated the data. A.E.T. and A.F. wrote the manuscript: All authors edited the manuscript and approved the final paper. All authors have accountability for all aspects of work.
Corresponding author
Ethics declarations
Competing interests
A.F. is a paid advisor and speaker for Ambry and Invitae. S.E.P. is on the scientific advisory board of Baylor Genetics. The remaining authors declare no competing financial interests.
Additional information
Publisher's note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Toland, A.E., Forman, A., Couch, F.J. et al. Clinical testing of BRCA1 and BRCA2: a worldwide snapshot of technological practices. npj Genomic Med 3, 7 (2018). https://doi.org/10.1038/s41525-018-0046-7
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41525-018-0046-7
This article is cited by
-
Gene-specific machine learning for pathogenicity prediction of rare BRCA1 and BRCA2 missense variants
Scientific Reports (2023)
-
Decision thresholds with genetic testing
The European Journal of Health Economics (2022)
-
Homologous recombination proficiency in ovarian and breast cancer patients
BMC Cancer (2021)
-
A novel BRCA1 duplication and new insights on the spectrum and frequency of germline large genomic rearrangements in BRCA1/BRCA2
Molecular Biology Reports (2021)
-
Mutations of BRCA2 in canine mammary tumors and their targeting potential in clinical therapy
BMC Veterinary Research (2020)