Abstract
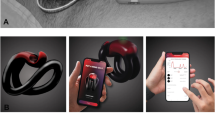
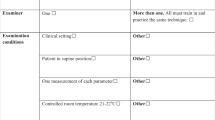
Assessment of Peyronie’s disease with penile injection is invasive and uncomfortable. We developed a smartphone application (UWPEN) to assess penile angulation in the home environment. The purpose of this study was to compare clinician and patient measurements and assess the patient experience with UWPEN in a clinical setting. We prospectively enrolled patients with Peyronie’s disease undergoing intracavernosal injection of alprostadil. Penile angulation and narrowing were then assessed by patients and clinicians using UWPEN and compared to values obtained via a goniometer and a ruler (gold standard). Measurements were compared using the Pearson correlation test. Upon completion of measurements, patients were surveyed regarding the ease of use, confidence with use, and measurement preferences. Twenty patients were enrolled in the study; two patients were excluded for poor penile turgidity after a maximum dosage of intracavernosal alprostadil. Correlation between UWPEN and gold standard measurements by patients and clinicians was R = 0.55 (p = 0.01) and R = 0.87 (p < 0.01) for dorsal measurements, R = 0.62 (p = 0.01) and R = 0.77 (p < 0.01) for lateral measurements, and R = 0.73 (p < 0.01) and R = 0.64 (p < 0.01) for girth measurements, respectively. Prior evaluation of correlation suggests a strong correlation at R = 0.8, and good correlation at R = 0.5. Overall, patients preferred using UWPEN to traditional measurements, and 75% reported UWPEN as their first preference for measurements. UWPEN enables patients to assess their disease severity with good correlation to gold standard measurements. Patients prefer mobile platforms for disease monitoring, and development of technology for disease monitoring should be a priority within the Peyronie’s disease research community.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 8 print issues and online access
$259.00 per year
only $32.38 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout




Similar content being viewed by others
References
Schwarzer U, Sommer F, Klotz T, Braun M, Reifenrath B, Engelmann U. The prevalence of Peyronie’s disease: results of a large survey. BJU Int. 2001;88:727–30.
Kadioglu A, Oktar T, Kandirali E, Kendirci M, Sanli O, Ozsoy C. Incidentally diagnosed Peyronie’s disease in men presenting with erectile dysfunction. Int J Impot Res. 2004;16:540–3.
Mulhall JP, Creech SD, Boorjian SA, Ghaly S, Kim ED, Moty A, et al. Subjective and objective analysis of the prevalence of Peyronie’s disease in a population of men presenting for prostate cancer screening.J Urol. 2004;171(Pt 1):2350–3.
Lue T. Peyronie’s disease: an anatomically-based hypothesis and beyond. Int J Impot Res. 2002;14:411–3.
Terrier JE, Nelson CJ. Psychological aspects of Peyronie’s disease. Transl Androl Urol. 2016;5:290–5.
Nehra A, Alterowitz R, Culkin DJ, Faraday MM, Hakim LS, Heidelbaugh JJ, et al. Peyronie’s Disease: AUA Guideline. J Urol. 2015;194:745–53. Available from: https://www.jurology.com/doi/10.1016/j.juro.2015.05.098.
Brant WO, Bella AJ, Lue TF, Hon S. Peyronie’s disease: diagnosis and medical management. UpToDate. 2013. https://www-uptodate-com.offcampus.lib.washington.edu/contents/peyronies-disease-diagnosis-and-medical-management?source=search_result&search=peyronies disease diagnosis and medical management&selectedTitle=1~150. Accessed 18 Apr 2017.
Bacal V, Rumohr J, Sturm R, Lipshultz LI, Schumacher M, Grober ED. Correlation of degree of penile curvature between patient estimates and objective measures among men with Peyronie’s disease. J Sex Med. 2009;6:862–5.
Hsi RS, Hotaling JM, Hartzler AL, Holt SK, Walsh TJ. Validity and reliability of a smartphone application for the assessment of penile deformity in Peyronie’s disease. J Sex Med. 2013;10:1867–73.
