Abstract
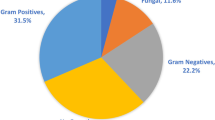
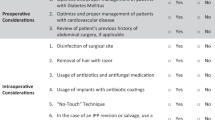
The purpose of this study is to investigate the relationship between inflatable penile prosthesis (IPP) infection, time of year, climate, temperature and humidity. This is a retrospective IRB-approved analysis of 211 patients at 25 institutions who underwent salvage procedure or device explant between 2001 and 2016. Patient data were compiled after an extensive review of all aspects of their electronic medical records. Climate data were compiled from monthly norms based on location, as well as specific data regarding temperature, dew point, and humidity from dates of surgery. Rigorous statistical analysis was performed. We found that penile prosthesis infections occurred more commonly in June (n = 24) and less frequently during the winter months (n = 39), with the lowest number occurring in March (n = 11). One-hundred thirty-nine infections occurred at average daily temperatures greater than 55 °F, compared to 72 infections at less than 55 °F. The incidence rate ratio for this trend was 1.93, with a p-value of <0.001. Humidity results were similar, and fungal infections correlate with daily humidity. Infected implants performed in the fall and summer were over 3 and 2.3 times, respectively, more likely to grow Gram-positive bacteria compared to implants performed in spring (p = 0.004; p = 0.039). This was consistent across geographic location, including in the Southern hemisphere. We found trends between climate factors and IPP infection like those seen and proven in other surgical literature. To our knowledge these data represent the first exploration of the relationship between temperature and infection in prosthetic urology.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 8 print issues and online access
$259.00 per year
only $32.38 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
References
Katz DJ, Stember DS, Nelson CJ, Mulhall JP. Perioperative prevention of penile prosthesis infection: practice patterns among surgeons of SMSNA and ISSM. J Sex Med. 2012;9:1705–12.
Eid JF. No-touch technique. J Sex Med. 2011;8:5–8.
Sadeghi-Nejad H, Ilbeigi P, Wilson SK, Delk JR, Siegel A, Seftel AD, et al. Multi-institutional outcome study on the efficacy of closed-suction drainage of the scrotum in three-piece inflatable penile prosthesis surgery. Int J Impot Res. 2005;17:535–8.
Balen A, Gross MS, Phillips EA, Henry GD, Munarriz R. Active polysubstance abuse concurrent with surgery as a possible newly identified infection risk factor in inflatable penile prosthesis placement based on a retrospective analysis of health and socioeconomic factors. J Sex Med. 2016;13:697–701.
Wilson SK, Delk JR II. Inflatable penile implant infection; predisposing factors and treatment suggestions. J Urol. 1995;153:659–61.
Wolf JS, Bennett CJ, Dmochowski RR, Hollenbeck BK, Pearle MS, Schaeffer AJ. Best practice policy statement on urologic surgery antimicrobial prophylaxis. J Urol. 2008;179:1379–90.
Grabe M, Bartoletti R, Bjerklund Johansen TE, Cai T, Cek M, Koves B, et al. Guidelines on urological infections. European Association of Urology 2015;55–58. https://uroweb.org/wp-content/uploads/19-Urological-infections_LR2.pdf.
Mandava SH, Serefoglu EC, Freier MT, Wilson SK, Hellstrom WJ. Infection retardant coated inflatable penile prostheses decrease the incidence of infection: a systematic review and meta-analysis. J Urol. 2012;188:1855–60.
Richardson B, Caire A, Hellstrom WJ. Retrospective long-term analysis of titan hydrophilic coating: positive reduction of infection compared to non-coated device. J Sx Med. 2010;7:28.
Dhabuwala C, Sheth S, Zamzow B. Infection rates of rifampin/gentamicin-coated titan coloplast implants. Comparison with inhibizone-impregnated AMS penile implants. J Sex Med. 2011;8:315–20.
Wilson SK, Costerton JW. Biofilm and penile prosthesis infections in the era of coated implants: a review. J Sex Med. 2012;9:44–53.
Carson CC III, Mulcahy JJ, Harsch MR. Long-term infection outcomes after original antibiotic impregnated inflatable penile prosthesis implants: up to 7.7 years of follow-up. J Urol. 2011;1:614–8.
Gross MS, Phillips EA, Carrasquillo RJ, Thornton A, Greenfield JM, Levine LA, et al. Multicenter investigation of the micro-organisms involved in penile prosthesis infection: an analysis of the efficacy of the AUA and EAU guidelines for penile prosthesis prophylaxis. J Sex Med. 2017;14:455–63.
Taplin D, Zaias N, Rebell G. Environmental influences on microbiology of the skin. Arch Environ Health. 1965;11:546–50.