Wessells H, Lue TF, Mcanincht JW. Penile length flaccid erect states: guidelines penile augmentation. 1996;156:996–7.
Guyatt G, Walter S, Shannon H, Cook D, Jaeschke R, Heddle N [statistics * statistique]. Basic statistics for clinicians: 4. Correlation and regression. https://www-ncbi-nlm-nih-gov.offcampus.lib.washington.edu/pmc/articles/PMC1337703/pdf/cmaj00064-0047.pdf. Accessed 3 Jan 2018.
Ebrahim S, Walter SD, Cook DJ, Jaeschke R, Guyatt G. Correlation and regression. In: Guyatt G, Rennie D, Meade MO, Cook DJ, editors. Users’ guides to the medical literature: a manual for evidence-based clinical practice. 3rd ed. New York, NY: McGraw-Hill Education; 2015.
Byrom B, Doll H, Muehlhausen W, Flood E, Cassedy C, McDowell B, et al. Measurement equivalence of patient-reported outcome measure response scale types collected using bring your own device compared to paper and a provisioned device: results of a randomized equivalence trial. 2018. https://doi.org/10.1016/j.jval.2017.10.008.
Ohebshalom M, Mulhall J, Guhring P, Parker M. Measurement of penile curvature in Peyronie’s disease patients: comparison of three methods. J Sex Med. 2007;4:199–203.
Manganello JA, Gerstner G, Pergolino K, Graham Y, Strogatz D. Understanding digital technology access and use among New York state residents to enhance dissemination of health information. JMIR Publ Heal Surveill. 2016;2:e9
Connolly SL, Miller CJ, Koenig CJ, Zamora KA, Wright PB, Stanley RL, et al. Veterans’ attitudes toward smartphone App use for mental health care: qualitative study of rurality and age differences. JMIR mHealth uHealth. 2018;6:e10748.
Evans HL, Lober WB, RJ L, M D. A pilot use of patient-generated wound data to improve postdischarge surgical site infection monitoring. JAMA Surg. 2017;23:514–25.
Ramirez V, Todd J. Top mobile-friendly U.S. cities—NerdWallet. NerdWallet. 2016. https://www.nerdwallet.com/blog/utilities/top-mobile-friendly-cities-2016/. Accessed 13 Aug 2018.
Peiris D, Miranda JJ, Mohr DC. Going beyond killer apps: building a better mHealth evidence base handling. BMJ Glob Health. 2018;3:676.
Gelbard M, Goldstein I, Hellstrom WJG, McMahon CG, Smith T, Tursi J, et al. Clinical efficacy, safety and tolerability of collagenase clostridium histolyticum for the treatment of peyronie disease in 2 large double-blind, randomized, placebo controlled phase 3 studies. J Urol.2013;190:199–207.
Hellstrom WJG, Feldman R, Rosen RC, Smith T, Kaufman G, Tursi J. Sexual function/infertility bother and distress associated with Peyronie’s disease: validation of the Peyronie’s Disease Questionnaire. 2013. http://ac.els-cdn.com/S0022534713002309/1-s2.0-S0022534713002309-main.pdf?_tid=f4a2d6fa-2542-11e7-8667-00000aacb361&acdnat=1492635696_0b53b12229ae5a1b5b9eb5bc98e376b7. Accessed 19 April 2017.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Brisbane, W.G., Rogers, M.J., Hsi, R.S. et al. Comparison of clinician and patient users of a mobile phone application to assess penile curvature in Peyronie’s disease. Int J Impot Res 32, 401–408 (2020). https://doi.org/10.1038/s41443-019-0150-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41443-019-0150-y
This article is cited by
-
3D-printed phantoms to quantify accuracy and variability of goniometric and volumetric assessment of Peyronie’s disease deformities
International Journal of Impotence Research (2022)
-
A model for digital innovations in sexual medicine
International Journal of Impotence Research (2020)