Jawad A, Heritage J, Snelling AM, Gascoyne-Binzi DM, Hawkey PM. Influence of relative humidity and suspending menstrua on survival of acinetobacter spp. on dry surfaces. J Clin Microbiol. 1996;34:2881–7.
Kaier K, Frank U, Conrad A, Meyer E, et al. Seasonal and ascending trends in the incidence of carriage of extended-spectrum-ß-lactamase-producing e. coli and klebsiella species in 2 german hospitals. Infect Control Hosp Epidemiol. 2010;31:1154–9.
Eber MR, Shardell M, Schweizer ML, Laxminarayan R, Perencevich EN. Seasonal and temperature-associated increase in gram negative bacterial bloodstream infections among hospitalized patients. PloS ONE. 2011;6:e25298.
Grassly NC, Fraser C. Seasonal infectious disease epidemiology. Proc R Soc B. 2006;273:2531–50.
Watcharananan SP, Junchotikul P, Srichanrusmi C, Chanchompoo P, Mavichal V, Kantachuvessiri S, et al. Adenovirus infection after kidney transplantation in thailand: seasonal distribution and potential route of acquisition. Transpl Proc. 2010;42:4091–3.
Ricciardi R, Roberts PL, Read TE, Marcella PW, Hall JF, Schoetz DJ. Cyclical increase in diverticulitis during the summer months. Arch Surg. 2011;146:319–23.
Spaeder MC, Carson KA, Varicella LA. Impact of the viral respiratory season on postoperative outcomes in children undergoing cardiac surgery. Pedia Cardiol. 2011;32:801–6.
Kane P, Chen C, Post Z, Radcliff K, Orozco, Ong A. Seasonality of infection rates after total joint arthroplasty. Orthopedics. 2014;37:182–6.
Gross MS, Phillips EA, Balen A, Eid JF, Yang C, Simon R, et al. The malleable implant salvage technique: infection outcomes after mulcahy salvage procedure and replacement of infected inflatable penile prosthesis with malleable prosthesis. J Urol. 2016;195:694–7.
Marks R, Dawber RP. In situ microbiology of the stratum corneum: an application of skin surface biopsy. Arch Dermatol. 1972;105:216–21.
Miller LG, Kaplan SL. Staphylococcus aureus: a community pathogen. Infect Dis Clin North Am. 2009;23:35–52.
Dailiana ZH, Rigopoulos N, Varitimidis SE, Poultsides L, Petinaki E, Malizos KN. Clinical and epidemiological features of upper-extremity infections caused by staphylococcus aureus carrying the pvl gene: a four-year study in Greece. Med Sci Monit. 2008;14:511–4.
Dhaliwal AS, Chu D, Deswal A, Bozkury B, Coselli JS, LeMaire SA, et al. The July effect and cardiac surgery: the effect of the beginning of the academic cycle on outcomes. Am J Surg. 2008;196:720–5.
Inaba K, Recinos G, Teixeira PG, Barmpara G, Talving P, Salim A, et al. Complications and death at the start of the new academic year: is there a July phenomenon? J Trauma. 2010;68:19–22.
Bakaeen FG, Huh J, Lemaire SA, Coselli JS, Sansgiry S, Atluri PV, et al. The July effect: impact of the beginning of the academic cycle on cardiac surgical outcomes in a cohort of 70,616 patients. Ann Thorac Surg. 2009;88:70–5.
Stout CL, Chapman JR, Scoglietti VC, Long EL, Vaughn DM, Abercrombie CL, et al. “July effect”: an evaluation of a level I teaching hospital’s trauma service seasonal mortality rates. Am Surg. 2008;74:878–9.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
MSG and RM are both consultants for Coloplast. The authors declare that they have no conflict of interest.
Additional information
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Gross, M.S., Vollstedt, A.J., Cleves, M.A. et al. Multicenter investigation on the influence of climate in penile prosthesis infection. Int J Impot Res 32, 387–392 (2020). https://doi.org/10.1038/s41443-019-0148-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41443-019-0148-5
This article is cited by
-
Fungal Infections of Urologic Prostheses and Permanent Devices: a Systematic Review of Current Literature
Current Sexual Health Reports (2022)
-
Prevention of Penile Prosthesis Infection
Current Urology Reports (2022)
-
Editorial Comment on: Multicentre investigation on the influence of climate in penile prosthesis infection
International Journal of Impotence Research (2020)
-
Editorial comment: Multicenter investigation on the influence of climate in penile prosthesis infection
International Journal of Impotence Research (2020)
-
Advances in Infection Prevention Strategies for Penile Prosthesis Surgery
Current Sexual Health Reports (2019)